Comparison of McGrath Videolaryngoscope versus Macintosh Laryngoscope in Tracheal Intubation: An Updated Systematic Review
Abstract
:1. Introduction
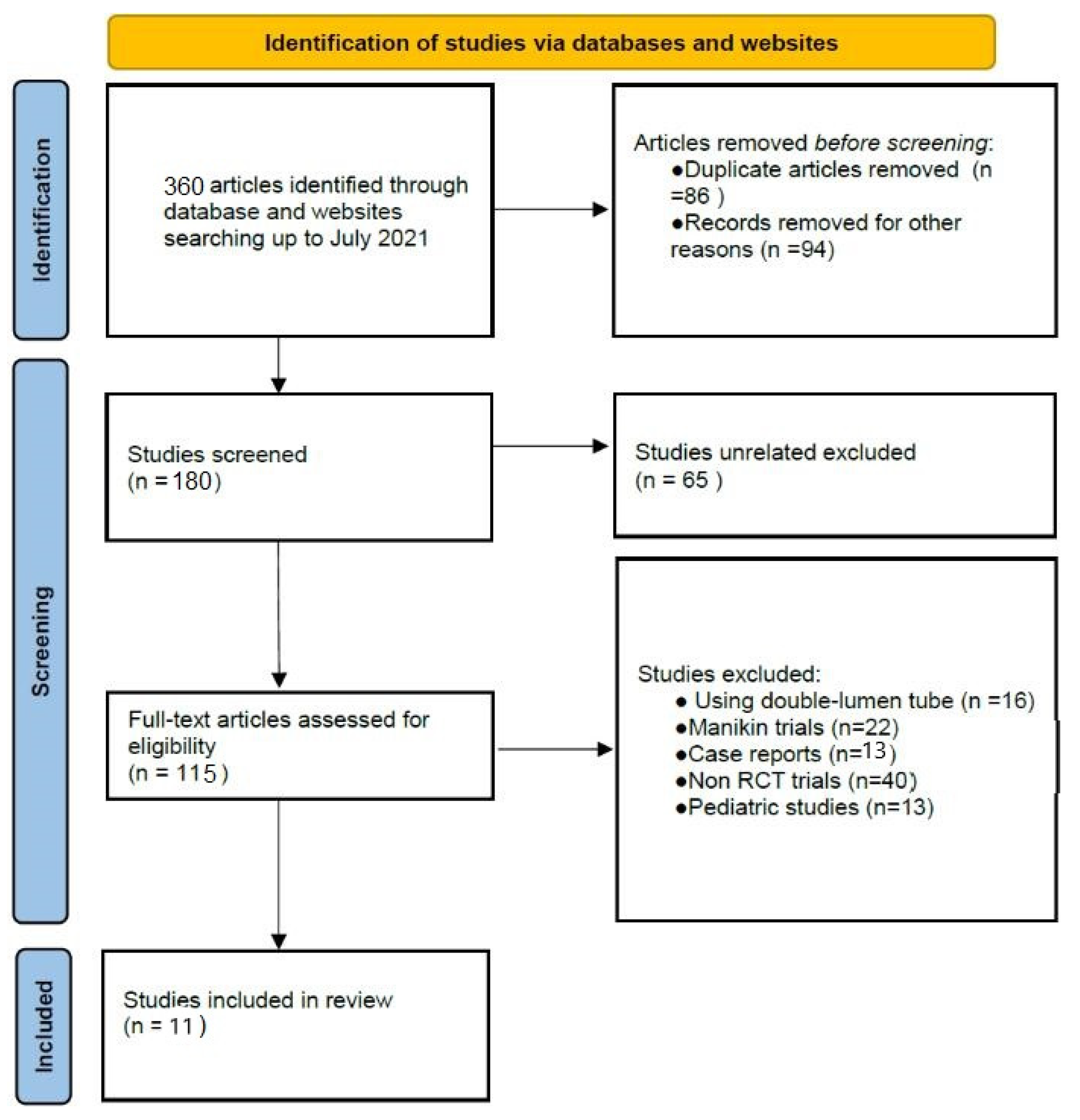
2. Materials and Methods
- 1.
- Number of participants involved in the study;
- 2.
- Age, sex and body mass index (BMI) of participants;
- 3.
- Type of operation;
- 4.
- ASA classifications;
- 5.
