Redo-TAVR: Essential Concepts, Updated Data and Current Gaps in Evidence
Abstract
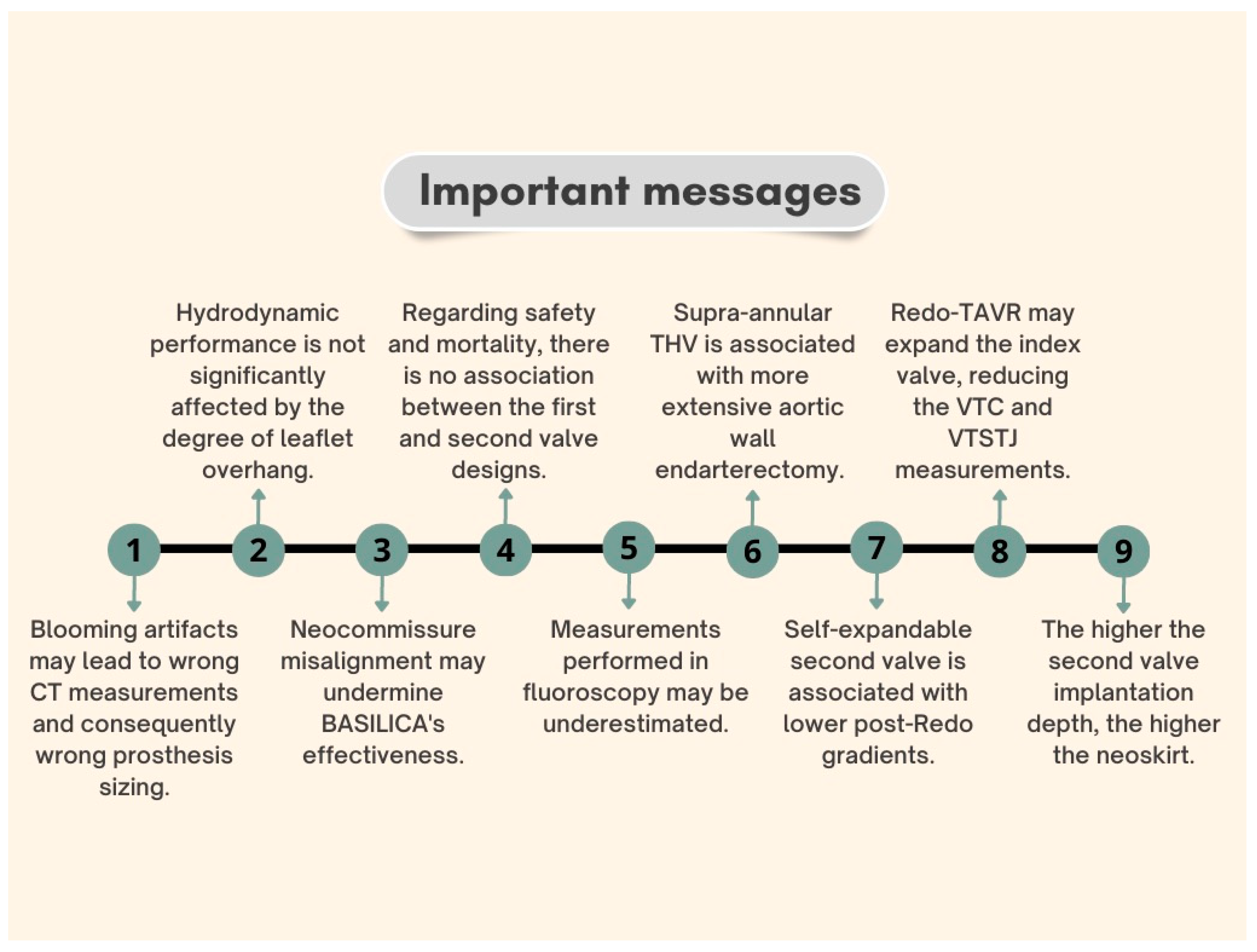
1. Introduction
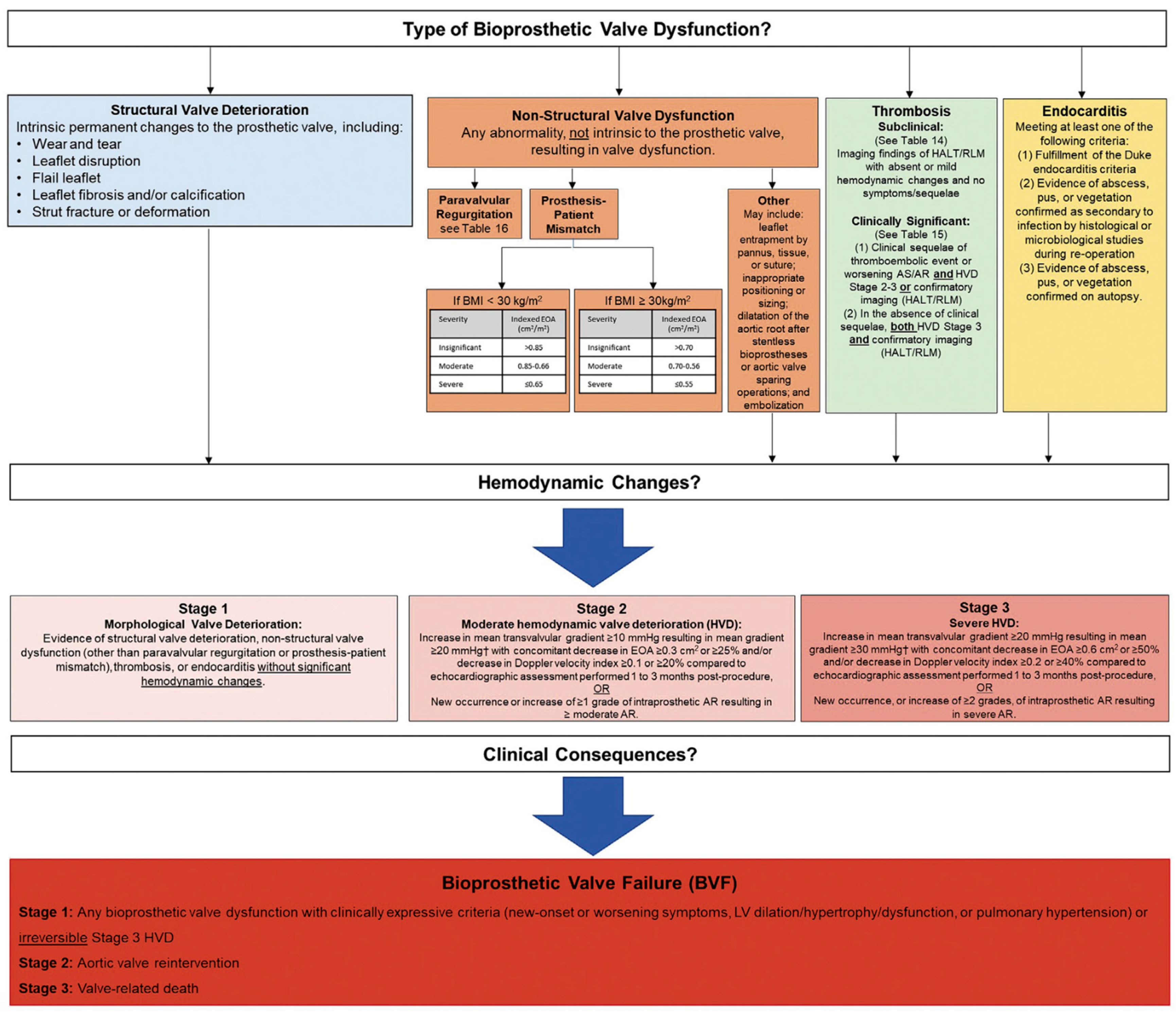
2. Bioprosthetic Valve Dysfunction and Structural Valve Deterioration Definitions
3. TAVR Explantation
4. Overall Mortality
5. Preprocedural Computed Tomography Planning
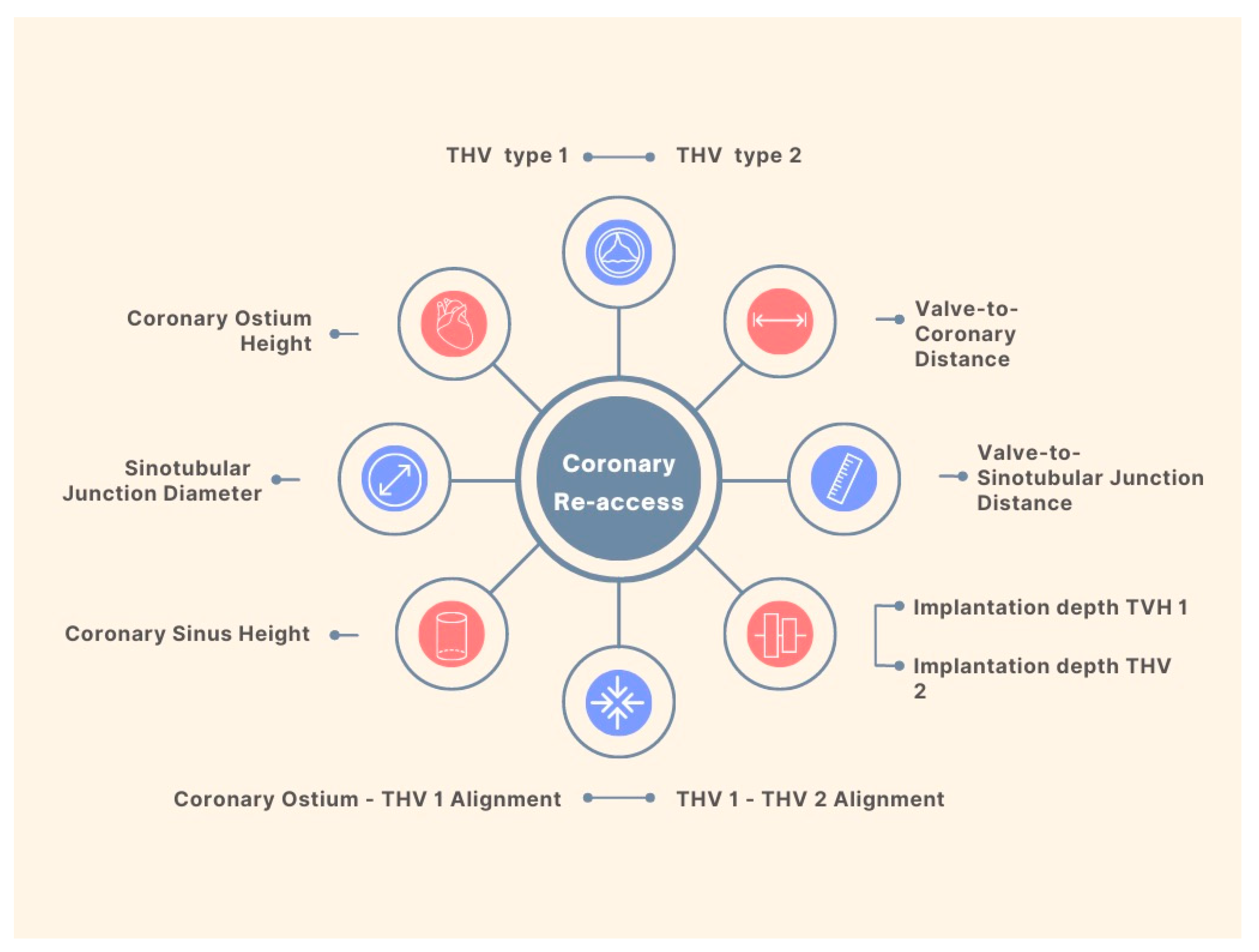
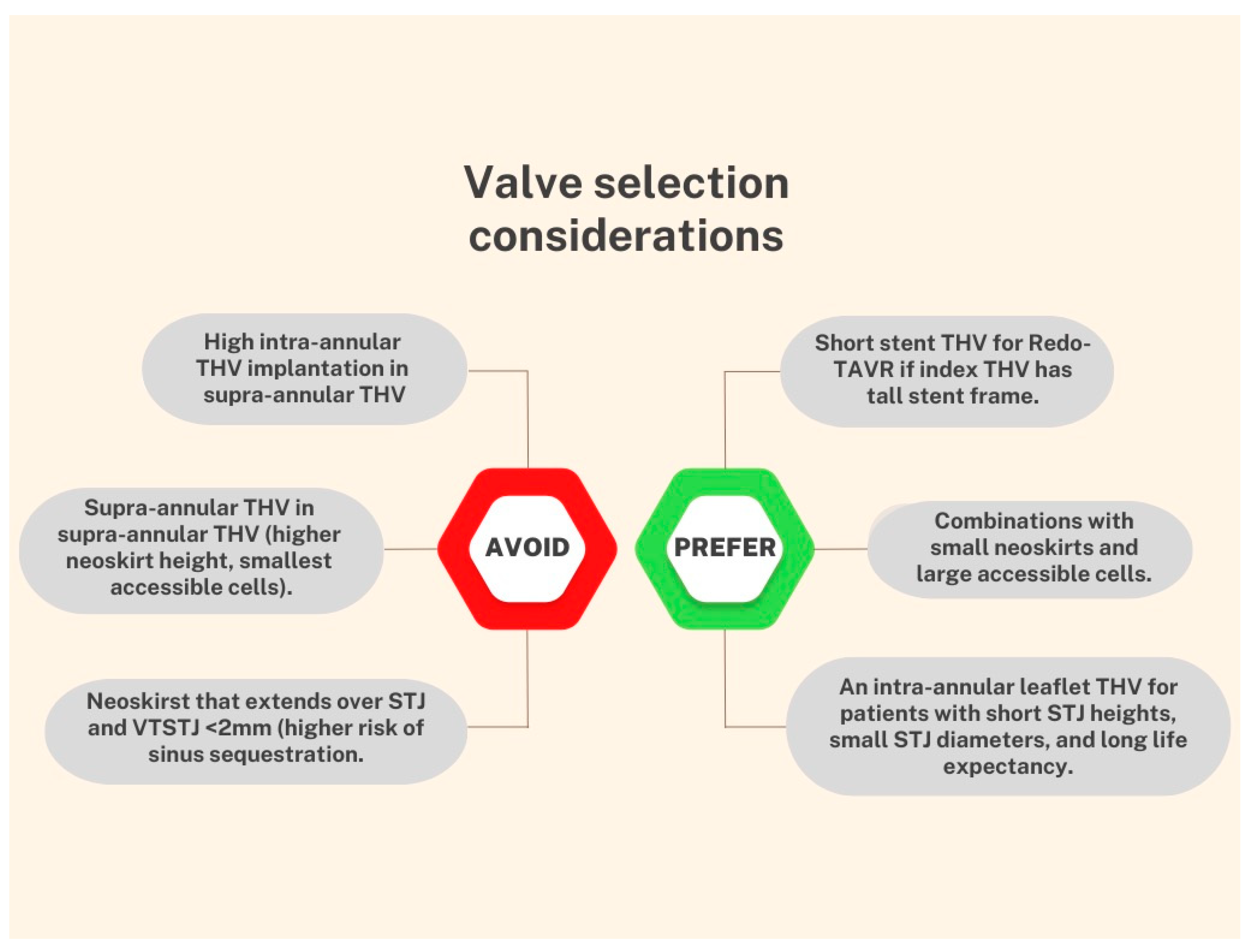
6. TAVR-in-TAVR: Procedural Complications
Coronary Obstruction
7. Mitigating the Risk of Coronary Obstruction
8. Patient-Prosthesis Mismatch
8.1. Stroke
8.2. Permanent Pacemaker Implantation
9. Post-Procedural Antithrombotic Management
10. Future Perspectives
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AS | aortic stenosis |
| BEV | balloon-expandable valve |
| BVD | bioprosthetic valve dysfunction |
| BVF | bioprosthetic valve failure |
| CT | computed tomography |
| EOA | effective orifice area |
| LVOT | left ventricular outflow tract |
| OR | odds-ratio |
| PCI | percutaneous coronary intervention |
| PPMI | permanent pacemaker implantation |
| PPM | patient-prosthesis mismatch |
| SAVR | surgical aortic valve replacement |
| SEV | self-expandable valve |
| STJ | sinotubular junction |
| SVD | structural valve degeneration |
| TAVR | transcatheter aortic valve replacement |
| THV | transcatheter heart valve |
| VARC | Valve Academic Research Consortium |
| ViV | valve-in-valve |
| VTC | valve-to-coronary |
| VTSTJ | valve-to-sinotubular junction |
References
- Cribier, A.; Eltchaninoff, H.; Bash, A.; Borenstein, N.; Tron, C.; Bauer, F.; Derumeaux, G.; Anselme, F.; Laborde, F.; Leon, M.B. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: First human case description. Circulation 2002, 106, 3006–3008. [Google Scholar] [CrossRef] [PubMed]
- Leon, M.B.; Smith, C.R.; Mack, M.; Miller, D.C.; Moses, J.W.; Svensson, L.G.; Tuzcu, E.M.; Webb, J.G.; Fontana, G.P.; Makkar, R.R.; et al. Transcatheter Aortic-Valve Implantation for Aortic Stenosis in Patients Who Cannot Undergo Surgery. N. Engl. J. Med. 2010, 363, 1597–1607. [Google Scholar] [CrossRef]
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2016, 374, 1609–1620. [Google Scholar] [CrossRef]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705. [Google Scholar] [CrossRef] [PubMed]
