The Risk of Retinal Vein Occlusion in Young Patients with Mental Disorders: A Nationwide Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Source of the Database
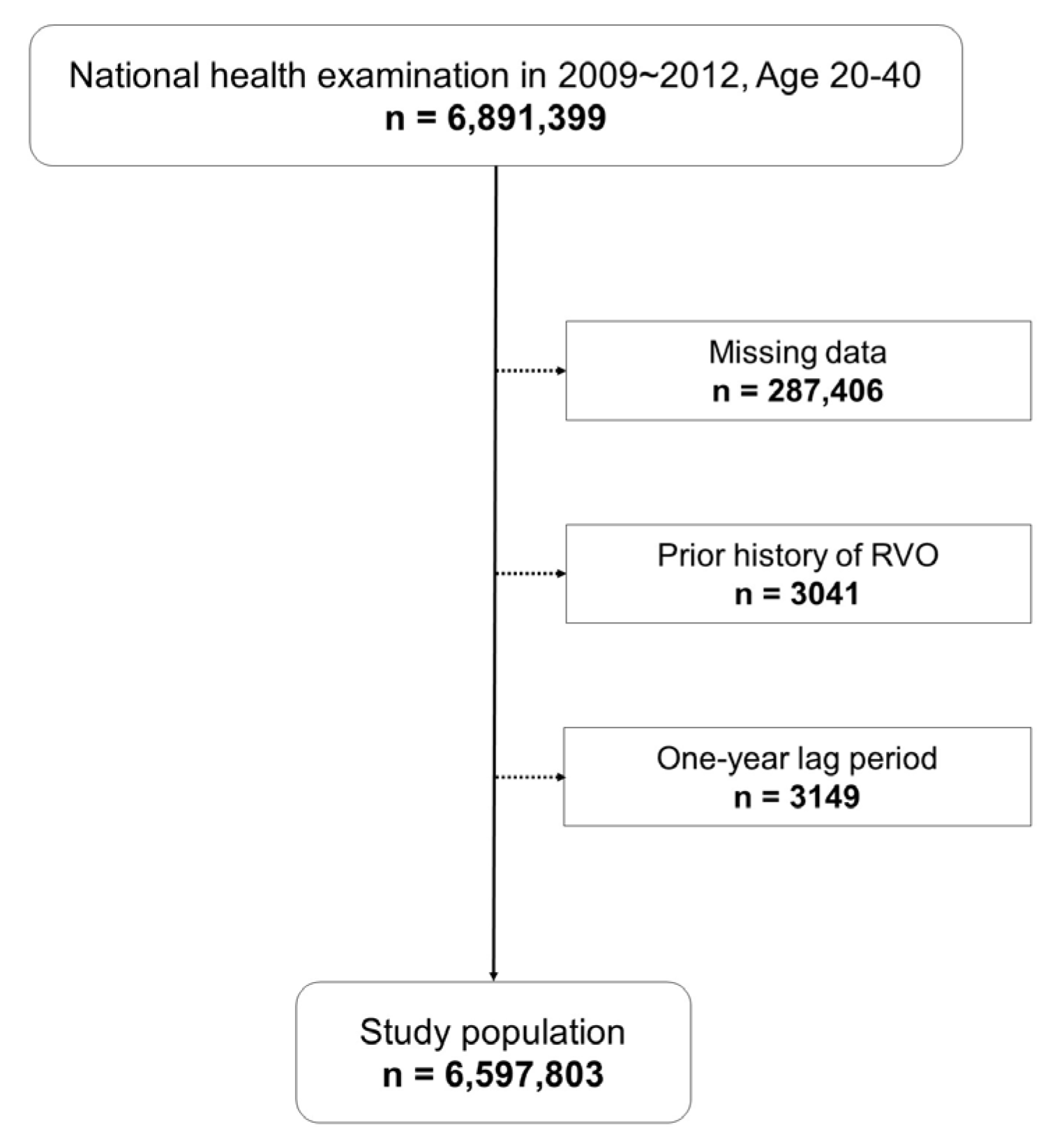
2.2. Study Population
2.3. Definition of RVO and Mental Disorders
2.4. Covariates
2.5. Statistical Analysis
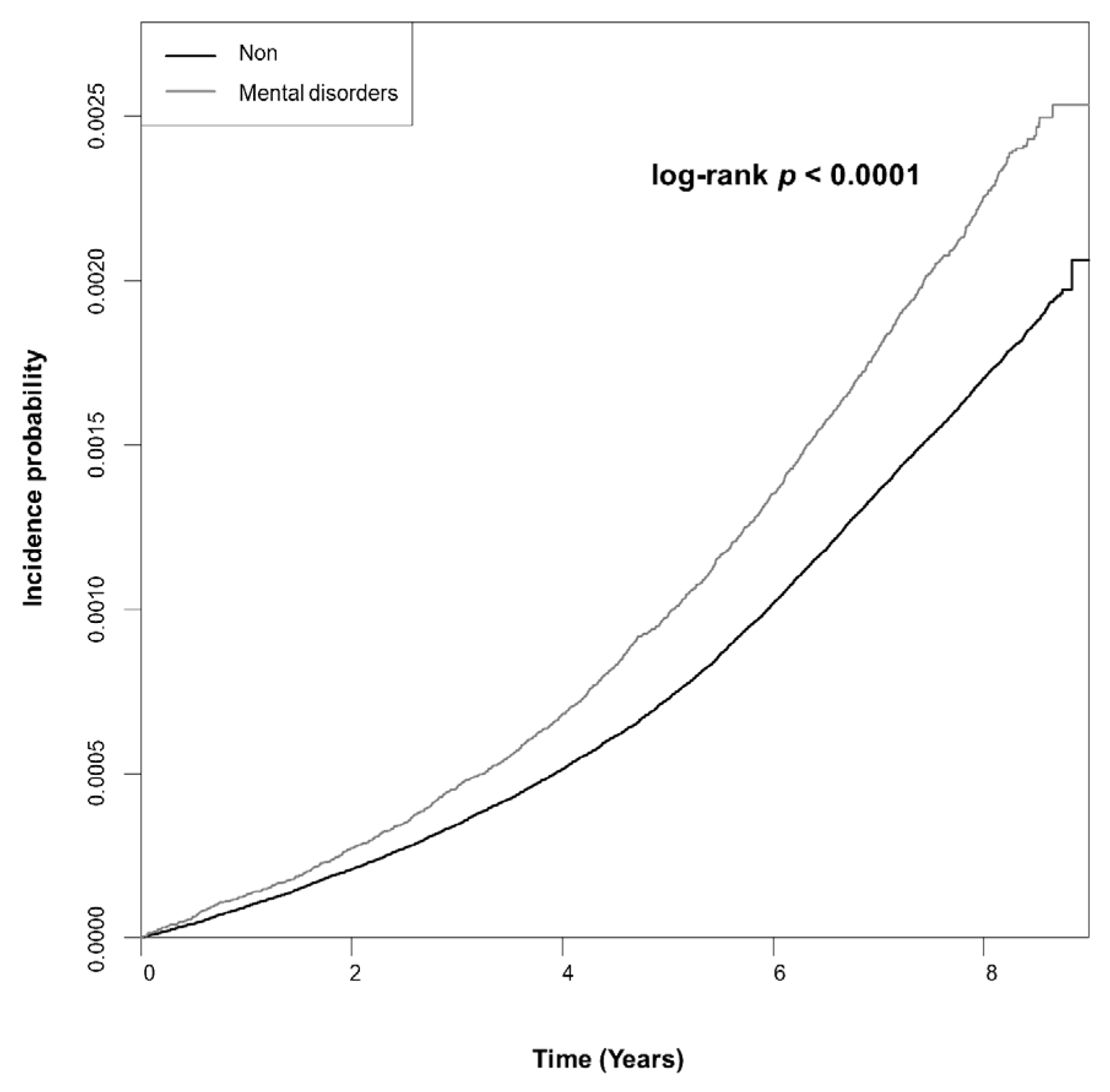
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rogers, S.; McIntosh, R.L.; Cheung, N.; Lim, L.; Wang, J.J.; Mitchell, P.; Kowalski, J.W.; Nguyen, H.; Wong, T.Y. The prevalence of retinal vein occlusion: Pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology 2010, 117, 313–319.e311. [Google Scholar] [CrossRef]
- Cugati, S.; Wang, J.J.; Rochtchina, E.; Mitchell, P. Ten-Year Incidence of Retinal Vein Occlusion in an Older Population: The Blue Mountains Eye Study. Arch. Ophthalmol. 2006, 124, 726–732. [Google Scholar] [CrossRef]
- Scott, I.U.; Campochiaro, P.A.; Newman, N.J.; Biousse, V. Retinal vascular occlusions. Lancet 2020, 396, 1927–1940. [Google Scholar] [CrossRef] [PubMed]
- Fong, A.C.; Schatz, H. Central retinal vein occlusion in young adults. Surv. Ophthalmol. 1993, 37, 393–417. [Google Scholar] [CrossRef] [PubMed]
- Song, P.; Xu, Y.; Zha, M.; Zhang, Y.; Rudan, I. Global epidemiology of retinal vein occlusion: A systematic review and meta-analysis of prevalence, incidence, and risk factors. J. Glob. Health 2019, 9, 010427. [Google Scholar] [CrossRef] [PubMed]
- Sinawat, S.; Bunyavee, C.; Ratanapakorn, T.; Sinawat, S.; Laovirojjanakul, W.; Yospaiboon, Y. Systemic abnormalities associated with retinal vein occlusion in young patients. Clin. Ophthalmol. 2017, 11, 441–447. [Google Scholar] [CrossRef]
- Rehak, M.; Krcova, V.; Slavik, L.; Fric, E.; Langova, K.; Ulehlova, J.; Rehak, J. The role of thrombophilia in patients with retinal vein occlusion and no systemic risk factors. Can. J. Ophthalmol. 2010, 45, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Asherson, R.A.; Merry, P.; Acheson, J.F.; Harris, E.N.; Hughes, G.R. Antiphospholipid antibodies: A risk factor for occlusive ocular vascular disease in systemic lupus erythematosus and the ‘primary’ antiphospholipid syndrome. Ann. Rheum. Dis. 1989, 48, 358–361. [Google Scholar] [CrossRef] [PubMed]
