Non-Specific Inhibition of Dipeptidyl Peptidases 8/9 by Dipeptidyl Peptidase 4 Inhibitors Negatively Affects Mesenchymal Stem Cell Differentiation
Abstract
1. Introduction
2. Materials and Methods
2.1. MSC Culture and Differentiation
2.2. Vildagliptin, Sitagliptin or 1G244 Treatments
2.3. Dipeptidyl Peptidase Activity
2.4. MTT Assay for Cell Viability
2.5. Apoptosis Assay
2.6. Mineralized Extracellular-Matrix (Osteoblasts) and Lipid Droplet (Adipocytes) Staining
2.7. Quantification of Gene Expression by Quantitative Real-Time PCR
2.8. Western Blot
2.9. Statistical Analyses
3. Results
3.1. Dipeptidyl Peptidase Activity in Culture Media
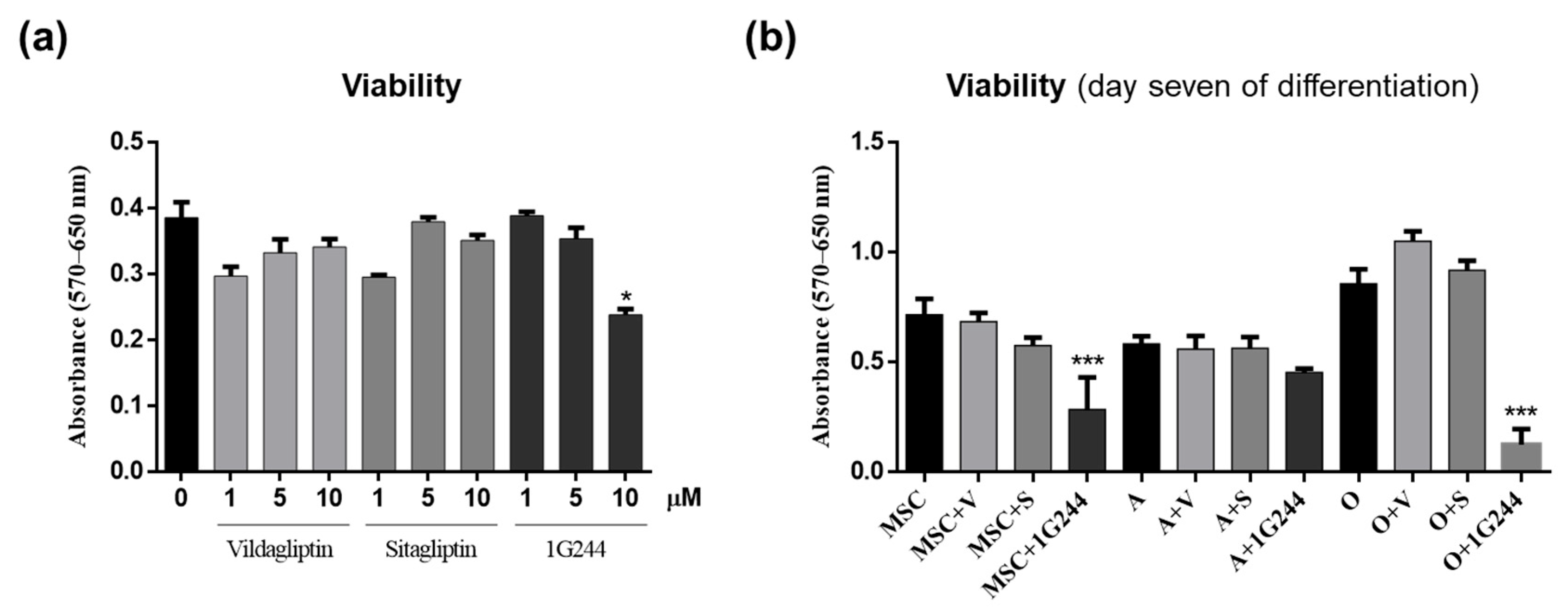
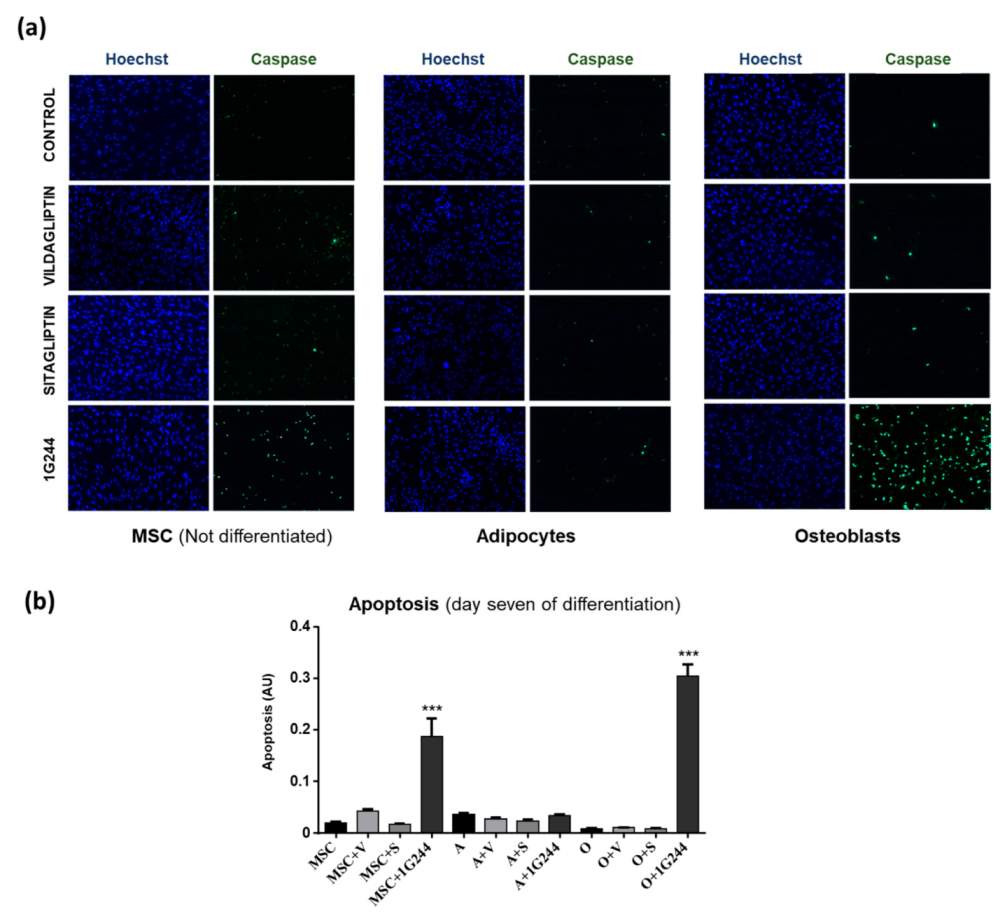
3.2. Effect of DPP4 and DPP8/9 Inhibition on MCS Viability and Apoptosis
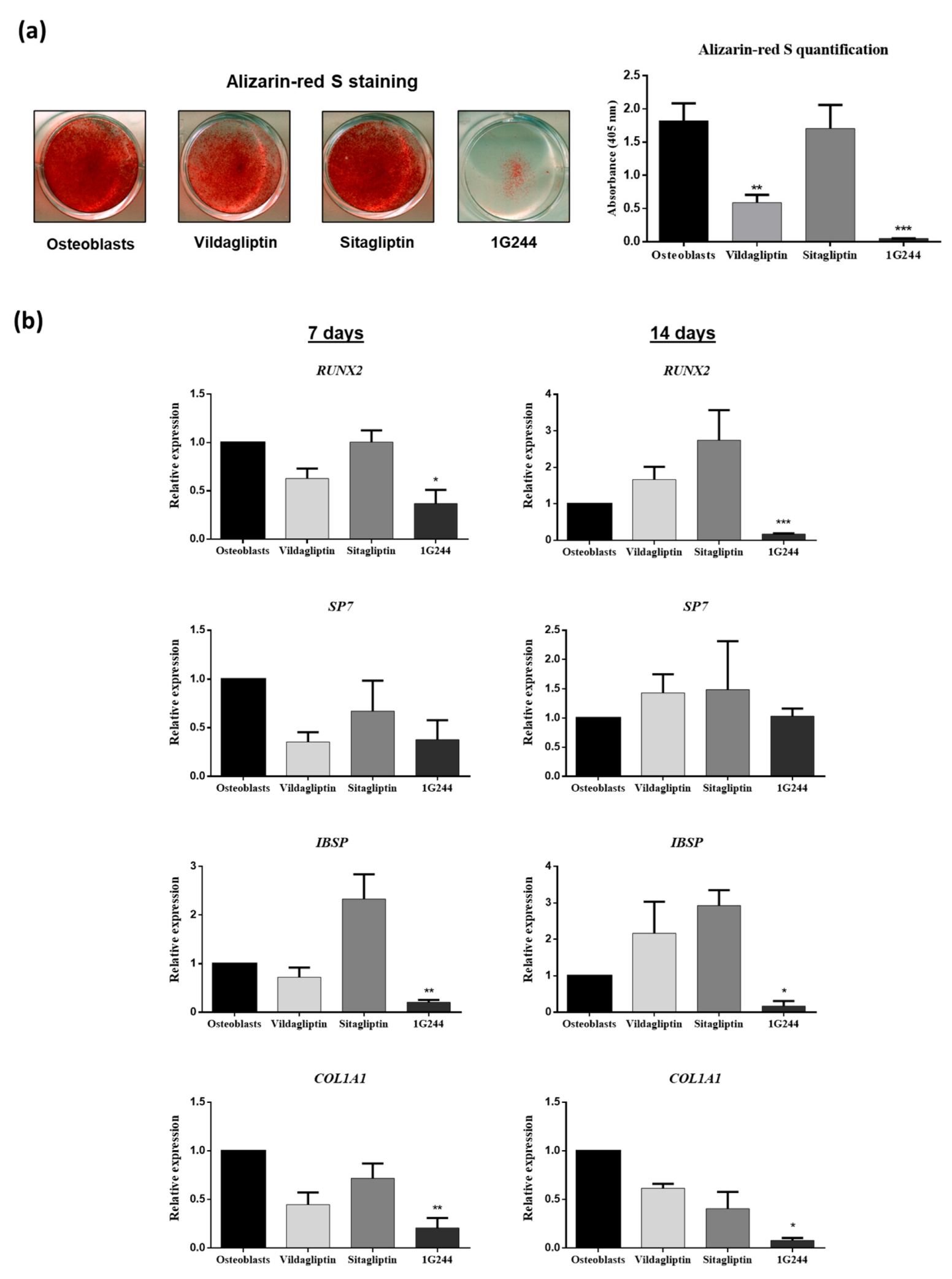
