Sex Differences in the Diagnosis, Management, and Outcomes of Suspected Non-ST-Elevation Acute Coronary Syndromes Meeting Rapid Rule-Out Criteria
Abstract
:1. Introduction
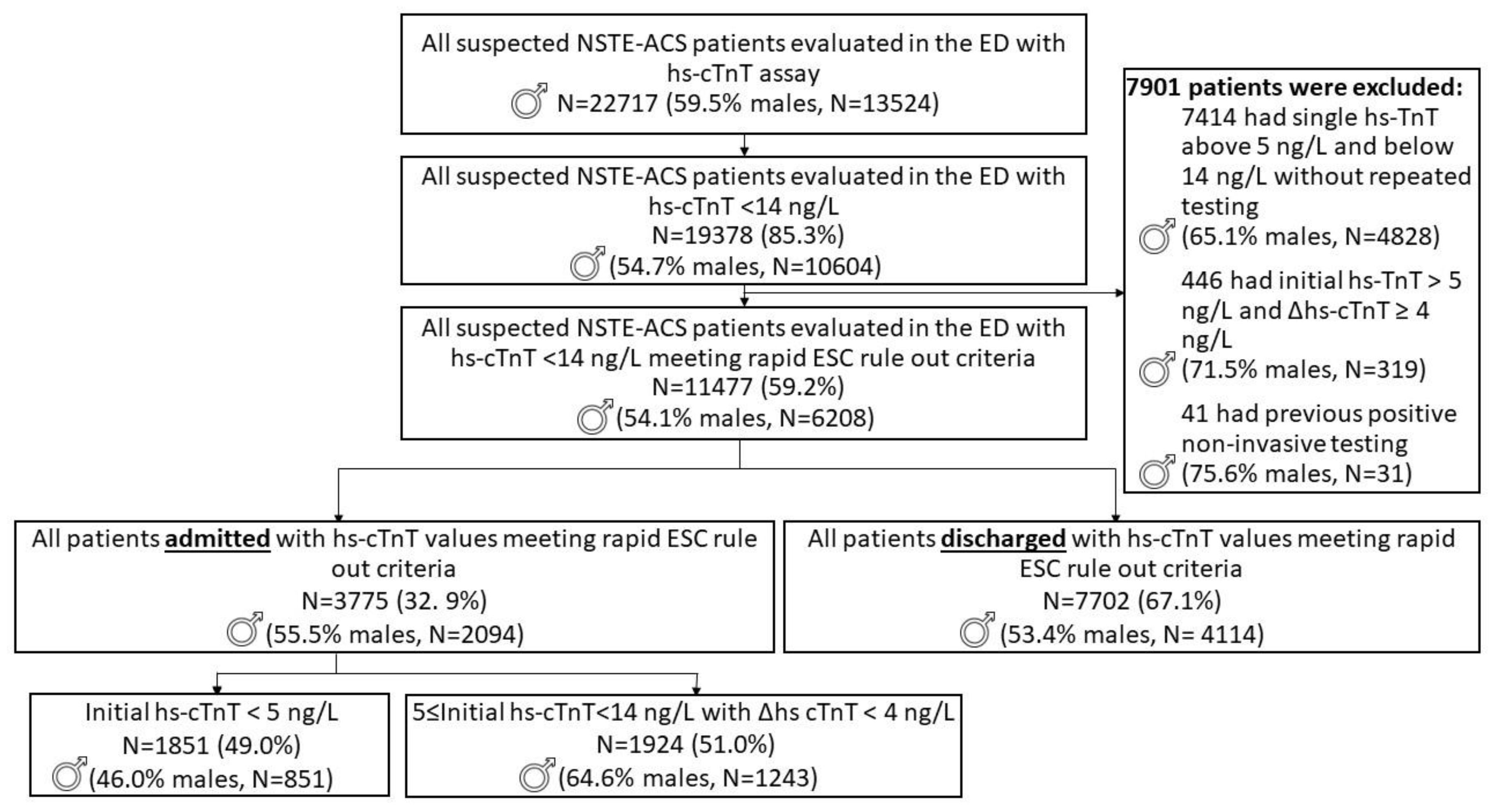
2. Materials and Methods
2.1. Study End Points
2.2. Statistical Analysis
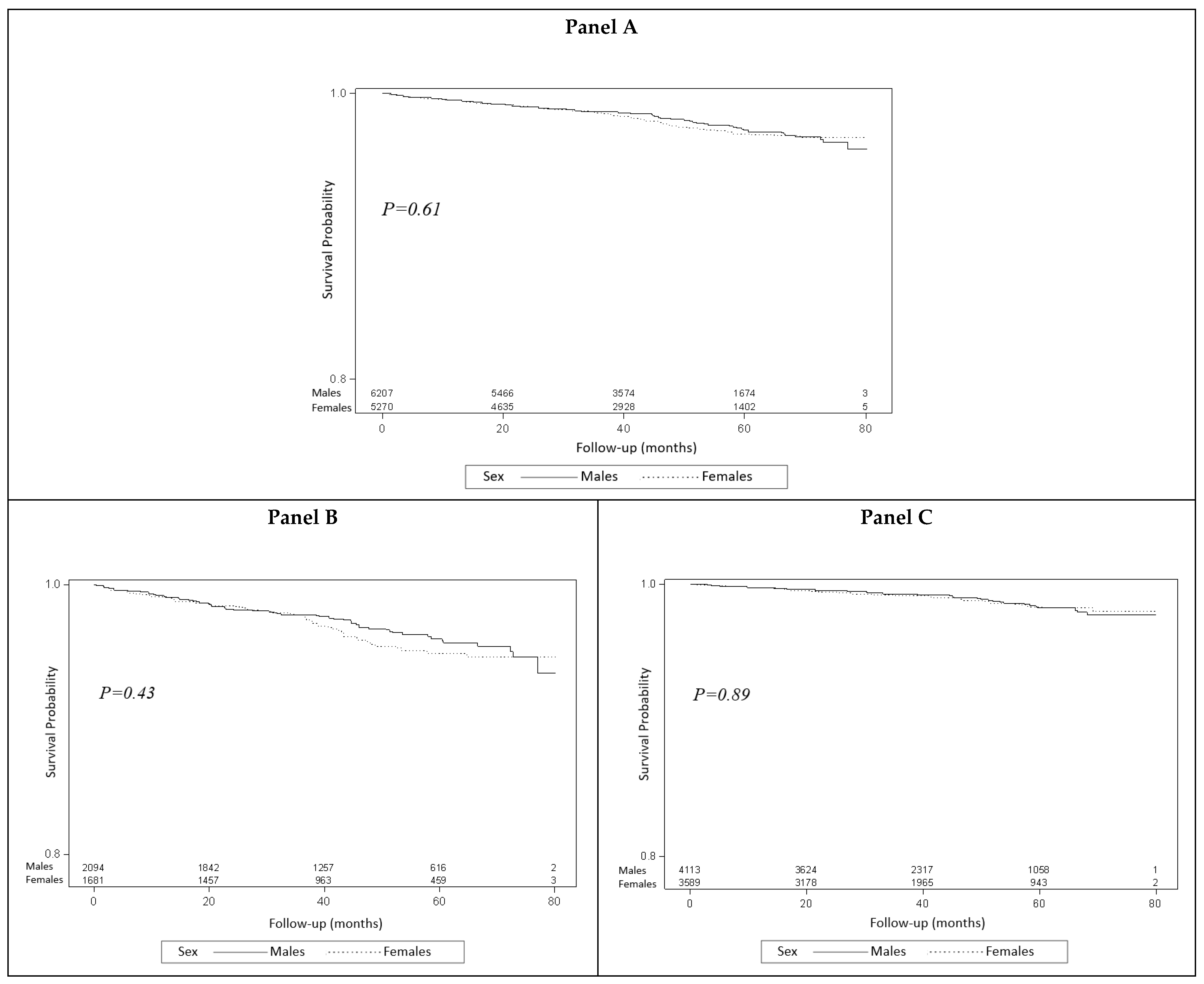
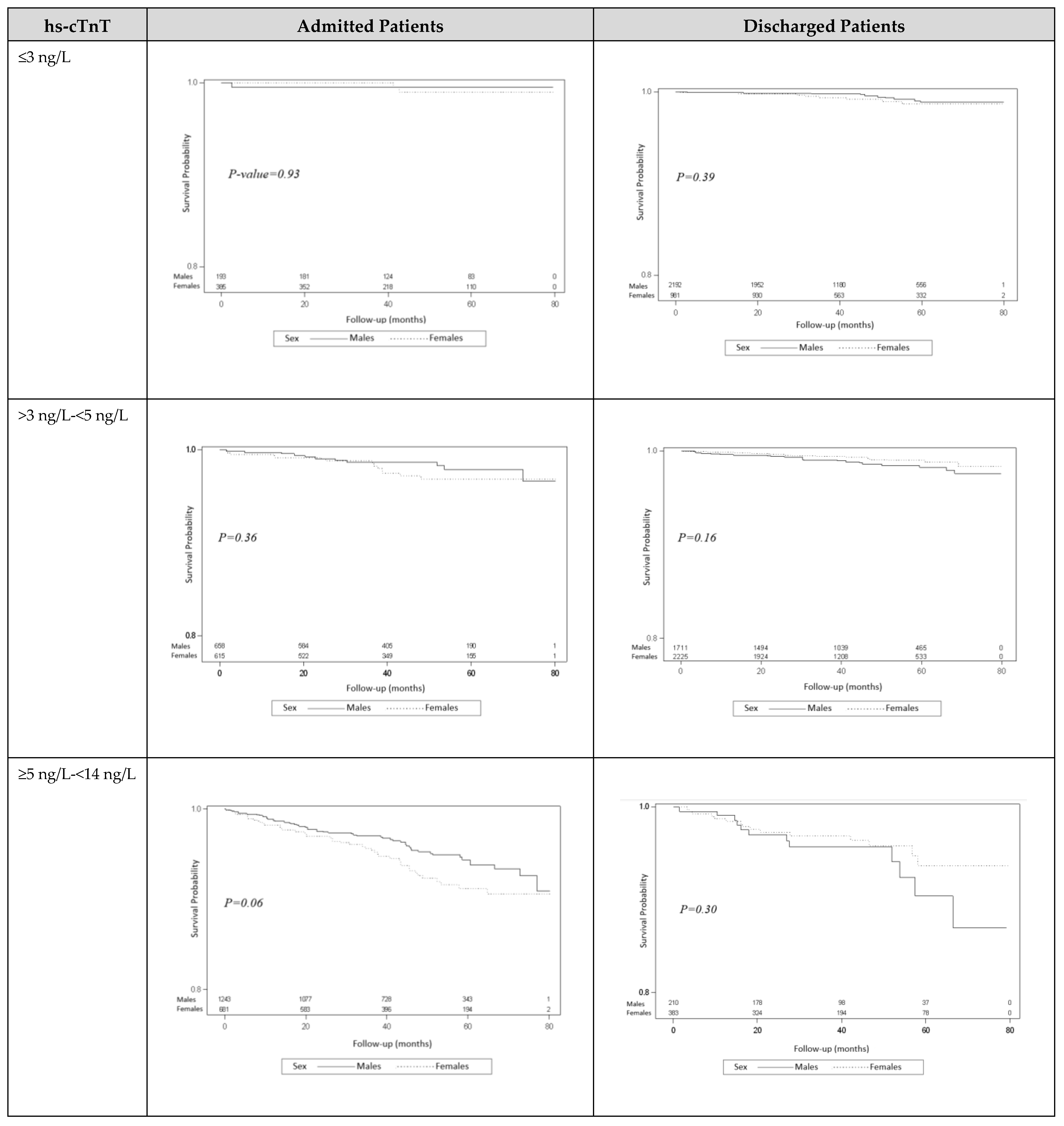
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Langabeer, J.R.; Champagne-Langabeer, T.; Fowler, R.; Henry, T. Gender-based outcome differences for emergency department presentation ofnon-STEMI acute coronary syndrome. Am. J. Emerg. Med. 2019, 37, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Bergström, G.; Persson, M.; Adiels, M.; Björnson, E.; Bonander, C.; Ahlström, H.; Alfredsson, J.; Angerås, O.; Berglund, G.; Blomberg, A.; et al. Prevalence of Subclinical Coronary Artery Atherosclerosis in the General Population. Circulation 2021, 144, 916–929. [Google Scholar] [CrossRef] [PubMed]
- Bugiardini, R.; Estrada, J.L.N.; Nikus, K.; Hall, A.S.; Manfrini, O. Gender bias in acute coronary syndromes. Curr. Vasc. Pharmacol. 2010, 8, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Hvelplund, A.; Galatius, S.; Madsen, M.; Rasmussen, J.N.; Rasmussen, S.; Madsen, J.K.; Sand, N.P.; Tilsted, H.-H.; Thayssen, P.; Sindby, E.; et al. Women with acute coronary syndrome are less invasively examined and subsequently less treated than men. Eur. Heart J. 2010, 31, 684–690. [Google Scholar] [CrossRef] [PubMed]