- Batioğlu, F.; Atmaca, L.S.; Karabulut, H.G.; Beyza Sayin, D. Factor V Leiden and prothrombin gene G20210A mutations in ocular Behçet disease. Acta Ophthalmol. Scand. 2003, 81, 283–285. [Google Scholar] [CrossRef] [PubMed]
- Vine, A.K. Hyperhomocysteinemia: A new risk factor for central retinal vein occlusion. Trans. Am. Ophthalmol. Soc. 2000, 98, 493–503. [Google Scholar] [CrossRef]
- Chiang, C.C.; Begley, S.; Henderson, S.O. Central retinal vein occlusion due to hyperviscosity syndrome. J. Emerg. Med. 2000, 18, 23–26. [Google Scholar] [CrossRef]
- Nalcaci, S.; Degirmenci, C.; Akkin, C.; Mentes, J. Etiological factors in young patients with Retinal Vein Occlusion. Pak. J. Med. Sci. 2019, 35, 1397–1401. [Google Scholar] [CrossRef]
- Chen, T.Y.; Uppuluri, A.; Zarbin, M.A.; Bhagat, N. Risk factors for central retinal vein occlusion in young adults. Eur. J. Ophthalmol. 2021, 31, 2546–2555. [Google Scholar] [CrossRef] [PubMed]
- Schwitzer, T.; Schwan, R.; Bubl, E.; Lalanne, L.; Angioi-Duprez, K.; Laprevote, V. Looking into the brain through the retinal ganglion cells in psychiatric disorders: A review of evidences. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2017, 76, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.; Saxena, S.; Lund, C.; Thornicroft, G.; Baingana, F.; Bolton, P.; Chisholm, D.; Collins, P.Y.; Cooper, J.L.; Eaton, J.; et al. The Lancet Commission on global mental health and sustainable development. Lancet 2018, 392, 1553–1598. [Google Scholar] [CrossRef]
- Park, M.J.; Scott, J.T.; Adams, S.H.; Brindis, C.D.; Irwin, C.E., Jr. Adolescent and young adult health in the United States in the past decade: Little improvement and young adults remain worse off than adolescents. J. Adolesc. Health 2014, 55, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Gagné, T.; Schoon, I.; Sacker, A. Trends in young adults’ mental distress and its association with employment: Evidence from the Behavioral Risk Factor Surveillance System, 1993–2019. Prev. Med. 2021, 150, 106691. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef]
- Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [CrossRef] [PubMed]
