Differences in Involvement of Whole-Body Compensatory Alignment for Decompensated Spinopelvic Sagittal Balance
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Whole-Body Sagittal-Plane Parameters
2.3. Correlations between Lack of Ideal Lumbar Lordosis and Whole-Body Compensation Alignment
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Diebo, B.G.; Varghese, J.J.; Lafage, R.; Schwab, F.J.; Lafage, V. Sagittal alignment of the spine: What do you need to know? Clin. Neurol. Neurosurg. 2015, 139, 295–301. [Google Scholar] [CrossRef]
- Kobayashi, T.; Atsuta, Y.; Matsuno, T.; Takeda, N. A Longitudinal Study of Congruent Sagittal Spinal Alignment in an Adult Cohort. Spine 2004, 29, 671–676. [Google Scholar] [CrossRef]
- Barrey, C.; Roussouly, P.; Le Huec, J.-C.; D’Acunzi, G.; Perrin, G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur. Spine J. 2013, 22, 834–841. [Google Scholar] [CrossRef]
- Le Huec, J.C.; Charosky, S.; Barrey, C.; Rigal, J.; Aunoble, S. Sagittal imbalance cascade for simple degenerative spine and consequences: Algorithm of decision for appropriate treatment. Eur. Spine J. 2011, 20, 699–703. [Google Scholar] [CrossRef]
- Obeid, I.; Hauger, O.; Aunoble, S.; Bourghli, A.; Pellet, N.; Vital, J.-M. Global analysis of sagittal spinal alignment in major deformities: Correlation between lack of lumbar lordosis and flexion of the knee. Eur. Spine J. 2011, 20, 681–685. [Google Scholar] [CrossRef]
- Schwab, F.; Lafage, V.; Patel, A.; Farcy, J.-P. Sagittal plane considerations and the pelvis in the adult patient. Spine 2009, 34, 1828–1833. [Google Scholar] [CrossRef]
- Ferrero, E.; Liabaud, B.; Challier, V.; Lafage, R.; Diebo, B.G.; Vira, S.; Liu, S.; Vital, J.M.; Ilharreborde, B.; Protopsaltis, T.S.; et al. Role of pelvic translation and lower-extremity compensation to maintain gravity line position in spinal deformity. J. Neurosurg. Spine 2016, 24, 436–446. [Google Scholar] [CrossRef]
- Diebo, B.G.; Ferrero, E.; Lafage, R.; Challier, V.; Liabaud, B.; Liu, S.; Vital, J.-M.; Errico, T.J.; Schwab, F.J.; Lafage, V. Recruitment of Compensatory Mechanisms in Sagittal Spinal Malalignment Is Age and Regional Deformity Dependent: A Full-Standing Axis Analysis of Key Radiographical Parameters. Spine 2015, 40, 642–649. [Google Scholar] [CrossRef]
