Length of Stay in Emergency Department by ICD-10 Specific and Non-Specific Diagnoses: A Single-Centre Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Methods
2.4. Statistical Analysis
3. Results
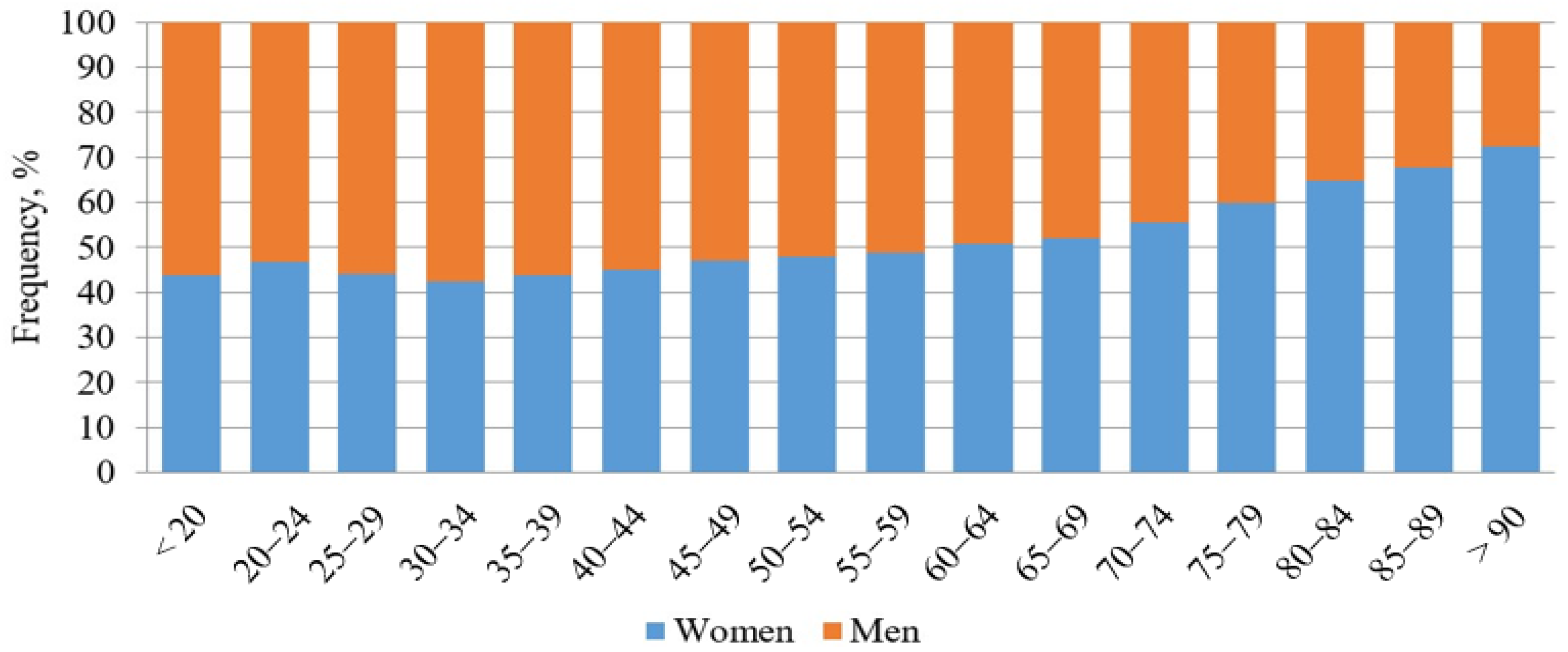
3.1. Baseline Characteristics
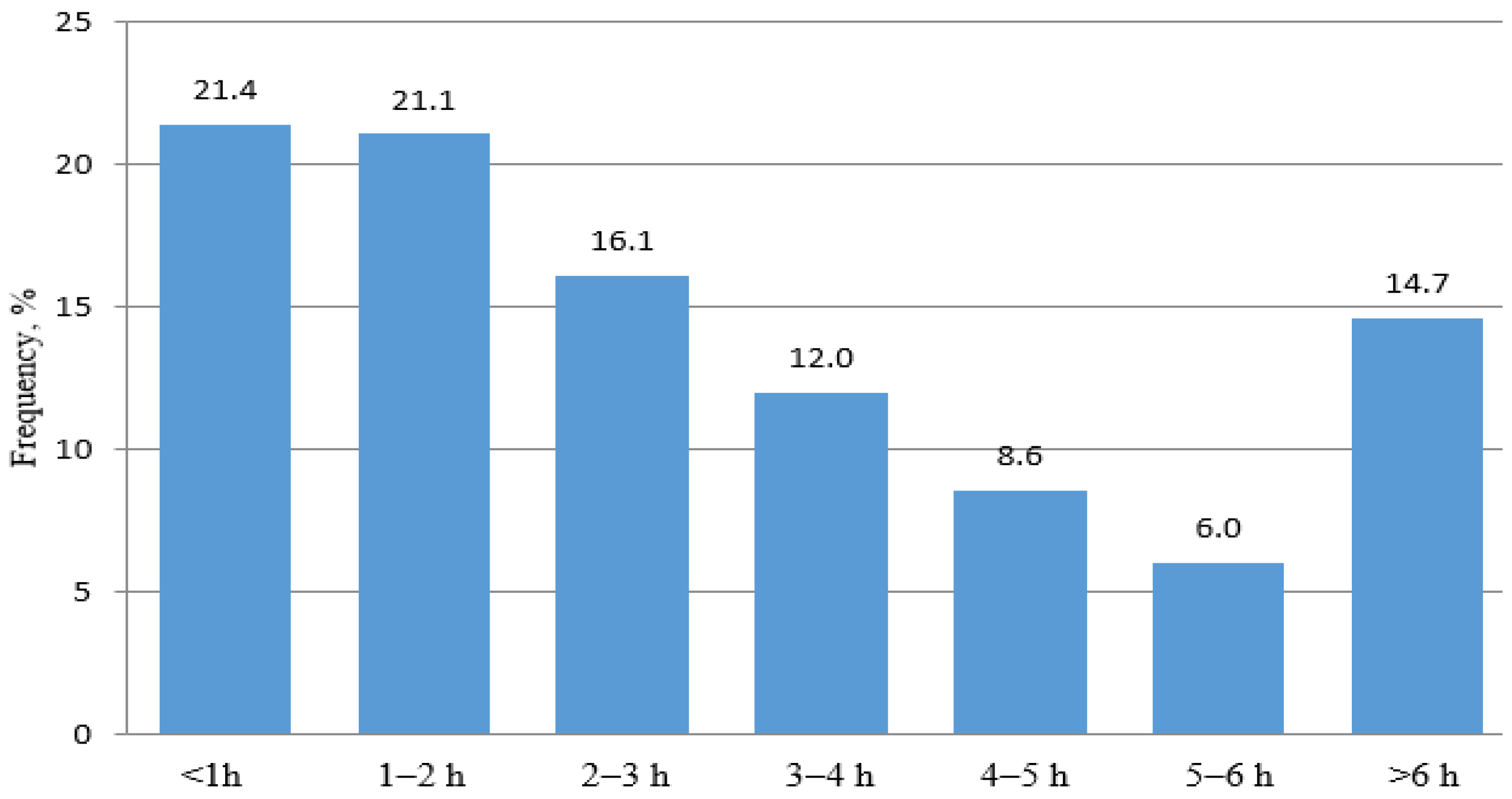
3.2. Analysis of LOS
3.3. LOS in the Specific and Non-Specific Groups
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wiler, J.L.; Welch, S.; Pines, J.; Schuur, J.; Jouriles, N.; Stone-Grifth, S. Emergency department performance measures updates: Proceedings of the 2014 emergency department benchmarking alliance consensus summit. Acad. Emerg. Med. 2015, 22, 542–553. [Google Scholar] [CrossRef] [PubMed]
- Kelen, G.D.; Wolfe, R.; D’Onofrio, G.; Mills, A.M.; Diercks, D.; Stern, S.A.; Wadman, M.C.; Sokolove, P.E. Emergency department crowding: The canary in the health care system. NEJM Catal. 2021, 2, 1–26. [Google Scholar]
- Newman-Toker, D.E.; Peterson, S.M.; Badihian, S.; Hassoon, A.; Nassery, N.; Parizadeh, D.; Wilson, L.M.; Jia, Y.; Omron, R.; Tharmarajah, S.; et al. Diagnostic Errors in the Emergency Department: A Systematic Review. Comparative Effectiveness Review No. 258; Prepared by the Johns Hopkins University Evidence-based Practice Center under Contract No. 75Q80120D00003; AHRQ Publication No. 22(23)-EHC043; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2022. [CrossRef]
- Howlett, M.; Doody, K.; Murray, J.; LeBlanc-Duchin, D.; Fraser, J.; Atkinson, P.R. Burnout in emergency department healthcare professionals is associated with coping style: A cross-sectional survey. Emerg. Med. J. 2015, 32, 722–727. [Google Scholar] [CrossRef]