- Eah, K.S.; Kim, Y.N.; Park, Y.J.; Lee, J.Y.; Kim, J.G.; Yoon, Y.H.; Kim, Y.J. Central Retinal Vein Occlusion in Young Patients: Clinical Characteristics and Prognostic Factors. Retina 2021, 41, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lee, J.S.; Park, S.-H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service–National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2016, 46, e15. [Google Scholar] [CrossRef] [PubMed]
- Seo, M.H.; Lee, W.-Y.; Kim, S.S.; Kang, J.-H.; Kang, J.-H.; Kim, K.K.; Kim, B.-Y.; Kim, Y.-H.; Kim, W.-J.; Kim, E.M.; et al. 2018 Korean Society for the Study of Obesity Guideline for the Management of Obesity in Korea. J. Obes. Metab. Syndr. 2019, 28, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.-Y.; Kang, S.M.; Kang, J.-H.; Kang, S.Y.; Kim, K.K.; Kim, K.-B.; Kim, B.; Kim, S.J.; Kim, Y.-H.; Kim, J.-H.; et al. 2020 Korean Society for the Study of Obesity Guidelines for the Management of Obesity in Korea. J. Obes. Metab. Syndr. 2021, 30, 81–92. [Google Scholar] [CrossRef] [PubMed]
- Ha, M.; Han, K.; Jung, Y.; Kim, D.; Paik, J.-S.; Na, K.-S. Is retinal vein occlusion associated with depression symptoms?: A nationwide cohort study. Medicine 2021, 100, e26937. [Google Scholar] [CrossRef]
- London, A.; Benhar, I.; Schwartz, M. The retina as a window to the brain—From eye research to CNS disorders. Nat. Rev. Neurol. 2013, 9, 44–53. [Google Scholar] [CrossRef]
- National Institutes of Health (US). Information about Mental Illness and the Brain. In NIH Curriculum Supplement Series; Biological Sciences Curriculum Study; National Institutes of Health (US): Bethesda, MD, USA, 2007. [Google Scholar]
- Hoon, M.; Okawa, H.; Della Santina, L.; Wong, R.O.L. Functional architecture of the retina: Development and disease. Prog. Retin. Eye Res. 2014, 42, 44–84. [Google Scholar] [CrossRef]
- Patton, N.; Aslam, T.; MacGillivray, T.; Pattie, A.; Deary, I.J.; Dhillon, B. Retinal vascular image analysis as a potential screening tool for cerebrovascular disease: A rationale based on homology between cerebral and retinal microvasculatures. J. Anat. 2005, 206, 319–348. [Google Scholar] [CrossRef]
