Oral Anticoagulant Use in Patients with Atrial Fibrillation at Low Risk of Stroke and Associated Bleeding Complications
Abstract
:1. Introduction
2. Methods
2.1. Data Source
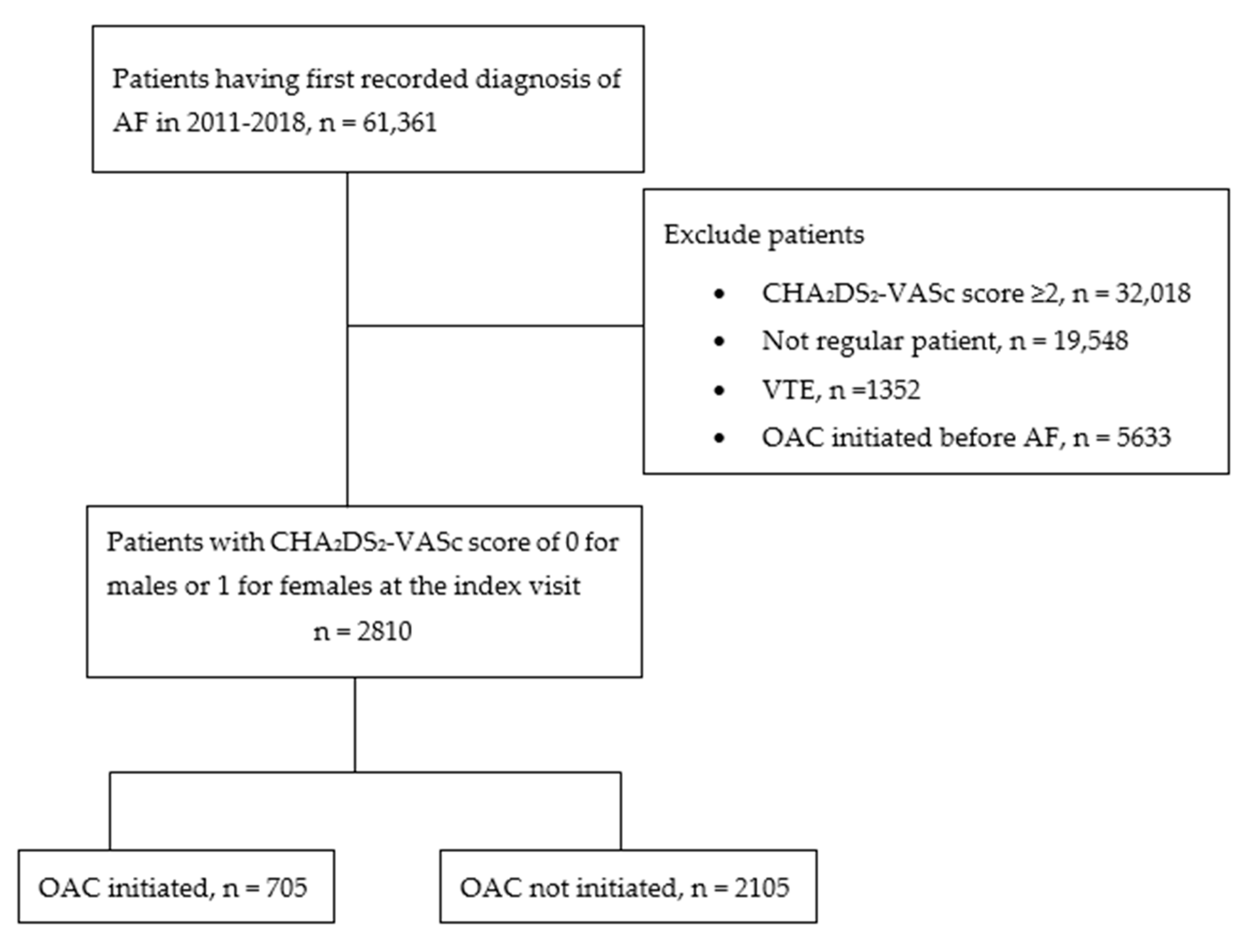
2.2. Study Population
2.3. Study Variables
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics of Study Participants
3.2. Prescription Patterns of OAC in Low-Risk Patients
3.3. Determinants of OAC Prescription in Low-Risk Patients
3.4. Incident Bleeding Events
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Freedman, B.; Potpara, T.S.; Lip, G.Y.H. Stroke prevention in atrial fibrillation. Lancet 2016, 388, 806–817. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Levy, D.; Vaziri, S.M.; D’Agostino, R.B.; Belanger, A.J.; Wolf, P.A. Independent Risk Factors for Atrial Fibrillation in a Population-Based Cohort: The Framingham Heart Study. JAMA 1994, 271, 840–844. [Google Scholar] [CrossRef]
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Hoffman, E.B.; Deenadayalu, N.; Ezekowitz, M.D.; Camm, A.J.; Weitz, J.I.; Lewis, B.S.; Parkhomenko, A.; et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet 2014, 383, 955–962. [Google Scholar] [CrossRef]
- Hart, R.G.; Pearce, L.A.; Aguilar, M.I. Meta-analysis: Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann. Intern. Med. 2007, 146, 857–867. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef]
- January Craig, T.; Wann, L.S.; Alpert Joseph, S.; Calkins, H.; Cigarroa Joaquin, E.; Cleveland Joseph, C.; Conti Jamie, B.; Ellinor Patrick, T.; Ezekowitz Michael, D.; Field Michael, E.; et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation. Circulation 2014, 130, e199–e267. [Google Scholar] [CrossRef]
- NHFA CSANZ Atrial Fibrillation Guideline Working Group; Brieger, D.; Amerena, J.; Attia, J.; Bajorek, B.; Chan, K.H.; Connell, C.; Freedman, B.; Ferguson, C.; Hall, T.; et al. National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand: Australian Clinical Guidelines for the Diagnosis and Management of Atrial Fibrillation 2018. Heart Lung. Circ. 2018, 27, 1209–1266. [Google Scholar] [CrossRef]
- Bezabhe, W.; Bereznicki, L.; Radford, J.; Wimmer, B.; Curtain, C.; Salahudeen, M.; Peterson, G. Ten-year Trends in the Use of Oral Anticoagulants in Australian General Practice Patients with Atrial Fibrillation. Front. Pharmacol. 2021, 12, 586370. [Google Scholar] [CrossRef]
- Grymonprez, M.; Simoens, C.; Steurbaut, S.; De Backer, T.L.; Lahousse, L. Worldwide trends in oral anticoagulant use in patients with atrial fibrillation from 2010 to 2018: A systematic review and meta-analysis. EP Eur. 2022, 24, 887–898. [Google Scholar] [CrossRef]
- Hsu, J.C.; Freeman, J.V. Underuse of Vitamin K Antagonist and Direct Oral Anticoagulants for Stroke Prevention in Patients with Atrial Fibrillation: A Contemporary Review. Clin. Pharmacol. Ther. 2018, 104, 301–310. [Google Scholar] [CrossRef]
- Forslund, T.; Komen, J.J.; Andersen, M.; Wettermark, B.; von Euler, M.; Mantel-Teeuwisse, A.K.; Braunschweig, F.; Hjemdahl, P. Improved Stroke Prevention in Atrial Fibrillation after the Introduction of Non-Vitamin K Antagonist Oral Anticoagulants. Stroke 2018, 49, 2122–2128. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Je, N.K. Underutilization of anticoagulants in patients with nonvalvular atrial fibrillation in the era of non-vitamin K antagonist oral anticoagulants. Int. J. Arrhythm. 2022, 23, 1. [Google Scholar] [CrossRef]
- Komen, J.J.; Pottegård, A.; Mantel-Teeuwisse, A.K.; Forslund, T.; Hjemdahl, P.; Wettermark, B.; Hallas, J.; Olesen, M.; Bennie, M.; Mueller, T.; et al. Oral anticoagulants in patients with atrial fibrillation at low stroke risk: A multicentre observational study. Eur. Heart J. 2022, 43, 3528–3538. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.C.; Chan, P.S.; Tang, F.; Maddox, T.M.; Marcus, G.M. Oral Anticoagulant Prescription in Patients with Atrial Fibrillation and a Low Risk of Thromboembolism: Insights from the NCDR PINNACLE Registry. JAMA Intern. Med. 2015, 175, 1062–1065. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.S.; He, M.; Gabriel, N.; Magnani, J.W.; Kimmel, S.E.; Gellad, W.F.; Hernandez, I. Underprescribing vs underfilling to oral anticoagulation: An analysis of linked medical record and claims data for a nationwide sample of patients with atrial fibrillation. J. Manag. Care Spec. Pharm. 2022, 28, 1400–1409. [Google Scholar] [CrossRef]
- Hsu, J.C.; Maddox, T.M.; Kennedy, K.F.; Katz, D.F.; Marzec, L.N.; Lubitz, S.A.; Gehi, A.K.; Turakhia, M.P.; Marcus, G.M. Oral Anticoagulant Therapy Prescription in Patients with Atrial Fibrillation across the Spectrum of Stroke Risk: Insights from the NCDR PINNACLE Registry. JAMA Cardiol. 2016, 1, 55–62. [Google Scholar] [CrossRef]
- Friberg, L.; Andersson, T.; Rosenqvist, M. Less dementia and stroke in low-risk patients with atrial fibrillation taking oral anticoagulation. Eur. Heart J. 2019, 40, 2327–2335. [Google Scholar] [CrossRef]
- Bezabhe, W.M.; Bereznicki, L.R.; Radford, J.; Wimmer, B.C.; Salahudeen, M.S.; Garrahy, E.; Bindoff, I.; Peterson, G.M. Oral Anticoagulant Treatment and the Risk of Dementia in Patients with Atrial Fibrillation: A Population-Based Cohort Study. J. Am. Heart Assoc. 2022, 11, e023098. [Google Scholar] [CrossRef]
- Bunch, T.J.; May, H.; Cutler, M.; Woller, S.C.; Jacobs, V.; Stevens, S.M.; Carlquist, J.; Knowlton, K.U.; Muhlestein, J.B.; Steinberg, B.A.; et al. Impact of anticoagulation therapy on the cognitive decline and dementia in patients with non-valvular atrial fibrillation (cognitive decline and dementia in patients with non-valvular atrial fibrillation [CAF] trial). J. Arrhythm. 2022, 38, 997–1008. [Google Scholar] [CrossRef]
- Williams, J.M.; Lovelace, B.; Christoph, M.J.; Li, S.; Guo, H.; Hoover, M.; Coleman, C.I. Clinical and health care resource use burden of hospitalizations for oral factor Xa inhibitor-associated major bleeding: A real-world analysis of Medicare beneficiaries. J. Am. Coll. Emerg. Physicians Open 2023, 4, e12956. [Google Scholar] [CrossRef]
- Geller, A.I.; Shehab, N.; Lovegrove, M.C.; Weidle, N.J.; Budnitz, D.S. Bleeding related to oral anticoagulants: Trends in US emergency department visits, 2016–2020. Thromb. Res. 2023, 225, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Bezabhe, W.M.; Bereznicki, L.R.; Radford, J.; Wimmer, B.C.; Curtain, C.; Salahudeen, M.S.; Peterson, G.M. Factors influencing oral anticoagulant use in patients newly diagnosed with atrial fibrillation. Eur. J. Clin. Invest. 2020, 51, e13457. [Google Scholar] [CrossRef] [PubMed]
- MedicineInsight Data Book Version 4.0; NPS MedicineWise: Syndey, Australia, 2021.
- Havard, A.; Manski-Nankervis, J.-A.; Thistlethwaite, J.; Daniels, B.; Myton, R.; Tu, K.; Chidwick, K. Validity of algorithms for identifying five chronic conditions in MedicineInsight, an Australian national general practice database. BMC Health Serv. Res. 2021, 21, 551. [Google Scholar] [CrossRef] [PubMed]
- Busingye, D.; Myton, R.; Mina, R.; Thistlethwaite, J.; Belcher, J.; Chidwick, K. MedicineInsight Report: Validation of the MedicineInsight Database: Completeness, Generalisability and Plausibility; NPS MedicineWise: Syndey, Australia, 2020. [Google Scholar]
- Busingye, D.; Gianacas, C.; Pollack, A.; Chidwick, K.; Merrifield, A.; Norman, S.; Mullin, B.; Hayhurst, R.; Blogg, S.; Havard, A.; et al. Data Resource Profile: MedicineInsight, an Australian national primary health care database. Int. J. Epidemiol. 2019, 48, 1741–1741h. [Google Scholar] [CrossRef]
- The Royal Australian College of General Practitioners. Standards for General Practices; RACGP: East Melbourne, Australia, 2020. [Google Scholar]
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. CHEST 2010, 137, 263–272. [Google Scholar] [CrossRef]
- O’Brien, E.C.; Simon, D.N.; Thomas, L.E.; Hylek, E.M.; Gersh, B.J.; Ansell, J.E.; Kowey, P.R.; Mahaffey, K.W.; Chang, P.; Fonarow, G.C.; et al. The ORBIT bleeding score: A simple bedside score to assess bleeding risk in atrial fibrillation. Eur. Heart J. 2015, 36, 3258–3264. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Australian Statistical Geography Standard; Australian Bureau of Statistics: Canberra, Australia, 2019. [Google Scholar]
- Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA); Australian Bureau of Statistics: Canberra, Australia, 2016. [Google Scholar]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Chen, Q.; Toorop, M.M.A.; Tops, L.F.; Lijfering, W.M.; Cannegieter, S.C. Time Trends in Patient Characteristics, Anticoagulation Treatment, and Prognosis of Incident Nonvalvular Atrial Fibrillation in the Netherlands. JAMA Netw. Open 2023, 6, e239973. [Google Scholar] [CrossRef]
- Phillips, K.; Subramanian, A.; Thomas, G.N.; Khan, N.; Chandan, J.S.; Brady, P.; Marshall, T.; Nirantharakumar, K.; Fabritz, L.; Adderley, N.J. Trends in the pharmacological management of atrial fibrillation in UK general practice 2008–2018. Heart 2022, 108, 517. [Google Scholar] [CrossRef]
- Gebreyohannes, E.; Salter, S.; Chalmers, L.; Bereznicki, L.; Lee, K. Non-adherence to Thromboprophylaxis Guidelines in Atrial Fibrillation: A Narrative Review of the Extent of and Factors in Guideline Non-adherence. Am. J. Cardiovasc. Drugs 2020, 21, 419–433. [Google Scholar] [CrossRef]
- Pilcher, S.M.; Alamneh, E.A.; Chalmers, L.; Bereznicki, L.R. The Tasmanian Atrial Fibrillation Study (TAFS): Differences in Stroke Prevention According to Sex. Ann. Pharmacother. 2020, 54, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Daly, D.J.; Essien, U.R.; Del Carmen, M.G.; Scirica, B.; Berman, A.N.; Searl Como, J.; Wasfy, J.H. Race, ethnicity, sex, and socioeconomic disparities in anticoagulation for atrial fibrillation: A narrative review of contemporary literature. J. Natl. Med. Assoc. 2023, 115, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Munir, M.B.; Hlavacek, P.; Keshishian, A.; Guo, J.D.; Mallampati, R.; Ferri, M.; Russ, C.; Emir, B.; Cato, M.; Yuce, H.; et al. Oral anticoagulant underutilization among elderly patients with atrial fibrillation: Insights from the United States Medicare database. J. Interv. Card Electrophysiol. 2023, 66, 771–782. [Google Scholar] [CrossRef]
- Essien, U.R.; Magnani, J.W.; Chen, N.; Gellad, W.F.; Fine, M.J.; Hernandez, I. Race/Ethnicity and Sex-Related Differences in Direct Oral Anticoagulant Initiation in Newly Diagnosed Atrial Fibrillation: A Retrospective Study of Medicare Data. J. Natl. Med. Assoc. 2020, 112, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Bjorck, F.; Renlund, H.; Lip, G.Y.; Wester, P.; Svensson, P.J.; Sjalander, A. Outcomes in a Warfarin-Treated Population with Atrial Fibrillation. JAMA Cardiol. 2016, 1, 172–180. [Google Scholar] [CrossRef]
- Amaraneni, A.; Chippa, V.; Rettew, A. Anticoagulation Safety. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519025/ (accessed on 18 August 2023).

| Characteristic | All, n (%) | OAC Users (n = 705) | Non-Users (n = 2105) | p-Value |
|---|---|---|---|---|
| Sex, male | 1750 (62.3) | 477 (67.7) | 1273 (60.5) | <0.001 |
| Age, mean (SD) years | 49.3 (10.8) | 51.9 (9.2) | 48.4 (11.1) | 0.022 |
| Diagnosis period | <0.001 | |||
| 2011–2012 | 408 (14.5) | 75 (10.6) | 333 (15.8) | |
| 2013–2014 | 613 (21.8) | 128 (18.2) | 485 (23.0) | |
| 2015–2016 | 788 (28.1) | 214 (30.4) | 574 (27.3) | |
| 2017–2018 | 1001 (35.6) | 288 (40.8) | 713 (33.9) | |
| Indigenous status | n = 2192 | n = 558 | n = 1634 | 0.746 |
| ATSI | 51 (2.3) | 14 (2.5) | 37 (2.3) | |
| Non-ATSI | 2141 (97.7) | 544 (97.5) | 1597 (97.7) | |
| Missing | 618 (22.0) | 147 (20.8) | 471 (22.4) | |
| SEIFA quintiles | n = 2790 | n = 699 | n = 2091 | 0.020 |
| 1 | 384 (13.8) | 122 (17.4) | 262 (12.5) | |
| 2 | 498 (17.9) | 112 (16.0) | 386 (18.5) | |
| 3 | 644 (23.1) | 161 (23.0) | 483 (23.1) | |
| 4 | 552 (19.8) | 132 (18.9) | 420 (20.1) | |
| 5 | 712 (25.5) | 172 (24.6) | 540 (25.8) | |
| States and territories | 0.396 | |||
| ACT | 67 (2.4) | 16 (2.3) | 51 (2.4) | |
| NSW | 1084 (38.6) | 291 (37.7) | 793 (41.3) | |
| NT | 36 (1.3) | 11 (1.6) | 25 (1.2) | |
| QLD | 551 (19.6) | 145 (20.6) | 406 (19.3) | |
| SA | 87 (3.1) | 20 (2.8) | 67 (3.2) | |
| TAS | 190 (6.8) | 47 (6.7) | 143 (6.8) | |
| VIC | 495 (17.6) | 112 (15.9) | 383 18.2) | |
| WA | 300 (10.7) | 63 (8.9) | 237 (11.3) | |
| Rurality | n = 2797 | n = 701 | n = 2096 | 0.108 |
| Major cities | 1684 (60.2) | 419 (59.8) | 1265 (60.4) | |
| Inner regional | 794 (28.4) | 188 (26.8) | 606 (28.9) | |
| Outer regional | 257 (9.2) | 80 (11.4) | 177 (8.4) | |
| Remote/very remote | 62 (2.2) | 14 (2.0) | 48 (2.3) | |
| Comorbidities | ||||
| Anxiety | 571 (20.3) | 121 (17.2) | 450 (21.4) | 0.017 |
| Arthritis | 641 (22.8) | 188 (26.7) | 453 (21.5) | 0.006 |
| Asthma | 454 (16.2) | 114 (16.2) | 340 (16.2) | 1.000 |
| COPD | 98 (3.5) | 34 (4.8) | 64 (3.0) | 0.032 |
| Depression | 692 (24.6) | 149 (21.1) | 543 (25.8) | 0.013 |
| Dementia | 4 (0.1) | 1 (0.1) | 3 (0.1) | 1.000 |
| CLD | 27 (1.0) | 3 (0.4) | 24 (1.1) | 0.118 |
| Cancer | 535 (19.0) | 145 (20.6) | 390 (18.5) | 0.430 |
| Anaemia Missing | 60 (3.3) 991 (35.3%) | 22 (4.8) 250 (35.5) | 38 (2.8) 741 (35.2) | 0.047 |
| CHD | 155 (5.5) | 50 (7.1) | 105 (5.0) | 0.036 |
| eGFR in mL/min | n = 1931 | n = 502 | n = 1429 | 0.305 |
| ≥60 | 1823 (94.4) | 468 (93.2) | 1355 (94.8) | |
| 45–59 | 84 (4.4) | 27 (5.4) | 57 (4.0) | |
| 30–44 | 15 (0.8) | 3 (0.6) | 12 (0.8) | |
| <30 | 9 (0.5) | 4 (0.8) | 5 (0.4) | |
| Missing | 879 (31.3) | 203 (28.8) | 676 (32.1) | |
| ORBIT Score, mean (SD) | 0.41 (0.60) | 0.37 (0.61) | 0.43 (0.59) | 0.021 |
| ORBIT risk category | 0.914 | |||
| Low | 2789 (99.3) | 699 (99.2) | 2090 (99.3) | |
| Medium | 18 (0.6) | 5 (0.7) | 13 (0.6) | |
| High | 3 (0.1) | 1 (0.1) | 2 (0.1) |
| Variables | Model 1 | Model 2 | ||
|---|---|---|---|---|
| AOR (95% CI) | p-Value | AOR (95% CI) | p-Value | |
| Sex | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | 0.72 (0.60–0.86) | <0.001 | 0.71 (0.59–0.85) | <0.001 |
| Age | 1.03 (1.02–1.04) | <0.001 | 1.03 (1.03–1.04) | <0.001 |
| Diagnosis period | ||||
| 2011–12 | Ref | Ref | Ref | Ref |
| 2013–14 | 1.17 (0.85–1.62) | 0.339 | 1.15 (0.83–1.58) | 0.402 |
| 2015–16 | 1.49 (1.12–1.98) | 0.006 | 1.46 (1.10–1.94) | 0.001 |
| 2017–18 | 1.65 (1.20–2.29) | 0.002 | 1.61 (1.17–2.23) | 0.004 |
| SEIFA quintile | ||||
| 1 | Ref | Ref | Ref | Ref |
| 2 | 0.65 (0.48–0.89) | 0.007 | 0.65 (0.48–0.88) | 0.006 |
| 3 | 0.75 (0.56–1.00) | 0.050 | 0.74 (0.56–0.98) | 0.034 |
| 4 | 0.70 (0.52–0.94) | 0.019 | 0.70 (0.52–0.94) | 0.018 |
| 5 | 0.70 (0.53–0.93) | 0.013 | 0.69 (0.52–0.91) | 0.009 |
| ORBIT score | 0.80 (0.68–0.93) | 0.005 | 0.80 (0.68–0.94) | 0.005 |
| Comorbidities | ||||
| Depression | 0.82 (0.66–1.01) | 0.067 | ||
| CLD | 0.26 (0.08–0.90) | 0.032 | ||
| COPD | 1.46 (0.94–2.26) | 0.096 | ||
| Types of Bleeding | OAC Users, n = 705 | OAC Non-Users, n = 2105 |
|---|---|---|
| Gastrointestinal bleeding | 3 | 14 |
| Urogenital bleeding | 7 | 10 |
| Haematoma | 3 | 4 |
| Subconjunctival haemorrhage | 1 | 3 |
| Intracranial haemorrhage | 1 | |
| Nasal bleeding | 2 | 1 |
| Anaemia secondary to blood loss | 1 | |
| Haemoptysis | 2 | |
| Total | 18 | 34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kefale, A.T.; Bezabhe, W.M.; Peterson, G.M. Oral Anticoagulant Use in Patients with Atrial Fibrillation at Low Risk of Stroke and Associated Bleeding Complications. J. Clin. Med. 2023, 12, 6182. https://doi.org/10.3390/jcm12196182
Kefale AT, Bezabhe WM, Peterson GM. Oral Anticoagulant Use in Patients with Atrial Fibrillation at Low Risk of Stroke and Associated Bleeding Complications. Journal of Clinical Medicine. 2023; 12(19):6182. https://doi.org/10.3390/jcm12196182
Chicago/Turabian StyleKefale, Adane Teshome, Woldesellassie M. Bezabhe, and Gregory M. Peterson. 2023. "Oral Anticoagulant Use in Patients with Atrial Fibrillation at Low Risk of Stroke and Associated Bleeding Complications" Journal of Clinical Medicine 12, no. 19: 6182. https://doi.org/10.3390/jcm12196182
APA StyleKefale, A. T., Bezabhe, W. M., & Peterson, G. M. (2023). Oral Anticoagulant Use in Patients with Atrial Fibrillation at Low Risk of Stroke and Associated Bleeding Complications. Journal of Clinical Medicine, 12(19), 6182. https://doi.org/10.3390/jcm12196182