- Carroll, J.D.; Mack, M.J.; Vemulapalli, S.; Herrmann, H.C.; Gleason, T.G.; Hanzel, G.; Deeb, G.M.; Thourani, V.H.; Cohen, D.J.; Desai, N.; et al. STS-ACC TVT Registry of Transcatheter Aortic Valve Replacement. J. Am. Coll. Cardiol. 2020, 76, 2492–2516. [Google Scholar] [CrossRef] [PubMed]
- Faroux, L.; Alperi, A.; Muntané-Carol, G.; Rodes-Cabau, J. Safety and efficacy of repeat transcatheter aortic valve replacement for the treatment of transcatheter prosthesis dysfunction. Expert Rev. Med. Devices 2020, 17, 1303–1310. [Google Scholar] [CrossRef] [PubMed]
- Généreux, P.; Piazza, N.; Alu, M.C.; Nazif, T.; Hahn, R.T.; Pibarot, P.; Bax, J.J.; Leipsic, J.A.; Blanke, P.; Blackstone, E.H.; et al. Valve Academic Research Consortium 3: Updated Endpoint Definitions for Aortic Valve Clinical Research. J. Am. Coll. Cardiol. 2021, 77, 2717–2746. [Google Scholar] [CrossRef]
- Bapat, V.N.; Zaid, S.; Fukuhara, S.; Saha, S.; Vitanova, K.; Kiefer, P.; Squiers, J.J.; Voisine, P.; Pirelli, L.; von Ballmoos, M.W.; et al. Surgical Explantation After TAVR Failure: Mid-Term Outcomes From the EXPLANT-TAVR International Registry. JACC Cardiovasc. Interv. 2021, 14, 1978–1991. [Google Scholar] [CrossRef] [PubMed]
- Fukuhara, S.; Nguyen, C.T.N.; Yang, B.; Patel, H.J.; Ailawadi, G.; Kim, K.M.; Deeb, G.M. Surgical Explantation of Transcatheter Aortic Bioprostheses: Balloon vs Self-Expandable Devices. Ann. Thorac. Surg. 2022, 113, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Fukuhara, S.; Brescia, A.A.; Deeb, G.M. Surgical Explantation of Transcatheter Aortic Bioprostheses An Analysis From the Society of Thoracic Surgeons Database. Circulation 2020, 142, 2285–2287. [Google Scholar] [CrossRef] [PubMed]
- Zaid, S.; Fukuhara, S.; Marin-Cuartas, M.; Backer, O.D.; Bhadra, O.; Grubb, K.; Shih, E.; Meier, D.; Goel, S.; Tang, G. TCT-399 Impact of Mechanism of TAVR Failure on Outcomes after Reintervention for Failed TAVR: Insights From the EXPLANTORREDO-TAVR International Registry. J. Am. Coll. Cardiol. 2022, 80, B161–B162. [Google Scholar] [CrossRef]