- Protopsaltis, T.; Schwab, F.; Bronsard, N.; Smith, J.S.; Klineberg, E.; Mundis, G.; Ryan, D.J.; Hostin, R.; Hart, R.; Burton, D.; et al. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J. Bone Jt. Surg. 2014, 96, 1631–1640. [Google Scholar] [CrossRef]
- Lafage, R.; Liabaud, B.; Diebo, B.G.; Oren, J.H.; Vira, S.; Pesenti, S.; Protopsaltis, T.S.; Errico, T.J.; Schwab, F.J.; Lafage, V. Defining the role of the lower limbs in compensating for sagittal malalignment. Spine 2017, 42, E1282–E1288. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Ungar, B.; Blondel, B.; Buchowski, J.; Coe, J.; Deinlein, D.; DeWald, C.; Mehdian, H.; Shaffrey, C.; Tribus, C.; et al. Scoliosis Research Society—Schwab adult spinal deformity classification: A validation study. Spine 2012, 37, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry disability index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef] [PubMed]
- Aoki, Y.; Nakajima, A.; Takahashi, H.; Sonobe, M.; Terajima, F.; Saito, M.; Takahashi, K.; Ohtori, S.; Watanabe, A.; Nakajima, T.; et al. Influence of pelvic incidence-lumbar lordosis mismatch on surgical outcomes of short-segment transforaminal lumbar interbody fusion. BMC Musculoskelet. Disord. 2015, 16, 213. [Google Scholar] [CrossRef]
- Lamartina, C.; Berjano, P. Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur. Spine J. 2014, 23, 1177–1189. [Google Scholar] [CrossRef]
- Hasegawa, K.; Okamoto, M.; Hatsushikano, S.; Watanabe, K.; Ohashi, M.; Vital, J.-M.; Dubousset, J. Compensation for standing posture by whole-body sagittal alignment in relation to health-related quality of life. Bone Jt. J. 2020, 102, 1359–1367. [Google Scholar] [CrossRef]
- Jalai, C.M.; Cruz, D.L.; Diebo, B.G.; Poorman, G.; Lafage, R.; Bess, S.; Ramchandran, S.; Day, L.M.; Vira, S.; Liabaud, B.; et al. Full-Body Analysis of Age-Adjusted Alignment in Adult Spinal Deformity Patients and Lower-Limb Compensation. Spine 2017, 42, 653–661. [Google Scholar] [CrossRef]
- Aubin, C.-E.; Bellefleur, C.; Joncas, J.; de Lanauze, D.; Kadoury, S.; Blanke, K.; Parent, S.; Labelle, H. Reliability and Accuracy Analysis of a New Semiautomatic Radiographic Measurement Software in Adult Scoliosis. Spine 2011, 36, E780–E790. [Google Scholar] [CrossRef]