- Gudnadottir, G.S.; Andersen, K.; Thrainsdottir, I.S.; James, S.K.; Lagerqvist, B.; Gudnason, T. Gender differences in coronary angiography, subsequent interventions, and outcomes among patients with acute coronary syndromes. Am. Heart J. 2017, 191, 65–74. [Google Scholar] [CrossRef] [PubMed]
- de Lemos, J.A. Increasingly sensitive assays for cardiac troponins: A review. JAMA 2013, 309, 2262–2269. [Google Scholar] [CrossRef] [PubMed]
- Mueller-Hennessen, M.; Lindahl, B.; Giannitsis, E.; Biener, M.; Vafaie, M.; de Filippi, C.R.; Christ, M.; Santalo-Bel, M.; Panteghini, M.; Plebani, M.; et al. Diagnostic and prognostic implications using age- and gender-specific cut-offs for high-sensitivity cardiac troponin T-Sub-analysis from the TRAPID-AMI study. Int. J. Cardiol. 2016, 209, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Boeddinghaus, J.; Nestelberger, T.; Twerenbold, R.; Wildi, K.; Badertscher, P.; Cupa, J.; Bürge, T.; Mächler, P.; Corbière, S.; Grimm, K.; et al. Direct Comparison of 4 Very Early Rule-Out Strategies for Acute Myocardial Infarction Using High-Sensitivity Cardiac Troponin, I. Circulation 2017, 135, 1597–1611. [Google Scholar] [CrossRef]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; Casey, D.E.; Ganiats, T.G.; Holmes, D.R.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.; et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 64, e139–e228. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef] [PubMed]
- Cohen, B.; Cohen, S.; Tor, R.; Shochat, T.; Fuchs, S.; Kornowski, R.; Grossman, A.; Hasdai, D. Suspected Non-ST-elevation acute coronary syndrome meeting rapid rule-out criteria: Resource utilization, diagnostic yield, and clinical outcomes of hospital admission. Eur. Heart