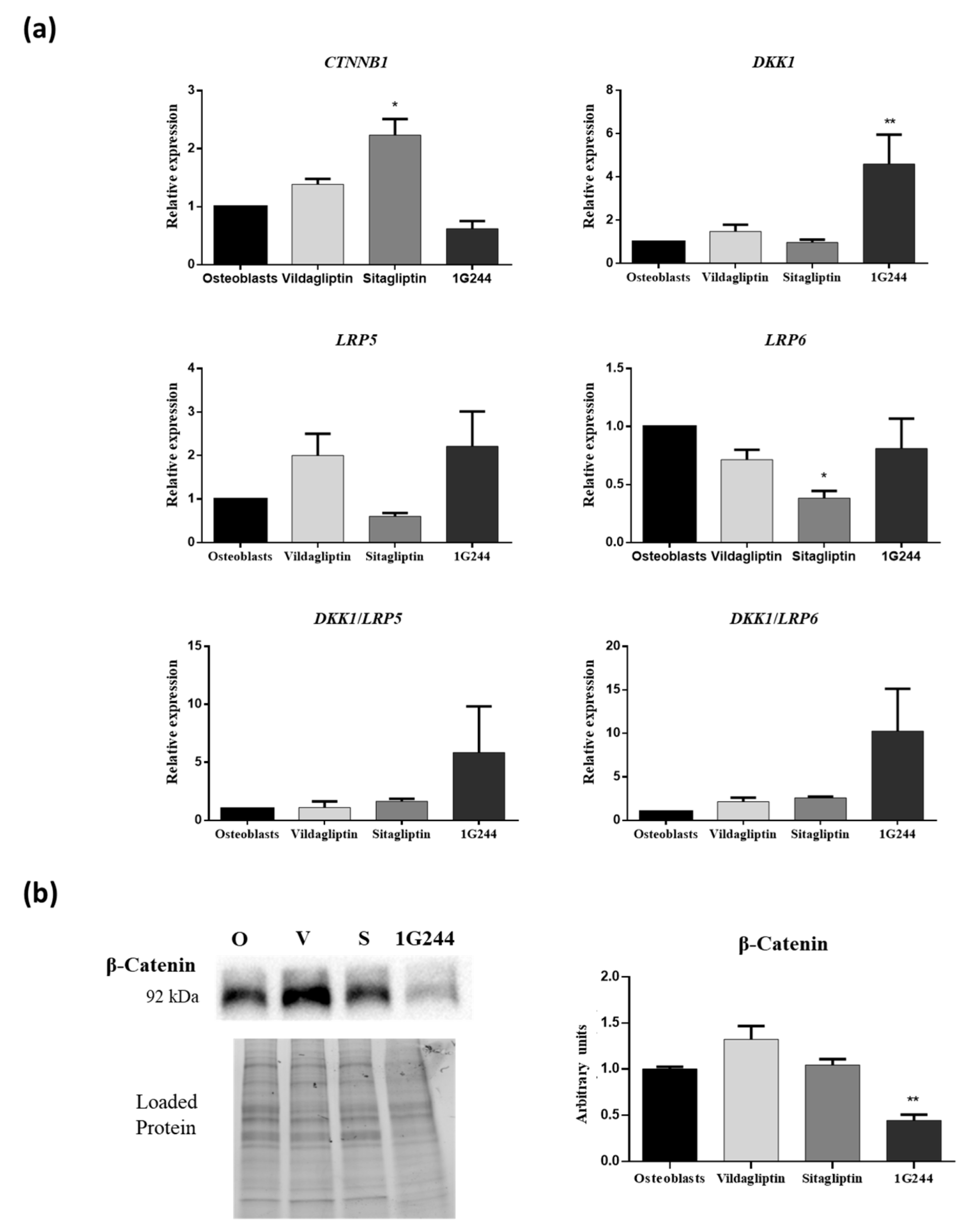
3.3. Effect of DPP4 and DPP8/9 Inhibition on Osteoblastic Differentiation
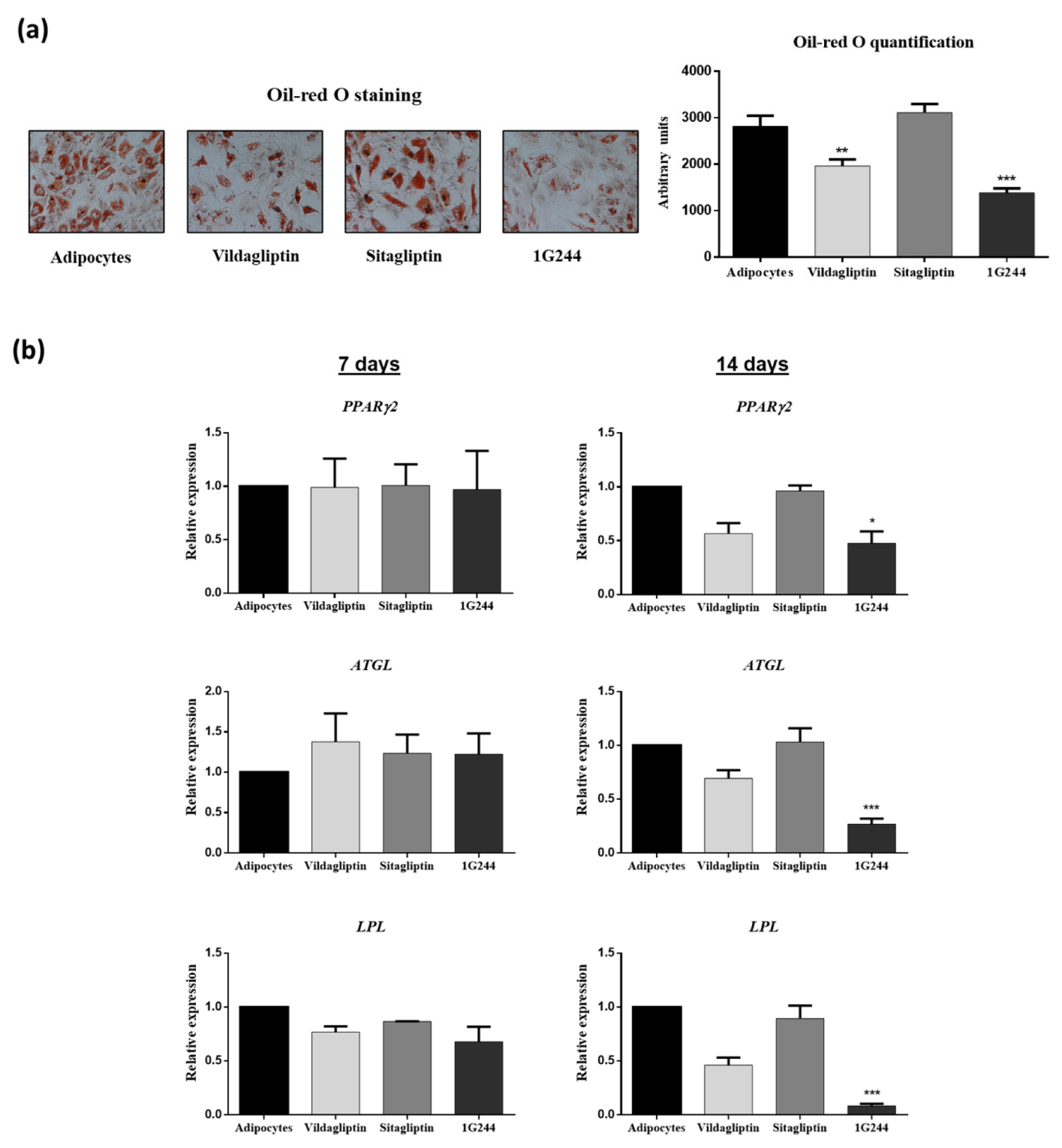
3.4. Effect of Vildagliptin, Sitagliptin or 1G244 on Adipogenic Differentiation
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhong, J.; Rao, X.; Rajagopalan, S. An emerging role of dipeptidyl peptidase 4 (DPP4) beyond glucose control: Potential implications in cardiovascular disease. Atherosclerosis 2013, 226, 305–314. [Google Scholar] [CrossRef]
- Rosmaninho-Salgado, J.; Marques, A.P.; Estrada, M.; Santana, M.; Cortez, V.; Grouzmann, E.; Cavadas, C. Dipeptidyl-peptidase-IV by cleaving neuropeptide y induces lipid accumulation and PPAR-γ expression. Peptides 2012, 37, 49–54. [Google Scholar] [CrossRef]
- Röhrborn, D.; Wronkowitz, N.; Eckel, J. DPP4 in diabetes. Front. Immunol. 2015, 6, 386. [Google Scholar] [CrossRef]
