Clinical Outcomes for Total Hip Arthroplasty with and without Previous Curved Periacetabular Osteotomy
Abstract
1. Introduction
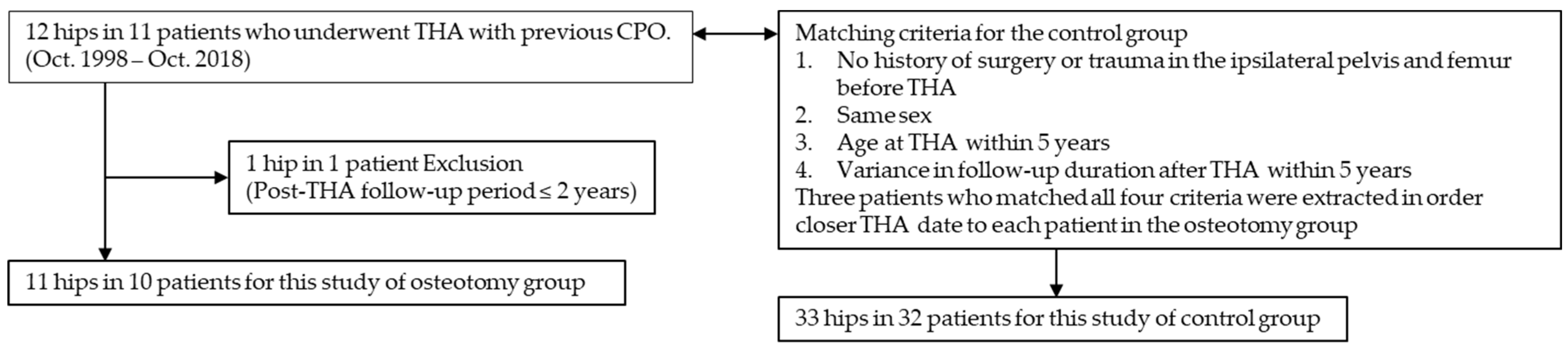
2. Materials and Methods
2.1. Study Design and Patients
2.2. Surgical Technique
2.3. Surgical Data and Clinical Evaluations
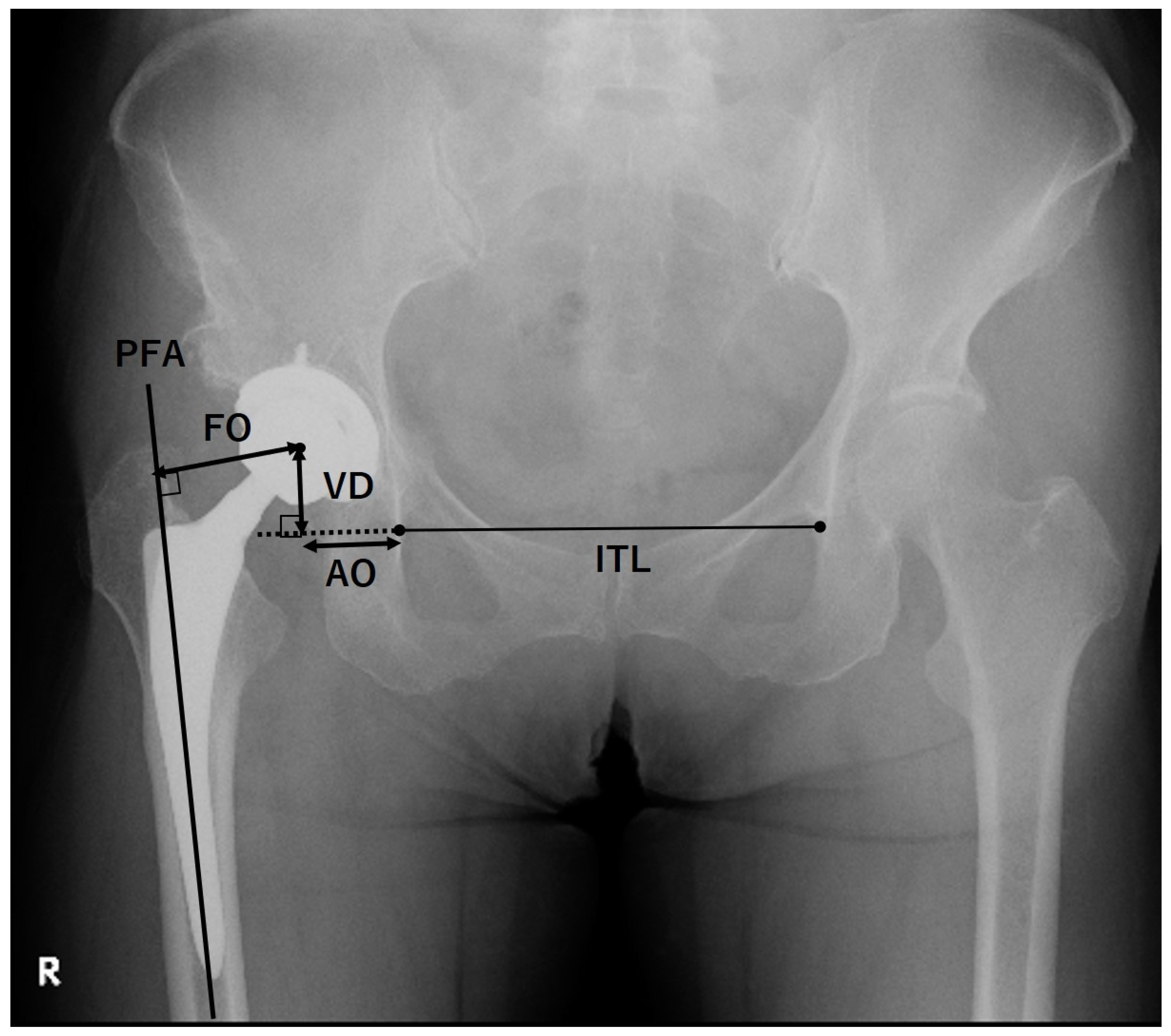
2.4. Radiographic Evaluations
2.5. Statistical Analysis
3. Results
3.1. Patient Demographic Characteristics
3.2. Surgical Data and Clinical Evaluations
3.3. Radiographic Evaluations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aronson, J. Osteoarthritis of the young adult hip: Etiology and treatment. Instr. Course Lect. 1986, 35, 119–128. [Google Scholar]
- Matsuo, A.; Jingushi, S.; Nakashima, Y.; Yamamoto, T.; Mawatari, T.; Noguchi, Y.; Shuto, T.; Iwamotoet, Y. Transposition osteotomy of the acetabulum for advanced-stage osteoarthritis of the hips. J. Orthop. Sci. 2009, 14, 266–273. [Google Scholar] [CrossRef]
- Ninomiya, S.; Tagawa, H. Rotational acetabular osteotomy for the dysplastic hip. J. Bone Joint Surg. Am. 1984, 66, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Ganz, R.; Klaue, K.; Vinh, T.S.; Mast, J.W. A new periacetabular osteotomy for the treatment of hip dysplasias: Technique and preliminary results. Clin. Orthop. Relat. Res. 1998, 232, 26–36. [Google Scholar] [CrossRef]
- Naito, M.; Shiramizu, K.; Akiyoshi, Y.; Ezoe, M.; Nakamura, Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin. Orthop. Relat. Res. 2005, 433, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, Y.; Iwase, T.; Kitamura, S.; Yamauchi, K.; Sakano, S.; Iwata, H. Eccentric rotational acetabular osteotomy for acetabular dysplasia: Follow-up of one hundred and thirty-two hips for five to ten years. J. Bone Joint Surg. Am. 2002, 84, 404–410. [Google Scholar] [CrossRef]
- Fujii, M.; Nakashima, Y.; Noguchi, Y.; Mawatari, T.; Motomura, G.; Iwamoto, Y. Effect of intra-articular lesions on the outcome of periacetabular osteotomy in patients with symptomatic hip dysplasia. J. Bone Joint Surg. Br. 2011, 93, 1449–1456. [Google Scholar] [CrossRef] [PubMed]
- Yasunaga, Y.; Ochi, M.; Yamasaki, T.; Shoji, T.; Izumi, S. Rotational acetabular osteotomy for pre- and early osteoarthritis secondary to dysplasia provides durable results at 20 years. Clin. Orthop. Relat. Res. 2016, 474, 2145–2153. [Google Scholar] [CrossRef]