J. Qual. Care Clin. Outcomes 2023, 9, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Romiti, G.F.; Cangemi, R.; Toriello, F.; Ruscio, E.; Sciomer, S.; Moscucci, F.; Vincenti, M.; Crescioli, C.; Proietti, M.; Basili, S.; et al. Sex-Specific Cut-Offs for High-Sensitivity Cardiac Troponin: Is Less More? Cardiovasc. Ther. 2019, 2019, 9546931. [Google Scholar] [CrossRef] [PubMed]
- Schofer, N.; Brunner, F.J.; Schlüter, M.; Ojeda, F.; Zeller, T.; Baldus, S.; Bickel, C.; Lackner, K.J.; Münzel, T.; Tzikas, S.; et al. Gender-specific diagnostic performance of a new high-sensitivity cardiac troponin I assay for detection of acute myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 2017, 6, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Huai, W.; Qiao, R.; Cui, L.; Liu, G.; Wu, J.; Li, A.; Zhang, J. Age and Gender Tailored Cutoff Value of hs-cTnT Contributes to Rapidly Diagnose Acute Myocardial Infarction in Chest Pain Patients. Clin. Lab. 2016, 62, 1451–1459. [Google Scholar] [CrossRef] [PubMed]
| Initial hs-cTnT | Patients, N | Females | Males | ||
|---|---|---|---|---|---|
| Discharge, N (%) | Admission, N (%) | Discharge, N (%) | Admission, N (%) | ||
| ≤3 ng/L | 3751 | 981 (27.3) | 385 (22.9) | 2192 (53.3) | 193 (9.2) |
| >3 ng/L–<5 ng/L | 5209 | 2224 (62.0) | 615 (36.6) | 1711 (41.6) | 658 (31.4) |
| ≥5 ng/L–<14 ng/L | 2517 | 383 (10.7) | 681 (40.5) | 210 (5.1) | 1243 (59.4) |
| All | 11,477 | 3588 | 1681 | 4113 | 2094 |
| All Admitted Females (N = 1681) | All Discharged Females (N = 3588) | All Admitted Males (N = 2094) | All Discharged Males (N = 4113) | |
