Antenatal Diagnosis and Management of Fetal Intestinal Volvulus: Case Series and Literature Review
Abstract
1. Introduction
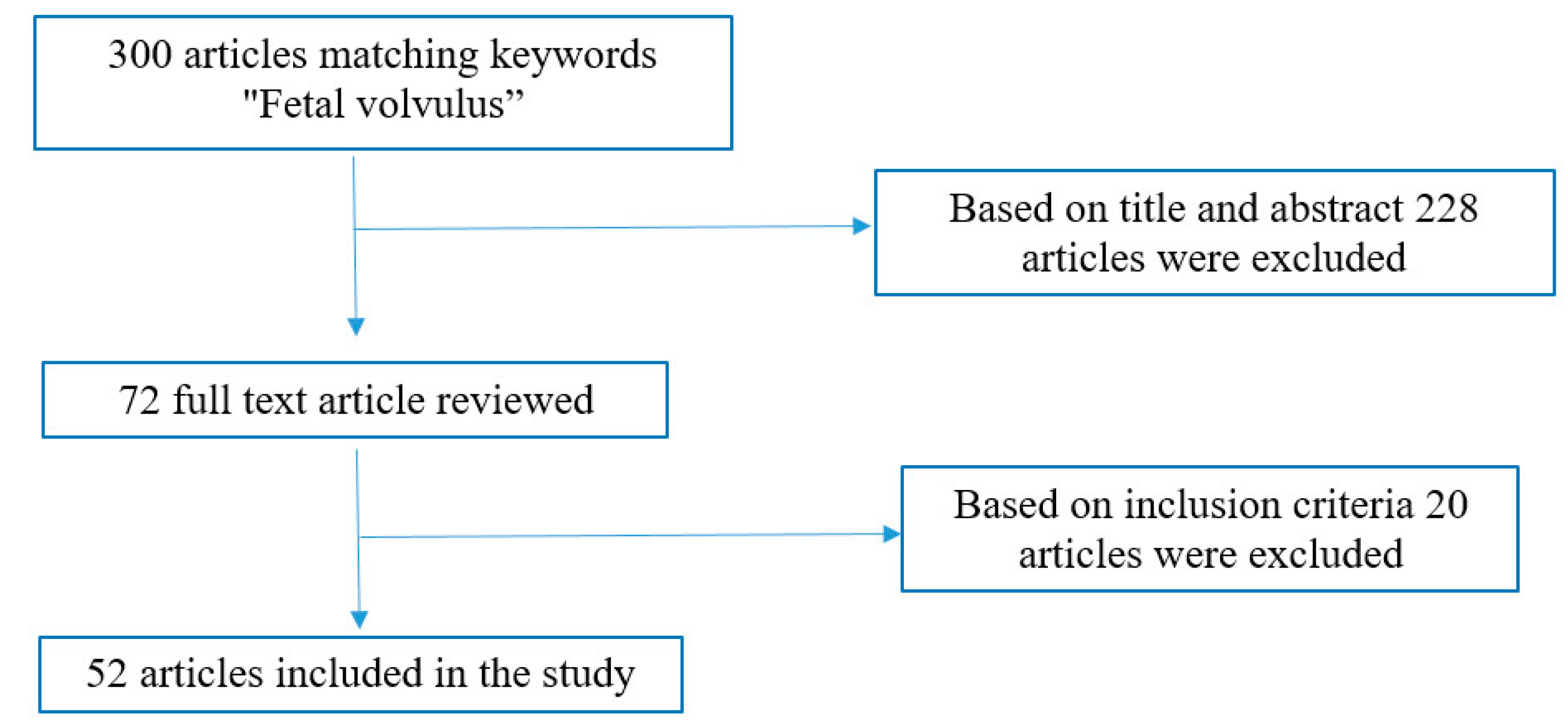
2. Materials and Methods
2.1. Case Series
2.2. Literature Review
3. Results
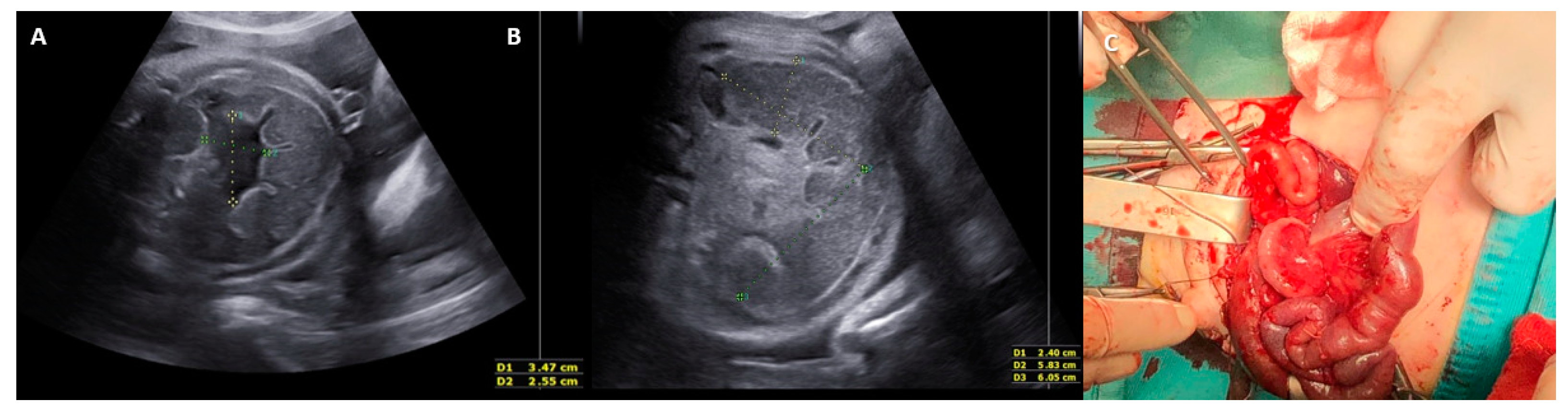
3.1. Case Series Results
3.2. Literature Review Results
3.2.1. Clinical Presentation of Fetal Intestinal Volvulus
3.2.2. Ultrasound Features of Fetal Intestinal Volvulus
3.2.3. Etiology of Fetal Intestinal Volvulus
3.2.4. Antenatal Management of Fetal Intestinal Volvulus
3.2.5. Postnatal Management of Fetal Intestinal Volvulus
3.2.6. Postoperative Outcome of Fetal Intestinal Volvulus
- One case of idiopathic midgut volvulus where the twisted bowel loop became a necrotized cyst mass of 7 cm in diameter. The baby died of multiorgan failure after spontaneous vaginal delivery and postnatal surgery at 30 GW. The fetus showed a 55 × 50 mm abdominal mass in the lower abdomen on US (with a thick wall and papillary projection) and signs of fetal distress (↑ peak of systolic velocity on the middle cerebral artery (PSV-MCA), preterm labor, and sinus rhythm).
- One case of idiopathic midgut volvulus born after a cesarean section performed at 35 GW for non-reassuring FHR, despite the fetus showing severe signs suggestive of intestinal volvulus on US (whirlpool sign, fluid-meconium levels, bowel dilatation, meconium peritonitis) and signs of fetal distress (↓ FMs) after 34 GW.
- One case of total volvulus on malrotated gut with necrosis, born at 38 GW after a spontaneous vaginal delivery and with no antenatal US findings.
- One case of midgut volvulus due to partial malrotation and obstruction of the Meckel diverticulum. The baby died on day 7 because of volume and electrolyte imbalance due to SBS. The baby was born at 28 GW after a cesarean section performed for worsening of US features (hydramnios, multiple cystic spaces in the abdomen, ascites, ↑ abdominal circumference > 95° percentile) and after PPROM at 28 GW.
- One case of idiopathic midgut volvulus died on day 10 after cardiac arrest. The baby was affected by Joubert syndrome and was born at 33 GW after a cesarean section performed for suspicion of fetal volvulus (dilated and hyperechoic bowel, gastric dilatation, mild ascites, and reduction in FMs).
