Endometriosis as an Uncommon Cause of Intestinal Obstruction—A Comprehensive Literature Review
Abstract
1. Introduction
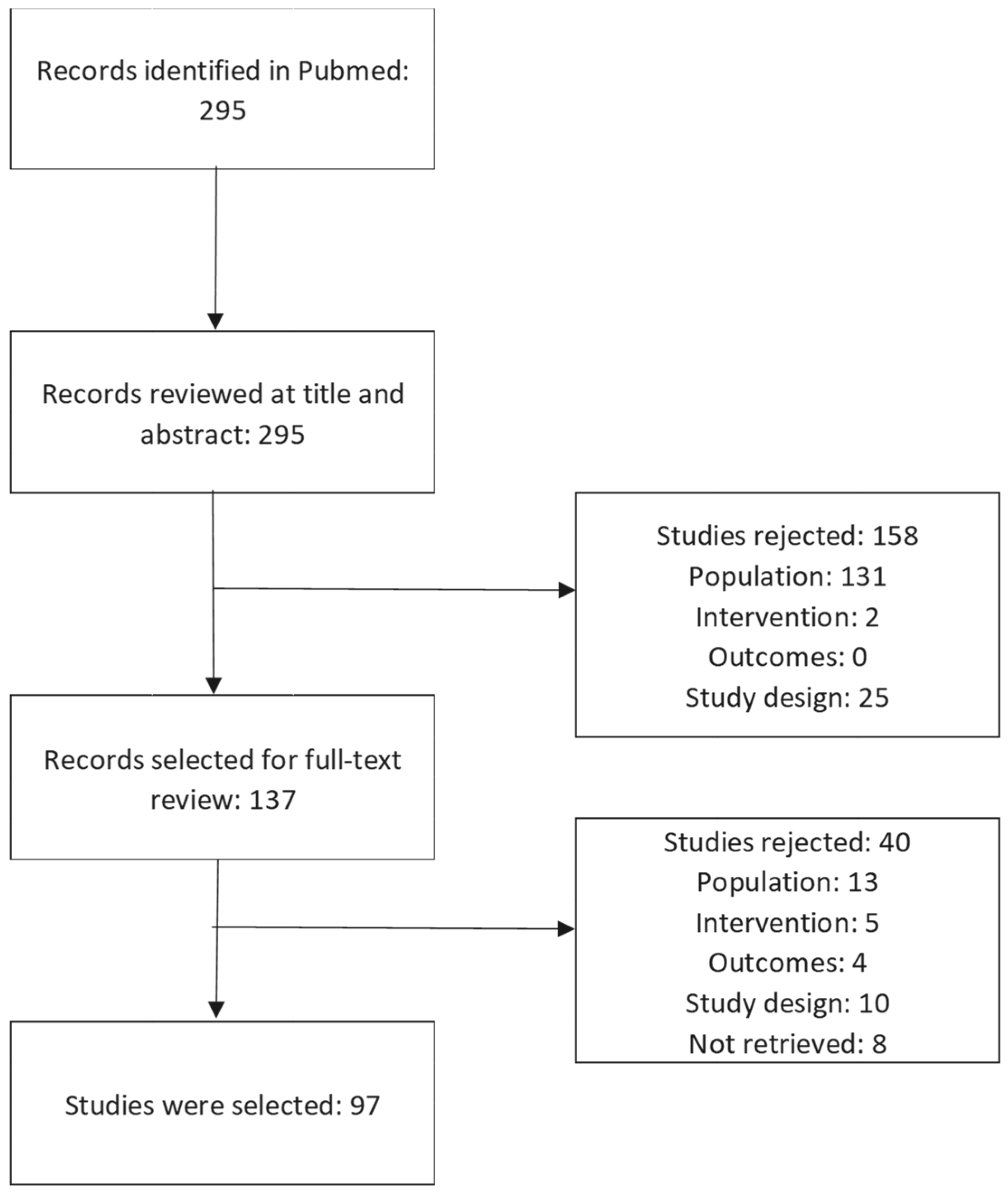
2. Materials and Methods
3. Results
3.1. Studies’ Characteristics
3.2. Patients’ Characteristics
3.3. General Considerations regarding Treatment Options
3.3.1. Colonoscopy Utility in the Emergency Setting
3.3.2. Conservative Treatment in the Emergency Setting
3.3.3. Surgical Treatment in the Emergency Setting
3.4. Malignant Degeneration of Endometriosis
3.5. Treatment Particularities Based on the Site of Obstruction
3.5.1. Ileal Obstruction
3.5.2. Ileocecal Obstruction
3.5.3. Rectal Obstruction
3.5.4. Sigmoid Colon Obstruction
3.5.5. Rectosigmoid Obstruction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cappell, M.S.; Batke, M. Mechanical Obstruction of the Small Bowel and Colon. Med. Clin. N. Am. 2008, 92, 575–597. [Google Scholar] [CrossRef]
- Hill, A.G. The Management of Adhesive Small Bowel Obstruction—An Update. Int. J. Surg. 2008, 6, 77–80. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Drożdż, W.; Budzyński, P. Change in mechanical bowel obstruction demographic and etiological patterns during the past century: Observations from one health care institution. Arch. Surg. 2012, 147, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Maung, A.A.; Johnson, D.C.; Piper, G.L.; Barbosa, R.R.; Rowell, S.E.; Bokhari, F.; Collins, J.N.; Gordon, J.R.; Ra, J.H.; Kerwin, A.J. Evaluation and Management of Small-Bowel Obstruction: An Eastern Association for the Surgery of Trauma Practice Management Guideline. J. Trauma Acute Care Surg. 2012, 73, S362–S369. [Google Scholar] [CrossRef] [PubMed]
- Richard, P.G.; Issa, Y.; van Santbrink, E.J.P.; Bouvy, N.D.; Kruitwagen, R.F.P.M.; Jeekel, J.; Bakkum, E.A.; Rovers, M.M.; van Goor, H. Burden of Adhesions in Abdominal and Pelvic Surgery: Systematic Review and Met-Analysis. BMJ 2013, 347, f5588. [Google Scholar] [CrossRef]
- Markogiannakis, H.; Messaris, E.; Dardamanis, D.; Pararas, N.; Tzertzemelis, D.; Giannopoulos, P.; Larentzakis, A.; Lagoudianakis, E.; Manouras, A.; Bramis, I. Acute Mechanical Bowel Obstruction: Clinical Presentation, Etiology, Management and Outcome Rapid Communication. World J. Gastroenterol. 2007, 13, 432–437. [Google Scholar] [CrossRef]
- Taourel, P.; Kessler, N.; Lesnik, A.; Pujol, J.; Morcos, L.; Bruel, J.M. Helical CT of Large Bowel Obstruction. Abdom. Imaging 2003, 28, 267–275. [Google Scholar] [CrossRef]
- Catena, F.; de Simone, B.; Coccolini, F.; di Saverio, S.; Sartelli, M.; Ansaloni, L. Bowel Obstruction: A Narrative Review for All Physicians. World J. Emerg. Surg. 2019, 14, 20. [Google Scholar] [CrossRef]
- Benagiano, G.; Brosens, I.; Lippi, D. The History of Endometriosis. Gynecol. Obstet. Investig. 2014, 78, 1–9. [Google Scholar] [CrossRef]
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256. [Google Scholar] [CrossRef]
- Maggiore, U.L.R.; Ferrero, S.; Mangili, G.; Bergamini, A.; Inversetti, A.; Giorgione, V.; Viganò, P.; Candiani, M. A Systematic Review on Endometriosis during Pregnancy: Diagnosis, Misdiagnosis, Complications and Outcomes. Hum. Reprod. Update 2016, 22, 70–103. [Google Scholar] [CrossRef] [PubMed]
- Smolarz, B.; Szyłło, K.; Romanowicz, H. Endometriosis: Epidemiology, Classification, Pathogenesis, Treatment and Genetics (Review of Literature). Int. J. Mol. Sci. 2021, 22, 10554. [Google Scholar] [CrossRef]
- Eskenazi, B.; Warner, M.L. Epidemiology Of Endometriosis. Obstet. Gynecol. Clin. N. Am. 1997, 24, 235–258. [Google Scholar] [CrossRef] [PubMed]
- Nap, A.W.; Groothuis, P.G.; Demir, A.Y.; Evers, J.L.H.; Dunselman, G.A.J. Pathogenesis of Endometriosis. Best Pract. Res. Clin. Obstet. Gynaecol. 2004, 18, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Roth, L.M. Endometriosis with Perineural Involvement. Am. J. Clin. Pathol. 1973, 59, 807–809. [Google Scholar] [CrossRef] [PubMed]
- Possover, M.; Rhiem, K.; Chiantera, V. The “Neurologic Hypothesis”: A New Concept in the Pathogenesis of the Endometriosis? Gynecol. Surg. 2005, 2, 107–111. [Google Scholar] [CrossRef]
- Ion, D.; Bolocan, A.; Piţuni, S.M.; Mateoiu, P.E.; Musat, F.; Andronic, O.; Pǎduraru, D.N. Concomitant Inguinal Endometriosis and Groin Hernia—Case Report. Arch. Balk. Med. Union 2017, 52, 462–466. [Google Scholar]
- Yong, P.J.; Bedaiwy, M.A.; Alotaibi, F.; Anglesio, M.S. Pathogenesis of bowel endometriosis. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 71, 2–13. [Google Scholar] [CrossRef]
- Sánchez-Cifuentes, Á.; Candel-Arenas, M.F.; Albarracín-Marín-Blázquez, A. Intestinal Endometriosis. Our Experience. Rev. Esp. Enferm. Dig. 2016, 108, 524–525. [Google Scholar] [CrossRef]
- Veeraswamy, A.; Lewis, M.; Mann, A.; Kotikela, S.; Hajhosseini, B.; Nezhat, C. Extragenital Endometriosis. Clin. Obstet. Gynecol. 2010, 53, 449–466. [Google Scholar] [CrossRef]
- Allan, Z. A Case of Endometriosis Causing Acute Large Bowel Obstruction. Int. J. Surg. Case Rep. 2018, 42, 247–249. [Google Scholar] [CrossRef] [PubMed]
- Palcău, C.; Bolocan, A.; Luiza Nechita, S.; Ion, D.; Păduraru, D.N. Acute Large Bowel Obstruction-A Rare Presentation Of Colonic Endometriosis Case Report. Rom. J. Emerg. Surg. 2021, 3, 2. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Dignen, B. English for Presentations; York Associates International: York, UK, 2008; ISBN 9781900991193. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Santos-Manzur, A.; Valdez-Bocanegra, D.R.; Ornelas-Flores, M.C.; Pineda-Díaz, J.; Stoopen-Margain, E. Ileal Obstruction Caused by Transmural Endometriosis in a Patient with Simultaneous C. Difficile Colitis and Influenza AH1N1. Case Report. Int. J. Surg. Case Rep. 2020, 76, 522–525. [Google Scholar] [CrossRef]
- Nagakari, K.; Azuma, D.; Takehara, K.; Ohuchi, M.; Ishizaki, Y.; Sakamoto, K. Laparoscopic Triple Segmental Bowel Resection for Endometriosis Revealed by Rectal Obstruction during Infertility Treatment. Case Rep. Gastroenterol. 2022, 16, 29–36. [Google Scholar] [CrossRef]
- Quicray, M.; Darwish, B.; Bridoux, V.; Roman, H. Bowel Occlusion in an Infertile Woman with Documented Deep Endometriosis of the Sigmoid Colon: Why Was It Not Unexpected? Gynecol. Obstet. Fertil. 2016, 44, 727–729. [Google Scholar] [CrossRef]
- Moktan, V.P.; Koop, A.H.; Olson, M.T.; Lewis, M.D.; Gomez, V.; Farraye, F.A. An Unusual Cause of Large Bowel Obstruction in a Patient With Ulcerative Colitis. ACG Case Rep. J. 2021, 8, e00638. [Google Scholar] [CrossRef]
- Naem, A.; Shamandi, A.; Al-Shiekh, A.; Alsaid, B. Free Large Sized Intra-Abdominal Endometrioma in a Postmenopausal Woman: A Case Report. BMC Women’s Health 2020, 20, 190. [Google Scholar] [CrossRef]
- Bidarmaghz, B.; Shekhar, A.; Hendahewa, R. Sigmoid Endometriosis in a Post-Menopausal Woman Leading to Acute Large Bowel Obstruction: A Case Report. Int. J. Surg. Case Rep. 2016, 28, 65–67. [Google Scholar] [CrossRef]
- Deval, B.; Rafii, A.; Dachez, M.F.; Kermanash, R.; Levardon, M. Sigmoid Endometriosis in a Postmenopausal Woman. Am. J. Obstet. Gynecol. 2002, 187, 1723–1725. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.T.; Jabbour, R.J.; Girling, J.C.; McDonald, P.J. Extraluminal Bowel Obstruction by Endometrioid Adenocarcinoma 34 Years Post-Hysterectomy: Risks of Unopposed Oestrogen Therapy. J. R. Soc. Med. 2011, 104, 421–423. [Google Scholar] [CrossRef] [PubMed]
- Izuishi, K.; Sano, T.; Shiota, A.; Mori, H.; Ebara, K. Small Bowel Obstruction Caused by Endometriosis in a Postmenopausal Woman. Asian J. Endosc. Surg. 2015, 8, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Popoutchi, P.; dos Reis Lemos, C.R.; Silva, J.C.; Nogueira, A.A.; Feres, O.; Ribeiro da Rocha, J.J. Postmenopausal Intestinal Obstructive Endometriosis: Case Report and Review of the Literature. Sao Paulo Med. J. 2008, 126, 190–193. [Google Scholar] [CrossRef]
- Calcagno, P.; Viti, M.; Cornelli, A.; Galli, D.; D’Urbano, C. Intestinal Obstruction Caused by Endometriosis: Endoscopic Stenting and Expedited Laparoscopic Resection Avoiding Stoma. A Case Report and Review of the Literature. Int. J. Surg. Case Rep. 2018, 44, 75–77. [Google Scholar] [CrossRef]
- Whelton, C.; Bhowmick, A. Acute Endometrial Bowel Obstruction—A Rare Indication for Colonic Stenting. Int. J. Surg. Case Rep. 2013, 4, 160–163. [Google Scholar] [CrossRef][Green Version]
- Navajas-Laboa, M.; Orive-Calzada, A.; Landaluce, A.; Zabalza-Estevez, I.; Larena, J.A.; Arévalo-Serna, J.A.; Bridet, L.; López-López, M.; Torres-Burgos, S.; Bernal-Martínez, A.; et al. Colonic Obstruction Caused by Endometriosis Solved with a Colonic Stent as a Bridge to Surgery. Arab. J. Gastroenterol. 2015, 16, 33–35. [Google Scholar] [CrossRef]
- Sali, P.A.; Yadav, K.S.; Desai, G.S.; Bhole, B.P.; George, A.; Parikh, S.S.; Mehta, H.S. Small Bowel Obstruction Due to an Endometriotic Ileal Stricture with Associated Appendiceal Endometriosis: A Case Report and Systematic Review of the Literature. Int. J. Surg. Case Rep. 2016, 23, 163–168. [Google Scholar] [CrossRef]
- Koyama, R.; Aiyama, T.; Yokoyama, R.; Nakano, S. Small Bowel Obstruction Caused by Ileal Endometriosis with Appendiceal and Lymph Node Involvement Treated with Single-Incision Laparoscopic Surgery: A Case Report and Review of the Literature. Am. J. Case Rep. 2021, 22, e930141. [Google Scholar] [CrossRef]
- Torralba-Morón, A.; Urbanowicz, M.; Andres, C.I.-D.; Lopez-Alonso, G.; Colina-Ruizdelgado, F.; Guerra-Vales, J.-M. Acute Small Bowel Obstruction and Small Bowel Perforation as a Clinical Debut of Intestinal Endometriosis: A Report of Four Cases and Review of the Literature. Intern. Med. 2016, 55, 2595–2599. [Google Scholar] [CrossRef]
- de Ceglie, A.; Bilardi, C.; Blanchi, S.; Picasso, M.; di Muzio, M.; Trimarchi, A.; Conio, M. Acute Small Bowel Obstruction Caused by Endometriosis: A Case Report and Review of the Literature. World J. Gastroenterol. 2008, 14, 3430–3434. [Google Scholar] [CrossRef] [PubMed]
- Lam, K.; Lang, E. Endometriosis as a Rare Cause of Small Bowel Obstruction. ANZ J. Surg. 2020, 90, E137–E138. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Yamadera, M.; Takeo, H.; Murayama, M. Small Bowel Obstruction Caused by Appendiceal and Ileal Endometriosis: A Case Report. J. Surg. Case Rep. 2022, 2022, rjac282. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.L.; Chua, D.; Ravindran, P.; Perez Cerdeira, M.; Mor, I. A Case Report of Endometriosis Presenting as an Acute Small Bowel Obstruction. Int. J. Surg. Case Rep. 2017, 41, 17–19. [Google Scholar] [CrossRef]
- López Carrasco, A.; Hernández Gutiérrez, A.; Hidalgo Gutiérrez, P.A.; Rodríguez González, R.; Marijuán Martín, J.L.; Zapardiel, I.; de Santiago García, J. Ileocecal Endometriosis: Diagnosis and Management. Taiwan J. Obstet. Gynecol. 2017, 56, 243–246. [Google Scholar] [CrossRef]
- Zepeda, M.R.; Win, S.K. A Rare Case of Endometriosis of the Small Bowel. Case Rep. Pathol. 2021, 2021, 6676855. [Google Scholar] [CrossRef]
- Morales-Morales, C.A.; Morales-Flores, L.F.; Gonzalez-Urquijo, M.; Suárez-Márquez, E.; Zambrano-Lara, M.; Baca-Arzaga, A.A.; Tijerina-Gómez, L.O. Ileocolonic Intussusception Due to Severe Endometriosis. Clin. J. Gastroenterol. 2021, 14, 1381–1385. [Google Scholar] [CrossRef]
- Arata, R.; Takakura, Y.; Ikeda, S.; Itamoto, T. A Case of Ileus Caused by Ileal Endometriosis with Lymph Node Involvement. Int. J. Surg. Case Rep. 2019, 54, 90–94. [Google Scholar] [CrossRef]
- Ávila Vergara, M.A.; Sánchez Carrillo, V.; Peraza Garay, F. Bowel Obstruction Secondary to Deep Infiltrating Endometriosis of the Ileum. Rev. Esp. Enferm. Dig. 2018, 110, 208–209. [Google Scholar] [CrossRef]
- Marchena-Gomez, J.; Conde-Martel, A.; Hemmersbach-Miller, M.; Alonso-Fernandez, A. Metachronic Malignant Transformation of Small Bowel and Rectal Endometriosis in the Same Patient. World J. Surg. Oncol. 2006, 4, 93. [Google Scholar] [CrossRef][Green Version]
- Arer, I.M.; Yabanoglu, H.; Hasbay, B. Anastomotic Leakage in a Patient with Acute Intestinal Obstruction Secondary to Appendiceal and Ileal Endometriosis: A Case Report. J. Clin. Diagn. Res. 2016, 10, PD21–PD22. [Google Scholar] [CrossRef]
- Khwaja, S.A.; Zakaria, R.; Carneiro, H.A.; Khwaja, H.A. Endometriosis: A Rare Cause of Small Bowel Obstruction. BMJ Case Rep. 2012, 2012, bcr0320125988. [Google Scholar] [CrossRef] [PubMed]
- Dhannoon, A.; Bajwa, A.; Kunna, M.; Canney, A.; Nugent, E. Beyond Borders: A Case Report of Small Bowel Obstruction Secondary to Undiagnosed Florid Endometriosis. Int. J. Surg. Case Rep. 2022, 93, 106994. [Google Scholar] [CrossRef] [PubMed]
- Karaman, K.; Pala, E.E.; Bayol, U.; Akman, O.; Olmez, M.; Unluoglu, S.; Ozturk, S. Endometriosis of the Terminal Ileum: A Diagnostic Dilemma. Case Rep. Pathol. 2012, 2012, 742035. [Google Scholar] [CrossRef] [PubMed]
- Bratu, D.; Chicea, R.; Ciprian, T.; Beli, L.; Dan, S.; Mihetiu, A.; Adrian, B. A Rare Case of Ileus Caused by Ileum Endometriosis. Int. J. Surg. Case Rep. 2016, 26, 24–26. [Google Scholar] [CrossRef]
- Lea, R.; Whorwell, P.J. Irritable Bowel Syndrome or Endometriosis, or Both? Eur. J. Gastroenterol. Hepatol. 2003, 15, 1131–1133. [Google Scholar] [CrossRef]
- Shah, M.; Tager, D.; Feller, E. Intestinal endometriosis masquerading as common digestive disorders. Arch. Intern. Med. 1995, 155, 977–980. [Google Scholar] [CrossRef]
- Ranaweera, R.K.; Gamage, S.M.; Ubayawansa, D.H.; Kumara, M.M. Terminal Ilial Intussusception in an Adult Due to Endometriosis. BMC Res. Notes 2016, 9, 239. [Google Scholar] [CrossRef]
- Laiz Díez, B.; García Muñoz-Najar, A.; Durán Poveda, M. Laparoscopic Management of a Small Bowel Obstruction Caused by an Endometriotic Focus. Rev. Esp. Enferm. Dig. 2019, 111, 887–888. [Google Scholar] [CrossRef]
- Dong, C.; Ngu, W.S.; Wakefield, S.E. Endometriosis Masquerading as Crohn’s Disease in a Patient with Acute Small Bowel Obstruction. BMJ Case Rep. 2015, 2015, bcr2014207229. [Google Scholar] [CrossRef]
- Upreti, S.; Bansal, R.; Upreti, S.; Mathur, S. Stromal Endometriosis of the Intestine: An Elusive Presentation with a Review of the Literature: A Case Report. J. Clin. Diagn. Res. 2013, 7, 378–380. [Google Scholar] [CrossRef] [PubMed]
- Ridha, J.R.; Cassaro, S. Acute Small Bowel Obstruction Secondary to Ileal Endometriosis: Report of a Case. Surg. Today 2003, 33, 944–947. [Google Scholar] [CrossRef] [PubMed]
- Poole, R.W. Acute Small Bowel Obstruction Due to Endometriosis. Can. Med. Assoc. J. 1961, 84, 903–905. [Google Scholar]
- Gregorić, P.; Doklestić, K.; Pandurović, M.; Radenković, D.; Karadžić, B.; Raspopović, M.; Micev, M.; Ivančević, N.; Šijački, A.; Bajec, D. Distal Ileal Endometriosis as a Cause of Ileus: A Case Report. Srp. Arh. Celok. Lek. 2012, 140, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Attar, A.; Lagorce, C. Small Bowel Obstruction Caused by Endometriosis. Clin. Gastroenterol. Hepatol. 2007, 5, PA30. [Google Scholar] [CrossRef]
- Koutsourelakis, I.; Markakis, H.; Koulas, S.; Mparmpantonakis, N.; Perraki, E.; Christodoulou, K. Ileocolic Intussusception Due to Endometriosis. J. Soc. Laparosc. Robot. Surg. 2007, 11, 131–135. [Google Scholar]
- Rancaño, R.S.; Choho, K.K.; Morales, M.D.; Bueno, V.M.S.; Soto, M.d.M.D.E.; Santacruz, Y.R.; Guillén, R.A. Ileal Obstruction Due to Endometriosis, with Associated Appendiceal Involvement: A Unique and Elusive Situation. Gastroenterol. Hepatol. 2022, 45, 135–136. [Google Scholar] [CrossRef]
- Fernández-Rey, C.L.; Álvarez-González, S.A.; Díaz-Solís, P.; Blanco-González, A.; Costilla-García, S. Small Bowel Obstruction Secondary to Ileal Endometriosis: Multisection Computer Tomography Evaluation. Rev. Esp. Enferm. Dig. 2009, 101, 872. [Google Scholar] [CrossRef]
- Harty, R.F.; Kaude, J.V. Invasive Endometriosis of the Terminal Ileum: A Cause of Small Bowel Obstruction of Obscure Origin. South. Med. J. 1983, 76, 253–255. [Google Scholar] [CrossRef]
- Collins, P.G. Endometriosis as a Cause of Intestinal Obstruction: A Report of Two Cases. Postgrad. Med. J. 1957, 33, 519–525. [Google Scholar] [CrossRef][Green Version]
- Mussa, F.F.; Younes, Z.; Tihan, T.; Lacy, B.E. Anasarca and Small Bowel Obstruction Secondary to Endometriosis. J. Clin. Gastroenterol. 2001, 32, 167–171. [Google Scholar] [CrossRef]
- Singh, K.K.; Lessells, A.M.; Adam, D.J.; Jordan, C.; Miles, W.F.A.; MacIntyre, I.M.C.; Greig, J.D. Presentation of Endometriosis to General Surgeons: A 10-Year Experience. Br. J. Surg. 2005, 82, 1349–1351. [Google Scholar] [CrossRef]
- Slesser, A.A.P.; Sultan, S.; Kubba, F.; Sellu, D.P. Acute Small Bowel Obstruction Secondary to Intestinal Endometriosis, an Elusive Condition: A Case Report. World J. Emerg. Surg. 2010, 5, 27. [Google Scholar] [CrossRef] [PubMed]
- Asanza-Llorente, J.A.; Serrano-Egea, A.; López-López, A.; García-Aparicio, M.; Calderón-Duque, T.; Timón-Peralta, J. Enterovesical Fistula and Intestinal Obstruction by Ileal Endometriosis. Rev. Esp. Enferm. Dig. 2013, 105, 504–506. [Google Scholar] [CrossRef] [PubMed]
- Popivanov, G.; Stoyanova, D.; Fakirova, A.; Konakchieva, M.; Stefanov, D.; Kjossev, K.; Mutafchiyski, V. Ileus Caused by Small Bowel, Ileocaecal and Rectal Endometriosis Misdiagnosed as Crohn’s Disease and Managed by Synchronous Ileocaecal and Rectal Resection. Ann. R. Coll. Surg. Engl. 2020, 102, e205–e208. [Google Scholar] [CrossRef] [PubMed]
- Bacalbasa, N.; Balescu, I.; Filipescu, A. Ileocecal Obstruction Due to Endometriosis—A Case Report and Literature Review. In Vivo 2017, 31, 999–1002. [Google Scholar] [CrossRef][Green Version]
- Shetty, S.; Varma, D. Rare Case of Ileocecal Obstruction Secondary to Endometriosis Presenting for the First Time. Cureus 2021, 13, e17074. [Google Scholar] [CrossRef]
- Preziosi, G.; Cristaldi, M.; Angelini, L. Intestinal Obstruction Secondary to Endometriosis: A Rare Case of Synchronous Bowel Localization. Surg. Oncol. 2007, 16, 161–163. [Google Scholar] [CrossRef]
- Benigno, L.; Lisarelli, L.; Sortino, R.; Neuweiler, J.; Steffen, T. A Rare Case of Ileocolic Intussusception Due to Severe Endometriosis. J. Surg. Case Rep. 2020, 2020, rjaa116. [Google Scholar] [CrossRef]
- Fujimoto, A.; Osuga, Y.; Tsutsumi, O.; Fujii, T.; Okagaki, R.; Taketani, Y. Successful Laparoscopic Treatment of Ileo-Cecal Endometriosis Producing Bowel Obstruction. J. Obstet. Gynaecol. Res. 2001, 27, 221–223. [Google Scholar] [CrossRef]
- Vahdat, M.; Sariri, E.; Mehdizadeh, A.; Najmi, Z.; Shayanfar, N. Colonic Obstruction as an Unusual Presentation of Endometrioma: A Case Report. Surg. Laparosc. Endosc. Percutaneous Tech. 2013, 23, e131–e133. [Google Scholar] [CrossRef]
- Kinder, C.H. Acute Small-Bowel Obstruction Due to Endometriosis. Br. J. Surg. 2005, 41, 550–552. [Google Scholar] [CrossRef] [PubMed]
- Nagar, H.S.; Tyagi, A.K.; Chouhan, A.; Mohanty, S.K. Ileocaecal Endometriosis with Intestinal Obstruction. Med. J. Armed Forces India 2005, 61, 82–83. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Imasogie, D.E.; Agbonrofo, P.I.; Momoh, M.I.; Obaseki, D.E.; Obahiagbon, I.; Azeke, A.T. Intestinal Obstruction Secondary to Cecal Endometriosis. Niger. J. Clin. Pract. 2018, 21, 1081–1085. [Google Scholar] [CrossRef] [PubMed]
- Molina, G.A.; Ramos, D.R.; Yu, A.; Paute, P.A.; Llerena, P.S.; Alexandra Valencia, S.; Fonseca, J.V.; Morillo, J.F.; López, S.C.; Gutierrez, B.M. Endometriosis Mimicking a Cecum Mass with Complete Bowel Obstruction: An Infrequent Cause of Acute Abdomen. Case Rep. Surg. 2019, 2019, 7024172. [Google Scholar] [CrossRef]
- Katagiri, H.; Lefor, A.K.; Nakata, T.; Matsuo, T.; Shimokawa, I. Intussusception Secondary to Endometriosis of the Cecum. Int. J. Surg. Case Rep. 2014, 5, 890–892. [Google Scholar] [CrossRef]
- Nozari, N.; Shafiei, M.; Sarmadi, S. An Unusual Presentation of Endometriosis as an Ileocolic Intussusception with Cecal Mass: A Case Report. J. Reprod. Infertil. 2018, 19, 247–249. [Google Scholar]
- Alexandrino, G.; Lourenço, L.C.; Carvalho, R.; Sobrinho, C.; Horta, D.V.; Reis, J. Endometriosis: A Rare Cause of Large Bowel Obstruction. GE Port. J. Gastroenterol. 2018, 25, 86–90. [Google Scholar] [CrossRef]
- Alvarado, L.E.R.; Bahmad, H.; Mejia, O.; Hollembeak, H.; Poppiti, R.; Howard, L.; Muddasani, K. Rectal Endometriosis Presenting as Toxic Megacolon. Autops. Case Rep. 2021, 11, e2021319. [Google Scholar] [CrossRef]
- Katsikogiannis, N.; Tsaroucha, A.K.; Dimakis, K.; Sivridis, E.; Simopoulos, C.E. Rectal Endometriosis Causing Colonic Obstruction and Concurrent Endometriosis of the Appendix: A Case Report. J. Med. Case Rep. 2011, 5, 320. [Google Scholar] [CrossRef]
- Ono, H.; Honda, S.; Danjo, Y.; Nakamura, K.; Okabe, M.; Kimura, T.; Kawakami, M.; Nagashima, K.; Nishihara, H. Rectal Obstruction Due to Endometriosis: A Case Report and Review of the Japanese Literature. Int. J. Surg. Case Rep. 2014, 5, 845–848. [Google Scholar] [CrossRef] [PubMed]
- Mourthé De Alvim Andrade, M.; Batista Pimenta, M.; de Freitas Belezia, B.; Duarte, T. Rectal Obstruction Due to Endometriosis. Tech. Coloproctol. 2008, 12, 57–59. [Google Scholar] [CrossRef]
- Jarmin, R.; Idris, M.A.; Shaharuddin, S.; Nadeson, S.; Rashid, L.M.; Mustaffa, W.M.W. Intestinal Obstruction Due to Rectal Endometriosis: A Surgical Enigma. Asian J. Surg. 2006, 29, 149–152. [Google Scholar] [CrossRef]
- Xu, Y.; Xu, Y.; Miao, L.; Cao, M.; Xu, W.; Shi, L. Comprehensive Surgical Treatment for Obstructive Rectal Endometriosis: A Case Report and Review of the Literature. BMC Women’s Health 2022, 22, 280. [Google Scholar] [CrossRef] [PubMed]
- Falleni, M.; Bauer, D.; Opocher, E.; Moneghini, L.; Bulfamante, G.P. A rare case of transmural endometriosis in primary adenocarcinoma of the rectum. Pathologica 2014, 106, 14–15. [Google Scholar]
- Insabato, L.; D’Armiento, F.P.; Tornillo, L. A Rectal Endometrioma Producing Intestinal Obstruction. J. Clin. Gastroenterol. 1994, 19, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Galazis, N.; Arul, D.; Wilson, J.; Pisal, N. Bowel endometriosis. BMJ Case Rep. 2014, 2014, bcr2013202140. [Google Scholar] [CrossRef]
- Stevens, K.; Wasfie, T.; Haus, C. Endometrioma Causing Near-Complete Obstruction of the Sigmoid Colon. Am. Surg. 2021, 89, 1264–1266. [Google Scholar] [CrossRef]
- El Bakouri, A.; El Karouachi, A.; Bouali, M.; Khouaja, A.; Elhattabi, K.; Bensardi, F.; Fadil, A.; Karkouri, M. Acute Colonic Occlusion over Endometriosis: About a Case. Int. J. Surg. Case Rep. 2021, 80, 105615. [Google Scholar] [CrossRef]
- Buldanlı, M.Z.; Özemir, İ.A.; Yener, O.; Dölek, Y. A Rare Case of Acute Mechanical Intestinal Obstruction: Colonic Endometriosis. Ulus. Travma Acil Cerrahi Derg. 2020, 26, 148–151. [Google Scholar] [CrossRef]
- Shaw, A.; Lund, J.N.; Semeraro, D.; Cartmill, M.; Reynolds, J.R.; Tierney, G.M. Large Bowel Obstruction and Perforation Secondary to Endometriosis Complicated by a Ventriculoperitoneal Shunt. Color. Dis. 2008, 10, 520–521. [Google Scholar] [CrossRef] [PubMed]
- Bascombe, N.A.; Naraynsingh, V.; Dan, D.; Harnanan, D. Isolated Endometriosis Causing Sigmoid Colon Obstruction: A Case Report. Int. J. Surg. Case Rep. 2013, 4, 1073–1075. [Google Scholar] [CrossRef] [PubMed]
- Baden, D.N.; van de Ven, A.; Verbeek, P.C. Endometriosis with an Acute Colon Obstruction: A Case Report. J. Med. Case Rep. 2015, 9, 150. [Google Scholar] [CrossRef] [PubMed]
- Sarofim, M.; Attwell-Heap, A.; Trautman, J.; Kwok, A.; Still, A. Unusual Case of Acute Large Bowel Obstruction: Endometriosis Mimicking Sigmoid Malignancy. ANZ J. Surg. 2019, 89, E542–E543. [Google Scholar] [CrossRef]
- De Weerdt, V.; Bossuyt, P.; Peperstraete, L. Colonic obstruction in a 45 year old female. Acta Gastro Enterol. Belg. 2014, 77, 433–434. [Google Scholar]
- Al-Qahtani, H.H.; Alfalah, H.; Al-Salamah, R.A.; Elshair, A.A. Sigmoid Colon Endometriotic Mass. Saudi Med. J. 2015, 36, 630–633. [Google Scholar] [CrossRef]
- Arafat, S.; Alsabek, M.B.; Almousa, F.; Kubtan, M.A. Rare Manifestation of Endometriosis Causing Complete Recto-Sigmoid Obstruction: A Case Report. Int. J. Surg. Case Rep. 2016, 26, 30–33. [Google Scholar] [CrossRef]
- Rana, R.; Sharma, S.; Narula, H.; Madhok, B. A Case of Recto-Sigmoid Endometriosis Mimicking Carcinoma. SpringerPlus 2016, 5, 643. [Google Scholar] [CrossRef]
- Murji, A.; Sobel, M.L. Bowel Obstruction and Pelvic Mass. Can. Med. Assoc. J. 2011, 183, 686–692. [Google Scholar] [CrossRef][Green Version]
- de Jong, M.J.H.; Mijatovic, V.; van Waesberghe, J.H.T.M.; Cuesta, M.A.; Hompes, P.G.A. Surgical Outcome and Long-Term Follow-up after Segmental Colorectal Resection in Women with a Complete Obstruction of the Rectosigmoid Due to Endometriosis. Dig. Surg. 2009, 26, 50–55. [Google Scholar] [CrossRef]
- Pramateftakis, M.G.; Psomas, S.; Kanellos, D.; Vrakas, G.; Roidos, G.; Makrantonakis, A.; Kanellos, I. Large Bowel Obstruction Due to Endometriosis. Tech. Coloproctol. 2010, 14, 87–89. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Kuo, L.-J.; Chuang, A.-Y.; Cheng, T.-I.; Hung, C.-F. Extrapelvic Endometriosis Complicated with Colonic Obstruction. J. Chin. Med. Assoc. 2006, 69, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Caselli, G.; Besa, C.; Pulgar, D. Intestinal Obstruction as Manifestation of a Multifocal Colonic Endometriosis. Clin. Gastroenterol. Hepatol. 2011, 9, e90–e91. [Google Scholar] [CrossRef]
- Yildirim, S.; Nursal, T.Z.; Tarim, A.; Torer, N.; Bal, N.; Yildirim, T. Colonic Obstruction Due to Rectal Endometriosis: Report of a Case. Turk. J. Gastroenterol. 2005, 16, 48–51. [Google Scholar] [PubMed]
- Tate, G.T. Acute Obstruction of the Large Bowel Due to Endometriosis. Br. J. Surg. 1963, 50, 771–773. [Google Scholar] [CrossRef]
- Lanitis, S.; Korontzi, M.; Karaliotas, C. Acute Bowel Obstruction in a Premenopausal Woman. Gastroenterology 2013, 144, e5–e6. [Google Scholar] [CrossRef] [PubMed]
- Eyers, T.; Morgan, B.; Bignold, L. Endometriosis Of The Sigmoid Colon And Rectum. ANZ J. Surg. 1978, 48, 639–643. [Google Scholar] [CrossRef]
- Sassi, S.; Bouassida, M.; Touinsi, H.; Mongi Mighri, M.; Baccari, S.; Chebbi, F.; Bouzeidi, K.; Sassi, S. Exceptional Cause of Bowel Obstruction: Rectal Endometriosis Mimicking Carcinoma of Rectum—A Case Report. Pan. Afr. Med. J. 2011, 10, 33. [Google Scholar] [PubMed]
- Choi, J.D.W.; Yunaev, M. Endometriosis of the Appendix Causing Small Bowel Obstruction in a Virgin Abdomen. BMJ Case Rep. 2019, 12, e230496. [Google Scholar] [CrossRef]
- Jeong, S.J.; Park, J. Endoscopic Management of Benign Colonic Obstruction and Pseudo-Obstruction. Clin. Endosc. 2020, 53, 18–28. [Google Scholar] [CrossRef]
- Beck, D.E. Endoscopic Management of Bowel Obstruction. Clin. Colon Rectal Surg. 2021, 34, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Lemberg, B.; Vargo, J.J. Balloon Dilation of Colonic Strictures. Am. J. Gastroenterol. 2007, 102, 2123–2125. [Google Scholar] [CrossRef] [PubMed]
- Small, A.J.; Young-Fadok, T.M.; Baron, T.H. Expandable Metal Stent Placement for Benign Colorectal Obstruction: Outcomes for 23 Cases. Surg. Endosc. 2008, 22, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-M.; Byeon, J.-S. Colorectal Stents: Current Status. Clin. Endosc. 2015, 48, 194–200. [Google Scholar] [CrossRef]
- Baron, T.H. Colonic Stenting: Technique, Technology, and Outcomes for Malignant and Benign Disease. Gastrointest. Endosc. Clin. N. Am. 2005, 15, 757–771. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Kennedy Burns, M.; DiFrancesco, L.; Nezhat, A.; Nezhat, C. Diagnostic and Treatment Guidelines for Gastrointestinal and Genitourinary Endometriosis. J. Turk.-Ger. Gynecol. Assoc. 2017, 18, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Nezhat, C.; Li, A.; Falik, R.; Copeland, D.; Razavi, G.; Shakib, A.; Mihailide, C.; Bamford, H.; DiFrancesco, L.; Tazuke, S.; et al. Bowel Endometriosis: Diagnosis and Management. Am. J. Obstet. Gynecol. 2018, 218, 549–562. [Google Scholar] [CrossRef]
- Remorgida, V.; Ferrero, S.; Fulcheri, E.; Ragni, N.; Martin, D.C. Bowel Endometriosis: Presentation, Diagnosis, and Treatment. Obstet. Gynecol. Surv. 2007, 62, 461–470. [Google Scholar] [CrossRef]
- Egekvist, A.G.; Marinovskij, E.; Forman, A.; Kesmodel, U.S.; Riiskjaer, M.; Seyer-Hansen, M. Conservative Approach to Rectosigmoid Endometriosis: A Cohort Study. Acta Obstet. Gynecol. Scand. 2017, 96, 745–750. [Google Scholar] [CrossRef]
- Egekvist, A.G.; Marinovskij, E.; Forman, A.; Kesmodel, U.S.; Graumann, O.; Seyer-Hansen, M. Conservative Treatment of Rectosigmoid Endometriosis: A Prospective Study. Acta Obstet. Gynecol. Scand. 2019, 98, 1139–1147. [Google Scholar] [CrossRef]
- Mușat, F.; Bolocan, A.; Ion, D.; Palcău, C.A.; Ginghină, O.; Andronic, O.; Oacheșu, I.M.; Păduraru, D.N. Ileal Endometriosis—A Rare Cause Of Bowel Obstruction. Rom. J. Emerg. Surg. 2022, 4, 132–136. [Google Scholar] [CrossRef]
| Criteria | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Outcomes |
|
|
| Study Design |
|
|
| Author, Year | Country | Patient Age | Previously Diagnosed Endometriosis | Site of the Obstruction | Initial Treatment | Surgical Procedure | Surgical Approach |
|---|---|---|---|---|---|---|---|
| Bidarmaghz et al. 2016 [31] | Australia | 63 | No | Rectosigmoid | Surgical | Hartmann’s procedure | LT |
| Deval et al. 2002 [32] | France | 63 | No | Sigmoid colon | Surgical | Hartmann’s procedure | LT |
| Wang et al. 2011 [33] | UK | 78 | Yes | Sigmoid colon | Surgical | Hartmann’s procedure | LT |
| Naem et al. 2020 [30] | Syria | 67 | No | Omental giant cyst | Surgical | Cystectomy and omentectomy | LT |
| Izuishi et al. 2015 [34] | Japan | 54 | No | Ileum | Conservative | Partial resection of the small bowel with end-to-end anastomosis | SILS |
| Popoutchi et al. 2008 [35] | Brazil | 74 | No | Ileum | Surgical | Segmental enterectomy | LT |
| Initial Treatment | Surgical Treatment | |||||||
|---|---|---|---|---|---|---|---|---|
| Site of the Occlusive Endometrial Foci | Number of Patients | % * | Mean Age | Conservative (for More than 24 h) | Emergency Surgery | Therapeutic Colonoscopy | LT | LS |
| Ileal [26,34,35,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73] | 41 | 38.3 | 42.06 | 7 | 33 | 1 | 30 | 11 |
| Ileocecal [74,75,76,77,78,79,80,81,82,83,84] | 11 | 10.2 | 37.55 | 4 | 7 | 0 | 9 | 2 |
| Cecal [85,86,87,88] | 4 | 3.7 | 38.75 | 0 | 4 | 0 | 4 | 0 |
| Rectal [27,89,90,91,92,93,94,95,96,97] | 11 | 10.2 | 38.45 | 2 | 9 | 0 | 9 | 2 |
| Sigmoidian [28,32,33,36,98,99,100,101,102,103,104,105,106,107] | 14 | 13 | 43.00 | 0 | 12 | 2 | 12 | 2 |
| Rectosigmoidian [21,31,37,38,108,109,110,111,112,113,114,115,116,117,118,119] | 23 | 21.5 | 40.48 | 1 | 20 | 2 | 20 | 2 |
| Hepatic Flexure of the Colon [29] | 1 | 0.9 | 39 | 1 | 0 | 0 | 1 | 0 |
| Appendiceal [120] | 1 | 0.9 | 29 | 0 | 1 | 0 | 0 | 1 |
| Others (Omental Giant Cyst) [30] | 1 | 0.9 | 67 | 0 | 1 | 0 | 1 | 0 |
| Total | 107 | 100 | - | 15 | 87 | 5 | 86 | 20 |
| Digestive Continuity (Number of Patients) | Approach (Number of Patients) | ||||||
|---|---|---|---|---|---|---|---|
| Site of the Occlusive Endometrial Foci | Procedure | Total | Anastomosis | Stoma | N.R. | LS | LT |
| Ileal | Ileocecal resection | 6 | 2 | 1 | 3 | 2 | 4 |
| Right hemicolectomy | 12 | 7 | 5 | 6 | 6 | ||
| Ileal resection | 19 | 11 | 1 | 7 | 3 | 16 | |
| Ileo-transverso-stomy | 1 | - | - | - | 0 | 1 | |
| Biopsy and side-to-side isoperistaltic ileo-transverso-anastomosis | 1 | - | - | - | 0 | 1 | |
| N.R. | 2 | - | - | - | - | - | |
| Ileocecal | Right hemicolectomy | 8 | 6 | 1 | 1 | 1 | 7 |
| Ileocecal resection | 3 | 1 | 1 | 1 | 1 | 2 | |
| Cecal | Right hemicolectomy | 2 | 2 | 0 | - | 0 | 2 |
| Ileocecal resection | 2 | 1 | 0 | 1 | 0 | 2 | |
| Rectal | Total colectomy | 1 | 0 | 1 | 0 | 0 | 1 |
| Colostomy | 3 | 0 | 3 | 0 | 0 | 3 | |
| Anterior resection | 3 | 2 | 0 | 1 | 1 | 2 | |
| Rectosigmoid resection | 4 | 0 | 1 | 3 | 1 | 3 | |
| Sigmoidian | Hartman procedure | 7 | 0 | 7 | 0 | 0 | 7 |
| Left hemicolectomy | 1 | 0 | 1 | 0 | 0 | 1 | |
| Sigmoid colectomy | 5 | 5 | 0 | 0 | 2 | 3 | |
| Sigmoid colostomy | 1 | 0 | 1 | 0 | 0 | 1 | |
| Rectosigmoidian | Hartman procedure | 6 | 0 | 6 | 0 | 0 | 6 |
| Colostomy | 8 | 0 | 8 | 0 | 0 | 8 | |
| Rectosigmoid resection | 5 | 5 | 0 | 0 | 2 | 3 | |
| Anterior resection No surgery | 3 1 | 3 0 | 0 0 | 0 0 | 0 0 | 3 0 | |
| Total Number of Patients * | 104 | 45 | 32 | 22 | 19 | 82 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mușat, F.; Păduraru, D.N.; Bolocan, A.; Constantinescu, A.; Ion, D.; Andronic, O. Endometriosis as an Uncommon Cause of Intestinal Obstruction—A Comprehensive Literature Review. J. Clin. Med. 2023, 12, 6376. https://doi.org/10.3390/jcm12196376
Mușat F, Păduraru DN, Bolocan A, Constantinescu A, Ion D, Andronic O. Endometriosis as an Uncommon Cause of Intestinal Obstruction—A Comprehensive Literature Review. Journal of Clinical Medicine. 2023; 12(19):6376. https://doi.org/10.3390/jcm12196376
Chicago/Turabian StyleMușat, Florentina, Dan Nicolae Păduraru, Alexandra Bolocan, Alexandru Constantinescu, Daniel Ion, and Octavian Andronic. 2023. "Endometriosis as an Uncommon Cause of Intestinal Obstruction—A Comprehensive Literature Review" Journal of Clinical Medicine 12, no. 19: 6376. https://doi.org/10.3390/jcm12196376
APA StyleMușat, F., Păduraru, D. N., Bolocan, A., Constantinescu, A., Ion, D., & Andronic, O. (2023). Endometriosis as an Uncommon Cause of Intestinal Obstruction—A Comprehensive Literature Review. Journal of Clinical Medicine, 12(19), 6376. https://doi.org/10.3390/jcm12196376







