T Cells Immunophenotyping and CD38 Overexpression as Hallmarks of the Severity of COVID-19 and Predictors of Patients’ Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
- Group 1: Controls: Included 14 age- and sex-matched apparently healthy individuals.
- Group 2: Mild group: Included 22 asymptomatic and clinically mild laboratory-confirmed COVID-19 cases with positive SARS-CoV-2 RT-PCR testing.
- Group 3: Moderate group: Included 22 moderate laboratory-confirmed COVID-19 cases.
- Group 4: Severe group: Included 26 severe and critical laboratory-confirmed COVID-19 cases.
2.2. Ethical Considerations
2.3. Laboratory Work and Data Collection
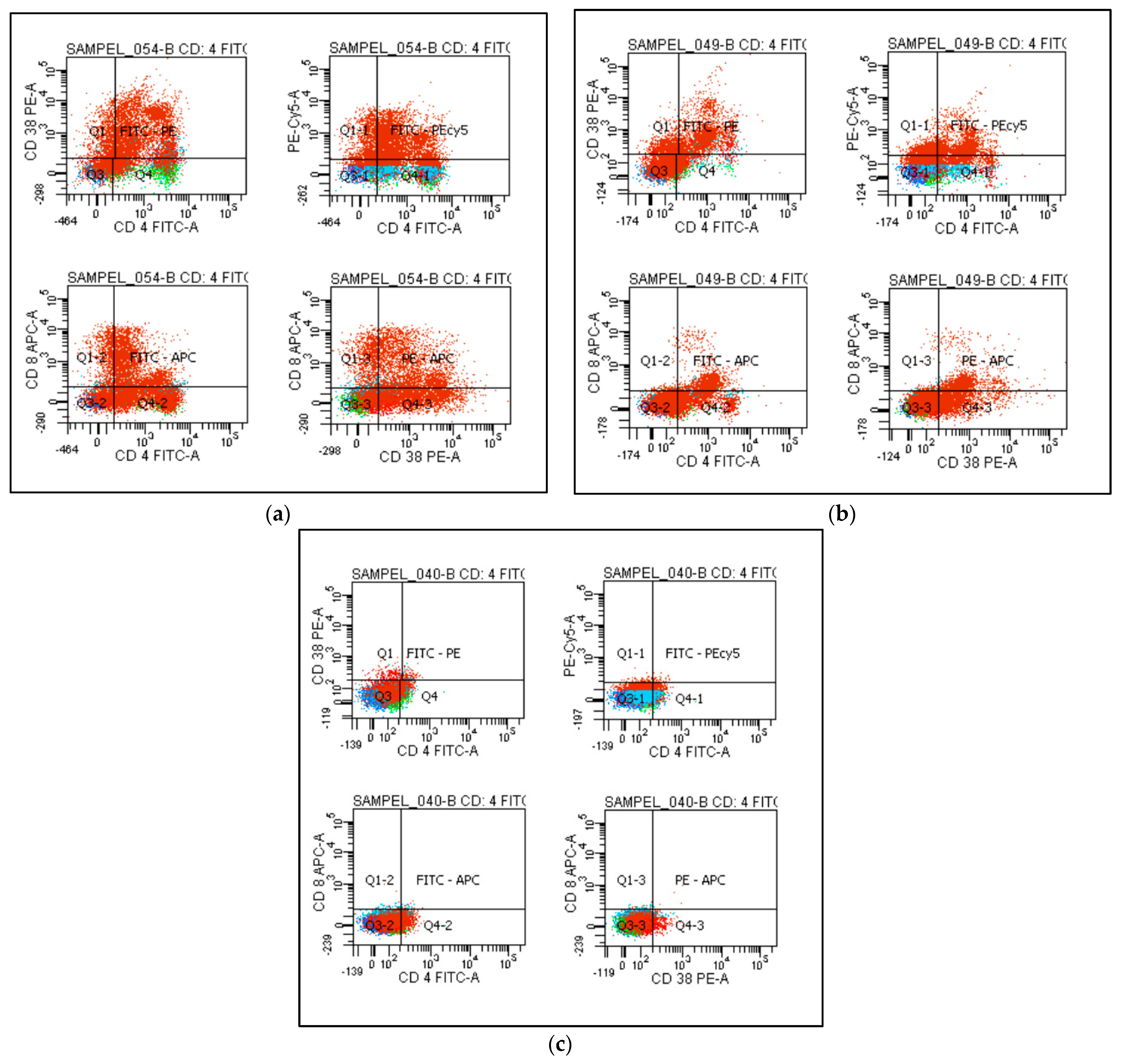
2.4. Flow Cytometry Analysis of T Cell Subtypes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Coronavirus COVID-19 Dashboard; World Health Organization: Geneva, Switzerland, 2020; Available online: https://covid19.who.int (accessed on 8 December 2021).
- Birindelli, S.; Tarkowski, M.S.; Gallucci, M.; Schiuma, M.; Covizzi, A.; Lewkowicz, P.; Aloisio, E.; Falvella, F.S.; Dolci, A.; Riva, A.; et al. Definition of the Immune Parameters Related to COVID-19 Severity. Front. Immunol. 2022, 13, 850846. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus—Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Yin, X.; Sun, H.; Zeng, W.; Xiang, Y.; Zhou, T.; Ma, D.; Yang, C. Manipulating the LUMO distribution of quinoxaline-containing architectures to design electron transport materials: Efficient blue phosphorescent organic light-emitting diodes. Org. Electron. 2020, 37, 439–447. [Google Scholar] [CrossRef]
- Qin, S.; Jiang, Y.; Wei, X.; Liu, X.; Guan, J.; Chen, Y.; Lu, H.; Qian, J.; Wang, Z.; Lin, X. Dynamic changes in monocytes subsets in COVID-19 patients. Hum. Immunol. 2021, 82, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.-D.; Ding, M.; Dong, X.; Zhang, J.-J.; Azkur, A.K.; Azkur, D.; Gan, H.; Sun, Y.-L.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef] [PubMed]
- Malik, P.; Patel, U.; Mehta, D.; Patel, N.; Kelkar, R.; Akrmah, M.; Gabrilove, J.L.; Sacks, H. Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis. BMJ Evid.-Based Med. 2021, 26, 107–108. [Google Scholar] [CrossRef]
- Ponti, G.; Maccaferri, M.; Ruini, C.; Tomasi, A.; Ozben, T. Biomarkers associated with COVID-19 disease progression. Crit. Rev. Clin. Lab. Sci. 2020, 57, 389–399. [Google Scholar] [CrossRef]
- Horenstein, A.; Faini, A.; Malavasi, F. CD38 in the age of COVID-19: A medical perspective. Physiol. Rev. 2021, 101, 1457–1486. [Google Scholar] [CrossRef]
- Siddiqi, H.K.; Mehra, M.R. COVID-19 illness in native and immunosuppressed states: A clinical–therapeutic staging proposal. J. Heart Lung Transplant. 2020, 39, 405–407. [Google Scholar] [CrossRef]
- Qin, C.; Zhou, L.; Hu, Z.; Zhang, S.; Yang, S.; Tao, Y.; Xie, C.; Ma, K.; Shang, K.; Wang, W.; et al. Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China. Clin. Infect. Dis. 2020, 71, 762–768. [Google Scholar] [CrossRef]
- Wang, F.; Hou, H.; Luo, Y.; Tang, G.; Wu, S.; Huang, M.; Liu, W.; Zhu, Y.; Lin, Q.; Mao, L.; et al. The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI Insight 2020, 5, e137799. [Google Scholar] [CrossRef] [PubMed]