- Shalev, I.; Moffitt, T.E.; Wong, T.Y.; Meier, M.H.; Houts, R.M.; Ding, J.; Cheung, C.Y.; Ikram, M.K.; Caspi, A.; Poulton, R. Retinal vessel caliber and lifelong neuropsychological functioning: Retinal imaging as an investigative tool for cognitive epidemiology. Psychol. Sci. 2013, 24, 1198–1207. [Google Scholar] [CrossRef]
- Hubbard, L.D.; Brothers, R.J.; King, W.N.; Clegg, L.X.; Klein, R.; Cooper, L.S.; Sharrett, A.R.; Davis, M.D.; Cai, J. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology 1999, 106, 2269–2280. [Google Scholar] [CrossRef] [PubMed]
- DeBuc, D.C.; Somfai, G.M.; Koller, A. Retinal microvascular network alterations: Potential biomarkers of cerebrovascular and neural diseases. Am. J. Physiol. Heart Circ. Physiol. 2017, 312, H201–H212. [Google Scholar] [CrossRef] [PubMed]
- Esch, T.; Stefano, G.B.; Fricchione, G.L.; Benson, H. The role of stress in neurodegenerative diseases and mental disorders. Neuro Endocrinol. Lett. 2002, 23, 199–208. [Google Scholar] [PubMed]
- Wong, T.Y.; Islam, F.M.A.; Klein, R.; Klein, B.E.K.; Cotch, M.F.; Castro, C.; Sharrett, A.R.; Shahar, E. Retinal Vascular Caliber, Cardiovascular Risk Factors, and Inflammation: The Multi-Ethnic Study of Atherosclerosis (MESA). Investig. Ophthalmol. Vis. Sci. 2006, 47, 2341–2350. [Google Scholar] [CrossRef] [PubMed]
- Sher, L.D.; Geddie, H.; Olivier, L.; Cairns, M.; Truter, N.; Beselaar, L.; Essop, M.F. Chronic stress and endothelial dysfunction: Mechanisms, experimental challenges, and the way ahead. Am. J. Physiol. Heart Circ. Physiol. 2020, 319, H488–H506. [Google Scholar] [CrossRef] [PubMed]
- Hänsel, A.; Hong, S.; Cámara, R.J.A.; von Känel, R. Inflammation as a psychophysiological biomarker in chronic psychosocial stress. Neurosci. Biobehav. Rev. 2010, 35, 115–121. [Google Scholar] [CrossRef]
- Li, L.; Li, X.; Zhou, W.; Messina, J.L. Acute psychological stress results in the rapid development of insulin resistance. J. Endocrinol. 2013, 217, 175–184. [Google Scholar] [CrossRef]
- Piao, L.; Zhao, G.; Zhu, E.; Inoue, A.; Shibata, R.; Lei, Y.; Hu, L.; Yu, C.; Yang, G.; Wu, H.; et al. Chronic Psychological Stress Accelerates Vascular Senescence and Impairs Ischemia-Induced Neovascularization: The Role of Dipeptidyl Peptidase-4/Glucagon-Like Peptide-1-Adiponectin Axis. J. Am. Heart Assoc. 2017, 6, e006421. [Google Scholar] [CrossRef]