- Nakamura, S.; Ninomiya, S.; Takatori, Y.; Morimoto, S.; Umeyama, T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10–23 years. Acta Orthop. Scand. 1998, 69, 259–265. [Google Scholar] [CrossRef]
- Kaneuji, A.; Sugimori, T.; Ichiseki, T.; Fukui, K.; Takahashi, E.; Matsumoto, T. Rotational acetabular osteotomy for osteoarthritis with acetabular dysplasia: Conversion rate to total hip arthroplasty within twenty years and osteoarthritis progression after a minimum of twenty years. J. Bone Joint Surg. Am. 2015, 97, 726–732. [Google Scholar] [CrossRef]
- Steppacher, S.D.; Tannast, M.; Ganz, R.; Siebenrock, K.A. Mean 20-year follow up of Bernese periacetabular osteotomy. Clin. Orthop. Relat. Res. 2008, 466, 1633–1644. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.; Millis, M.; Kim, Y.J.; Bulat, E.; Miller, P.; Matheney, T. Survivorship of the Bernese periacetabular osteotomy: What factors are associated with long-term failure? Clin. Orthop. Relat. Res. 2017, 475, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Siebenrock, K.A.; Schöll, E.; Lottenbach, M.; Ganz, R. Bernese periacetabular osteotomy. Clin. Orthop. Relat. Res. 1999, 363, 9–20. [Google Scholar] [CrossRef]
- Teratani, T.; Naito, M.; Kiyama, T.; Maeyama, A. Periacetabular osteotomy in patients fifty years of age or older. J. Bone Joint Surg. Am. 2019, 92, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, T.; Naito, M.; Nakamura, Y. Outcome of peri-acetabular osteotomy for hip dysplasia in teenagers. Int. Orthop. 2015, 39, 2281–2286. [Google Scholar] [CrossRef]
- Karashima, H.; Naito, M.; Shiramizu, K.; Kiyama, T.; Maeyama, A. A periacetabular osteotomy for the treatment of severe dysplastic hips. Clin. Orthop. Relat. Res. 2011, 469, 1436–1441. [Google Scholar] [CrossRef]
- Hasegawa, Y.; Iwase, T.; Kitamura, S.; Kawasaki, M.; Yamaguchi, J. Eccentric rotational acetabular osteotomy for acetabular dysplasia and osteoarthritis: Follow-up at a mean duration of twenty years. J. Bone Joint Surg. Am. 2014, 96, 1975–1982. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Wibowo, D.B.; Kurdi, O.; Tauviqirrahman, M.; Jamari, J. Minimizing risk of failure from ceramic-on-ceramic total hip prosthesis by selecting ceramic materials based on tresca stress. Sustainability 2022, 14, 13413. [Google Scholar] [CrossRef]
- Komiyama, K.; Hamai, S.; Motomura, G.; Ikemura, S.; Fujii, M.; Kawahara, S.; Nakashima, Y. Total hip arthroplasty after periacetabular osteotomy versus primary total hip arthroplasty: A propensity-matched cohort study. Arch. Orthop. Trauma. Surg. 2021, 141, 1411–1417. [Google Scholar] [CrossRef] [PubMed]
- Ito, H.; Takatori, Y.; Moro, T.; Oshima, H.; Oka, H.; Tanaka, S. Total hip arthroplasty after rotational acetabular osteotomy. J. Arthroplast. 2015, 30, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Fukui, K.; Kaneuji, A.; Sugimori, T.; Ichiseki, T.; Matsumoto, T. Does rotational acetabular osteotomy affect subsequent total hip arthroplasty? Arch. Orthop. Trauma. Surg. 2015, 135, 407–415. [Google Scholar] [CrossRef]
- Amanatullah, D.F.; Stryker, L.; Schoenecker, P.; Taunton, M.J.; Clohisy, J.C.; Trousdale, R.T.; Sierra, R.J. Similar clinical outcomes for THAs with and without prior periacetabular osteotomy. Clin. Orthop. Relat. Res. 2015, 473, 685–691. [Google Scholar] [CrossRef]
- Osawa, Y.; Hasegawa, Y.; Seki, T.; Amano, T.; Higuchi, Y.; Ishiguro, N. Significantly poor outcomes of total hip arthroplasty after failed periacetabular osteotomy. J. Arthroplast. 2016, 31, 1904–1909. [Google Scholar] [CrossRef] [PubMed]
- Lecerf, G.; Fessy, M.H.; Philippot, R.; Massin, P.; Giraud, F.; Flecher, X.; Girard, J.; Mertl, P.; Marchetti, E.; Stindel, E. Femoral offset: Anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Biggi, S.; Banci, L.; Tedino, R.; Capuzzo, A.; Cattaneo, G.; Tornago, S.; Camera, A. Restoring global offset and lower limb length with a 3 offset option double-tapered stem. BMC Musculoskelet. Disord. 2020, 21, 646. [Google Scholar] [CrossRef] [PubMed]
- Wiberg, G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir. Scand. 1939, 83, 7–38. [Google Scholar]
- Smith-Petersen, M.N. Approach to and exposure of the hip joint for mold arthroplasty. J. Bone Joint Surg. Am. 1949, 31, 40–46. [Google Scholar] [CrossRef]
- Leunig, M.; Faas, M.; Knoch, F.V.; Naal, F.D. Skin crease ‘bikini’ incision for anterior approach total hip arthroplasty: Surgical technique and preliminary results. Clin. Orthop. Relat. Res. 2013, 471, 2245–2252. [Google Scholar] [CrossRef] [PubMed]
- Leunig, M.; Siebenrock, K.A.; Ganz, R. Rationale of periacetabular osteotomy and background work. Instr. Course Lect. 2001, 50, 229–238. [Google Scholar] [CrossRef]