|---|---|---|---|---|
| Age (years) | 61 (52–70) | 39 (31–48) | 56 (47–65) | 44 (33–55) |
| Laboratory | ||||
| hs-cTnT ≤3 ng/L (N, %) | 385 (22.9) | 981 (27.3) | 193 (9.2) | 2192 (53.3) |
| hs-cTnT >3 ng/L–<5 ng/L (N, %) | 615 (36.6) | 2224 (62.0) | 658 (31.4) | 1711 (41.6) |
| hs-cTnT ≥5 ng/L–<14 ng/L (N, %) | 681 (40.5) | 383 (10.7) | 1243 (59.4) | 210 (5.1) |
| Hs-cTnT increment above 4 ng/L in first 24 h (N, %) | 21 (1.3) | 17 (0.5) | 44 (2.1) | 12 (0.3) |
| ≥2 hs-cTnT tests performed (N, %) | 1091 (64.9) | 690 (19.2) | 1707 (81.5) | 430 (10.5) |
| Max hs-cTnT value in first 24 h above the 99th percentile (N, %) | 54 (3.2) | 12 (0.3) | 124 (5.9) | 9 (0.2) |
| Creatinine (mg/dL) | 0.73 (0.6–0.8) | 0.9 (0.8–1.0) | 0.92 (0.8–1.0) | 0.7 (0.6–0.8) |
| CRP (mg/dL) | 0.38 (0.2–0.9) | 0.27 (0.1–0.6) | 0.31 (0.2–0.7) | 0.36 (0.2–0.8) |
| LDH (U/L) | 382.0 (337.0–445.0) | 356 (317–406) | 355.0 (314.0–406.0) | 356 (310–410) |
| WBC (K/uL) | 7.8 (6.4–9.5) | 8.1 (6.7–9.7) | 8.2 (6.8–9.8) | 7.9 (6.5–9.5) |
| Hemoglobin (gr/dL) | 13.1 (12.2–13.8) | 14.9 (14.2–15.6) | 14.6 (13.7–15.4) | 13.1 (12.3–13.7) |
| Vital Signs | ||||
| SBP (mm Hg) | 138 (123–152) | 130 (120–140) | 135 (125–149) | 126 (115–139) |
| DBP (mm Hg) | 78 (70–87) | 80 (73–89) | 82 (74–90) | 77 (69–85) |
| Oxygen Saturation (%) | 99 (97–100) | 99 (99–99) | 98 (97–100) | 99.5 (97–100) |
| Temperature (°C) | 36.6 (36.5–36.8) | 36.3 (36.3–36.3) | 36.6 (36.5–36.8) | 36.6 (36.5–36.7) |
| Pulse (beats/min) | 77 (68–87) | 78 (68–87) | 76 (66–86) | 80 (71–89) |
| Past Medical History * | ||||
| Hypertension (N, %) | 458 (27.3) | 56 (1.6) | 534 (25.5) | 133 (3.2) |