- Varma, P.; Junge, M.; Meaklim, H.; Jackson, M.L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2021, 109, 110236. [Google Scholar] [CrossRef]
- Van Aart, C.J.C.; Nawrot, T.S.; Sioen, I.; De Boever, P.; Zaqout, M.; De Henauw, S.; Michels, N. Longitudinal association between psychosocial stress and retinal microvasculature in children and adolescents. Psychoneuroendocrinology 2018, 92, 50–56. [Google Scholar] [CrossRef]
- Caspi, A.; Houts, R.M.; Belsky, D.W.; Goldman-Mellor, S.J.; Harrington, H.; Israel, S.; Meier, M.H.; Ramrakha, S.; Shalev, I.; Poulton, R.; et al. The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders? Clin. Psychol. Sci. 2014, 2, 119–137. [Google Scholar] [CrossRef] [PubMed]
- Van Gennip, A.C.E.; Sedaghat, S.; Carnethon, M.R.; Allen, N.B.; Klein, B.E.K.; Cotch, M.F.; Chirinos, D.A.; Stehouwer, C.D.A.; van Sloten, T.T. Retinal Microvascular Caliber and Incident Depressive Symptoms: The Multi-Ethnic Study of Atherosclerosis. Am. J. Epidemiol. 2021, 191, 843–855. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.C.; Gu, J.K.; Andrew, M.E.; Fekedulegn, D.; Violanti, J.M.; Klein, B.; Tinney-Zara, C.; Charles, L.E. Associations of Sleep Measures with Retinal Microvascular Diameters among Police Officers. Ophthalmic Epidemiol. 2020, 27, 487–497. [Google Scholar] [CrossRef]
- Appaji, A.; Nagendra, B.; Chako, D.M.; Padmanabha, A.; Hiremath, C.V.; Jacob, A.; Varambally, S.; Kesavan, M.; Venkatasubramanian, G.; Rao, S.V.; et al. Retinal vascular abnormalities in schizophrenia and bipolar disorder: A window to the brain. Bipolar Disord. 2019, 21, 634–641. [Google Scholar] [CrossRef]
- Fatemi, S.H.; Folsom, T.D. The Neurodevelopmental Hypothesis of Schizophrenia, Revisited. Schizophr. Bull. 2009, 35, 528–548. [Google Scholar] [CrossRef]
- Owen, M.J.; Sawa, A.; Mortensen, P.B. Schizophrenia. Lancet 2016, 388, 86–97. [Google Scholar] [CrossRef]