- Boer, G.A.; Holst, J.J. Incretin hormones and type 2 diabetes—Mechanistic insights and therapeutic approaches. Biology 2020, 9, 473. [Google Scholar] [CrossRef] [PubMed]
- Deacon, C.F. Dipeptidyl peptidase 4 inhibitors in the treatment of type 2 diabetes mellitus. Nat. Rev. Endocrinol. 2020, 16, 642–653. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; D’Alessio, D.A.; Fradkin, J.; Kernan, W.N.; Mathieu, C.; Mingrone, G.; Rossing, P.; Tsapas, A.; Wexler, D.J.; Buse, J.B. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the european association for the study of diabetes (EASD). Diabetes Care 2018, 41, 2669–2701. [Google Scholar] [CrossRef]
- Avogaro, A.; Fadini, G.P. The pleiotropic cardiovascular effects of dipeptidyl peptidase-4 inhibitors. Br. J. Clin. Pharmacol. 2018, 84, 1686–1695. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Guo, L.; Xing, J.; Li, P.; Sang, H.; Hu, X.; Du, Y.; Zhao, L.; Song, R.; Gu, H. The protective role of DPP4 inhibitors in atherosclerosis. Eur. J. Pharmacol. 2020, 875, 173037. [Google Scholar] [CrossRef]
- Yang, Y.; Zhao, C.; Liang, J.; Yu, M.; Qu, X. Effect of dipeptidyl peptidase-4 inhibitors on bone metabolism and the possible underlying mechanisms. Front. Pharmacol. 2017, 8, 487. [Google Scholar] [CrossRef]
- Nicotera, R.; Casarella, A.; Longhitano, E.; Bolignano, D.; Andreucci, M.; De Sarro, G.; Cernaro, V.; Russo, E.; Coppolino, G. Antiproteinuric effect of DPP-IV inhibitors in diabetic and non-diabetic kidney diseases. Pharmacol. Res. 2020, 159, 105019. [Google Scholar] [CrossRef]