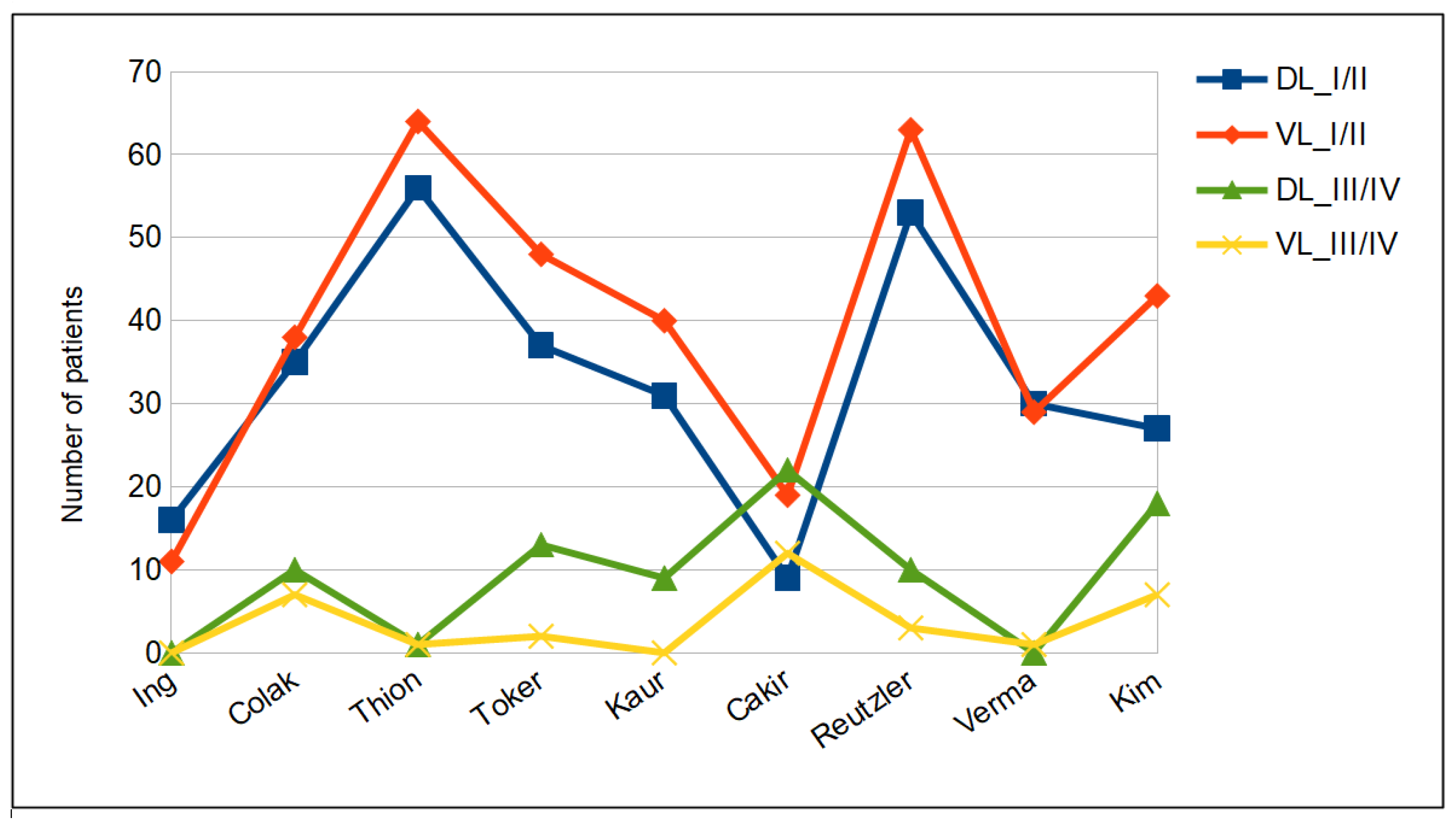
- Airway status, using Modified Mallampati score: class I—visualization of soft palate, uvula, fauces and pillars; class II—visualization of soft palate, major part of uvula and fauces; class III—visualization of soft palate and base of uvula; and class IV—visualization of hard palate.
- 6.