- One case of midgut volvulus with necrosis and perforation, intestinal atresia, and duplication. The baby died on day 36 of intraventricular hemorrhage and sepsis. The baby was born at 35 GW after a spontaneous vaginal delivery. A US follow-up was carried out from GW 34 despite the fetus showing signs of distress (preterm labor) and worsening of US findings of the volvulus, such as severe hydramnios, whirlpool sign (with no flow signal and subsequent disappearance), ↑ bowel dilatation, and thick ascites of mixed echogenicity.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Noreldeen, S.A.; Hodgett, S.G.; Venkat-Raman, N. Midgut volvulus with hemorrhagic ascites: A rare cause of fetal anemia. Ultrasound Obstet. Gynecol. 2008, 31, 352–354. [Google Scholar] [CrossRef] [PubMed]
- Steffensen, T.S.; Gilbert-Barness, E.; DeStefano, K.A.; Kontopoulos, E.V. Midgut volvulus causing fetal demise in utero. Fetal Pediatr. Pathol. 2008, 27, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Has, R.; Gunay, S. Whirlpool sign in the prenatal diagnosis of intestinal volvulus. Ultrasound Obstet. Gynecol. 2002, 20, 307–308. [Google Scholar] [CrossRef] [PubMed]
- Raherison, R.; Grosos, C.; Lemale, J.; Blondiaux, E.; Sabourdin, N.; Dahan, S.; Rosenblatt, J.; Guilbert, J.; Jouannic, J.M.; Mitanchez, D.; et al. Prenatal intestinal volvulus: A life-threatening event with good long-term outcome. Arch. Pediatr. 2012, 19, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Kaba, M.; Oksuzoglu, A.; Kaba, G.; Timur, H.; Akbaba, E.; Turgut, K. Fetal midgut volvulus with a cystic appearance, accompanying a sinus rhythm and an increased peak systolic velocity without anemia. Case Rep. Obstet. Gynecol. 2015, 2015, 354619. [Google Scholar] [CrossRef]
- Park, J.S.; Cha, S.J.; Kim, B.G.; Kim, Y.S.; Choi, Y.S.; Chang, I.T.; Kim, G.J.; Lee, W.S.; Kim, G.H. Intrauterine midgut volvulus without malrotation: Diagnosis from the “coffee bean sign”. World J. Gastroenterol. 2008, 14, 1456–1458. [Google Scholar] [CrossRef]
- Uerpairojkit, B.; Charoenvidhya, D.; Tanawattanacharoen, S.; Manotaya, S.; Wacharaprechanont, T.; Tannirandorn, Y. Fetal intestinal volvulus: A clinic-sonographic finding. Ultrasound Obstet. Gynecol. 2002, 18, 186–187. [Google Scholar] [CrossRef]
- Van Winckel, M.; Voet, D.; Robberecht, E. ‘‘Whirlpool sign’’: Not always associated with volvulus in intestinal malrotation. J. Clin. Ultrasound 1996, 24, 367–370. [Google Scholar] [CrossRef]
- Jéquier, S.; Hanquinet, S.; Bugmann, P.; Pfizenmaier, M. Antenatal small-bowel volvulus without malrotation: Ultrasound demonstration and discussion of pathogenesis. Pediatr. Radiol. 2003, 33, 263–265. [Google Scholar] [CrossRef]
- Vallarades, E.; Rodriguez, D.; Vela, A.; Cabré, S.; Lailla, J.M. Meconium pseudocyst secondary to ileum volvulus perforation without peritoneal calcification: A case report. J. Med. Case Rep. 2010, 4, 292. [Google Scholar] [CrossRef]
- Kornacki, J.; Czarnecka, M.; Błaszczyński, M.; Skrzypczak, J.; Gadzinowski, J.; Jankowski, A.; Sardesai, S. Congenital midgut volvulus associated with fetal anemia. Fetal Diagn. Ther. 2010, 28, 119–122. [Google Scholar] [CrossRef] [PubMed]