- Perimal-Lewis, L.; Ben-Tovim, D.I.; Li, J.Y.; Hakendorf, P.; Thompson, C. Emergency department lengths of stay: Characteristics favouring a delay to the admission decision as distinct from a delay while awaiting an inpatient bed. Intern. Med. J. 2014, 44, 384–389. [Google Scholar] [CrossRef]
- Horng, S.; Joseph, J.W.; Calder, S.; Stevens, J.P.; O’Donoghue, A.L.; Safran, C.; Nathanson, L.A.; Leventhal, E.L. Assessment of unintentional duplicate orders by emergency department clinicians before and after implementation of a visual aid in the electronic health record ordering system. JAMA Netw. Open 2019, 2, e1916499. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, A.K.; Hajdasz, D.; Rothenberg, C.; Dashevsky, M.; Parwani, V.; Sevilla, M.; Shapiro, M.; Schwartz, I. Reducing unnecessary blood chemistry testing in the emergency department: Implementation of choosing wisely. Am. J. Med. Qual. 2018, 33, 81–85. [Google Scholar] [CrossRef]
- Ahmed, A.A.; Ibro, S.A.; Melkamu, G.; Seid, S.S.; Tesfaye, T. Length of stay in the emergency department and its associated factors at Jimma Medical Center, Southwest Ethiopia. Open Access Emerg. Med. 2020, 12, 227–235. [Google Scholar] [CrossRef]
- Wong, H.J.; Morra, D. Excellent hospital care for all: Open and operating 24/7. J. Gen. Intern. Med. 2011, 26, 1050–1052. [Google Scholar] [CrossRef]
- Mchomvu, E.; Mbunda, G.; Simon, N.; Kitila, F.; Temba, Y.; Msumba, I.; Namamba, J.; Kilindimo, S.; Mgubike, H.; Gingo, W.; et al. Diagnoses made in an emergency department in rural sub-Saharan Africa. Swiss Med. Wkly. 2019, 149, w20018. [Google Scholar] [CrossRef]
- Al-Mashat, H.; Lindskou, T.A.; Møller, J.M.; Ludwig, M.; Christensen, E.F.; Søvsø, M.B. Assessed and discharged—Diagnosis, mortality and revisits in short-term emergency department contacts. BMC Health Serv. Res. 2022, 22, 816. [Google Scholar] [CrossRef]