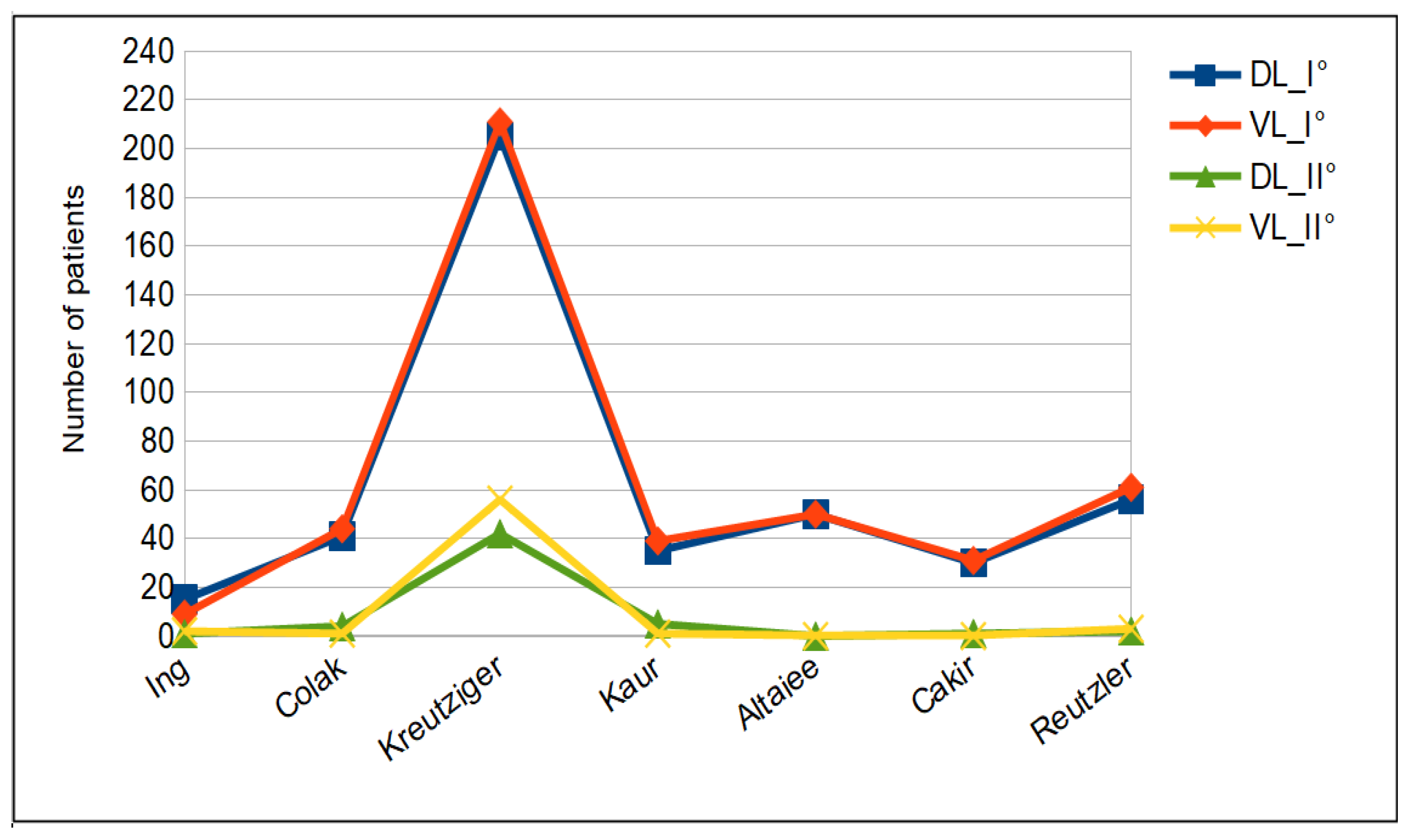
- Cormack and Lehane classification of glottic view: grade I—visualization of entire vocal cords; grade II—visualization of posterior part of the laryngeal aditus; grade III—visualization of epiglottis only; and grade IV—no glottic structures seen.
- 7.