- Bawa, N.; Kannan, N.L. Even a single third trimester antenatal fetal screening for congenital anomalies can be life saving. Indian. J. Pediatr. 2010, 77, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Ailu, C.; Bing, W. Sonographic diagnosis of fetal intestinal volvulus with ileal atresia: A case report. J. Clin. Ultrasound 2012, 41, 255–257. [Google Scholar] [CrossRef] [PubMed]
- Sanders, R.C. Structural Fetal Abnormalities: The Total Picture; Mosby–Year Book: St. Louis, MO, USA, 1996; p. 137. [Google Scholar]
- Best, E.J.; O’Brien, C.M.; Carseldine, W.; Deshpande, A.; Glover, R.; Park, F. Fetal midgut volvulus with meconium peritonitis detected on prenatal ultrasound. Case Rep. Obstet. Gynecol. 2018, 2018, 5312179. [Google Scholar] [CrossRef]
- Sciarrone, A.; Teruzzi, E.; Pertusio, A.; Bastonero, S.; Errante, G.; Todros, T.; Viora, E. Fetal midgut volvulus: Report of eight cases. J. Matern. Fetal Neonatal. Med. 2016, 29, 1322–1327. [Google Scholar] [CrossRef]
- Bartholmot, C.; Faure, J.M.; Grosjean, F.; Couture, A.; Forgues, D.; Fuchs, F.; Prodhomme, O. Prenatal diagnosis of antenatal midgut volvulus: Specific ultrasound features. Prenat. Diagn. 2019, 39, 16–25. [Google Scholar] [CrossRef]
- Suzumori, K.; Adachi, R.; Yagami, Y.; Togari, H. A fetal case with midgut volvulus. Asia-Oceania J. Obstet. Gynecol. 1990, 16, 13–16. [Google Scholar] [CrossRef]
- Leung, W.C.; Pandya, P.; Seaward, G.; Windrim, R.; Ryan, G. Changes in fetal heart rate pattern after intrauterine paracentesis in one twin with meconium peritonitis. Prenat. Diagn. 2001, 21, 693–696. [Google Scholar] [CrossRef]
- Fukushima, S.; Fujioka, K.; Ashina, M.; Ohyama, S.; Ikuta, T.; Nishida, K.; Miyauchi, H.; Okata, Y.; Bitoh, Y.; Tanimura, K.; et al. Fetal primary small bowel volvulus associated with acute gastric dilatation detected by ultrasonography. Kobe J. Med. Sci. 2019, 64, E157–E159. [Google Scholar]
- Durand, M.; Coste, K.; Martin, A.; Scheye, T.; Creveaux, I.; Vanlieferinghen, P.; Laurichesse-Delmas, H.; Dechelotte, P.J.; Labbe, A.; Jacquetin, B.; et al. Fetal midgut volvulus as a sign for cystic fibrosis. Prenat. Diagn. 2008, 28, 973–974. [Google Scholar] [CrossRef]
- Jakhere, S.G.; Saifi, S.A.; Ranwaka, A.A. Fetal small bowel volvulus without malrotation: The whirlpool & coffee bean signs. J. Neonatal Perinat. Med. 2014, 7, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.H.; Lim, G.Y.; Wec, J.S. Fetal primary small bowel volvulus in a child without intestinal malrotation. J. Pediatr. Surg. 2013, 48, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Herrera, T.T.; Rueda, K.; Espinosa, H.; Britton, G.B. Intestinal volvulus in the pump twin of a twin reversed arterial perfusion (TRAP) sequence after laser therapy at 18 weeks: A case report. J. Med. Case Rep. 2020, 14, 123. [Google Scholar] [CrossRef] [PubMed]
- Molvarec, A.; Bábinszki, A.; Kovács, K.; Tóth, F.; Szalay, J. Intrauterine intestinal obstruction due to fetal midgut volvulus: A report of two cases. Fetal Diagn. Ther. 2007, 22, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Chouikh, T.; Mottet, N.; Cabrol, C.; Chaussy, Y. Prenatal intestinal volvulus: Look for cystic fibrosis. BMJ Case Rep. 2016, 2016, bcr2016217003. [Google Scholar] [CrossRef] [PubMed]