- Legaye, J. The femoro-sacral posterior angle: An anatomical sagittal pelvic parameter usable with dome-shaped sacrum. Eur. Spine J. 2007, 16, 219–225. [Google Scholar] [CrossRef]
- Murata, Y.; Takahashi, K.; Yamagata, M.; Hanaoka, E.; Moriya, H. The knee-spine syndrome: Association between lumbar lordosis and extension of the knee. J. Bone Joint Surg. Br. 2003, 85, 95–99. [Google Scholar] [CrossRef]
- Tsukagoshi, R.; Tateuchi, H.; Fukumoto, Y.; Akiyama, H.; So, K.; Kuroda, Y.; Okumura, H.; Ichihashi, N. Factors associated with restricted hip extension during gait in women after total hip arthroplasty. HIP Int. 2015, 25, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Ouchida, J.; Nakashima, H.; Kanemura, T.; Satake, K.; Ando, K.; Ito, K.; Tsushima, M.; Machino, M.; Ito, S.; Yamaguchi, H.; et al. Impact of the hip joint mobility on whole-body sagittal alignment: Prospective analysis in case with hip arthroplasty. Eur. Spine J. 2022, 31, 2399–2407. [Google Scholar] [CrossRef]
| Overall | Compensated (Group C) | Decompensated (Group D) | p | |
|---|---|---|---|---|
| Cases, n | 294 | 253 | 41 | |
| Age, years | 58.0 ± 12.7 | 56.7 ± 12.8 | 65.7 ± 9.5 | <0.001 |
| Sex, Male, % | 176 (59.9%) | 151 (59.9%) | 25 (61.0%) | |
| Height, cm | 161.8 ± 9.1 | 162.2 ± 9.1 | 159.3 ± 9.0 | 0.043 |
| Weight, kg | 59.8 ± 12.1 | 60.1 ± 12.3 | 57.8 ± 10.0 | 0.254 |
| BMI, kg/m2 | 22.5 ± 4.0 | 22.5 ± 4.0 | 22.7 ± 3.4 | 0.858 |
| ODIscore, % | 11.0 ± 10.2 | 10.1 ± 9.7 | 16.8 ± 11.4 | 0.001 |
| Radiographical parameters | ||||
| O-C2 angle, degrees | 16.4 ± 7.9 | 16.3 ± 8.0 | 16.8 ± 7.0 | 0.990 |
| C2–7 lordotic angle, degrees | 2.3 ± 11.4 | 1.3 ± 11.3 | 8.2 ± 10.2 | <0.001 |
| T1-slope, degrees | 24.1 ± 8.7 | 23.3 ± 8.6 | 29.2 ± 8.2 | <0.001 |
| TK (T1–12), degrees | 40.5 ± 12.0 | 41.1 ± 11.9 | 36.8 ± 11.7 | 0.061 |
| LL (L1-S1), degrees | 45.7 ± 13.6 | 47.4 ± 12.0 | 35.3 ± 18.1 | <0.001 |
| lack of iLL, degrees | −12.6 ± 12.5 | −10.4 ± 10.2 | −26.3 ± 15.9 | <0.001 |
| SS, degrees | 33.7 ± 9.5 | 34.2 ± 8.8 | 30.7 ± 12.7 | 0.066 |
| PT, degrees | 15.1 ± 8.0 | 14.2 ± 7.1 | 20.9 ± 10.2 | <0.001 |
| PI, degrees | 49.3 ± 10.9 | 48.8 ± 10.5 | 52.6 ± 12.8 | 0.109 |
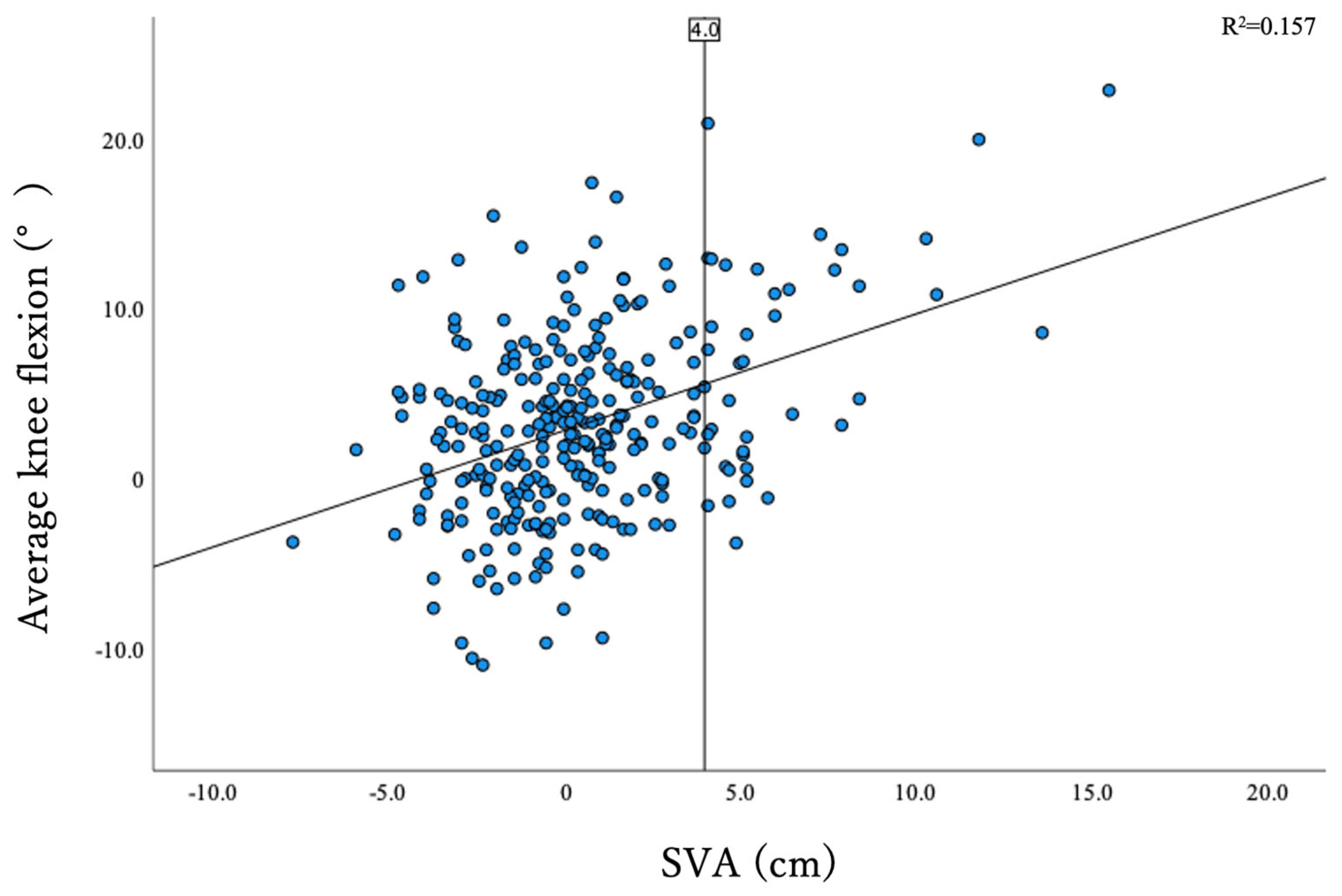
| KneeFlex, degrees | 3.2 ± 5.5 | 2.5 ± 5.0 | 7.3 ± 6.5 | <0.001 |
| AA, degrees | 5.5 ± 3.1 | 5.3 ± 3.0 | 6.6 ± 3.3 | 0.028 |