- Vitanova, K.; Zaid, S.; Tang, G.H.L.; Kaneko, T.; Bapat, V.N.; Modine, T.; Denti, P. Aortic valve versus root surgery after failed transcatheter aortic valve replacement. J. Thorac. Cardiovasc. Surg. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Sá, M.P.B.O.; Van den Eynde, J.; Simonato, M.; Cavalcanti, L.R.P.; Doulamis, I.P.; Weixler, V.; Kampaktsis, P.N.; Gallo, M.; Laforgia, P.L.; Zhigalov, K.; et al. Valve-in-Valve Transcatheter Aortic Valve Replacement Versus Redo Surgical Aortic Valve Replacement: An Updated Meta-Analysis. JACC Cardiovasc. Interv. 2021, 14, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Gallo, M.; Fovino, N.; Blitzer, D.; Doulamis, I.P.; Guariento, A.; Salvador, L.; Tagliari, A.P.; Ferrari, E. Transcatheter aortic valve replacement for structural degeneration of previously implanted transcatheter valves (TAVR-in-TAVR): A systematic review. Eur. J. Cardio-Thorac. Surg. 2022, 61, 967–976. [Google Scholar] [CrossRef]
- Landes, U.; Webb, J.G.; De Backer, O.; Sondergaard, L.; Abdel-Wahab, M.; Crusius, L.; Kim, W.K.; Hamm, C.; Buzzatti, N.; Montorfano, M.; et al. Repeat Transcatheter Aortic Valve Replacement for Transcatheter Prosthesis Dysfunction. J. Am. Coll. Cardiol. 2020, 75, 1882–1893. [Google Scholar] [CrossRef]
- Ribeiro, H.B.; Rodés-Cabau, J.; Blanke, P.; Leipsic, J.; Kwan Park, J.; Bapat, V.; Makkar, R.; Simonato, M.; Barbanti, M.; Schofer, J.; et al. Incidence, predictors, and clinical outcomes of coronary obstruction following transcatheter aortic valve replacement for degenerative bioprosthetic surgical valves: Insights from the VIVID registry. Eur. Heart J. 2018, 39, 687–695. [Google Scholar] [CrossRef]
- Landes, U.; Sathananthan, J.; Witberg, G.; de Backer, O.; Sondergaard, L.; Abdel-Wahab, M.; Holzhey, D.; Kim, W.K.; Hamm, C.; Buzzatti, N.; et al. Transcatheter Replacement of Transcatheter Versus Surgically Implanted Aortic Valve Bioprostheses. J. Am. Coll. Cardiol. 2021, 77, 1–14. [Google Scholar] [CrossRef]
- Triche, B.L.; Nelson, J.T.; McGill, N.S.; Porter, K.K.; Sanyal, R.; Tessler, F.N.; McConathy, J.E.; Gauntt, D.M.; Yester, M.V.; Singh, S.P. Recognizing and Minimizing Artifacts at CT, MRI, US, and Molecular Imaging. Radiographics 2019, 39, 1017–1018. [Google Scholar] [CrossRef] [PubMed]
- Faroux, L.; Guimaraes, L.; Wintzer-Wehekind, J.; Junquera, L.; Ferreira-Neto, A.N.; del Val, D.; Muntané-Carol, G.; Mohammadi, S.; Paradis, J.M.; Rodés-Cabau, J. Coronary Artery Disease and Transcatheter Aortic Valve Replacement: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 74, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2021, 143, e72–e227. [Google Scholar] [CrossRef] [PubMed]