- Yip, K.W.; Cheng, Y.K.Y.; Leung, T.Y. Antenatal diagnosis and management of foetal intestinal volvulus. Med. J. Malays. 2017, 72, 126–127. [Google Scholar]
- Ohuoba, E.; Fruhman, G.; Olutoye, O.; Zacharias, N. Perinatal survival of a fetus with intestinal volvulus and intussusception: A case report and review of the literature. AJP Rep. 2013, 3, 107–112. [Google Scholar] [CrossRef]
- Takacs, Z.F.; Meier, C.M.; Solomayer, E.F.; Gortner, L.; Meyberg-Solomayer, G. Prenatal diagnosis and management of an intestinal volvulus with meconium ileus and peritonitis. Arch. Gynecol. Obstet. 2014, 290, 385–387. [Google Scholar] [CrossRef]
- Witter, F.R.; Molteni, R.A. Intrauterine intestinal volvulus with hemoperitoneum presenting as fetal distress at 34 weeks’ gestation. Am. J. Obstet. Gynecol. 1986, 155, 1080–1081. [Google Scholar] [CrossRef]
- Monard, B.; Mottet, N.; Ramanah, R.; Riethmuller, D. Prenatal Diagnosis of a Segmental Small Bowel Volvulus with Threatened Premature Labor. Case Rep. Obstet. Gynecol. 2017, 2017, 7642784. [Google Scholar] [CrossRef]
- Hasegawa, T.; Yoshioka, Y.; Sasaki, T.; Iwasaki, Y.; Miki, Y.; Sumimura, J.; Tomimatsu, T.; Shimizu, K.; Ban, H.; Dezawa, T. Infarcted intestinal volvulus detected by prenatal ultrasonography. Pediatr. Surg. Int. 1996, 11, 498–499. [Google Scholar] [CrossRef] [PubMed]
- Aurégan, C.; Donciu, V.; Millischer, A.E.; Khen-Dunlop, N.; Deloison, B.; Sonigo, P.; Magny, J.F. Prenatal discovery of Joubert syndrome associated with small bowel volvulus. Arch. Pediatr. 2016, 23, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Ridley, A.; Chaussy, Y.; Mottet, N.; Auber, F. Dual intestinal anomalies in dizygotic twins. BMJ Case Rep. 2018, 2018, bcr2018225176. [Google Scholar] [CrossRef] [PubMed]
- Samuel, N.; Dicker, D.; Feldberg, D.; Goldman, J.A. Ultrasound diagnosis and management of fetal intestinal obstruction and volvulus in utero. J. Perinat. Med. 1984, 12, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Kutuk, M.S.; Balta, B.; Doganay, S.; Guzel, M.; Ozgun, M.T. Prenatal diagnosis of intestinal volvulus in a foetus with homozygous M470V cystic fibrosis gene polymorphism. J. Obstet. Gynaecol. 2014, 35, 522–525. [Google Scholar] [CrossRef]
- Yoo, S.J.; Park, K.W.; Cho, S.Y.; Sim, J.S.; Hhan, K.S. Definitive diagnosis of intestinal volvulus in utero. Ultrasound Obstet. Gynecol. 1999, 13, 200–203. [Google Scholar] [CrossRef]
- Finley, B.E.; Burlbaw, J.; Bennett, T.L.; Levitch, L. Delayed return of the fetal midgut to the abdomen resulting in volvulus, bowel obstruction, and gangrene of the small intestine. J. Ultrasound Med. 1992, 11, 233–235. [Google Scholar] [CrossRef]
- Miyakoshi, K.; Ishimoto, H.; Tanigaki, S.; Minegishi, K.; Tanaka, M.; Miyazaki, T.; Yoshimura, Y. Prenatal diagnosis of midgut volvulus by sonography and magnetic resonance imaging. Am. J. Perinatol. 2001, 18, 447–450. [Google Scholar] [CrossRef]
- Allahdin, S.; Kay, V. Ischaemic haemorrhagic necrosis of the intestine secondary to volvulus of the midgut: A silent cause of intrauterine death. J. Obstet. Gynaecol. 2004, 24, 310. [Google Scholar] [CrossRef]