| Diabetes Mellitus (N, %) | 253 (15.1) | 36 (1.0) | 272 (13.0) | 77 (1.9) |
| Dyslipidemia (N, %) | 438 (26.1) | 79 (2.2) | 585 (27.9) | 130 (3.2) |
| Atrial Fibrillation (N, %) | 77 (4.6) | 8 (0.2) | 69 (3.3) | 11 (0.3) |
| Hypothyroidism (N, %) | 132 (7.9) | 6 (0.2) | 37 (1.8) | 98 (2.4) |
| Heart Failure (N, %) | 16 (1.0) | 1 (0.03) | 18 (0.9) | 4 (0.1) |
| Ischemic Heart Disease (N, %) | 148 (8.8) | 43 (1.2) | 341 (16.3) | 29 (0.7) |
| Smoking (N, %) | 82 (4.9) | 54 (1.5) | 251 (12.0) | 18 (0.4) |
| All Admitted Males (N = 2094) | All Admitted Females (N = 1681) | |||||
|---|---|---|---|---|---|---|
| ≤3 ng/L | >3 ng/L–<5 ng/L | ≥5 ng/L–<14 ng/L | ≤3 ng/L | >3 ng/L–<5 ng/L | ≥5 ng/L–<14 ng/L | |
| N = 193 | N = 658 | N = 1243 | N = 385 | N = 615 | N = 681 | |
| Primary Outcomes | ||||||
| Myocardial Infarction (N, %) | 1 (0.5) | 3 (0.5) | 5 (0.4) | 0 (0) | 0 (0) | 1 (0.2) |
| In-hospital Death (N, %) | 0 (0) | 0 (0) | 1 (0.1) | 0 (0) | 0 (0) | 1 (0.2) |
| 30-day Mortality (N, %) | 0 (0) | 0 (0) | 1 (0.1) | 0 (0) | 0 (0) | 1 (0.2) |
| Combined Primary Outcome (N, %) | 1 (0.5) | 3 (0.5) | 6 (0.5) | 0 (0) | 0 (0) | 2 (0.3) |
| Resource Utilization | ||||||
| Emergency Department Stay (hours) | 5 (3.07–6.37) | 6 (4–7) | 5 (4–7) | 6 (4–7) | 5 (4–7) | 6 (4–7) |
| Hospital Stay (days) | 4 (2–5) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) |
| Electrocardiogram Treadmill Test (N, %) | 19 (9.8) | 32 (4.9) | 32 (2.6) | 15 (3.9) | 9 (1.5) | 3 (0.4) |
| Radionuclide Test (N, %) | 10 (5.2) | 69 (10.5) | 204 (16.4) | 24 (6.2) | 72 (11.7) | 129 (18.9) |