- Hooker, E.A.; Mallow, P.; Oglesby, M. Characteristics and trends of emergency department visits in the United States (2010–2014). J. Emerg. Med. 2019, 56, 344–351. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Otto, R.; Blaschke, S.; Schirrmeister, W.; Drynda, S.; Walcher, F.; Greiner, F. Length of stay as quality indicator in emergency departments: Analysis of determinants in the German Emergency Department Data Registry (AKTIN registry). Intern. Emerg. Med. 2022, 17, 1199–1209. [Google Scholar] [CrossRef]
- Kemp, K.; Mertanen, R.; Lääperi, M.; Niemi-Murola, L.; Lehtonen, L.; Castren, M. Nonspecific complaints in the emergency department—A systematic review. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 6. [Google Scholar] [CrossRef] [PubMed]
- Scott, I.; Sullivan, C.; Staib, A.; Bell, A. Deconstructing the 4-h rule for access to emergency care and putting patients first. Aust. Health Rev. 2018, 42, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Mason, S.; Weber, E.J.; Coster, J.; Freeman, J.; Locker, T. Time patients spend in the emergency department: England’s 4-h rule-a case of hitting the target but missing the point? Ann. Emerg. Med. 2012, 59, 341–349. [Google Scholar] [CrossRef]
- Mortimore, A.; Cooper, S. The “4-h target”: Emergency nurses’ views. Emerg. Med. J. 2007, 6, 402–404. [Google Scholar] [CrossRef]
- Tenbensel, T.; Chalmers, L.; Jones, P.; Appleton-Dyer, S.; Walton, L.I.; Ameratunga, S. New Zealand’s emergency department target—Did it reduce ED length of stay, and if so, how and when? BMC Health Serv. Res. 2017, 17, 678. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2019 Emergency Department Summary Tables. Available online: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2019-nhamcs-ed-web-tables-508.pdf (accessed on 26 March 2023).