- Altibi, A.M.; Hammad, F.; Patel, J.; Song, H.K.; Golwala, H.; Zahr, F.E.; Rahmouni, H. Clinical Outcomes of Revascularization with Percutaneous Coronary Intervention Prior to Transcatheter Aortic Valve Replacement: A Comprehensive Meta-Analysis. Curr. Probl. Cardiol. 2022, 47, 101339. [Google Scholar] [CrossRef]
- Patterson, T.; Clayton, T.; Dodd, M.; Khawaja, Z.; Morice, M.C.; Wilson, K.; Kim, W.K.; Meneveau, N.; Hambrecht, R.; Byrne, J.; et al. ACTIVATION (PercutAneous Coronary inTervention prIor to transcatheter aortic VAlve implantaTION): A Randomized Clinical Trial. JACC Cardiovasc. Interv. 2021, 14, 1965–1974. [Google Scholar] [CrossRef] [PubMed]
- Stefanini, G.G.; Cerrato, E.; Pivato, C.A.; Joner, M.; Testa, L.; Rheude, T.; Pilgrim, T.; Pavani, M.; Brouwer, J.; Lopez Otero, D.; et al. Unplanned Percutaneous Coronary Revascularization After TAVR: A Multicenter International Registry. JACC Cardiovasc. Interv. 2021, 14, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.K.; Pellegrini, C.; Ludwig, S.; Möllmann, H.; Leuschner, F.; Makkar, R.; Leick, J.; Amat-Santos, I.J.; Dörr, O.; Breitbart, P.; et al. Feasibility of Coronary Access in Patients With Acute Coronary Syndrome and Previous TAVR. JACC Cardiovasc. Interv. 2021, 14, 1578–1590. [Google Scholar] [CrossRef]
- de Backer, O.; Landes, U.; Fuchs, A.; Yoon, S.H.; Mathiassen, O.N.; Sedaghat, A.; Kim, W.K.; Pilgrim, T.; Buzzatti, N.; Ruile, P.; et al. Coronary Access after TAVR-in-TAVR as Evaluated by Multidetector Computed Tomography. JACC Cardiovasc. Interv. 2020, 13, 2528–2538. [Google Scholar] [CrossRef] [PubMed]
- Meier, D.; Akodad, M.; Landes, U.; Barlow, A.M.; Chatfield, A.G.; Lai, A.; Tzimas, G.; Tang, G.H.L.; Puehler, T.; Lutter, G.; et al. Coronary Access Following Redo TAVR: Impact of THV Design, Implant Technique, and Cell Misalignment. JACC Cardiovasc. Interv. 2022, 15, 1519–1531. [Google Scholar] [CrossRef]
- Wijesinghe, N.; Ye, J.; Rodés-Cabau, J.; Cheung, A.; Velianou, J.L.; Natarajan, M.K.; Dumont, E.; Nietlispach, F.; Gurvitch, R.; Wood, D.A.; et al. Transcatheter aortic valve implantation in patients with bicuspid aortic valve stenosis. JACC Cardiovasc. Interv. 2010, 3, 1122–1125. [Google Scholar] [CrossRef]