- Mescher, M.F.; Curtsinger, J.M.; Agarwal, P.; Casey, K.A.; Gerner, M.; Hammerbeck, C.D.; Popescu, F.; Xiao, Z. Signals required for programming effector and memory development by CD8+ T cells. Immunol. Rev. 2006, 211, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Ganji, A.; Farahani, I.; Khansarinejad, B.; Ghazavi, A.; Mosayebi, G. Increased expression of CD8 marker on T-cells in COVID-19 patients. Blood Cells Mol. Dis. 2020, 83, 102437. [Google Scholar] [CrossRef]
- Diao, B.; Wang, C.; Tan, Y.; Chen, X.; Liu, Y.; Ning, L.; Chen, L.; Li, M.; Liu, Y.; Wang, G.; et al. Reduction and Functional Exhaustion of T Cells in Patients with Coronavirus Disease 2019 (COVID-19). Front. Immunol. 2020, 11, 827. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.T.; Snell, L.M.; Brooks, D.G.; Oldstone, M.B. Networking at the Level of Host Immunity: Immune Cell Interactions during Persistent Viral Infections. Cell Host Microbe 2013, 13, 652–664. [Google Scholar] [CrossRef]
- Nesrin, I. Tarbiah: COVID-19, T Cells, Cytokines and Immunotherapy: Review. J. Pharm. Res. Int. 2021, 33, 70–82. [Google Scholar]
- Huang, I.; Pranata, R. Lymphopenia in severe coronavirus disease-2019 (COVID-19): Systematic review and meta-analysis. J. Intensive Care 2020, 8, 36. [Google Scholar] [CrossRef] [PubMed]
- Dennison, D.; Al Khabori, M.; Al Mamari, S.; Aurelio, A.; Al Hinai, H.; Al Maamari, K.; Alshekaili, J.; Al Khadouri, G. Circulating activated neutrophils in COVID-19: An independent predictor for mechanical ventilation and death. Int. J. Infect. Dis. 2021, 106, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Wherry, E.J. T cell responses in patients with COVID-19. Nat. Rev. Immunol. 2020, 20, 529–536. [Google Scholar] [CrossRef]
- Mathew, D.; Giles, J.R.; Baxter, A.E.; Oldridge, D.A.; Greenplate, A.R.; Wu, J.E.; Alanio, C.; Kuri-Cervantes, L.; Pampena, M.B.; D’Andrea, K.; et al. Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science 2020, 369, eabc8511. [Google Scholar] [CrossRef]
- Sriram, K.; Insel, P.A. Inflammation and thrombosis in COVID-19 pathophysiology: Proteinase-activated and purinergic receptors as drivers and candidate therapeutic targets. Physiol. Rev. 2021, 101, 545–567. [Google Scholar] [CrossRef]
- Fajgenbaum, D.C.; June, C.H. Cytokine Storm. N. Engl. J. Med. 2020, 383, 2255–2273. [Google Scholar] [CrossRef]
- Moccia, F.; Gerbino, A.; Lionetti, V.; Miragoli, M.; Munaron, L.M.; Pagliaro, P.; Pasqua, T.; Penna, C.; Rocca, C.; Samaja, M.; et al. COVID-19-associated cardiovascular morbidity in older adults: A position paper from the Italian Society of Cardiovascular Researches. Geroscience 2020, 42, 1021–1049. [Google Scholar] [CrossRef] [PubMed]
- Chini, C.; Hogan, K.A.; Warner, G.M.; Tarragó, M.G.; Peclat, T.R.; Tchkonia, T.; Kirkland, J.L.; Chini, E. The NADase CD38 is induced by factors secreted from senescent cells providing a potential link between senescence and age-related cellular NAD+ decline. Biochem. Biophys. Res. Commun. 2019, 513, 486–493. [Google Scholar] [CrossRef] [PubMed]
- Kouhpayeh, S.; Shariati, L.; Boshtam, M.; Rahimmanesh, I.; Mirian, M.; Zeinalian, M.; Salari-Jazi, A.; Khanahmad, N.; Damavandi, M.S.; Sadeghi, P.; et al. The molecular story of COVID-19; NAD+ depletion addresses all questions in this infection. Preprints 2020, 2020030346. [Google Scholar] [CrossRef]
- Gul, R.; Kim, U.-H.; Alfadda, A.A. Renin-angiotensin system at the interface of COVID-19 infection. Eur. J. Pharmacol. 2021, 890, 173656. [Google Scholar] [CrossRef]
- National Health Commission of China. New Coronavirus Pneumonia Prevention and Control Program. Available online: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtmlspm=C73544894212.P59511941341.0.0, (accessed on 5 July 2020).
- Iype, E.; Gulati, S. Understanding the asymmetric spread and case fatality rate (CFR) for COVID-19 among countries. medRxiv 2020, 20073791. [Google Scholar] [CrossRef]
- Moore, J.B.; June, C.H. Cytokine release syndrome in severe COVID-19. Science 2020, 368, 473–474. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Melo, D.; Nilsson-Payant, B.E.; Liu, W.-C.; Uhl, S.; Hoagland, D.; Møller, R.; Jordan, T.X.; Oishi, K.; Panis, M.; Sachs, D.; et al. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell 2020, 181, 1036–1045.e9. [Google Scholar] [CrossRef]
- Zheng, M.; Gao, Y.; Wang, G.; Song, G.; Liu, S.; Sun, D.; Xu, Y.; Tian, Z. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell. Mol. Immunol. 2020, 17, 533–535. [Google Scholar] [CrossRef]
- Zheng, H.-Y.; Zhang, M.; Yang, C.-X.; Zhang, N.; Wang, X.-C.; Yang, X.-P.; Dong, X.-Q.; Zheng, Y.-T. Elevated exhaustion levels and reduced functional diversity of T cells in peripheral blood may predict severe progression in COVID-19 patients. Cell. Mol. Immunol. 2020, 17, 541–543. [Google Scholar] [CrossRef]
- Thevarajan, I.; Nguyen, T.H.O.; Koutsakos, M.; Druce, J.; Caly, L.; van de Sandt, C.E.; Jia, X.; Nicholson, S.; Catton, M.; Cowie, B.; et al. Breadth of concomitant immune responses prior to patient recovery: A case report of non-severe COVID-19. Nat. Med. 2020, 26, 453–455. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H.; et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. 2020, 130, 2620–2629. [Google Scholar] [CrossRef]
- Zhao, Q.; Meng, M.; Kumar, R.; Wu, Y.; Huang, J.; Deng, Y.; Weng, Z.; Yang, L. Lymphopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A systemic review and meta-analysis. Int. J. Infect. Dis. 2020, 96, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Zeidler, J.D.; Kashyap, S.; Hogan, K.A.; Chini, E.N. Hogan, and Eduardo Nunes Chini. Implications of The NADase CD38 in COVID Pathophysiology. Physiol. Rev. 2022, 102, 339–341. [Google Scholar] [CrossRef]
- Obeid, D.A.; Alsanea, M.S.; Alnemari, R.T.; Al-Qahtani, A.A.; Althawadi, S.I.; Mutabagani, M.S.; Almaghrabi, R.S.; Alhadheq, F.M.; Alahideb, B.M.; Alhamlan, F.S. SARS-CoV-2 genetic diversity and variants of concern in Saudi Arabia. J. Infect. Dev. Ctries 2021, 15, 1782–1791. [Google Scholar] [CrossRef] [PubMed]
- Alhamlan, F.; Al-Qahtani, A.; Obeid, D.; Aljumaah, S.; Alghamdi, S.; Alnafee, K.; Alsanea, M.; Alahideb, B.; Almutairi, S.; Alsuwairi, F.; et al. SARS-CoV-2 Delta Variant Predominant at a Tertiary-Care Hospital in Saudi Arabia. Res. Sq. Prepr. 2021, 1–20. [Google Scholar] [CrossRef]