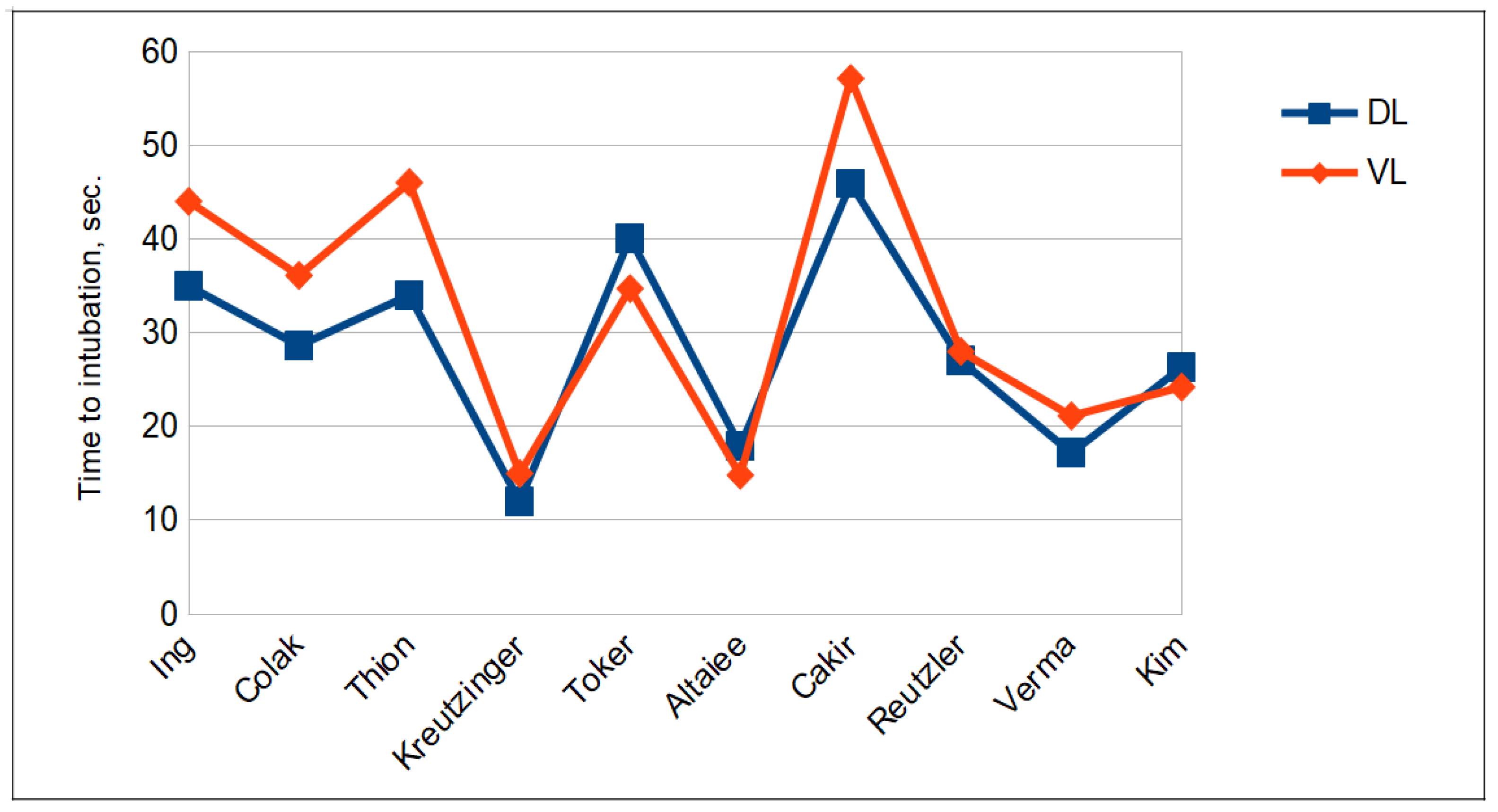
- Duration of intubation, defined as the time between placement of the endotracheal tube (ETT) between the dental arches and the appearance of the first capnographic curve.
- 8.
- Number of attempts. Each attempt corresponded to the time between the introduction of the laryngoscope into the oral cavity and its removal. Intubation failure was defined as the inability to intubate after three attempts. In the case of failure, an alternative technique was used at the discretion of the anesthesiologist.
- 9.
- Number and type of optimization maneuvers, like the use of a bougie, cricoid pressure and a second assistant, were recorded.
- 10.
- Hemodynamic changes, considering the change in heart rate (HR) and blood pressure (BP) before and after intubation.
- 11.