- European Society for Emergency Medicine. European Medicine in Numbers. Epidemiology Series 1.0. LGCAST (2020 July). Available online: https://eusem.org/images/1_epidemiology_series.pdf (accessed on 30 March 2023).
- Szwamel, K.; Kurpas, D. Analysis of the structure of medical services branch of the hospital emergency ward with special reference to the benefits provided to patient with minor injuries. Fam. Med. Primary Care Rev. 2015, 17, 124–130. [Google Scholar]
- Australian Institute of Health and Welfare, Emergency Department Care Activity. Available online: https://www.aihw.gov.au/reports-data/myhospitals/intersection/activity/ed (accessed on 30 June 2023).
- Birrenbach, T.; Hoffmann, M.; Hautz, S.C.; Kämmer, J.E.; Exadaktylos, A.K.; Sauter, T.C.; Müller, M.; Hautz, W. Frequency and predictors of unspecific medical diagnoses in the emergency department: A prospective observational study. BMC Emerg. Med. 2022, 22, 109. [Google Scholar] [CrossRef]
- Wogan, J.M. ED follow-up: A comparison of admission and discharge diagnoses. Am. J. Emerg. Med. 2001, 19, 249–251. [Google Scholar] [CrossRef]
- Yang, Z.; Song, K.; Lin, H.; Li, C.; Ding, N. Factors associated with emergency department length of stay in critically ill patients: A single-center retrospective study. Med. Sci. Monit. 2021, 27, e931286. [Google Scholar] [CrossRef]
- van der Veen, D.; Remeijer, C.; Fogteloo, A.J.; Heringhaus, C.; de Groot, B. Independent determinants of prolonged emergency department length of stay in a tertiary care centre: A prospective cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 81. [Google Scholar] [CrossRef]
- Lee, K.S.; Min, H.S.; Moon, J.Y.; Lim, D.; Kim, Y.; Ko, E.; Kim, Y.S.; Kim, J.; Lee, J.; Sung, H.K. Patient and hospital characteristics predict prolonged emergency department length of stay and in-hospital mortality: A nationwide analysis in Korea. BMC Emerg. Med. 2022, 22, 183. [Google Scholar] [CrossRef]
- Kaushik, N.; Khangulov, V.S.; O’Hara, M.; Arnaout, R. Reduction in laboratory turnaround time decreases emergency room length of stay. Open Access Emerg. Med. 2018, 20, 37–45. [Google Scholar] [CrossRef]
- Tudela, P.; Carreres, A.; Ballester, M. Diagnostic errors in emergency departments. Med. Clin. 2017, 149, 170–175. [Google Scholar] [CrossRef]
- Paling, S.; Lambert, J.; Clouting, J.; González-Esquerré, J.; Auterson, T. Waiting times in emergency departments: Exploring the factors associated with longer patient waits for emergency care in England using routinely collected daily data. Emerg. Med. J. 2020, 37, 781–786. [Google Scholar] [CrossRef]
| Internal Medicine | Surgical | Traumatic | Neurological | Non-Specific | |||||
|---|---|---|---|---|---|---|---|---|---|
| ICD-10 | n | ICD-10 | n | ICD-10 | n | ICD-10 | n | ICD-10 | n |
| I10 | 2061 | R10 | 3040 | T92 | 2548 | R51 | 1764 | Z03.8 | 1395 |