- Moore, A.T. The self-locking metal hip prothesis. J. Bone Joint Surg. Am. 1957, 39, 811–827. [Google Scholar] [CrossRef] [PubMed]
- Hardinge, K. The direct lateral approach to the hip. J. Bone Joint Surg. Br. 1982, 64, 17–19. [Google Scholar] [CrossRef] [PubMed]
- Oinuma, K.; Eingartner, C.; Saito, Y.; Shiratsuchi, H. Total hip arthroplasty by a minimally invasive, direct anterior approach. Oper. Orthop. Traumatol. 2007, 19, 310–326. [Google Scholar] [CrossRef]
- Watson-Jones, R. Fracture of the neck of the femur. Br. J. Surg. 1936, 23, 787–808. [Google Scholar] [CrossRef]
- Gross, J.B. Estimating allowable blood loss: Corrected for dilution. Anesthesiology 1983, 58, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Joint Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef]
- Kiyama, T.; Naito, M.; Shitama, H.; Maeyama, A. Effect of superior placement of the hip center on abductor muscle strength in total hip arthroplasty. J. Arthroplast. 2009, 24, 240–245. [Google Scholar] [CrossRef]
- Crowe, J.F.; Mani, V.J.; Ranawat, C.S. Total hip replacement in congenital dislocation and dysplasia of the hip. J. Bone Joint Surg. Am. 1979, 61, 15–23. [Google Scholar] [CrossRef] [PubMed]
- McPherson, E.J.; Dorr, L.D.; Gruen, T.A.; Saberi, M.T. Hydroxyapatite-coated proximal ingrowth femoral stem. A matched pair control study. Clin. Orthop. Relat. Res. 1995, 315, 223–230. [Google Scholar]
- Engh, C.A.; Bobyn, J.D.; Glassman, A.H. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J. Bone Joint Surg. Br. 1987, 69, 45–55. [Google Scholar] [CrossRef]
- Tanaka, H.; Yamada, N.; Kurishima, H.; Mori, Y.; Aizawa, T. Association between Hip Center Position and Isokinetic Hip Muscle Performance after Anterolateral Muscle-Sparing Total Hip Arthroplasty. Medicina 2022, 58, 538. [Google Scholar] [CrossRef]
- Baqué, F.; Brown, A.; Matta, J. Total hip arthroplasty after periacetabular osteotomy. Orthopedics 2009, 32, 399. [Google Scholar] [PubMed]
- Peters, C.L.; Beck, M.; Dunn, H.K. Total hip arthroplasty in young adults after failed triple innominate osteotomy. J. Arthroplast. 2001, 16, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Hartig, A.C.; Stilling, M.; Søballe, K.; Thillemann, T.M.; Troelsen, A. Is cup positioning challenged in hips previously treated with periacetabular osteotomy? J. Arthroplast. 2014, 29, 763–768. [Google Scholar] [CrossRef]
- Parvizi, J.; Burmeister, H.; Ganz, R. Previous Bernese periacetabular osteotomy does not compromise the results of total hip arthroplasty. Clin. Orthop. Relat. Res. 2004, 423, 118–122. [Google Scholar] [CrossRef] [PubMed]
| Osteotomy Group | Control Group | ||
|---|---|---|---|
| (n = 11) | (n = 33) | p | |
| Operative time (min) | 113.5 ± 39.0 (50–180) | 101.2 ± 31.8 (56–175) | 0.32 |
| Perioperative blood loss (mL) | 912.1 ± 407.2 (225–1503) | 828.5 ± 376.9 (27–175) | 0.46 |
| Resection of osteophyte | 5 (45.5) | 5 (15.2) | 0.038 * |
| Approaches | 0.54 | ||
| Posterolateral | 7 (63.6) | 16 (48.5) | |
| Direct lateral | 0 | 4 (12.1) | |
| Direct anterior | 2 (18.2) | 7 (21.2) | |
| Anterolateral supine | 2 (18.2) | 6 (18.2) | |
| Cup size | 49.6 ± 1.5 (48–52) | 49.4 ± 2.0 (46–54) | 0.75 |
| Acetabular components | |||
| Natural hip system †† | 1 | 0 | |
| RingLock Acetabular System †† | 1 | 4 | |
| Trilogy †† | 6 | 8 | |
| Mallory Head †† | 0 | 2 | |
| G7 †† | 0 | 1 | |
| Plasmacup † | 1 | 1 | |
| Triad HA ‡ | 0 | 2 | |
| Tritanium ‡ | 0 | 2 | |
| PINNACLE § | 0 | 1 | |
| SQRUM TT shell || | 2 | 6 | |
| Escalade ¶ | 0 | 1 | |
| Nakashima # | 0 | 5 | |
| Femoral components | |||
| Multilock †† | 0 | 1 | |
| Natural hip system †† | 1 | 0 | |
| VerSys HA †† | 2 | 3 | |
| Kinectiv †† | 2 | 1 | |
| TaperLock Microplasty †† | 1 | 5 | |
| Bi-Metric †† | 0 | 2 | |
| Mayo conservative †† | 0 | 1 | |
| Excia † | 1 | 1 | |
| Centpillar TMZF ‡ | 0 | 2 | |
| Accolade II ‡ | 0 | 2 | |
| S-ROM § | 0 | 1 | |
| Initia || | 2 | 3 | |
| 910 PerFix HA || | 0 | 3 | |
| OVATION Tribute ¶ | 0 | 1 | |
| FS # | 2 | 7 |
| Osteotomy Group | Control Group | p | |
|---|---|---|---|
| Number of hips | 11 | 33 | |
| Number of patients | 10 | 32 | |
| Male-to-female ratio | 0:10 | 0:32 | 1.00 |
| Age at THA (years) | 51.9 ± 7.2 (34–59) | 52.8 ± 6.8 (36–63) | 0.73 |
| BMI (kg/m2) | 24.0 ± 6.0 (17.1–34.8) | 24.2 ± 3.9 (18.1–34.4) | 0.46 |
| Crowe classification | 0.23 | ||
| I | 11 | 29 | |
| II | 0 | 4 | |
| Pre-THA diagnosis | 0.17 | ||
| OA | 11 | 28 | |
| ONFH | 0 | 11 | |
| Interval between CPO and THA | 8.8 ± 4.4 (1.4–14.0) | N/A | |
| Duration of follow-up after THA (years) | 8.6 ± 5.4 (3.0–17.6) | 8.1 ± 4.6 (2.6–21.4) | 0.81 |