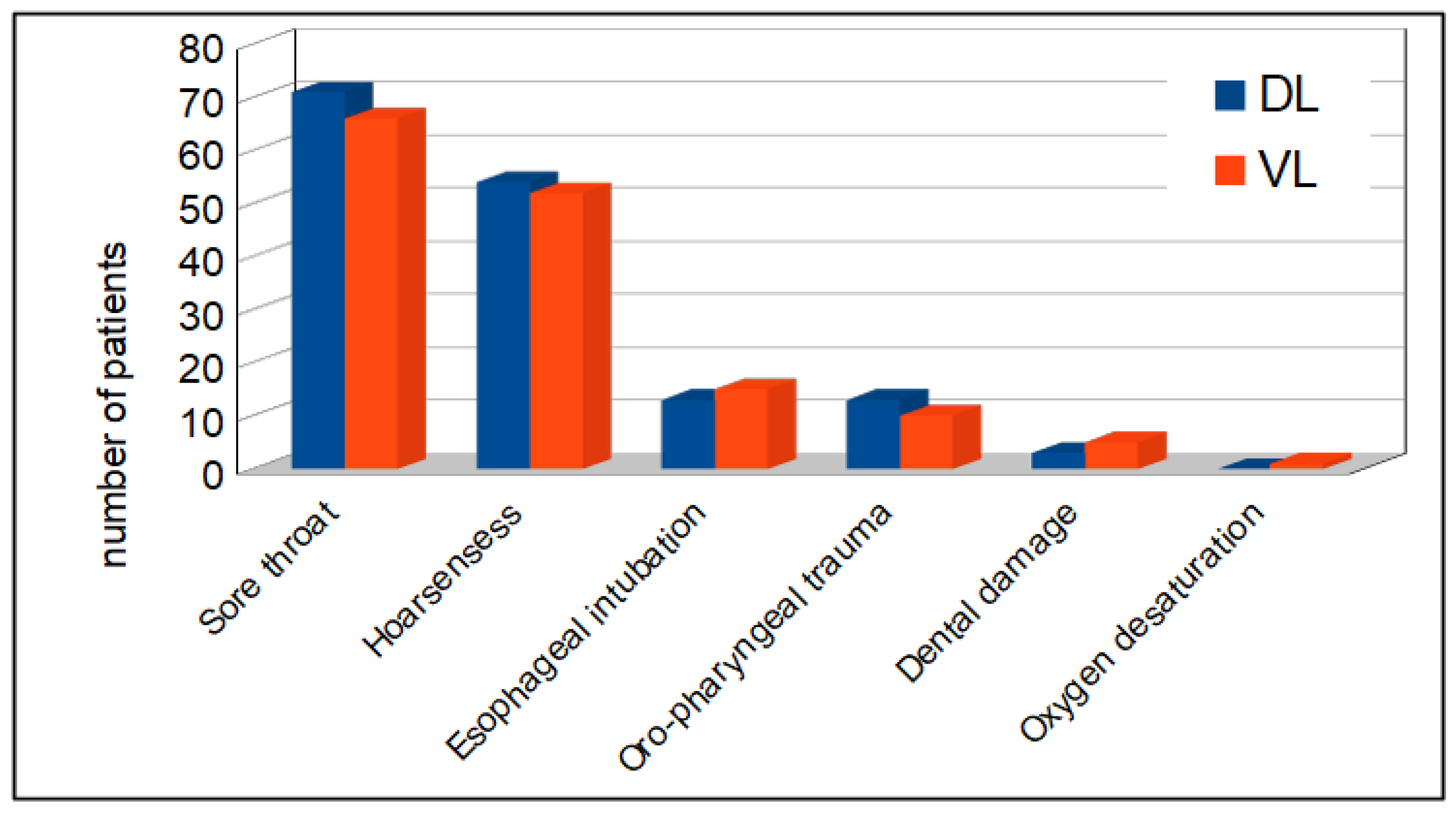
- Adverse events (AEs), such as oxygen desaturation, dental damage, oro-pharyngeal trauma, esophageal intubation, postoperative hoarseness and postoperative sore throat.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Taylor, A.M.; Peck, M.; Launcelott, S.; Hung, O.R.; Law, J.A.; MacQuarrie, K.; McKeen, D.; George, R.B.; Ngan, J. The McGrath® series 5 videolaryngoscope vs Macintosh laryngoscope: A randomised, controlled trial in patients with a simulated difficult airway. Anesthesia 2013, 68, 142–147. [Google Scholar] [CrossRef]
- Ng, I.; Sim, X.L.; Williams, D.; Segal, R. A randomised controlled trial comparing the McGrath® videolaryngoscope with the straight blade laryngoscope when used in adult patients with potential difficult airways. Anesthesia 2011, 66, 709–714. [Google Scholar] [CrossRef]
- Sargin, M.; Uluer, M.S. Comparison of McGrath® serie 5 video laryngoscope with Macintosh laryngoscope: A prospective, randomised trial in patients with normal airways. Pak. J. Med. Sci. 2016, 32, 869–874. [Google Scholar]
- Frohlich, S.; Borovickova, L.; Foley, E.; O’Sullivan, E. A comparison of tracheal intubation using the McGrath or the Macintosh laryngoscopes in routine airway management. Eur. J. Anaesthesiol. 2011, 28, 465–467. [Google Scholar] [CrossRef]
- Kwak, H.J.; Lee, S.Y.; Cho, S.H.; Kim, H.S.; Kim, J.Y. McGrath video laryngoscopy facilitates routine nasotracheal intubation in patients undergoing oral and maxillofacial surgery: A comparison with Macintosh laryngoscopy. J. Oral. Maxillofac. Surg. 2016, 74, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Ilyas, S.; Symons, J.; Bradley, W.P.L.; Segal, R.; Taylor, H.; Lee, K.; Balkin, M.; Bain, C.; Ng, I. A prospective randomised controlled trial comparing tracheal intubation plus manual in-line stabilisation of the cervicale spine using the Macintosh laryngoscope vs the McGrath® series 5 videolaryngoscope. Anaesthesia 2014, 69, 1345–1350. [Google Scholar] [CrossRef] [PubMed]
- Arici, S.; Karaman, S.; Doğru, S.; Karaman, T.; Tapar, H.; Özsoy, A.Z.; Kaya, Z.; Süren, M. The McGrath series 5 videolaryngoscope versus the Macintosh laryngoscope: A randomised trial in obstetric patient. Turj. J. Med. Sci. 2014, 44, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.J.; Guo, W.J.; Ma, C.; Huang, Y.G. Comparison of McGrath series 3 and Macintosh laryngoscopes for tracheal intubation in patients with normal airway by inexeperienced anesthetists: A randomized study. Medicine 2016, 95, e2514. [Google Scholar] [CrossRef]
- Wallace, C.D.; Foulds, L.T.; McLeod, G.A.; Younger, R.A.; McGuire, B.E. A comparison of the ease of tracheal intubation using a McGrath MAC® laryngoscope and a standard Macintosh laryngoscope. Anaesthesia 2015, 70, 1281–1285. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.; Brampton, W.; Halai, M.; Hoy, C.; Lee, E.; Scott, I.; McLernon, D. Randomized controlled trial of intubation with the McGrath series 5 videolaryngoscope by inexperienced anaesthetists. Br. J. Anaesth. 2009, 103, 440–445. [Google Scholar] [CrossRef]
- Foulds, L.T.; McGuire, B.E.; Shippey, B.J. A randomised cross-over trial comparing the McGrath® series 5 videolaryngoscope with the Macintosh laryngoscope in patients with cervical spine immobilisation. Anaesthesia 2016, 71, 437–442. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews andMeta-Analyses: The PRISMA Statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Hoshijima, H.; Mihara, T.; Maruyama, K.; Denawa, Y.; Takahashi, M.; Shiga, T.; Nagasaka, H. McGrath videolaryngoscope versus Macintosh laryngoscope for tracheal intubation: A systematic review and meta-analysis with trial sequential analysis. J. Clin. Anesth. 2018, 46, 25–32. [Google Scholar] [CrossRef]
- Ing, R.; Liu, N.; Chazot, T.; Fessler, J.; Dreyfus, J.F.; Fischler, M.; Le Guen, M. Nociceptive stimulation during Macintosh direct laryngoscopy compared with McGrath Mac videolaryngoscopy: A randomized trial using indirect evaluation using an automated administration of propofol and remifentanil. Medicine 2017, 96, e8087. [Google Scholar] [CrossRef]
- Colak, F.; Ozgul, U.; Erdogan, M.A.; Kayhan, G.E.; Erdil, F.A.; Colak, C.; Durmus, M. Comparison of hemodinamic responses and QTc intervals to tracheal intubation with the McGRATH MAC videolaryngoscope and Macintosh direct laryngoscope in elderly patients. Kaohsiung J. Med. Sci. 2019, 35, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Thion, L.A.; Belze, O.; Fischler, M.; Le Guen, M. Comparison of the ease of tracheal intubation using a McGrath Mac videolaryngoscope and a standard Macintosh laryngoscope in normal airways: A randomised trial. Eur. J. Anaesthesiol. 2018, 35, 631–633. [Google Scholar] [CrossRef] [PubMed]
- Kreutziger, J.; Hornung, S.; Urschl, W.; Doppler, R.; GVoelckel, W.; Trimmel, H. Comparing the McGrath Mac Video Laryngoscope and Direct Laryngoscopy for Prehospital Emergency Intubation in Air Rescue Patients: A Multicenter, Randomized, Controlled Trial. Crit. Care Med. 2019, 47, 1362–1370. [Google Scholar] [CrossRef] [PubMed]
- Toker, M.K.; Altıparmak, B.; Karabay, A.G. Comparison of the McGrath video laryngoscope and macintosh direct laryngoscope in obstetric patients: A randomized controlled trial. Pak. J. Med. Sci. 2019, 35, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Kaur, G.; Gupta, S.; Metha, N.; Dhingra, J.S. Comparative Evaluation of McGrath MAC, Truview Video Laryngoscopes and Macintosh Laryngoscope for Endotracheal Intubation in Patients Undergoing Surgery under General Anaesthesia. Anesth. Essays Res. 2020, 14, 20–24. [Google Scholar]
- Altaiee, A.H.; Hassen, H.A.; Fadeel, S.J. Video laryngoscopy versus direct laryngoscopy on time of orotracheal intubation in normal adult in elective surgeries. Med. Sci. 2020, 24, 4264–4269. [Google Scholar]
- Çakir, M.; Özyurt, E. Comparison of direct laryngoscope and McGrath videolaryngoscope in terms of glottic view and hemodynamics in bariatric surgery. Turk. J. Med. Sci. 2020, 50, 213–218. [Google Scholar]
- Ruetzler, K.; Rivas, E.; Cohen, B.; Mosteller, L.; Martin, A.; Keebler, A.; Maheshwari, K.; Steckner, K.; Wang, M.; Praveen, C.; et al. McGrath Video Laryngoscope Versus Macintosh Direct Laryngoscopy for Intubation of Morbidly Obese Patients: A Randomized Trial. Anesth. Analg. 2020, 131, 586–593. [Google Scholar] [CrossRef]
- Verma, I.; Verma, C.; Dhaked, S.; Sharma, R. A Randomised Comparative Interventional Prospective Study of Intubation by Macintosh Laryngoscope Versus McGrath Video Laryngoscope in Patients Undergoing Cardiac Surgery. Anesth. Crit. Care 2020, 2, 052–065. [Google Scholar] [CrossRef]
- Kim, J.Y.; Park, S.; Oh, M.; Choi, J.B.; John, H.J.; Lee, S.K.; Choi, Y.H. Comparison of the McGRATHTM Video Laryngoscope and Macintosh Laryngoscope for Orotracheal Intubation in a Simulated Difficult Airway Scenario: An Open-Label, Randomized Clinical Trial. Medicina 2023, 59, 282. [Google Scholar] [CrossRef] [PubMed]
- Singhal, S.K.; Kaur, K.; Yadav, P. A study to evaluate the role of experience in acquisition of the skill of orotracheal intubation in adults. J. Anaesthesiol. Clin. Pharmacol. 2021, 37, 469–474. [Google Scholar] [PubMed]
- Aziz, M.F.; Abrons, R.O.; Cattano, D.; Bayman, E.O.; Swanson, D.E.; Hagberg, C.A.; Todd, M.M.; Brambrink, A.M. First-attempt intubation success of video laryngoscopy in patients with anticipated difficult direct laryngoscopy: A multicenter randomized controlled trial comparing the C-MAC D-blade versus the GlideScope in a mixed provider and diverse patient population. Anesth. Analg. 2016, 122, 740–750. [Google Scholar] [PubMed]
- Sulser, S.; Ubmann, D.; Schlaepfer, M.; Brueesch, M.; Goliasch, G.; Seifert, B.; Spahn, D.R.; Ruetzler, K. C-MAC videolaryngoscope compared with direct laryngoscopy for rapid sequence intubation in an emergency department: A randomised clinical trial. Eur. J. Anaesthesiol. 2016, 33, 943–948. [Google Scholar] [CrossRef] [PubMed]
- Ruetzler, K.; Imach, S.; Weiss, M.; Haas, T.; Schmidt, A.R. Comparison of five video laryngoscopes and conventional direct laryngoscopy: Investigations on simple and simulated difficult airways on the intubation trainer. Anaesthesist 2015, 64, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Lascarrou, J.B.; Boisrame-Helms, J.; Bailly, A.; Le Thuaut, A.; Kamel, T.; Mercier, E.; Ricard, J.D.; Lemiale, V.; Colin, G.; Mira, J.P.; et al. Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation Among ICU Patients: A Randomized Clinical Trial. JAMA 2017, 317, 483–493. [Google Scholar] [CrossRef]
| Population | Patients of at least 18 years undergoing general anesthesia. |
| Intervention | Tracheal intubation using the McGRATH™ MAC videolaryngoscope. |
| Comparator | Tracheal intubation using the Macintosh laryngoscope. |
| Outcomes | Rate of successful tracheal intubation, the duration of the intubation maneuvers, the number of attempts, the need for external maneuvers or other alternative techniques, the hemodynamic changes and the incidence of adverse events. |
| Study type | Randomized controlled trials (RCTs). |
| Time | From September 2017 to February 2023. |
| Year | N° of Patients (DL/VL) | Type of Surgery | |
|---|---|---|---|
| Ing et al. [14] | 2017 | 27 (16/11) | Elective surgery |
| Colak et al. [15] | 2018 | 90 (45/45) | Elective surgery |
| Thion et al. [16] | 2018 | 122 (57/65) | Elective surgery |
| Kreutziger et al. [17] | 2019 | 514 (247/267) | Emergency |
| Toker et al. [18] | 2019 | 100 (50/50) | Elective cesarean section |
| Kaur et al. [19] | 2020 | 80 (40/40) | Elective surgery |
| Altaiee et al. [20] | 2020 | 100 (50/50) | Elective surgery |
| Çakir et al. [21] | 2020 | 62 (31/31) | Elective bariatric surgery |
| Ruetzler et al. [22] | 2020 | 129 (63/66) | Elective surgery |
| Verma et al. [23] | 2020 | 60 (30/30) | Elective cardiac surgery |
| Kim et al. [24] | 2023 | 95 (50/45) | Elective surgery |
| KERRYPNX | DL | VL |
|---|---|---|
| Male/Female | 323/304 | 328/307 |
| Age (years) | 47.3 ± 13.4 | 48.4 ± 14.1 |
| BMI (kg/m2) | 30.3 ± 10.4 | 30.4 ± 10.0 |
| Mallampati | ||
| – I | 124 | 122 |
| – II | 79 | 87 |
| – III | 59 | 52 |
| – IV | 6 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sansone, P.; Giaccari, L.G.; Bonomo, A.; Gargano, F.; Aurilio, C.; Coppolino, F.; Passavanti, M.B.; Pota, V.; Pace, M.C. Comparison of McGrath Videolaryngoscope versus Macintosh Laryngoscope in Tracheal Intubation: An Updated Systematic Review. J. Clin. Med. 2023, 12, 6168. https://doi.org/10.3390/jcm12196168
Sansone P, Giaccari LG, Bonomo A, Gargano F, Aurilio C, Coppolino F, Passavanti MB, Pota V, Pace MC. Comparison of McGrath Videolaryngoscope versus Macintosh Laryngoscope in Tracheal Intubation: An Updated Systematic Review. Journal of Clinical Medicine. 2023; 12(19):6168. https://doi.org/10.3390/jcm12196168
Chicago/Turabian StyleSansone, Pasquale, Luca Gregorio Giaccari, Antonio Bonomo, Francesca Gargano, Caterina Aurilio, Francesco Coppolino, Maria Beatrice Passavanti, Vincenzo Pota, and Maria Caterina Pace. 2023. "Comparison of McGrath Videolaryngoscope versus Macintosh Laryngoscope in Tracheal Intubation: An Updated Systematic Review" Journal of Clinical Medicine 12, no. 19: 6168. https://doi.org/10.3390/jcm12196168
APA StyleSansone, P., Giaccari, L. G., Bonomo, A., Gargano, F., Aurilio, C., Coppolino, F., Passavanti, M. B., Pota, V., & Pace, M. C. (2023). Comparison of McGrath Videolaryngoscope versus Macintosh Laryngoscope in Tracheal Intubation: An Updated Systematic Review. Journal of Clinical Medicine, 12(19), 6168. https://doi.org/10.3390/jcm12196168