- Craddock, N.; Owen, M.J. The Kraepelinian dichotomy-going, going... but still not gone. Br. J. Psychiatry 2010, 196, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.; Curtis, V.; Murray, R.M. Schizophrenia and bipolar disorder: Similarities in pathogenic mechanisms but differences in neurodevelopment. Int. Clin. Psychopharmacol. 2002, 17 (Suppl. 3), S11–S19. [Google Scholar]
- Cho, S.J.; Lee, J.Y.; Hong, J.P.; Lee, H.B.; Cho, M.J.; Hahm, B.J. Mental health service use in a nationwide sample of Korean adults. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 943. [Google Scholar] [CrossRef]
- Leong, F.T.; Lau, A.S. Barriers to providing effective mental health services to Asian Americans. Ment Health Serv. Res. 2001, 3, 201–214. [Google Scholar] [CrossRef]
- McAllister, I.L. Central retinal vein occlusion: A review. Clin. Exp. Ophthalmol. 2012, 40, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Jaulim, A.; Ahmed, B.; Khanam, T.; Chatziralli, I.P. Branch retinal vein occlusion: Epidemiology, pathogenesis, risk factors, clinical features, diagnosis, and complications. An update of the literature. Retina 2013, 33, 901–910. [Google Scholar] [CrossRef] [PubMed]

| Non-Diagnosed Group (n = 5,923,268) | Mental Disorders Group (n = 674,535) | p Value | |
|---|---|---|---|
| Age (years) | 30.8 ± 4.99 | 31.42 ± 4.99 | <0.0001 |
| 20–29 (%) | 2,524,133 (42.61) | 253,333 (37.56) | <0.0001 |
| 30–39 (%) | 3,399,135 (57.39) | 421,202 (62.44) | <0.0001 |
| Sex, male (%) | 3,620,948 (61.13) | 311,227 (46.14) | <0.0001 |
| Current smoker (%) | 2,112,635 (35.67) | 192,330 (28.51) | <0.0001 |
| Heavy alcohol drinker (%) | 529,997 (8.95) | 52,157 (7.73) | <0.0001 |
| Intense exercise (%) | 2,219,545 (37.47) | 270,225 (40.06) | <0.0001 |
| Low economic status (%) | 917,240 (15.49) | 122,873 (18.22) | <0.0001 |
| DM | 116,372 (1.96) | 14,231 (2.11) | <0.0001 |
| HTN | 440,577 (7.44) | 49,305 (7.31) | 0.0001 |
| Dyslipidemia | 411,080 (6.94) | 49,485 (7.34) | <0.0001 |
| Metabolic syndrome | 647,552 (10.93) | 69,571 (10.31) | <0.0001 |
| Obesity | 1,593,096 (26.9) | 161,717 (23.97) | <0.0001 |
| BMI (kg/m2) | 23.05 ± 3.61 | 22.69 ± 3.65 | <0.0001 |
| Waist circumference (cm) | 77.69 ± 10.24 | 76.3 ± 10.58 | <0.0001 |
| FBS (mg/dL) | 90.99 ± 16.9 | 90.7 ± 16.71 | <0.0001 |
| SBP (mmHg) | 117.94 ± 13.2 | 116.16 ± 13.1 | <0.0001 |