- Mesnier, J.; Panagides, V.; Nuche, J.; Rodés-Cabau, J. Evolving Indications of Transcatheter Aortic Valve Replacement—Where Are We Now, and Where Are We Going. J. Clin. Med. 2022, 11, 3090. [Google Scholar] [PubMed]
- Chen, F.; Xiong, T.; Li, Y.; Wang, X.; Zhu, Z.; Yao, Y.; Ou, Y.; Li, X.; Wei, X.; Zhao, Z.; et al. Risk of Coronary Obstruction During Redo-TAVR in Patients With Bicuspid Versus Tricuspid Aortic Valve Stenosis. JACC Cardiovasc. Interv. 2022, 15, 712–724. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.M.; Dvir, D.; Greenbaum, A.B.; Babaliaros, V.C.; Rogers, T.; Aldea, G.; Reisman, M.; Mackensen, G.B.; Eng, M.H.K.; Paone, G.; et al. Transcatheter Laceration of Aortic Leaflets to Prevent Coronary Obstruction During Transcatheter Aortic Valve Replacement: Concept to First-in-Human. JACC Cardiovasc. Interv. 2018, 11, 677–689. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.M.; Babaliaros, V.C.; Greenbaum, A.B.; Spies, C.; Daniels, D.; Depta, J.P.; Oldemeyer, J.B.; Whisenant, B.; McCabe, J.M.; Muhammad, K.I.; et al. Preventing Coronary Obstruction During Transcatheter Aortic Valve Replacement: Results From the Multicenter International BASILICA Registry. JACC Cardiovasc. Interv. 2021, 14, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Khan, J.M.; Greenbaum, A.B.; Babaliaros, V.C.; Dvir, D.; Reisman, M.; McCabe, J.M.; Satler, L.; Waksman, R.; Eng, M.H.; Paone, G.; et al. BASILICA Trial: One-Year Outcomes of Transcatheter Electrosurgical Leaflet Laceration to Prevent TAVR Coronary Obstruction. Circ. Cardiovasc. Interv. 2021, 14, E010238. [Google Scholar] [CrossRef]
- Greenbaum, A.B.; Kamioka, N.; Vavalle, J.P.; Lisko, J.C.; Gleason, P.T.; Paone, G.; Grubb, K.J.; Bruce, C.G.; Lederman, R.J.; Babaliaros, V.C.; et al. Balloon-Assisted BASILICA to Facilitate Redo TAVR. JACC Cardiovasc. Interv. 2021, 14, 578–580. [Google Scholar] [CrossRef]
- Dvir, D.; Leon, M.B.; Abdel-Wahab, M.; Unbehaun, A.; Kodali, S.; Tchetche, D.; Pibarot, P.; Leipsic, J.; Blanke, P.; Gerckens, U.; et al. First-in-Human Dedicated Leaflet Splitting Device for Prevention of Coronary Obstruction in Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2023, 16, 94–102. [Google Scholar] [CrossRef]
- Tang, G.H.L.; Amat-Santos, I.J.; De Backer, O.; Avvedimento, M.; Redondo, A.; Barbanti, M.; Costa, G.; Tchétché, D.; Eltchaninoff, H.; Kim, W.K.; et al. Rationale, Definitions, Techniques, and Outcomes of Commissural Alignment in TAVR: From the ALIGN-TAVR Consortium. Cardiovasc. Interv. 2022, 15, 1497–1518. [Google Scholar]