- Cloutier, M.G.; Fried, A.M.; Selke, A.C. Antenatal observation of midgut volvulus by ultrasound. J. Clin. Ultrasound 1983, 11, 286–288. [Google Scholar] [CrossRef]
- Schiermeier, S.; Reinhard, J.; Westhof, G.; Hatzmann, W. The significance of electronic CTG for intrauterine volvulus in the 32nd week of gestation. Z. Geburtsh Neonatol. 2008, 212, 30–33. [Google Scholar] [CrossRef] [PubMed]
- De Felice, C.; Massafra, C.; Centini, G.; Di Maggio, G.; Tota, G.; Bracci, R. Relationship between intrauterine midgut volvulus without malrotation and preterm delivery. Acta Obstet. Gynecol. Scand. 1997, 76, 386. [Google Scholar] [CrossRef] [PubMed]
- Neis, K.J.; Seeliger, H. Intrauterine volvulus with complete necrosis of the small bowel and pseudocystic tumour. Z. Kinderchir. 1983, 38, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Taba, R.; Yamakawa, M.; Harada, S.; Yamada, Y. A case of massive meconium peritonitis in utero successfully managed by planned cardiopulmonary resuscitation of the newborn. Adv. Neonatal Care 2010, 10, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Ogunyemi, D. Prenatal ultrasonographic diagnosis of ileal atresia and volvulus in a twin pregnancy. J. Ultrasound Med. 2000, 19, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Im, S.A.; Lee, G. Evolution of sonographic findings in a fetus with ileal atresia. J. Clin. Ultrasound 2011, 39, 359–362. [Google Scholar] [CrossRef]
- Alvarez, M.; Lasker, M.R.; Friedman, F., Jr.; Chitkara, U.; Berkowitz, R.L.; Holzman, I.R. Sonographic findings in a twin with congenital fetal volvulus. J. Clin. Ultrasound 1991, 19, 98–100. [Google Scholar] [CrossRef]
- Baxi, L.V.; Yeh, M.N.; Blanc, W.A.; Schullinger, J.N. Antepartum diagnosis and management of in utero intestinal volvulus with perforation. N. Engl. J. Med. 1983, 308, 1519–1521. [Google Scholar] [CrossRef]
- Casaccia, G.; Trucchi, A.; Nahom, A.; Aite, L.; Lucidi, V.; Giorlandino, C.; Bagolan, P. The impact of cystic fibrosis on neonatal intestinal obstruction: The need for prenatal/neonatal screening. Pediatr. Surg. Int. 2003, 19, 75–78. [Google Scholar] [CrossRef]
- Chen, J.; Wu, D. Prenatal diagnosis of fetal midgut volvulus: A case description. Quant. Imaging Med. Surg. 2022, 12, 4326–4330. [Google Scholar] [CrossRef]
- Jain, N.; Awal, S.S.; Biswas, S.; Ghosh, T. Prenatal diagnosis of fetal midgut volvulus: A case report. J. Med. Case Rep. 2022, 16, 482. [Google Scholar] [CrossRef] [PubMed]
- Matsushima, H.; Katsura, M.; Ie, M.; Genkawa, R. Intrauterine intestinal volvulus without malrotation presenting neonatal abdominal compartment syndrome. Int. J. Surg. Case Rep. 2022, 100, 107742. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Huang, T.; Zhou, M.; Zhang, C. Prenatal diagnosis of midgut volvulus using two-dimensional and three-dimensional ultrasound. Am. J. Transl. Res. 2022, 14, 1859–1867. [Google Scholar] [PubMed]
- Yang, L.; Chen, H.; Lv, G.; Li, F.; Liao, J.; Ke, L. Evaluation of ultrasonography in fetal intestinal malrotation with midgut volvulus. Ginekol. Pol. 2022, 93, 296–301. [Google Scholar] [CrossRef]