| SVA, cm | 0.5 ± 3.2 | −0.4 ± 2.1 | 6.2 ± 2.7 | <0.001 |
| CAM-HA, cm | −1.7 ± 3.5 | −2.4 ± 2.9 | 2.5 ± 3.9 | <0.001 |
| CAM-knee offset, cm | 0.2 ± 3.2 | −0.2 ± 2.9 | 2.9 ± 3.8 | <0.001 |
| CAM-ankle offset, cm | 3.3 ± 3.3 | 2.7 ± 3.0 | 6.8 ± 3.4 | <0.001 |
| TPA, degrees | 11.0 ± 8.3 | 9.3 ± 6.5 | 21.0 ± 11.0 | <0.001 |
| Compensated (Group C) | ||||||||
| O-C2 Angle | C2–7 Lordotic Angle | T1-Slope | TK(T1–12) | SS | PT | KF | AA | |
| Pearson’s Correlation Coefficient | 0.002 | −0.017 | 0.016 | 0.275 ** | 0.267 ** | −0.723 ** | −0.153 * | −0.129 * |
| p | 0.978 | 0.782 | 0.795 | <0.001 | <0.001 | <0.001 | 0.015 | 0.040 |
| Decompensated (Group D) | ||||||||
| O-C2 Angle | C2–7 Lordotic Angle | T1-Slope | TK(T1–12) | SS | PT | KF | AA | |
| Pearson’s Correlation Coefficient | 0.088 | −0.297 | −0.180 | 0.462 ** | 0.577 ** | −0.796 ** | −0.415 ** | −0.334 * |
| p | 0.585 | 0.059 | 0.261 | 0.002 | <0.001 | <0.001 | 0.007 | 0.033 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ouchida, J.; Nakashima, H.; Kanemura, T.; Ito, K.; Tsushima, M.; Machino, M.; Ito, S.; Segi, N.; Ode, Y.; Imagama, S. Differences in Involvement of Whole-Body Compensatory Alignment for Decompensated Spinopelvic Sagittal Balance. J. Clin. Med. 2023, 12, 4690. https://doi.org/10.3390/jcm12144690
Ouchida J, Nakashima H, Kanemura T, Ito K, Tsushima M, Machino M, Ito S, Segi N, Ode Y, Imagama S. Differences in Involvement of Whole-Body Compensatory Alignment for Decompensated Spinopelvic Sagittal Balance. Journal of Clinical Medicine. 2023; 12(14):4690. https://doi.org/10.3390/jcm12144690
Chicago/Turabian StyleOuchida, Jun, Hiroaki Nakashima, Tokumi Kanemura, Kenyu Ito, Mikito Tsushima, Masaaki Machino, Sadayuki Ito, Naoki Segi, Yukihito Ode, and Shiro Imagama. 2023. "Differences in Involvement of Whole-Body Compensatory Alignment for Decompensated Spinopelvic Sagittal Balance" Journal of Clinical Medicine 12, no. 14: 4690. https://doi.org/10.3390/jcm12144690
APA StyleOuchida, J., Nakashima, H., Kanemura, T., Ito, K., Tsushima, M., Machino, M., Ito, S., Segi, N., Ode, Y., & Imagama, S. (2023). Differences in Involvement of Whole-Body Compensatory Alignment for Decompensated Spinopelvic Sagittal Balance. Journal of Clinical Medicine, 12(14), 4690. https://doi.org/10.3390/jcm12144690