- Sá, M.P.; Jacquemyn, X.; Van den Eynde, J.; Tasoudis, P.; Dokollari, A.; Torregrossa, G.; Sicouri, S.; Clavel, M.A.; Pibarot, P.; Ramlawi, B. Impact of Prosthesis-Patient Mismatch After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Imaging 2022, 114, 1612–1619. [Google Scholar] [CrossRef]
- Testa, L.; Casenghi, M.; Criscione, E.; Van Mieghem, N.M.; Tchétché, D.; Asgar, A.W.; De Backer, O.; Latib, A.; Reimers, B.; Stefanini, G.; et al. Prosthesis-patient mismatch following transcatheter aortic valve replacement for degenerated transcatheter aortic valves: The TRANSIT-PPM international project. Front. Cardiovasc. Med. 2022, 9, 931207. [Google Scholar] [CrossRef] [PubMed]
- Sabbagh, A.; Al-Hijji, M.; Guerrero, M. Transcatheter Aortic Valve Implantation for Degenerated Surgical Aortic Bioprosthesis: A Systematic Review. Heart Views 2022, 23, 1–9. [Google Scholar]
- Muralidharan, A.; Thiagarajan, K.; Van Ham, R.; Gleason, T.G.; Mulukutla, S.; Schindler, J.T.; Jeevanantham, V.; Thirumala, P.D. Meta-Analysis of Perioperative Stroke and Mortality in Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2016, 118, 1031–1045. [Google Scholar] [CrossRef] [PubMed]
- Percy, E.D.; Harloff, M.T.; Hirji, S.; McGurk, S.; Yazdchi, F.; Newell, P.; Malarczyk, A.; Sabe, A.; Landes, U.; Webb, J.; et al. Nationally Representative Repeat Transcatheter Aortic Valve Replacement Outcomes: Report From the Centers for Medicare and Medicaid Services. JACC Cardiovasc. Interv. 2021, 14, 1717–1726. [Google Scholar] [CrossRef]
- Popma, J.J.; Deeb, G.M.; Yakubov, S.J.; Mumtaz, M.; Gada, H.; O’Hair, D.; Bajwa, T.; Heiser, J.C.; Merhi, W.; Kleiman, N.S.; et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1706–1715. [Google Scholar] [CrossRef]
- Kapadia, S.R.; Makkar, R.; Leon, M.; Abdel-Wahab, M.; Waggoner, T.; Massberg, S.; Rottbauer, W.; Horr, S.; Sondergaard, L.; Karha, J.; et al. Cerebral Embolic Protection during Transcatheter Aortic-Valve Replacement. N. Engl. J. Med. 2022, 387, 1253–1263. [Google Scholar] [CrossRef]