| DBP (mmHg) | 73.9 ± 9.47 | 72.92 ± 9.42 | <0.0001 |
| Total cholesterol (mg/dL) | 184.92 ± 36.38 | 184.06 ± 36.1 | <0.0001 |
| HDL cholesterol (mg/dL) | 57.53 ± 28.76 | 58.77 ± 27.85 | <0.0001 |
| Triglyceride (mg/dL) | 120.25 ± 101.55 | 114.76 ± 97.45 | <0.0001 |
| Mental Disorders | N | RVO | IR | HR (95% CI) | |||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||
| Total | No | 5,923,268 | 8841 | 20.256 | 1 (reference) | 1 (reference) | 1 (reference) |
| Yes | 674,535 | 1304 | 26.574 | 1.323 (1.249, 1.402) | 1.275 (1.202, 1.352) | 1.268 (1.196, 1.344) | |
| p < 0.0001 | p < 0.0001 | p < 0.0001 | |||||
| Depression | No | 6,411,698 | 9768 | 20.691 | 1 (reference) | 1 (reference) | 1 (reference) |
| Yes | 186,105 | 377 | 28.037 | 1.373 (1.239, 1.522) | 1.318 (1.189, 1.462) | 1.308 (1.18, 1.451) | |
| p < 0.0001 | p < 0.0001 | p < 0.0001 | |||||
| Bipolar disorder | No | 6,586,616 | 10,121 | 20.879 | 1 (reference) | 1 (reference) | 1 (reference) |
| Yes | 11,187 | 24 | 30.753 | 1.531 (1.027, 2.283) | 1.496 (1.003, 2.23) | 1.441 (0.965, 2.151) | |
| p = 0.0367 | p = 0.0484 | p = 0.0738 | |||||
| Schizophrenia | No | 6,590,065 | 10,131 | 20.890 | 1 (reference) | 1 (reference) | 1 (reference) |
| Yes | 7738 | 14 | 25.534 | 1.249 (0.739, 2.109) | 1.179 (0.698, 1.992) | 1.132 (0.67, 1.913) | |
| p = 0.4063 | p = 0.5375 | p = 0.6419 | |||||
| Anxiety disorder | No | 6,179,990 | 9362 | 20.573 | 1 (reference) | 1 (reference) | 1 (reference) |
| Yes | 417,813 | 783 | 25.704 | 1.258 (1.169, 1.353) | 1.212 (1.127, 1.304) | 1.208 (1.122, 1.299) | |
| p < 0.0001 | p < 0.0001 | p < 0.0001 | |||||
| Sleep disorder | No | 6,422,836 | 9759 | 20.638 | 1 (reference) | 1 (reference) | 1 (reference) |
| Yes | 174,967 | 386 | 30.479 | 1.493 (1.348, 1.652) | 1.418 (1.281, 1.571) | 1.406 (1.269, 1.557) | |
| p < 0.0001 | p < 0.0001 | p < 0.0001 | |||||
| RVO, Retinal Vein Occlusion; HR, Hazard Ratio; CI, Confidential Interval | |||||||
| Incidence Rates | 100,000 person years | ||||||
| Model 1 | Non-Adjusted | ||||||
| Model 2 | Age, Sex, Current smoker, Heavy drinker, Intense exercise, Low economic status | ||||||
| Model 3 | Age, Sex, Current smoker, Heavy drinker, Intense exercise, Low economic status, Metabolic syndrome | ||||||