| Clinical Presentation | No. (%) | ||
|---|---|---|---|
| Review | Case Series | Total | |
| ND | 39 | 3 | 42 (37.1) |
| ↓ FMs and/or non-reassuring CTG | 33 | 3 | 36 (31.8) |
| N | 19 | 0 | 19 (16.8) |
| ↑ PSV MCA | 7 | 0 | 7 (6.19) |
| Preterm labor | 6 | 1 | 7 (6.19) |
| PPROM | 6 | 1 | 7 (6.19) |
| IUFD | 2 | 0 | 2 (1.7) |
| Presumed Etiology | No. (%) | ||
|---|---|---|---|
| Review | Case Series | Total | |
| Idiopathic | 39 | 1 | 40 (35.3) |
| Malrotation | 25 | 1 | 26 (23.0) |
| CF | 12 | 0 | 12 (10.6) |
| Minor GI defects (persistent entero-mesenteric umbilical connection, mesentery fusion, mesentery dysplasia, primitive mesenteric breach, microcolon, hypoplastic distal segment of small bowel, partial malrotation with obstruction of Meckel diverticulum, bowel duplication) | 11 | 2 | 13 (11.5) |
| Small bowel atresia | 10 | 2 | 12 (10.6) |
| Not defined | 7 | 0 | 7 (6.19) |
| Immaturity of intramural ganglion cells in descending and sigmoid colon | 1 | 0 | 1 (0.8) |
| Meconium Ileum | 1 | 0 | 1 (0.8) |
| Delayed return of midgut to abdomen beyond 13 weeks of gestation | 1 | 0 | 1(0.8) |
| Total | 107 | 6 | 113 (100) |
| Postoperative Outcome | No. (%) | ||
|---|---|---|---|
| Review | Case Series | Total | |
| Uneventful | 58 | 2 | 60 (58.2) |
| Postoperative complications | 29 | 4 | 33 (32.0) |
| short bowel syndrome | 12 | 2 | 14 |
| sepsis | 3 | 0 | 3 |
| peritonitis | 2 | 0 | 2 |
| perforation | 2 | 0 | 2 |
| cholestasis | 2 | 1 | 3 |
| delayed intestinal continuity restoration | 1 | 0 | 1 |
| intestinal obstruction | 7 | 1 | 8 |
| Neonatal death (including one total volvulus and one with Joubert syndrome) | 6 | 0 | 6 (5.8) |
| Respiratory complications due to CF | 2 | 0 | 2 (1.9) |
| No data available | 2 | 0 | 2 (1.9) |
| Total | 97 | 6 | 103 (100) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montironi, R.; Tosto, V.; Quintili, D.; Crescenzi, D.; Battistoni, G.I.; Cobellis, G.; Giannubilo, S.R.; Ciavattini, A. Antenatal Diagnosis and Management of Fetal Intestinal Volvulus: Case Series and Literature Review. J. Clin. Med. 2023, 12, 4790. https://doi.org/10.3390/jcm12144790
Montironi R, Tosto V, Quintili D, Crescenzi D, Battistoni GI, Cobellis G, Giannubilo SR, Ciavattini A. Antenatal Diagnosis and Management of Fetal Intestinal Volvulus: Case Series and Literature Review. Journal of Clinical Medicine. 2023; 12(14):4790. https://doi.org/10.3390/jcm12144790
Chicago/Turabian StyleMontironi, Ramona, Valentina Tosto, Dayana Quintili, Daniele Crescenzi, Giovanna Irene Battistoni, Giovanni Cobellis, Stefano Raffaele Giannubilo, and Andrea Ciavattini. 2023. "Antenatal Diagnosis and Management of Fetal Intestinal Volvulus: Case Series and Literature Review" Journal of Clinical Medicine 12, no. 14: 4790. https://doi.org/10.3390/jcm12144790
APA StyleMontironi, R., Tosto, V., Quintili, D., Crescenzi, D., Battistoni, G. I., Cobellis, G., Giannubilo, S. R., & Ciavattini, A. (2023). Antenatal Diagnosis and Management of Fetal Intestinal Volvulus: Case Series and Literature Review. Journal of Clinical Medicine, 12(14), 4790. https://doi.org/10.3390/jcm12144790