- Rodés-Cabau, J.; Ellenbogen, K.A.; Krahn, A.D.; Latib, A.; Mack, M.; Mittal, S.; Muntané-Carol, G.; Nazif, T.M.; Sondergaard, L.; Urena, M.; et al. Management of Conduction Disturbances Associated With Transcatheter Aortic Valve Replacement: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 2019, 74, 1086–1106. [Google Scholar] [CrossRef]
- Bruno, F.; D’Ascenzo, F.; Vaira, M.P.; Elia, E.; Omedè, P.; Kodali, S.; Barbanti, M.; Rodès-Cabau, J.; Husser, O.; Sossalla, S.; et al. Predictors of pacemaker implantation after transcatheter aortic valve implantation according to kind of prosthesis and risk profile: A systematic review and contemporary meta-analysis. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Alperi, A.; Rodés-Cabau, J.; Simonato, M.; Tchetche, D.; Charbonnier, G.; Ribeiro, H.B.; Latib, A.; Montorfano, M.; Barbanti, M.; Bleiziffer, S.; et al. Permanent Pacemaker Implantation Following Valve-in-Valve Transcatheter Aortic Valve Replacement: VIVID Registry. J. Am. Coll. Cardiol. 2021, 77, 2263–2273. [Google Scholar] [CrossRef] [PubMed]
- Van Mieghem, N.M.; El Faquir, N.; Rahhab, Z.; Rodríguez-Olivares, R.; Wilschut, J.; Ouhlous, M.; Galema, T.W.; Geleijnse, M.L.; Kappetein, A.P.; Schipper, M.E.; et al. Incidence and predictors of debris embolizing to the brain during transcatheter aortic valve implantation. JACC Cardiovasc. Interv. 2015, 8, 718–724. [Google Scholar] [CrossRef]
- Mangieri, A.; Montalto, C.; Poletti, E.; Sticchi, A.; Crimi, G.; Giannini, F.; Latib, A.; Capodanno, D.; Colombo, A. Thrombotic Versus Bleeding Risk After Transcatheter Aortic Valve Replacement: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 74, 2088–2101. [Google Scholar] [CrossRef]
- Capodanno, D.; Collet, J.P.; Dangas, G.; Montalescot, G.; ten Berg, J.M.; Windecker, S.; Angiolillo, D.J. Antithrombotic Therapy After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2021, 14, 1688–1703. [Google Scholar] [CrossRef]
- Ten Berg, J.; Sibbing, D.; Rocca, B.; Van Belle, E.; Chevalier, B.; Collet, J.P.; Dudek, D.; Gilard, M.; Gorog, D.A.; Grapsa, J.; et al. Management of antithrombotic therapy in patients undergoing transcatheter aortic valve implantation: A consensus document of the ESC Working Group on Thrombosis and the European Association of Percutaneous Cardiovascular Interventions (EAPCI), in collaboration with the ESC Council on Valvular Heart Disease. Eur. Heart J. 2021, 42, 2265–2269. [Google Scholar]