| Cardiac Computerized Tomography Angiography (N, %) | 63 (32.6) | 193 (29.3) | 178 (14.3) | 123 (32.0) | 168 (27.3) | 96 (14.1) |
| Coronary Angiography (N, %) | 8 (4.2) | 34 (5.2) | 100 (8.1) | 6 (1.6) | 18 (2.9) | 25 (3.7) |
| Coronary Revascularization (N, %) | 2 (1.0) | 28 (4.3) | 41 (3.3) | 1 (0.3) | 10 (1.6) | 8 (1.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cohen, B.; Tor, R.; Grossman, A.; Kornowski, R.; Porter, A.; Hasdai, D. Sex Differences in the Diagnosis, Management, and Outcomes of Suspected Non-ST-Elevation Acute Coronary Syndromes Meeting Rapid Rule-Out Criteria. J. Clin. Med. 2023, 12, 5704. https://doi.org/10.3390/jcm12175704
Cohen B, Tor R, Grossman A, Kornowski R, Porter A, Hasdai D. Sex Differences in the Diagnosis, Management, and Outcomes of Suspected Non-ST-Elevation Acute Coronary Syndromes Meeting Rapid Rule-Out Criteria. Journal of Clinical Medicine. 2023; 12(17):5704. https://doi.org/10.3390/jcm12175704
Chicago/Turabian StyleCohen, Ben, Ruth Tor, Alon Grossman, Ran Kornowski, Avital Porter, and David Hasdai. 2023. "Sex Differences in the Diagnosis, Management, and Outcomes of Suspected Non-ST-Elevation Acute Coronary Syndromes Meeting Rapid Rule-Out Criteria" Journal of Clinical Medicine 12, no. 17: 5704. https://doi.org/10.3390/jcm12175704
APA StyleCohen, B., Tor, R., Grossman, A., Kornowski, R., Porter, A., & Hasdai, D. (2023). Sex Differences in the Diagnosis, Management, and Outcomes of Suspected Non-ST-Elevation Acute Coronary Syndromes Meeting Rapid Rule-Out Criteria. Journal of Clinical Medicine, 12(17), 5704. https://doi.org/10.3390/jcm12175704