- Alhasan, K.; Aljamaan, F.; Temsah, M.-H.; Alshahrani, F.; Bassrawi, R.; Alhaboob, A.; Assiri, R.; Alenezi, S.; Alaraj, A.; Alhomoudi, R.I.; et al. COVID-19 Delta Variant: Perceptions, Worries, and Vaccine-Booster Acceptability among Healthcare Workers. Healthcare 2021, 9, 1566. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Nie, J.; Wang, H.; Zhao, Q.; Xiong, Y.; Deng, L.; Song, S.; Ma, Z.; Mo, P.; Zhang, Y. Characteristics of Peripheral Lymphocyte Subset Alteration in COVID-19 Pneumonia. J. Infect. Dis. 2020, 221, 1762–1769. [Google Scholar] [CrossRef]
- Ashrafi, F.; Nematollahi, P.; Salmasi, M.; Hedayat, A.; Amra, B. Association of lymphocyte subsets with mortality in severe COVID-19 pneumonia patients. J. Clin. Lab. Anal. 2021, 35, e24046. [Google Scholar] [CrossRef]
- Sekine, T.; Perez-Potti, A.; Rivera-Ballesteros, O.; Strålin, K.; Gorin, J.-B.; Olsson, A.; Llewellyn-Lacey, S.; Kamal, H.; Bogdanovic, G.; Muschiol, S.; et al. Robust T Cell Immunity in Convalescent Individuals with Asymptomatic or Mild COVID-19. Cell 2020, 183, 158–168.e14. [Google Scholar] [CrossRef]
- He, R.; Lu, Z.; Zhang, L.; Fan, T.; Xiong, R.; Shen, X.; Feng, H.; Meng, H.; Lin, W.; Jiang, W.; et al. The clinical course and its correlated immune status in COVID-19 pneumonia. J. Clin. Virol. 2020, 127, 104361. [Google Scholar] [CrossRef]
- Liu, J.; Li, S.; Liu, J.; Liang, B.; Wang, X.; Wang, H.; Li, W.; Tong, Q.; Yi, J.; Zhao, L.; et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine 2020, 55, 102763. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Berube, J.; McNamara, M.; Saksena, S.; Hartman, M.; Arshad, T.; Bornheimer, S.J.; O’Gorman, M. Lymphocyte subset counts in COVID-19 patients: A meta-analysis. Cytom. Part A 2020, 97, 772–776. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Xu, H.; Yang, M.; Zeng, Y.; Chen, H.; Liu, R.; Li, Q.; Zhang, N.; Wang, D. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J. Clin. Virol. 2020, 127, 104366. [Google Scholar] [CrossRef]
- Chan, S.S.W.; Christopher, D.; Tan, G.B.; Chong, V.C.L.; Fan, B.E.; Lin, C.Y.; Ong, K.H. Peripheral lymphocyte subset alterations in COVID-19 patients. Int. J. Lab. Hematol. 2020, 42, e199–e203. [Google Scholar] [CrossRef]
- Bobcakova, A.; Barnova, M.; Vysehradsky, R.; Petriskova, J.; Kocan, I.; Diamant, Z.; Jesenak, M. Activated CD8+CD38+ Cells Are Associated with Worse Clinical Outcome in Hospitalized COVID-19 Patients. Front. Immunol. 2022, 13, 861666. [Google Scholar] [CrossRef] [PubMed]
- Wilk, A.J.; Rustagi, A.; Zhao, N.Q.; Roque, J.; Martínez-Colón, G.J.; McKechnie, J.L.; Ivison, G.T.; Ranganath, T.; Vergara, R.; Hollis, T.; et al. A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat. Med. 2020, 26, 1070–1076. [Google Scholar] [CrossRef]
- Lagunas-Rangel, F.A. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): A meta-analysis. J. Med. Virol. 2020, 92, 1733–1734. [Google Scholar] [CrossRef] [PubMed]
- Agrati, C.; Castilletti, C.; Casetti, R.; Sacchi, A.; Falasca, L.; Turchi, F.; Tumino, N.; Bordoni, V.; Cimini, E.; Viola, D.; et al. Longitudinal characterization of dysfunctional T cell-activation during human acute Ebola infection. Cell Death Dis. 2016, 7, e2164. [Google Scholar] [CrossRef]