- Dangas, G.D.; Tijssen, J.G.P.; Wöhrle, J.; Søndergaard, L.; Gilard, M.; Möllmann, H.; Makkar, R.R.; Herrmann, H.C.; Giustino, G.; Baldus, S.; et al. A Controlled Trial of Rivaroxaban after Transcatheter Aortic-Valve Replacement. N. Engl. J. Med. 2020, 382, 120–129. [Google Scholar] [CrossRef]
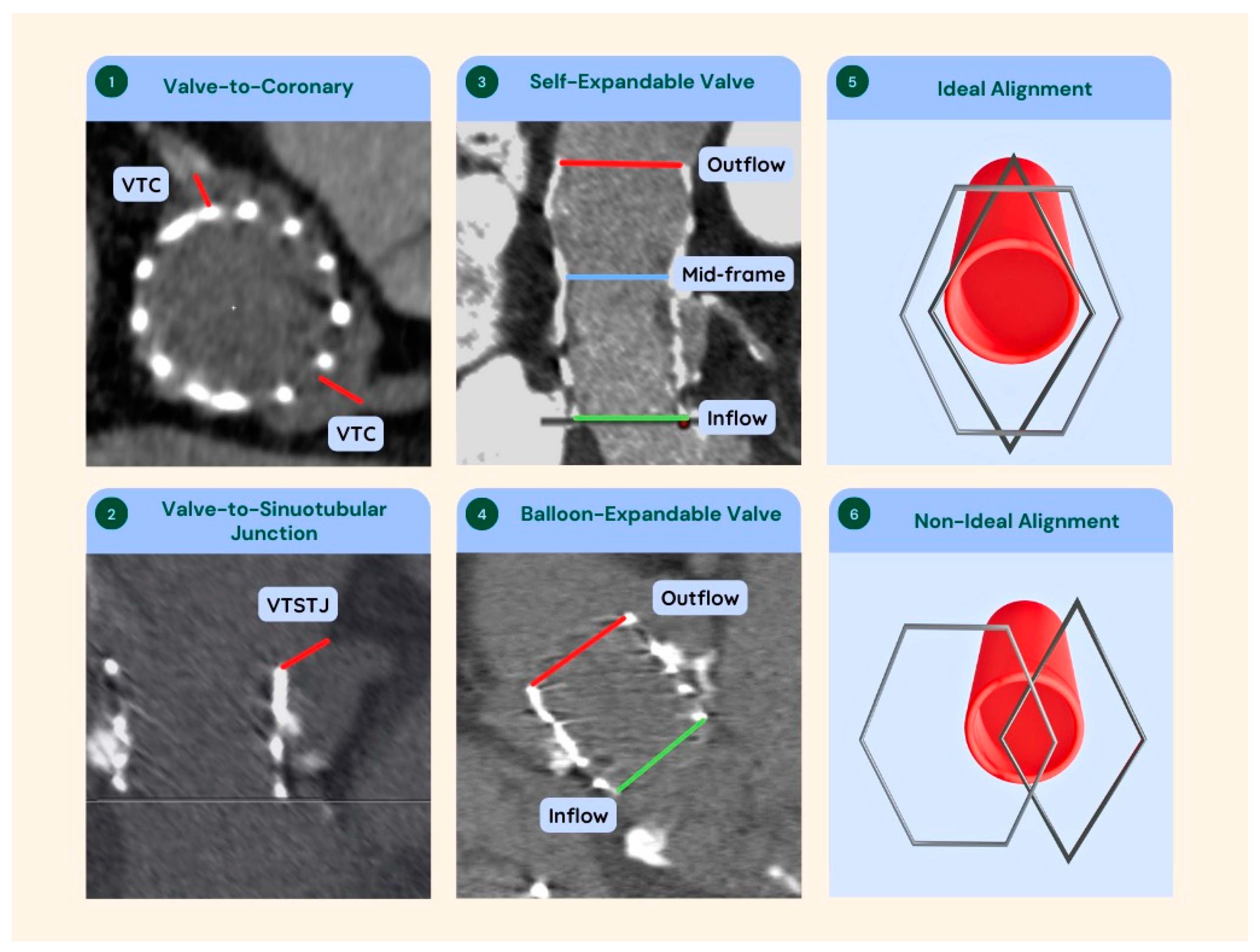
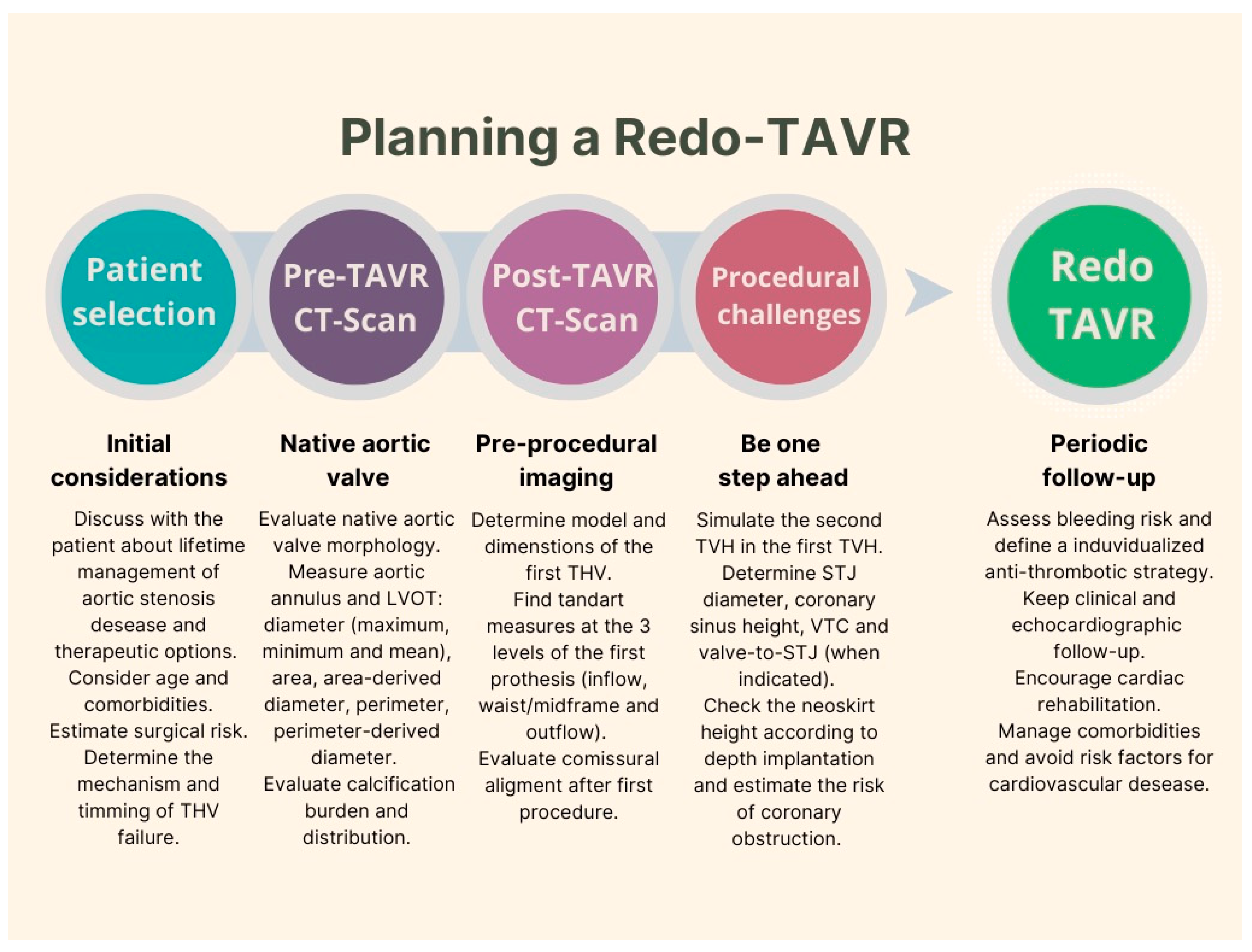
| Analyze native valve images looking for calcification and its distribution, coronary height, bulky calcified leaflets, dilated left ventricular outflow tract (LVOT), and calcified STJ. |
| Before starting the measurements, check for artifacts and adjust image gain, if necessary. |
| Measure the inflow diameter, the middle part, and the outflow diameter of the first prosthesis. Compare these dimensions to the native valve and decide whether the first prosthesis expansion can be optimized. |
| Estimate the size of the neoskirt that will be formed by knowing the height of the leaflets of the first prosthesis and the implantation depth of the second valve. |
| Evaluate the alignment between the coronary ostium and posts of the first prosthesis to predict whether leaflet modification techniques are feasible. |
| Evaluate the height of the coronary ostia in relation to the height of the first valve stent. |
| If the stent is framed below the coronary ostium, measure VTC. If the stent frame is above the coronary ostium, measure VTSTJ. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galhardo, A.; Avvedimento, M.; Mengi, S.; Rodés-Cabau, J. Redo-TAVR: Essential Concepts, Updated Data and Current Gaps in Evidence. J. Clin. Med. 2023, 12, 4788. https://doi.org/10.3390/jcm12144788
Galhardo A, Avvedimento M, Mengi S, Rodés-Cabau J. Redo-TAVR: Essential Concepts, Updated Data and Current Gaps in Evidence. Journal of Clinical Medicine. 2023; 12(14):4788. https://doi.org/10.3390/jcm12144788
Chicago/Turabian StyleGalhardo, Attílio, Marisa Avvedimento, Siddhartha Mengi, and Josep Rodés-Cabau. 2023. "Redo-TAVR: Essential Concepts, Updated Data and Current Gaps in Evidence" Journal of Clinical Medicine 12, no. 14: 4788. https://doi.org/10.3390/jcm12144788
APA StyleGalhardo, A., Avvedimento, M., Mengi, S., & Rodés-Cabau, J. (2023). Redo-TAVR: Essential Concepts, Updated Data and Current Gaps in Evidence. Journal of Clinical Medicine, 12(14), 4788. https://doi.org/10.3390/jcm12144788