| Osteotomy Group | Control Group | ||
|---|---|---|---|
| (n = 11) | (n = 33) | p | |
| Preoperative HHS | 47.5 ± 12.2 (33–66) | 60.9 ± 12.6 (31–81) | 0.0072 * |
| Postoperative HHS | 94.9 ± 3.8 (86–99) | 92.7 ± 12.2 (32–100) | 0.99 |
| Complications | |||
| Dislocation | 0 | 0 | 1.00 |
| Infection | 0 | 0 | 1.00 |
| VTE | 0 | 0 | 1.00 |
| Nerve palsy | 0 | 1 (3.0) | 0.56 |
| Revision surgery | 0 | 1 (3.0) | 0.56 |
| Osteotomy Group | Control Group | ||
|---|---|---|---|
| (n = 11) | (n = 33) | p | |
| McPherson’s criteria | 0.40 | ||
| Grade IA | 10 (90.9) | 32 (97.0) | |
| Grade IB | 1 (9.1) | 1 (3.0) | |
| Engh’s criteria | 0.56 | ||
| Fixation by bone ingrowth | 11 (100) | 32 (97.0) | |
| Unstable implant | 0 (0) | 1 (3.0) | |
| Cup inclination (°) | 37.6 ± 8.6 (26.8–56.2) | 41.4 ± 7.1 (31.9–62.5) | 0.11 |
| Cup anteversion (°) | 21.3 ± 8.3 (4.5–34.8) | 21.2 ± 8.3 (5.6–35.2) | 0.99 |
| Vertical distance (mm) | 27.5 ± 4.6 (22.7–34.9) | 24.3 ± 4.3 (16.8–36.5) | 0.16 |
| Acetabular offset (mm) | 35.6 ± 2.8 (29.6–38.5) | 34.0 ± 5.2 (21.3–43.5) | 0.22 |
| Femoral offset (mm) | 34.5 ± 5.3 (26.2–43.9) | 37.4 ± 6.6 (23.9–56.3) | 0.27 |
| Global offset (mm) | 70.1 ± 7.2 (57.7–81.4) | 71.4 ± 7.6 (56.4–86.0) | 0.67 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kinoshita, K.; Seo, H.; Matsunaga, T.; Doi, K.; Yamamoto, T. Clinical Outcomes for Total Hip Arthroplasty with and without Previous Curved Periacetabular Osteotomy. J. Clin. Med. 2023, 12, 694. https://doi.org/10.3390/jcm12020694
Kinoshita K, Seo H, Matsunaga T, Doi K, Yamamoto T. Clinical Outcomes for Total Hip Arthroplasty with and without Previous Curved Periacetabular Osteotomy. Journal of Clinical Medicine. 2023; 12(2):694. https://doi.org/10.3390/jcm12020694
Chicago/Turabian StyleKinoshita, Koichi, Hajime Seo, Taiki Matsunaga, Kenichiro Doi, and Takuaki Yamamoto. 2023. "Clinical Outcomes for Total Hip Arthroplasty with and without Previous Curved Periacetabular Osteotomy" Journal of Clinical Medicine 12, no. 2: 694. https://doi.org/10.3390/jcm12020694
APA StyleKinoshita, K., Seo, H., Matsunaga, T., Doi, K., & Yamamoto, T. (2023). Clinical Outcomes for Total Hip Arthroplasty with and without Previous Curved Periacetabular Osteotomy. Journal of Clinical Medicine, 12(2), 694. https://doi.org/10.3390/jcm12020694