| Subgroup Factor | HR (95% CI) | p for Interaction | |
|---|---|---|---|
| Age (years) | 20–29 | 1.363 (1.201, 1.547) | 0.1024 |
| 30–39 | 1.244 (1.165, 1.329) | ||
| Sex | Male | 1.237 (1.145, 1.338) | 0.4452 |
| Female | 1.303 (1.192, 1.424) | ||
| Smoking | No | 1.256 (1.171, 1.348) | 0.5717 |
| Current | 1.289 (1.161, 1.432) | ||
| Drinking alcohol | No | 1.267 (1.191, 1.347) | 0.8818 |
| Heavy | 1.281 (1.055, 1.556) | ||
| Intense exercise | No | 1.28 (1.191, 1.376) | 0.6836 |
| Yes | 1.243 (1.124, 1.374) | ||
| Low economic status | No | 1.265 (1.187, 1.349) | 0.7111 |
| Yes | 1.272 (1.098, 1.474) | ||
| DM | No | 1.277 (1.201, 1.357) | 0.406 |
| Yes | 1.109 (0.907, 1.356) | ||
| HTN | No | 1.295 (1.215, 1.38) | 0.0709 |
| Yes | 1.095 (0.942, 1.273) | ||
| Dyslipidemia | No | 1.291 (1.213, 1.374) | 0.0909 |
| Yes | 1.071 (0.898, 1.276) | ||
| Metabolic syndrome | No | 1.318 (1.234, 1.406) | 0.0555 |
| Yes | 1.088 (0.952, 1.243) | ||
| Obesity | No | 1.293 (1.202, 1.39) | 0.5504 |
| Yes | 1.228 (1.113, 1.356) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-y.; Wang, S.-m.; Jeon, S.-h.; Kim, M.-h.; Han, K.-d.; Roh, Y.-j. The Risk of Retinal Vein Occlusion in Young Patients with Mental Disorders: A Nationwide Cohort Study. J. Clin. Med. 2023, 12, 4874. https://doi.org/10.3390/jcm12144874
Lee J-y, Wang S-m, Jeon S-h, Kim M-h, Han K-d, Roh Y-j. The Risk of Retinal Vein Occlusion in Young Patients with Mental Disorders: A Nationwide Cohort Study. Journal of Clinical Medicine. 2023; 12(14):4874. https://doi.org/10.3390/jcm12144874
Chicago/Turabian StyleLee, Ji-young, Sheng-min Wang, Seung-hee Jeon, Min-hee Kim, Kyung-do Han, and Young-jung Roh. 2023. "The Risk of Retinal Vein Occlusion in Young Patients with Mental Disorders: A Nationwide Cohort Study" Journal of Clinical Medicine 12, no. 14: 4874. https://doi.org/10.3390/jcm12144874
APA StyleLee, J.-y., Wang, S.-m., Jeon, S.-h., Kim, M.-h., Han, K.-d., & Roh, Y.-j. (2023). The Risk of Retinal Vein Occlusion in Young Patients with Mental Disorders: A Nationwide Cohort Study. Journal of Clinical Medicine, 12(14), 4874. https://doi.org/10.3390/jcm12144874