- Torrecillas-Baena, B.; Gálvez-Moreno, M.Á.; Quesada-Gómez, J.M.; Dorado, G.; Casado-Díaz, A. Influence of Dipeptidyl Peptidase-4 (DPP4) on Mesenchymal Stem-Cell (MSC) Biology: Implications for Regenerative Medicine—Review. Stem Cell Rev. Rep. 2022, 18, 56–76. [Google Scholar] [CrossRef]
- Merrick, D.; Sakers, A.; Irgebay, Z.; Okada, C.; Calvert, C.; Morley, M.P.; Percec, I.; Seale, P. Identification of a mesenchymal progenitor cell hierarchy in adipose tissue. Science 2019, 364, 6438. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.M.; Yang, Y.J.; Wu, Y.J.; Zhang, Q.; Qian, H.Y. Attenuating Hypoxia-Induced Apoptosis and Autophagy of Mesenchymal Stem Cells: The Potential of Sitagliptin in Stem Cell-Based Therapy. Cell. Physiol. Biochem. 2015, 37, 1914–1926. [Google Scholar] [CrossRef]
- Shi, C. Recent progress toward understanding the physiological function of bone marrow mesenchymal stem cells. Immunology 2012, 136, 133–138. [Google Scholar] [CrossRef]
- Huang, S.; Leung, V.; Peng, S.; Li, L.; Lu, F.J.; Wang, T.; Lu, W.; Cheung, K.M.C.; Zhou, G. Developmental Definition of MSCs: New Insights Into Pending Questions. Cell. Reprogram. 2011, 13, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.; Horwitz, E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Casado-Díaz, A.; Quesada-Gómez, J.M.; Dorado, G. Stem Cell Research and Molecular Markers in Medicine. In Reference Module in Biomedical Sciences; Elsevier: Amsterdam, The Netherlands, 2016; ISBN 9780128012383. [Google Scholar]
- Sui, B.D.; Hu, C.H.; Zheng, C.X.; Jin, Y. Microenvironmental views on mesenchymal stem cell differentiation in aging. J. Dent. Res. 2016, 95, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Baek, K.H.; Lee, S.Y.; Ahn, S.H.; Lee, S.H.; Koh, J.M.; Rhee, Y.; Kim, C.H.; