How Epinephrine Administration Interval Impacts the Outcomes of Resuscitation during Adult Cardiac Arrest: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
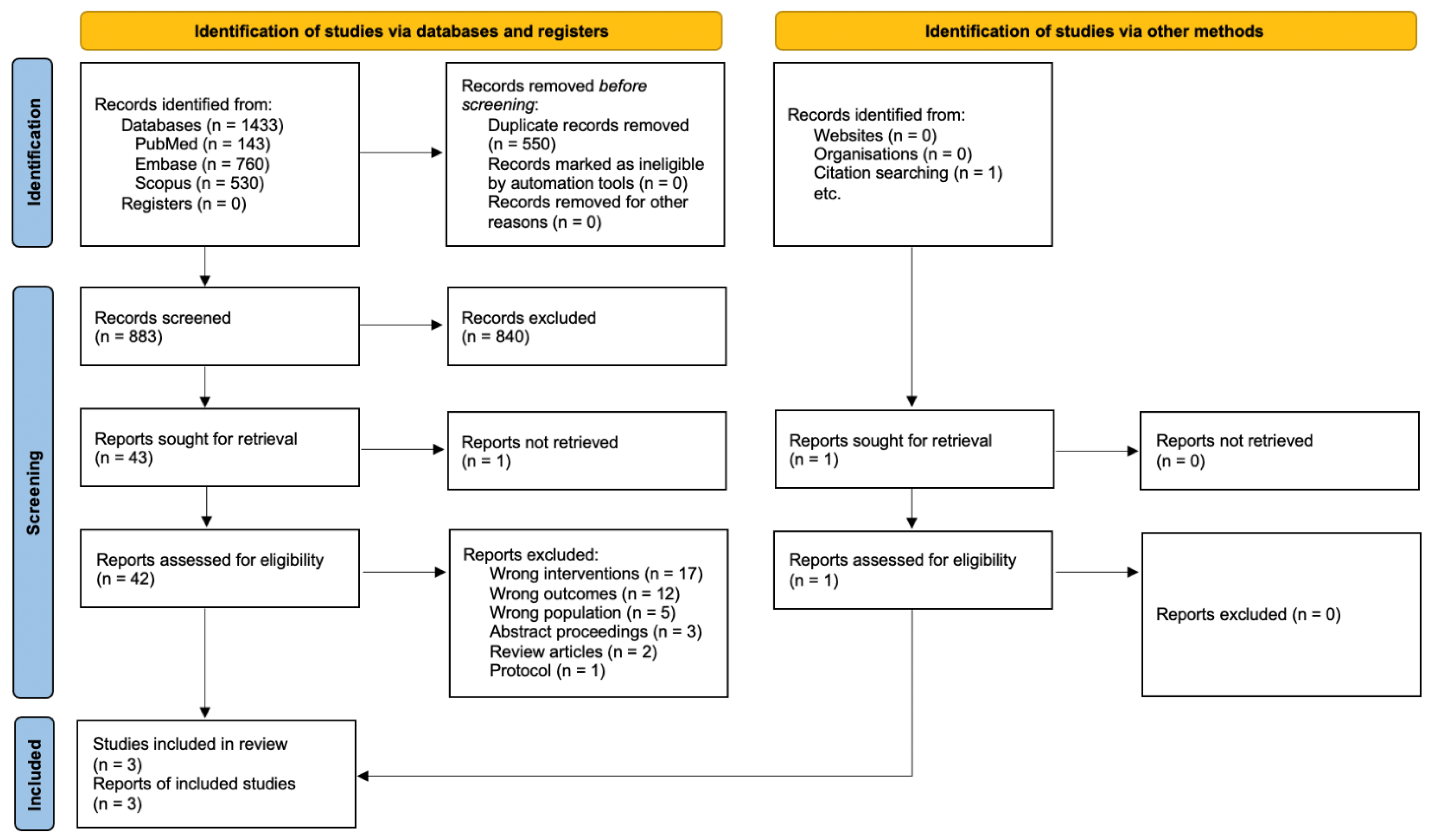
2.1. Search Strategy and Study Selection
2.2. Inclusion Criteria and Outcome of Interest
- Any study including adults 18 years of age and older who received CPR.
- At least one arm reported EAI during CPA of 3–5 min.
- Comparing EAIs other than 3–5 min (higher or lower intervals).
- Reporting of an outcome on neurological status at hospital discharge.
2.3. Data Extraction and Assessment of the Study Risk of Bias
2.4. Data Synthesis and Statistical Analysis
3. Results
3.1. Characteristics and Quality of the Included Studies
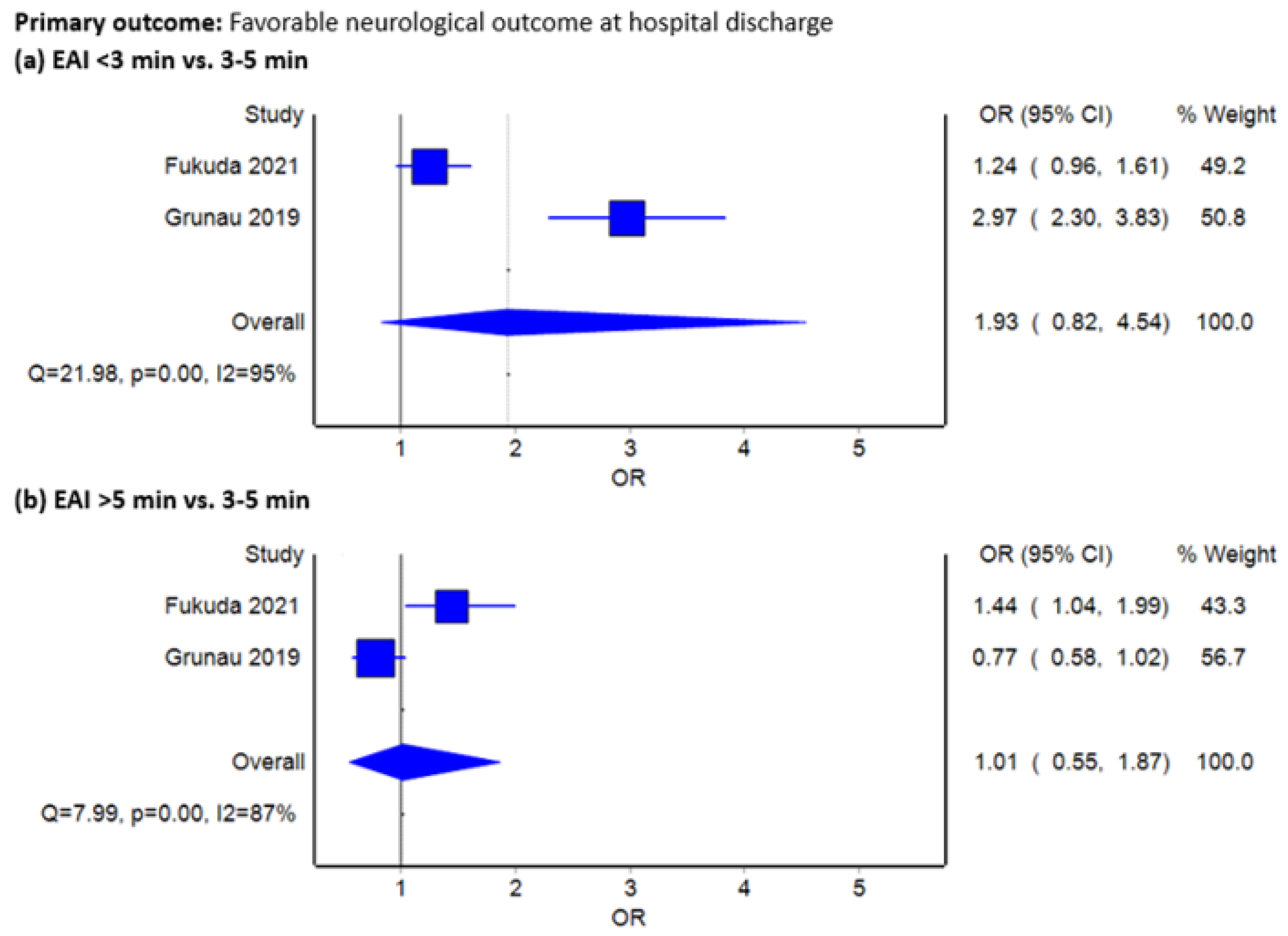
3.2. Favorable Neurological Outcome at Hospital Discharge
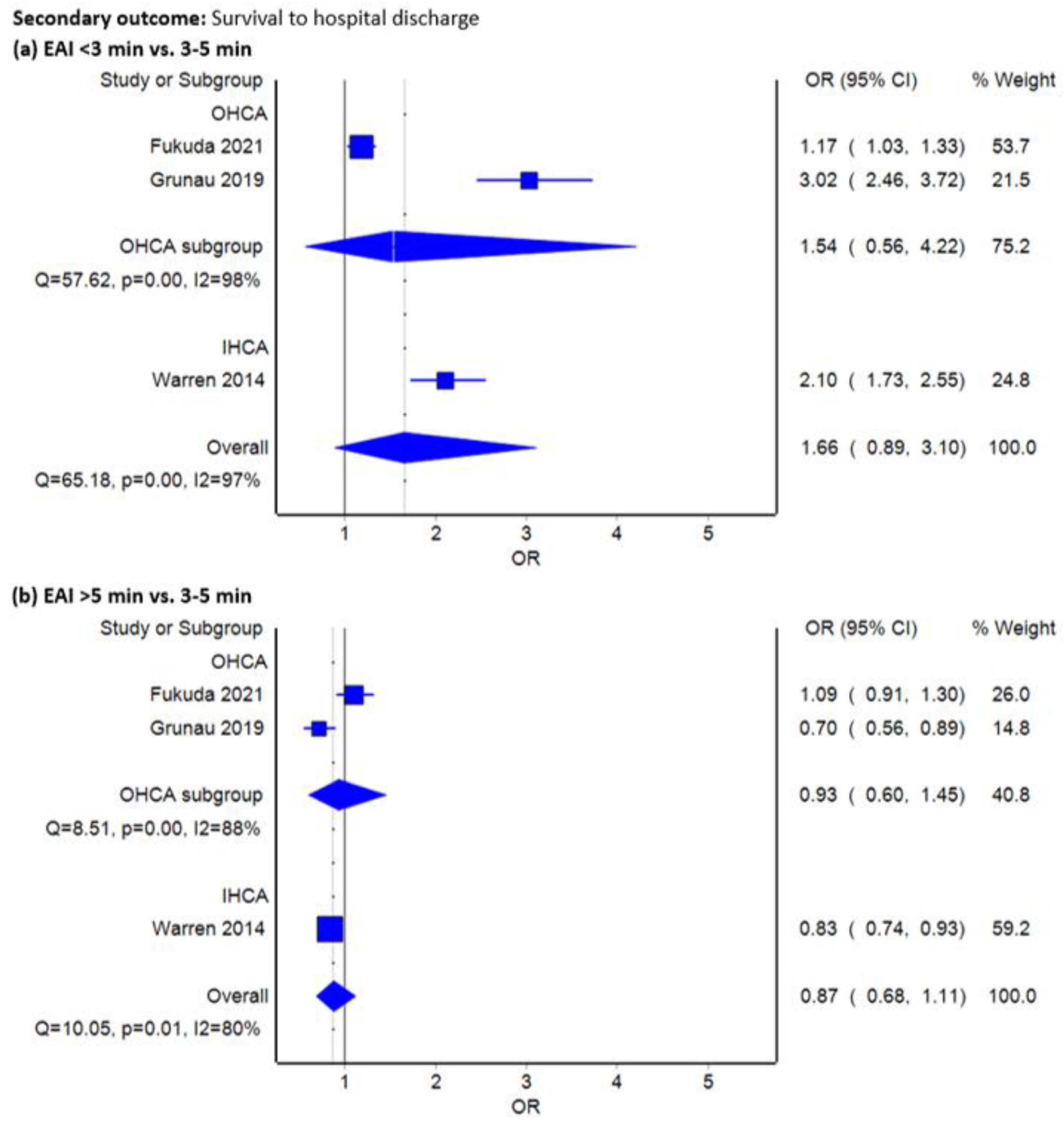
3.3. Survival to Hospital Discharge
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2021 Update: A Report From the American Heart Association. Circulation 2021, 143, E254–E743. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Gan, Y.; Jiang, N.; Wang, R.; Chen, Y.; Luo, Z.; Zong, Q.; Chen, S.; Lv, C. The Global Survival Rate among Adult Out-of-Hospital Cardiac Arrest Patients Who Received Cardiopulmonary Resuscitation: A Systematic Review and Meta-Analysis. Crit. Care 2020, 24, 61. [Google Scholar] [CrossRef] [PubMed]
- Wongtanasarasin, W.; Ungrungseesopon, N.; Namsongwong, N.; Chotipongkul, P.; Visavakul, O.; Banping, N.; Kampeera, W.; Phinyo, P. Association between Calcium Administration and Outcomes during Adult Cardiopulmonary Resuscitation at the Emergency Department. Turk. J. Emerg. Med. 2022, 22, 67. [Google Scholar] [CrossRef] [PubMed]
- Kienzle, M.F.; Morgan, R.W.; Faerber, J.A.; Graham, K.; Katcoff, H.; Landis, W.P.; Topjian, A.A.; Kilbaugh, T.J.; Nadkarni, V.M.; Berg, R.A.; et al. The Effect of Epinephrine Dosing Intervals on Outcomes from Pediatric In-Hospital Cardiac Arrest. Am. J. Respir. Crit. Care Med. 2021, 204, 977–985. [Google Scholar] [CrossRef]
- Perkins, G.D.; Kenna, C.; Ji, C.; Deakin, C.D.; Nolan, J.P.; Quinn, T.; Fothergill, R.; Gunson, I.; Pocock, H.; Rees, N.; et al. The Effects of Adrenaline in out of Hospital Cardiac Arrest with Shockable and Non-Shockable Rhythms: Findings from the PACA and PARAMEDIC-2 Randomised Controlled Trials. Resuscitation 2019, 140, 55–63. [Google Scholar] [CrossRef]
- Perkins, G.D.; Ji, C.; Deakin, C.D.; Quinn, T.; Nolan, J.P.; Scomparin, C.; Regan, S.; Long, J.; Slowther, A.; Pocock, H.; et al. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2018, 379, 711–721. [Google Scholar] [CrossRef]
- Berg, R.A.; Sutton, R.M.; Reeder, R.W.; Berger, J.T.; Newth, C.J.; Carcillo, J.A.; McQuillen, P.S.; Meert, K.L.; Yates, A.R.; Harrison, R.E.; et al. Association between Diastolic Blood Pressure during Pediatric In-Hospital Cardiopulmonary Resuscitation and Survival. Circulation 2018, 137, 1784–1795. [Google Scholar] [CrossRef]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef]
- Warren, S.A.; Huszti, E.; Bradley, S.M.; Chan, P.S.; Bryson, C.L.; Fitzpatrick, A.L.; Nichol, G. Adrenaline (Epinephrine) Dosing Period and Survival after in-Hospital Cardiac Arrest: A Retrospective Review of Prospectively Collected Data. Resuscitation 2014, 85, 350–358. [Google Scholar] [CrossRef]
- Hoyme, D.B.; Patel, S.S.; Samson, R.A.; Raymond, T.T.; Nadkarni, V.M.; Gaies, M.G.; Atkins, D.L. Epinephrine Dosing Interval and Survival Outcomes during Pediatric In-Hospital Cardiac Arrest. Resuscitation 2017, 117, 18–23. [Google Scholar] [CrossRef]
- Wongtanasarasin, W.; Thepchinda, T.; Kasirawat, C.; Saetiao, S.; Leungvorawat, J.; Kittivorakanchai, N. Treatment Outcomes of Epinephrine for Traumatic Out-of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. J. Emerg. Trauma Shock 2021, 14, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.H.; Huang, C.H.; Chang, W.T.; Tsai, M.S.; Yu, P.H.; Wu, Y.W.; Hung, K.Y.; Chen, W.J. The Influences of Adrenaline Dosing Frequency and Dosage on Outcomes of Adult In-Hospital Cardiac Arrest: A Retrospective Cohort Study. Resuscitation 2016, 103, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Grunau, B.; Kawano, T.; Scheuermeyer, F.X.; Drennan, I.; Fordyce, C.B.; van Diepen, S.; Reynolds, J.; Lin, S.; Christenson, J. The Association of the Average Epinephrine Dosing Interval and Survival With Favorable Neurologic Status at Hospital Discharge in Out-of-Hospital Cardiac Arrest. Ann. Emerg. Med. 2019, 74, 797–806. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef] [PubMed]
- Ka-Lok Lo, C.; Mertz, D.; Loeb, M. Newcastle-Ottawa Scale: Comparing Reviewers’ to Authors’ Assessments. BMC Med. Res. Methodol. 2014, 14, 45. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Doi, S.A.R.; Barendregt, J.J.; Khan, S.; Thalib, L.; Williams, G.M. Advances in the Meta-Analysis of Heterogeneous Clinical Trials I: The Inverse Variance Heterogeneity Model. Contemp. Clin. Trials 2015, 45, 130–138. [Google Scholar] [CrossRef]
- Fletcher, J. What Is Heterogeneity and Is It Important? BMJ 2007, 334, 94–96. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- EpiGear International MetaXL 2016. Available online: https://www.epigear.com/index_files/metaxl.html (accessed on 20 December 2022).
- Fukuda, T.; Kaneshima, H.; Matsudaira, A.; Chinen, T.; Sekiguchi, H.; Ohashi-Fukuda, N.; Inokuchi, R.; Kukita, I. Epinephrine Dosing Interval and Neurological Outcome in Out-of-Hospital Cardiac Arrest. Perfusion 2021, 37, 835–846. [Google Scholar] [CrossRef]
- Hilwig, R.W.; Berg, R.A.; Kern, K.B.; Ewy, G.A. Endothelin-1 Vasoconstriction During Swine Cardiopulmonary Resuscitation Improves Coronary Perfusion Pressures but Worsens Postresuscitation Outcome. Circulation 2000, 101, 2097–2102. [Google Scholar] [CrossRef] [PubMed]
- Larabee, T.M.; Liu, K.Y.; Campbell, J.A.; Little, C.M. Vasopressors in Cardiac Arrest: A Systematic Review. Resuscitation 2012, 83, 932–939. [Google Scholar] [CrossRef]
- Al-Mulhim, M.A.; Alshahrani, M.S.; Asonto, L.P.; Abdulhady, A.; Almutairi, T.M.; Hajji, M.; Alrubaish, M.A.; Almulhim, K.N.; Al-Sulaiman, M.H.; Al-Qahtani, L.B. Impact of Epinephrine Administration Frequency in Out-of-Hospital Cardiac Arrest Patients: A Retrospective Analysis in a Tertiary Hospital Setting. J. Int. Med. Res. 2019, 47, 4272–4283. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Yu, J.; Pan, Q.; Lu, Y.; Li, L.; Cao, H.; Gonzalez-Muñoz, M.; Justen Kilbaugh, T. Impact of Total Epinephrine Dose on Long Term Neurological Outcome for Cardiac Arrest Patients: A Cohort Study. Front. Pharmacol. 2021, 12, 580234. [Google Scholar] [CrossRef] [PubMed]
- Putzer, G.; Martini, J.; Spraider, P.; Hornung, R.; Pinggera, D.; Abram, J.; Altaner, N.; Hell, T.; Glodny, B.; Helbok, R.; et al. Effects of Different Adrenaline Doses on Cerebral Oxygenation and Cerebral Metabolism during Cardiopulmonary Resuscitation in Pigs. Resuscitation 2020, 156, 223–229. [Google Scholar] [CrossRef]
- Madsen Hardig, B.; Götberg, M.; Rundgren, M.; Götberg, M.; Zughaft, D.; Kopotic, R.; Wagner, H. Physiologic Effect of Repeated Adrenaline (Epinephrine) Doses during Cardiopulmonary Resuscitation in the Cath Lab Setting: A Randomised Porcine Study. Resuscitation 2016, 101, 77–83. [Google Scholar] [CrossRef]
- Redding, J.S.; Pearson, J.W. Resuscitation From Ventricular Fibrillation Drug Therapy. JAMA 1968, 203, 255–260. [Google Scholar] [CrossRef]
- Sutton, R.M.; Friess, S.H.; Bhalala, U.; Maltese, M.R.; Naim, M.Y.; Bratinov, G.; Niles, D.; Nadkarni, V.M.; Becker, L.B.; Berg, R.A. Hemodynamic Directed CPR Improves Short-Term Survival from Asphyxia-Associated Cardiac Arrest. Resuscitation 2013, 84, 696–701. [Google Scholar] [CrossRef]
- Sutton, R.M.; Friess, S.H.; Naim, M.Y.; Lampe, J.W.; Bratinov, G.; Weiland, T.R.; Garuccio, M.; Nadkarni, V.M.; Becker, L.B.; Berg, R.A. Patient-Centric Blood Pressure-Targeted Cardiopulmonary Resuscitation Improves Survival from Cardiac Arrest. Am. J. Respir. Crit. Care Med. 2014, 190, 1255–1262. [Google Scholar] [CrossRef]
- Friess, S.H.; Sutton, R.M.; Bhalala, U.; Maltese, M.R.; Naim, M.Y.; Bratinov, G.; Weiland, T.R.; Garuccio, M.; Nadkarni, V.M.; Becker, L.B.; et al. Hemodynamic Directed Cardiopulmonary Resuscitation Improves Short-Term Survival from Ventricular Fibrillation Cardiac Arrest. Crit. Care Med. 2013, 41, 2698–2704. [Google Scholar] [CrossRef]
- Thompson, S.G.; Higgins, J.P.T. How Should Meta-Regression Analyses Be Undertaken and Interpreted? Stat. Med. 2002, 21, 1559–1573. [Google Scholar] [CrossRef] [PubMed]
| Study (Publication Year) | Type of Study, Study Location, Enrollment Period | Participants (Total Enrolled; Mean Age ± SD) | Epinephrine Administration Interval | Number of Patients | Male, % | Age, Years (Mean ± SD) | Shockable Rhythm, % | Witnessed Arrest, % | Bystander CPR, % | Presumed Cardiac Cause, % |
|---|---|---|---|---|---|---|---|---|---|---|
| Fukuda et al. (2021) [21] | Retrospective observational study, Japan, 2011–2017 | Adult OHCAs (n = 10,965), 75.8 ± 14.3 | <3 min | 3446 | 2165, 62.8 | 73.0 ± 15.1 | 551, 16.0 | 2312, 67.1 | 1877, 54.5 | 1939, 56.3 |
| 3–5 min | 5995 | 3518, 58.7 | 77.2 ± 13.6 | 615, 10.2 | 4024, 67.1 | 3162, 52.7 | 3403, 56.8 | |||
| >5 min | 1524 | 879, 57.7 | 76.3 ± 14.5 | 205, 13.5 | 1054, 69.2 | 866, 56.8 | 853, 56.0 | |||
| Grunau et al. (2019) [13] | Retrospective observational study, USA and Canada, 2011–2015 | Adult OHCAs (n = 15,909), 68 (56–80) a | <3 min | 2059 | 1287, 62.5 | 68 (56–81) a | 413, 20.1 | 805, 40.2 | 960, 47.3 | N/A |
| 3–5 min | 8599 | 5604, 65.2 | 68 (56–80) a | 1527, 17.8 | 3184, 37.0 | 3998, 46.5 | N/A | |||
| >5 min | 5251 | 3397, 64.7 | 67 (55–79) a | 1062, 20.2 | 2074, 40.3 | 2226, 42.9 | N/A | |||
| Warren et al. (2014) [9] | Retrospective observational study, USA, 2000–2009 | Adult IHCAs (n = 20,909), 68 ± 16 | <3 min | 1100 | 674, 61.3 | 67.0 ± 16.1 | 152, 13.8 | 779, 70.8 | N/A | N/A |
| 3–5 min | 6093 | 3720, 61.1 | 67.6 ± 15.9 | 709, 11.6 | 4042, 66.3 | N/A | N/A | |||
| >5 min | 13,716 | 8304, 60.5 | 67.5 ± 15.8 | 1744, 12.7 | 9021, 65.8 | N/A | N/A |
| Study | Selection | Comparability † | Outcome | Total Score (Out of 9) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of Exposed Cohort (Maximum: ✩) | Selection of Non-Exposed Cohort (Maximum: ✩) | Ascertainment of Exposure (Maximum: ✩) | Demonstration That Outcome of Interest Was Not Present at Start of Study (Maximum: ✩) | Comparability of Cohorts Based on the Design or Analysis (Maximum: ✩✩) | Assessment of Outcome (Maximum: ✩) | Follow-Up Length (Maximum: ✩) | Loss to Follow-Up Rate (Maximum: ✩) | ||
| Fukuda et al., 2021 [14] | ✩✩ | ✩ | ✩ | ✩ | ✩✩ | ✩ | ✩ | ✩ | 9 |
| Grunau et al., 2019 [13] | ✩ | ✩ | ✩ | ✩ | ✩✩ | ✩ | ✩ | ✩ | 9 |
| Warren et al., 2014 [9] | ✩ | ✩ | ✩ | ✩ | ✩✩ | ✩ | ✩ | ✩ | 9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wongtanasarasin, W.; Srisurapanont, K.; Nishijima, D.K. How Epinephrine Administration Interval Impacts the Outcomes of Resuscitation during Adult Cardiac Arrest: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 481. https://doi.org/10.3390/jcm12020481
Wongtanasarasin W, Srisurapanont K, Nishijima DK. How Epinephrine Administration Interval Impacts the Outcomes of Resuscitation during Adult Cardiac Arrest: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(2):481. https://doi.org/10.3390/jcm12020481
Chicago/Turabian StyleWongtanasarasin, Wachira, Karan Srisurapanont, and Daniel K. Nishijima. 2023. "How Epinephrine Administration Interval Impacts the Outcomes of Resuscitation during Adult Cardiac Arrest: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 2: 481. https://doi.org/10.3390/jcm12020481
APA StyleWongtanasarasin, W., Srisurapanont, K., & Nishijima, D. K. (2023). How Epinephrine Administration Interval Impacts the Outcomes of Resuscitation during Adult Cardiac Arrest: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(2), 481. https://doi.org/10.3390/jcm12020481