- Ndhlovu, Z.M.; Kamya, P.; Mewalal, N.; Kløverpris, H.N.; Nkosi, T.; Pretorius, K.; Laher, F.; Ogunshola, F.; Chopera, D.; Shekhar, K.; et al. Magnitude and Kinetics of CD8+ T Cell Activation during Hyperacute HIV Infection Impact Viral Set Point. Immunity 2015, 43, 591–604. [Google Scholar] [CrossRef]
- Clavarino, G.; Leroy, C.; Epaulard, O.; Raskovalova, T.; Vilotitch, A.; Pernollet, M.; Dumestre-Pérard, C.; Defendi, F.; Le Maréchal, M.; Le Gouellec, A.; et al. Fine Analysis of Lymphocyte Subpopulations in SARS-CoV-2 Infected Patients: Differential Profiling of Patients with Severe Outcome. Front. Immunol. 2022, 13, 889813. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Liu, J.; Zhang, D.; Xu, Z.; Ji, J.; Wen, C. Cytokine Storm in COVID-19: The Current Evidence and Treatment Strategies. Front. Immunol. 2020, 11, 1708. [Google Scholar] [CrossRef]
- Miller, R.; Wentzel, A.R.; Richards, G.A. COVID-19: NAD+ deficiency may predispose the aged, obese and type2 diabetics to mortality through its effect on SIRT1 activity. Med. Hypothes. 2020, 144, 110044. [Google Scholar] [CrossRef]
- Shaw, A.C.; Goldstein, D.R.; Montgomery, R.R. Age-dependent dysregulation of innate immunity. Nat. Rev. Immunol. 2013, 13, 875–887. [Google Scholar] [CrossRef] [PubMed]
- Kapustova, L.; Petrovicova, O.; Banovcin, P.; Antosova, M.; Bobcakova, A.; Urbancikova, I.; Rennerova, Z.; Jesenak, M. COVID-19 and the Differences in Physiological Background between Children and Adults and Their Clinical Consequences. Physiol. Res. 2021, 70, S209–S225. [Google Scholar] [CrossRef] [PubMed]
- Conti, P.; Younes, A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: Clinical response to viral infection. J. Biol. Regul. Homeost. Agents 2020, 34, 339–343. [Google Scholar] [PubMed]
- Sharma, G.; Volgman, A.S.; Michos, E.D. Sex differences in mortality from COVID-19 pandemic: Are men vulnerable and women protected? Case Rep. 2020, 2, 1407–1410. [Google Scholar]
- Matalonga, J.; Glaria, E.; Bresque, M.; Escande, C.; Carbó, J.M.; Kiefer, K.; Vicente, R.; León, T.E.; Beceiro, S.; Pascual-García, M.; et al. The Nuclear Receptor LXR Limits Bacterial Infection of Host Macrophages through a Mechanism that Impacts Cellular NAD Metabolism. Cell Rep. 2017, 18, 1241–1255. [Google Scholar] [CrossRef]
- Partida-Sánchez, S.; Cockayne, D.A.; Monard, S.; Jacobson, E.L.; Oppenheimer, N.; Garvy, B.; Kusser, K.; Goodrich, S.; Howard, M.; Harmsen, A.; et al. Cyclic ADP-ribose production by CD38 regulates intracellular calcium release, extracellular calcium influx and chemotaxis in neutrophils and is required for bacterial clearance in vivo. Nat. Med. 2001, 7, 1209–1216. [Google Scholar] [CrossRef] [PubMed]
| Participants | N | % | ||
|---|---|---|---|---|
| Groups/ Age (First Quartiles, Median, Third Quartiles) | Group 1 | Controls | 14 | 17.6% |
| Age (40.25) (44.5) (52) | ||||
| Group 2 | Mild or asymptomatic cases | 22 | 25.9% | |
| Age (33.75) (38.5) (44.25) | ||||
| Group 3 | Moderate cases | 22 | 25.9% | |