| R10.4 | 1287 | S61 | 2330 | T93 | 1955 | R42 | 1074 | Z76.9 | 1392 |
| R19.8 | 979 | S52 | 1760 | S02 | 1747 | R55 | 952 | R42 | 1074 |
| R07 | 866 | S63 | 1533 | S90 | 1546 | G40.0 | 764 | R51 | 1001 |
| D38 | 575 | S93 | 1292 | S00 | 1523 | I63 | 716 | R10 | 946 |
| J18 | 538 | M54 | 1280 | S60 | 1444 | I64 | 608 | R11 | 942 |
| I48 | 486 | M23 | 935 | M70 | 1312 | R29 | 528 | R55 | 938 |
| I50 | 268 | S83 | 930 | S01 | 1103 | M47 | 512 | R07 | 865 |
| E05 | 189 | M17 | 740 | S40 | 420 | G54 | 506 | R53 | 820 |
| J15 | 122 | S80 | 669 | S43 | 340 | G44 | 486 | R06.4 | 610 |
| J45.9 | 108 | S92 | 598 | T00 | 308 | G98 | 310 | R04.0 | 509 |
| I25 | 102 | S66 | 521 | S09 | 201 | R26 | 309 | Z76.8 | 235 |
| Group | n | Age (Years) | F/M (%) | LOS, Mean ± SD (min) | LOS, Median (IQR) (min) | Hospitalizations (%) |
|---|---|---|---|---|---|---|
| Internal medicine | 11,476 | 63.6 ± 25 | 58/42 | 318.5 ± 255 | 228 (103–309) | 17.7 |
| Surgical | 18,510 | 58.8 ± 23 | 51/49 | 196.3 ± 187 | 132 (45–171) | 8.8 |
| Traumatic | 18,310 | 41.7 ± 22 | 39/61 | 160.1 ± 164 | 99 (23–169) | 7.1 |
| Neurological | 11,534 | 62.6 ± 26 | 48/52 | 345.0 ± 253 | 237 (65–336) | 21.5 |
| Non-specific | 15,826 | 56.9 ± 26 | 52/48 | 185.4 ± 191 | 141 (70–217) | 29.3 |
| All | 134,675 | 52.4 ± 23 | 50/50 | 254.0 ± 205 | 212 (93–251) | 22.0 |
| Group | Hospitalization | No Hospitalization | p | ||
|---|---|---|---|---|---|
| n | LOS (min) | n | LOS (min) | ||
| Internal medicine | 2031 | 311.5 ± 229 | 9445 | 321.4 ± 262 | 0.111 |
| Surgical | 1629 | 189.2 ± 169 | 16,881 | 201.6 ± 187 | 0.010 |
| Traumatic | 1300 | 158.2 ± 140 | 17,010 | 166.1 ± 159 | 0.082 |
| Neurological | 2480 | 343.3 ± 243 | 9054 | 349.0 ± 257 | 0.321 |
| Non-specific | 4637 | 180.4 ± 179 | 11,189 | 189.2 ± 181 | 0.024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miazgowski, B.; Pakulski, C.; Miazgowski, T. Length of Stay in Emergency Department by ICD-10 Specific and Non-Specific Diagnoses: A Single-Centre Retrospective Study. J. Clin. Med. 2023, 12, 4679. https://doi.org/10.3390/jcm12144679
Miazgowski B, Pakulski C, Miazgowski T. Length of Stay in Emergency Department by ICD-10 Specific and Non-Specific Diagnoses: A Single-Centre Retrospective Study. Journal of Clinical Medicine. 2023; 12(14):4679. https://doi.org/10.3390/jcm12144679
Chicago/Turabian StyleMiazgowski, Bartosz, Cezary Pakulski, and Tomasz Miazgowski. 2023. "Length of Stay in Emergency Department by ICD-10 Specific and Non-Specific Diagnoses: A Single-Centre Retrospective Study" Journal of Clinical Medicine 12, no. 14: 4679. https://doi.org/10.3390/jcm12144679
APA StyleMiazgowski, B., Pakulski, C., & Miazgowski, T. (2023). Length of Stay in Emergency Department by ICD-10 Specific and Non-Specific Diagnoses: A Single-Centre Retrospective Study. Journal of Clinical Medicine, 12(14), 4679. https://doi.org/10.3390/jcm12144679