| Age (42.75) (54) (65.25) | ||||
| Group 4 | Severe or critical cases | 26 | 30.6% | |
| Age (46) (63) (67.25) | ||||
| Gender | Male | 47 | 55.9% | |
| Female | 37 | 44.1% | ||
| Controls | Cases | ||
|---|---|---|---|
| Mean ± SD | Mean ± SD | Reference Range | |
| WBCs K/UL | 6.01 ± 1.4 | 9.3 ± 4.99 | 4.5–10.5 |
| NU K/UL | 3.48 ± 1.32 | 7.45 ± 5.04 | 2.5–8 |
| LY K/UL | 2.17 ± 0.51 | 1.49 ± 1.03 | 0.9–5.1 |
| NU/LY | 1.74 ± 0.97 | 9.81 ± 13.84 | - |
| EO K/UL | 0.12 ± 0.13 | 0.14 ± 0.28 | 0.1–0.7 |
| Plat. K/UL | 288.73 ± 66.83 | 296.73 ± 104.84 | 150–450 |
| HB gm/dL | 12.19 ± 1.35 | 12.61 ± 1.89 | 12–15.5 |
| AST U/L | 23 ± 6.72 | 49.2 ± 39.47 | 0–50 |
| ALT U/L | 24.93 ± 10.05 | 47.89 ± 45.05 | 0–50 |
| S. Cr Umol/L | 58.87 ± 13.33 | 82.48 ± 42.74 | 53–123 |
| BUN mmol/L | 3.4 ± 1.05 | 6.84 ± 5.21 | 2.5–6.4 |
| Controls | Cases | ||
|---|---|---|---|
| N (%) | N (%) | ||
| Gender | Male | 7 (46.67%) | 40 (57.14%) |
| Female | 8 (53.33%) | 30 (42.86%) | |
| WBC count | Normal | 15 (100%) | 44 (62.86%) |
| Increased | 0 (0%) | 23 (32.86%) | |
| Decreased | 0 (0%) | 3 (4.29%) | |
| NU count | Normal | 15 (100%) | 69 (98.57%) |
| Increased | 0 (0%) | 1 (1.43%) | |
| LY count | Normal | 15 (100%) | 41 (58.57%) |
| Decreased | 0 (0%) | 29 (41.43%) | |
| EO count | Normal | 14 (93.33%) | 26 (37.14%) |
| Increased | 0 (0%) | 3 (4.29%) | |
| Decreased | 1 (6.67%) | 41 (58.57%) | |
| Plat. count | Normal | 15 (100%) | 60 (85.71%) |
| Increased | 0 (0%) | 6 (8.57%) | |
| Decreased | 0 (0%) | 4 (5.71%) | |
| HB level | Normal | 14 (93.33%) | 56 (80%) |
| Decreased | 1 (6.67%) | 14 (20%) | |
| AST level | Normal | 15 (100%) | 48 (68.57%) |
| Increased | 0 (0%) | 22 (31.43%) | |
| ALT level | Normal | 15 (100%) | 49 (70%) |
| Increased | 0 (0%) | 21 (30%) | |
| S. Cr level | Normal | 15 (100%) | 59 (84.29%) |
| Increased | 0 (0%) | 10 (14.29%) | |
| Decreased | 0 (0%) | 1 (1.43%) | |
| BUN level | Normal | 15 (100%) | 39 (55.71%) |
| Increased | 0 (0%) | 30 (42.86%) | |
| Decreased | 0 (0%) | 1 (1.43%) | |
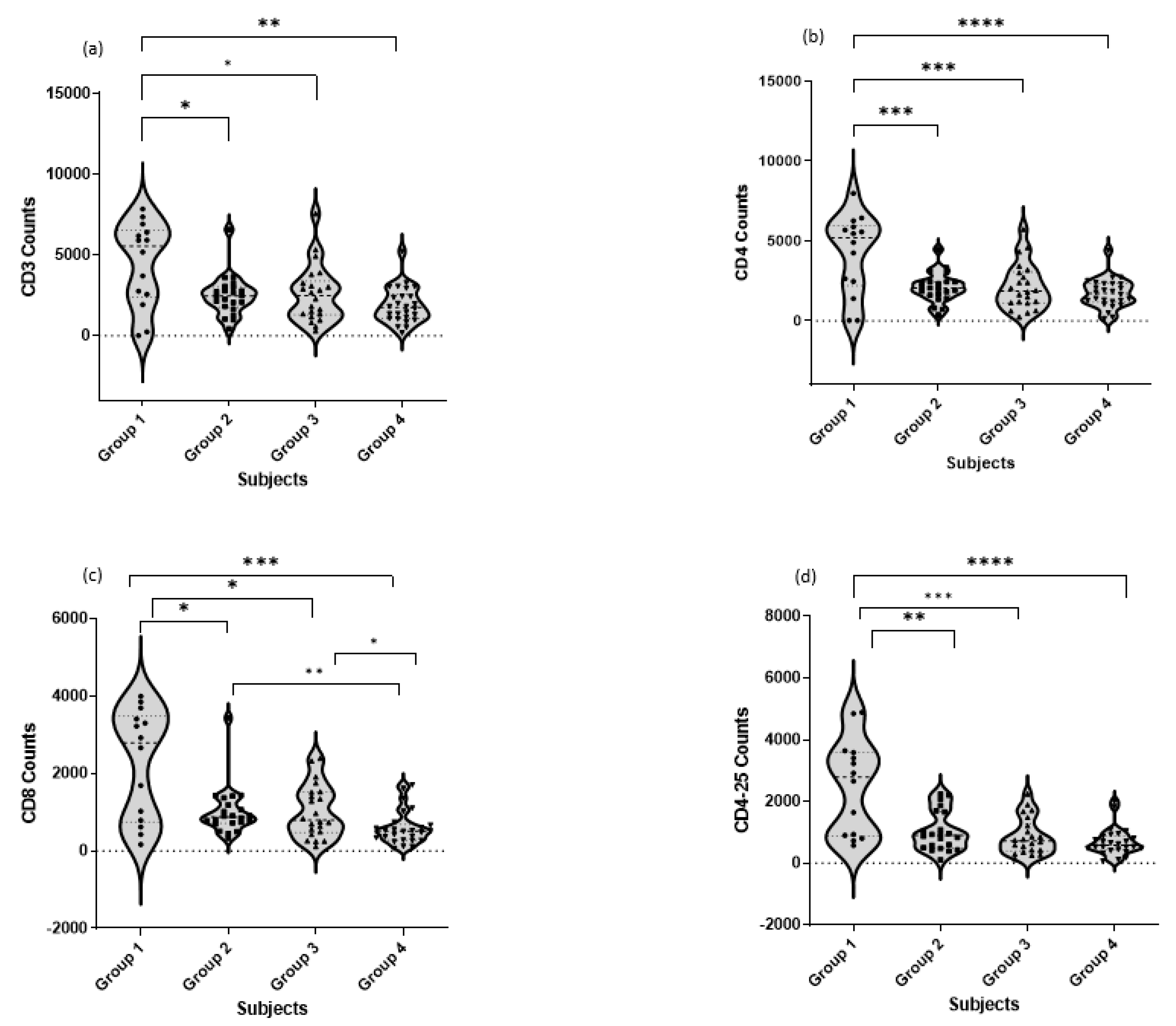
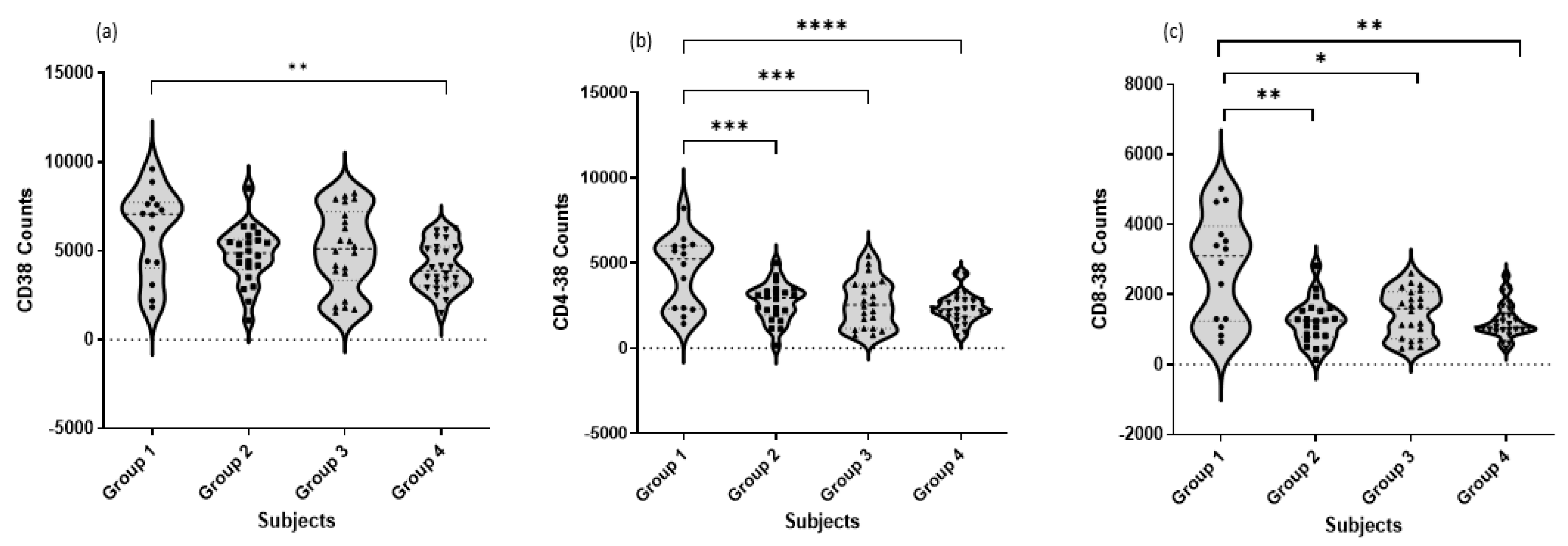
| T Cell Subtypes | Controls | Mild/Asymptomatic Cases | Moderate Cases | Severe/Critical Cases |
|---|---|---|---|---|
| CD3 Cells % Mean ± SD | 41.15 ± 4.823 | 23.45 ± 2.701 | 22.49 ± 2.894 | 17.55 ± 2.083 |
| CD4 Cells % Mean ± SD | 39.11 ± 4.488 | 20.11 ± 2.026 | 20.11 ± 2.026 | 16.08 ± 1.734 |
| CD8 Cells % of Mean ± SD | 20.85 ± 3.201 | 12.22 ± 2.302 | 8.868 ± 1.304 | 5.492 ± 0.7858 |
| CD4CD25 Cells % Mean ± SD | 21.94 ± 3.517 | 9.500 ± 1.205 | 7.718 ± 1.022 | 6.592 ± 0.8424 |
| CD38 Cells % of Mean ± SD | 55.38 ± 6.092 | 44.10 ± 3.331 | 43.83 ± 4.186 | 39.13 ± 2.821 |
| CD4CD38 Cells % Mean ± SD | 36.93 ± 3.868 | 24.42 ± 2.136 | 19.46 ± 2.330 | 16.61 ± 1.782 |
| CD8CD38 Cells % Mean ± SD | 24.85 ± 3.501 | 11.31 ± 1.278 | 13.32 ± 1.313 | 11.85 ± 0.9256 |
| Mild/Asymptomatic Cases | Moderate Cases | Severe/Critical Cases | |||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | F | p-Value | |
| Age | 38.23 ± 8.09 | 52.68 ± 14.86 | 60.5 ± 14.07 | 18.324 | <0.001 a |
| WBCs K/UL | 7.56 ± 2.49 | 7.07 ± 3.77 | 12.66 ± 5.74 | 12.565 | <0.001 b |
| NU K/UL | 4.52 ± 2 | 5.63 ± 3.54 | 11.47 ± 5.37 | 21.371 | <0.001 b |
| LY K/UL | 2.49 ± 0.64 | 1.16 ± 0.63 | 0.91 ± 0.95 | 27.933 | <0.001 a |
| NU/LY | 1.81 ± 0.58 | 5.71 ± 4.21 | 20.06 ± 18.26 | 17.33 | <0.001 b |
| EO K/UL | 0.27 ± 0.24 | 0.06 ± 0.14 | 0.1 ± 0.35 | 4.046 | 0.022 c |
| Plat. K/UL | 290.68 ± 82.98 | 285.05 ± 86.21 | 311.73 ± 133.88 | 0.432 | 0.651 |
| HB gm/dL | 12.95 ± 1.55 | 12.24 ± 1.81 | 12.65 ± 2.21 | 0.784 | 0.461 |
| AST U/L | 25.64 ± 9.82 | 47.38 ± 34.11 | 70.62 ± 47.51 | 9.775 | <0.001 d |
| ALT U/L | 23.23 ± 8.53 | 55.18 ± 60.51 | 62.58 ± 40.72 | 5.634 | 0.005 a |
| S.Cr Umol/L | 62.59 ± 14.79 | 73.24 ± 37.37 | 106.77 ± 51.32 | 8.668 | <0.001 b |
| BUN mmol/L | 3.47 ± 1.53 | 5.39 ± 2.31 | 10.91 ± 6.28 | 21.235 | <0.001 b |
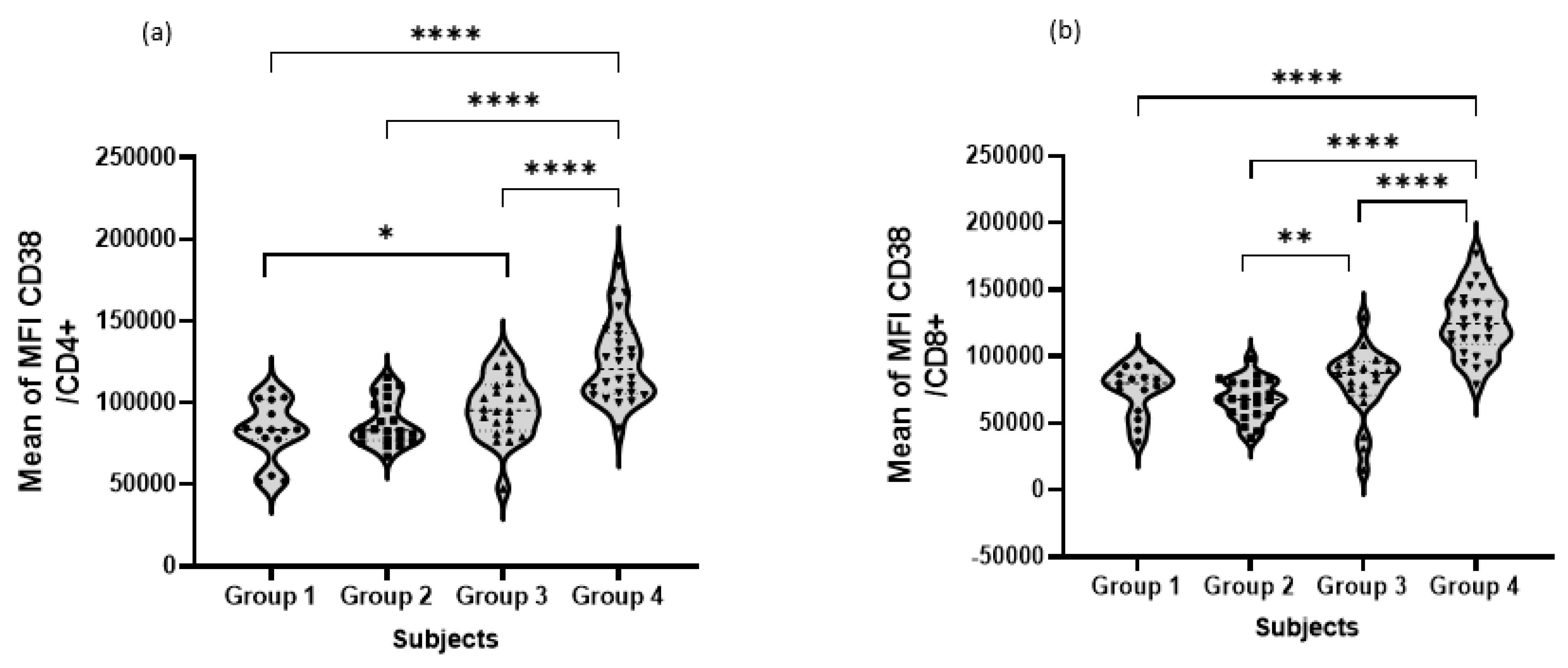
| CD38 exp. on CD4+ T cells (MFI) × 103 | 88.00 ± 13,947.66 | 96.94 ± 19,301.2 | 125.64 ± 24,802.79 | 23.147 | <0.001 b |
| CD38 exp. on CD8+ T cells (MFI) × 103 | 67.74 ± 14,828.01 | 78.52 ± 23,801.7 | 125.77 ± 24,581.98 | 49.259 | <0.001 b |
| Mild/Asymptomatic Cases | Moderate Cases | Severe/Critical Cases | ||||
|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | Value | p-Value | ||
| Gender | Male | 5 (22.73%) a | 13 (59.09%) b | 22 (84.62%) b | X2 = 18.69 | <0.001 |
| Female | 17(77.27%) a | 9 (40.91%) b | 4 (15.38%) b | |||
| WBC count | Normal | 18 (81.82%) a | 17 (77.27%) a | 9 (34.62%) b | Fisher exact test | 0.001 |
| Increased | 3 (13.64%) a | 4 (18.18%) a | 16 (61.54%) b | |||
| Decreased | 1 (4.55%) a | 1 (4.55%) a | 1 (3.85%) a | |||
| NU count | Normal | 22 (100%) | 22 (100%) | 25 (96.15%) | Fisher exact test | 1.000 |
| Increased | 0 (0%) | 0 (0%) | 1 (3.85%) | |||
| LY count | Normal | 22 (100%) a | 15 (68.18%) b | 4 (15.38%) c | X2 = 36.38 | <0.001 |
| Decreased | 0 (0%) a | 7 (31.82%) b | 22 (84.62%) c | |||
| EO count | Normal | 18 (81.82%) a | 6 (27.27%) b | 2 (7.69%) b | Fisher exact test | <0.001 |
| Increased | 2 (9.09%) a | 0 (0%) a | 1 (3.85%) a | |||
| Decreased | 2 (9.09%) a | 16 (72.73%) b | 23 (88.46%) b | |||
| Plat. count | Normal | 21 (95.45%) a | 21 (95.45%) a | 18 (69.23%) b | Fisher exact test | 0.027 |
| Increased | 0 (0%) a | 1 (4.55%) a | 5 (19.23%) b | |||
| Decreased | 1 (4.55%) a | 0 (0%) a | 3 (11.54%) b | |||
| HB level | Normal | 21 (95.45%) | 16 (72.73%) | 19 (73.08%) | Fisher exact test | 0.072 |
| Decreased | 1 (4.55%) | 6 (27.27%) | 7 (26.92%) | |||
| AST level | Normal | 22 (100%) a | 15 (68.18%) b | 11 (42.31%) b | X2 = 18.41 | <0.001 |
| Increased | 0 (0%) a | 7 (31.82%) b | 15 (57.69%) b | |||
| ALT level | Normal | 22 (100%) a | 16 (72.73%) b | 11 (42.31%) b | X2 = 19 | <0.001 |
| Increased | 0 (0%) a | 6 (27.27%) b | 15 (57.69%) b | |||
| S. Cr level | Normal | 22 (100%) a | 19 (86.36%) a,b | 18 (69.23%) b | Fisher exact test | 0.005 |
| Increased | 0 (0%) a | 2 (9.09%) a,b | 8 (30.77%) b | |||
| Decreased | 0 (0%) a | 1 (4.55%) a | 0 (0%) a | |||
| BUN level | Normal | 20 (90.91%) a | 15 (68.18%) a | 4 (15.38%) b | Fisher exact test | <0.001 |
| Increased | 2 (9.09%) a | 6 (27.27%) a | 22 (84.62%) b | |||
| Decreased | 0 (0%) a | 1 (4.55%) a | 0 (0%) a | |||
| Mortality | Survivors | 22 (100%) a | 21 (95.45%) a | 15 (57.69%) b | Fisher exact test | <0.001 |
| Deceased | 0 (0%) a | 1 (4.55%) a | 11 (42.31%) b |
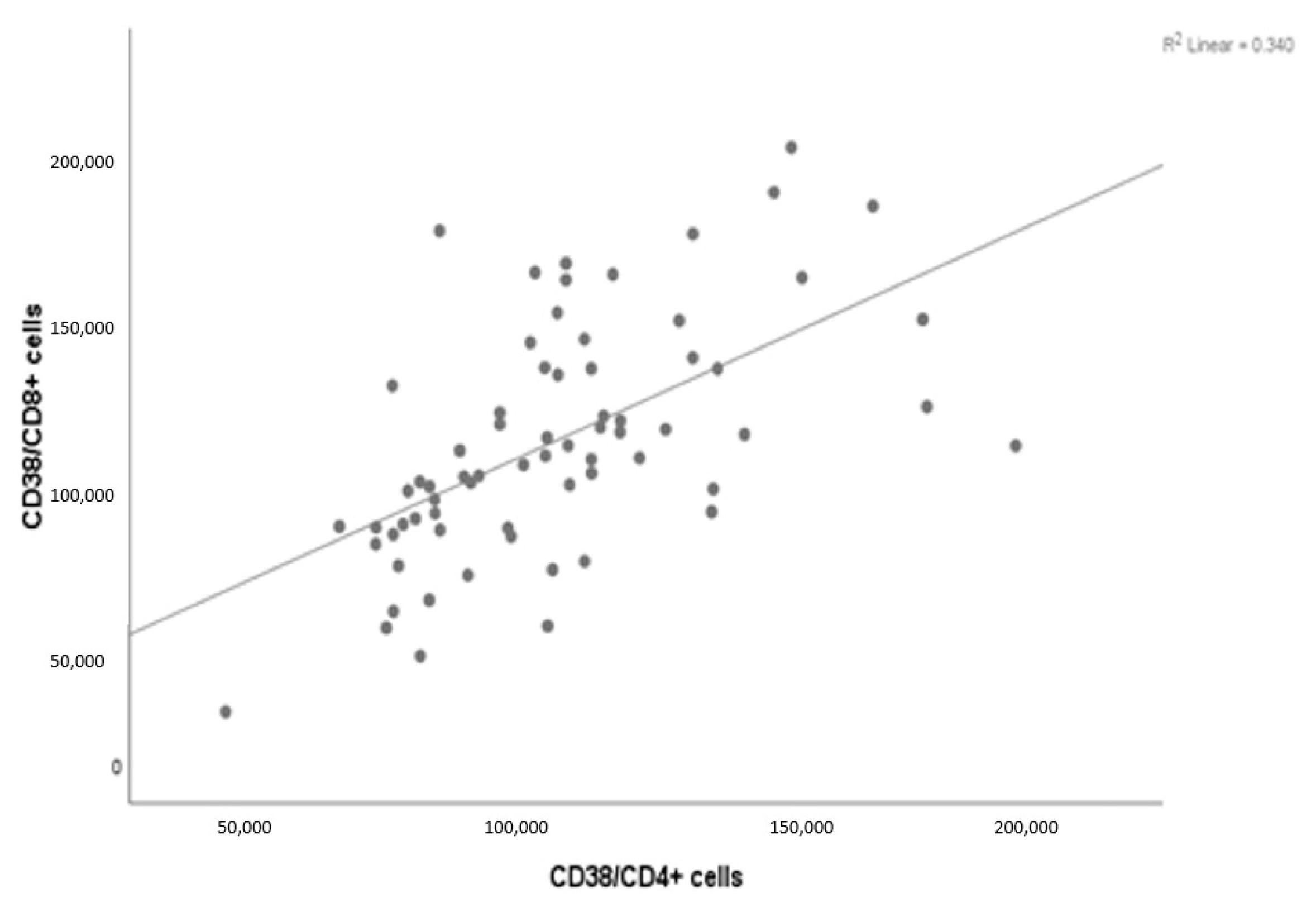
| CD38/CD8+ Cells | ||
|---|---|---|
| CD38/CD4+ cells | r | 0.583 |
| p-value | <0.001 | |
| Sig | S | |
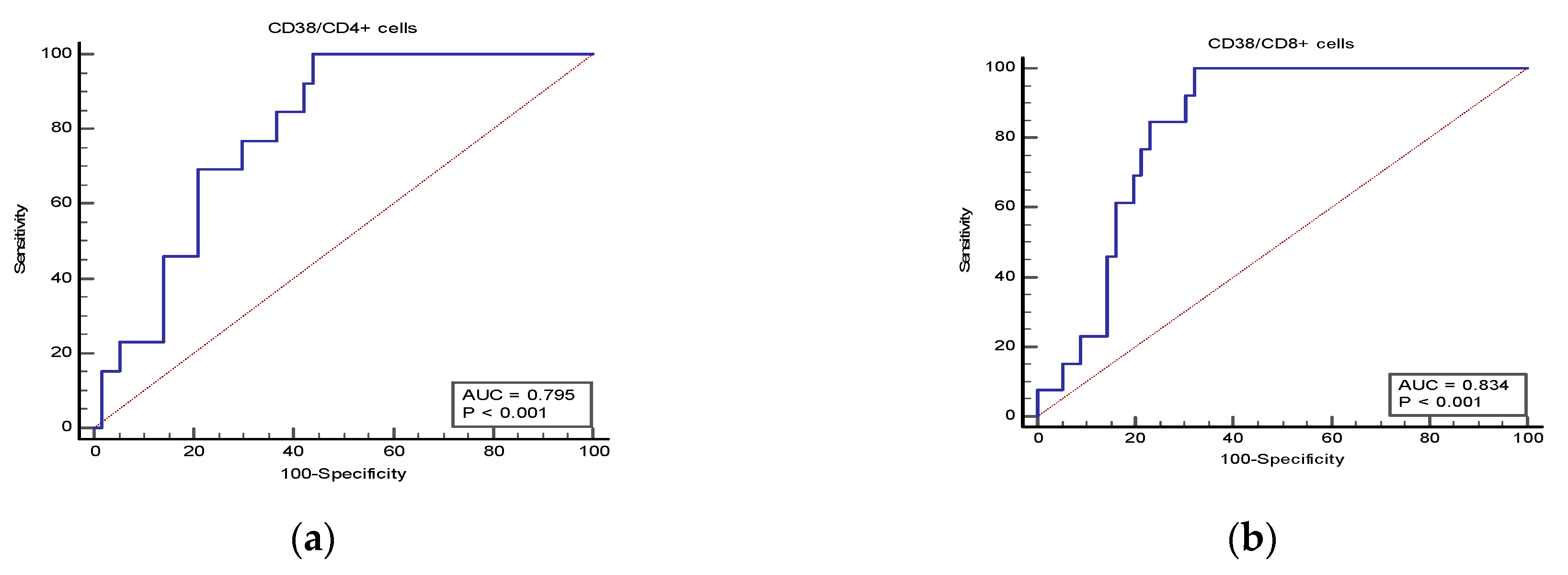
| Variable | AUC | SE | 95% CI |
|---|---|---|---|
| CD38 expression in CD4+ T cells | 0.801 | 0.06 | 0.687 to 0.887 |
| CD38 expression in CD8+ T cells | 0.834 | 0.05 | 0.725 to 0.913 |
| Predictive Value | |||||
|---|---|---|---|---|---|
| Cutoff | Sensitivity % | Specificity % | +PV | −PV | |
| CD38 expression in CD4+ T cells MFI (× 103) | >100.87 | 100 | 56.14 | 34.2 | 100 |
| CD38 expression in CD8+ T cells MFI (× 103) | >91.46 | 100 | 67.86 | 41.9 | 100 |
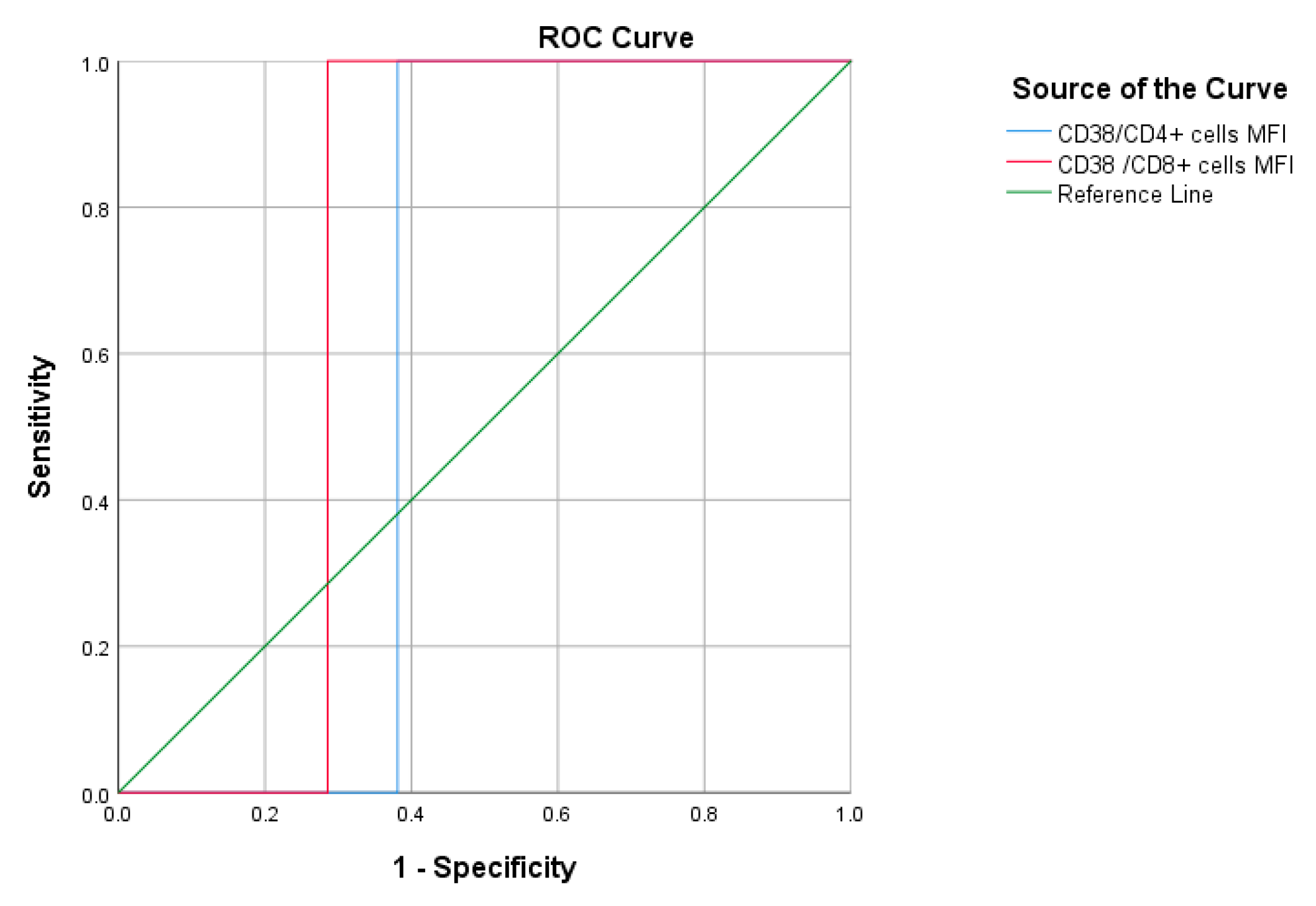
| Area Under the Curve | |||||
|---|---|---|---|---|---|
| Test Result Variable(s) | Area | Std. Error | Asymptotic Sig. * | Asymptotic 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||||
| CD38/CD4+ cells MFI | 0.619 | 0.106 | 0.694 | 0.411 | 0.827 |
| CD38/CD8+ cells MFI | 0.714 | 0.099 | 0.478 | 0.521 | 0.908 |
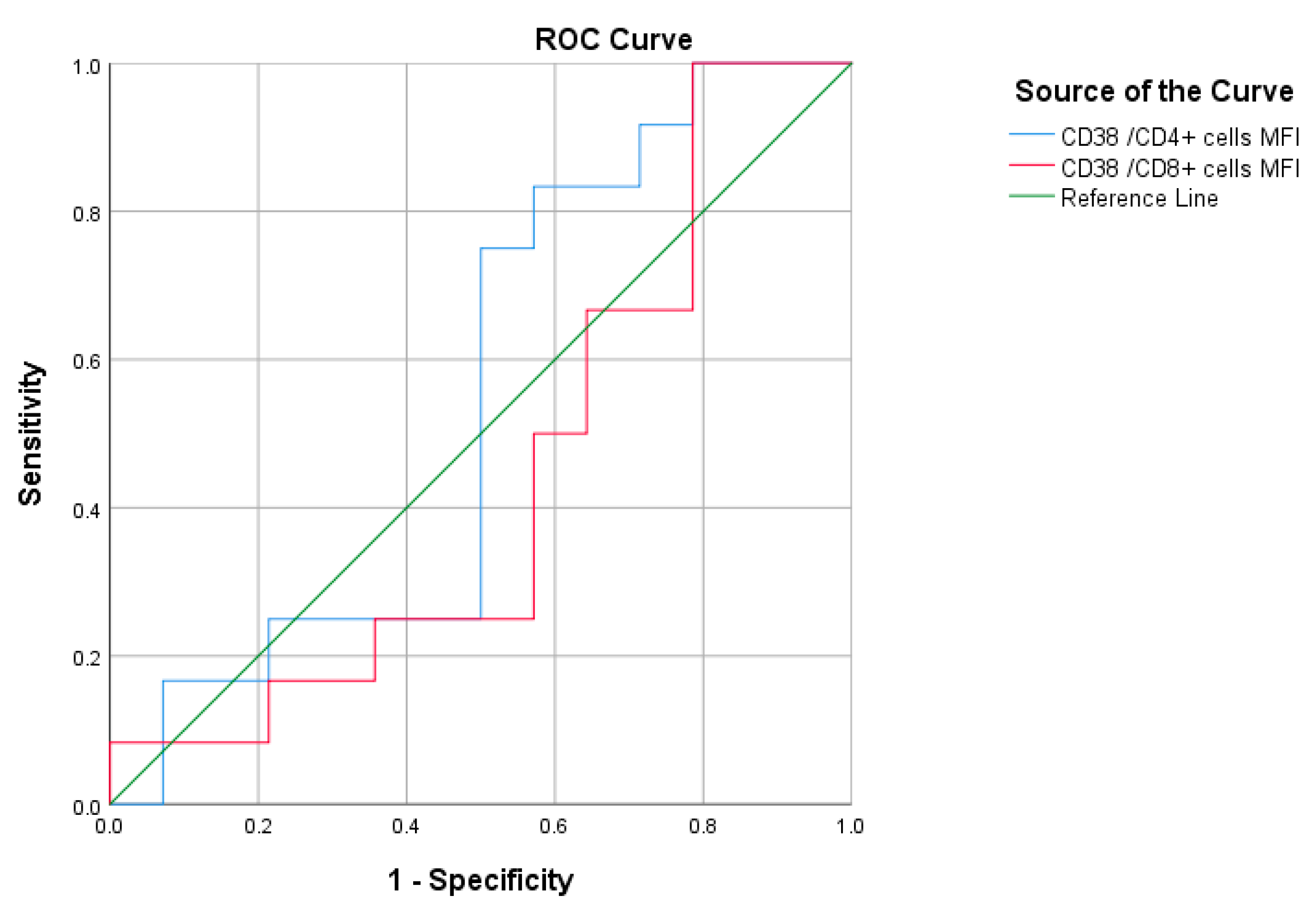
| Area Under the Curve | |||||
|---|---|---|---|---|---|
| Test Result Variable(s) | Area | Std. Error | Asymptotic Sig. * | Asymptotic 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||||
| CD38/CD4+ cells MFI | 0.548 | 0.118 | 0.681 | 0.316 | 0.779 |
| CD38/CD8+ cells MFI | 0.440 | 0.118 | 0.607 | 0.210 | 0.671 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tarbiah, N.I.; Alkhattabi, N.A.; Alsahafi, A.J.; Aljahdali, H.S.; Joharjy, H.M.; Al-Zahrani, M.H.; Sabban, A.M.; Alghamdi, R.A.; Balgoon, M.J.; Khalifa, R.A. T Cells Immunophenotyping and CD38 Overexpression as Hallmarks of the Severity of COVID-19 and Predictors of Patients’ Outcomes. J. Clin. Med. 2023, 12, 710. https://doi.org/10.3390/jcm12020710
Tarbiah NI, Alkhattabi NA, Alsahafi AJ, Aljahdali HS, Joharjy HM, Al-Zahrani MH, Sabban AM, Alghamdi RA, Balgoon MJ, Khalifa RA. T Cells Immunophenotyping and CD38 Overexpression as Hallmarks of the Severity of COVID-19 and Predictors of Patients’ Outcomes. Journal of Clinical Medicine. 2023; 12(2):710. https://doi.org/10.3390/jcm12020710
Chicago/Turabian StyleTarbiah, Nesrin I., Nuha A. Alkhattabi, Abdullah J. Alsahafi, Hani S. Aljahdali, Husam M. Joharjy, Maryam H. Al-Zahrani, Aliaa M. Sabban, Rana A. Alghamdi, Maha J. Balgoon, and Reham A. Khalifa. 2023. "T Cells Immunophenotyping and CD38 Overexpression as Hallmarks of the Severity of COVID-19 and Predictors of Patients’ Outcomes" Journal of Clinical Medicine 12, no. 2: 710. https://doi.org/10.3390/jcm12020710
APA StyleTarbiah, N. I., Alkhattabi, N. A., Alsahafi, A. J., Aljahdali, H. S., Joharjy, H. M., Al-Zahrani, M. H., Sabban, A. M., Alghamdi, R. A., Balgoon, M. J., & Khalifa, R. A. (2023). T Cells Immunophenotyping and CD38 Overexpression as Hallmarks of the Severity of COVID-19 and Predictors of Patients’ Outcomes. Journal of Clinical Medicine, 12(2), 710. https://doi.org/10.3390/jcm12020710









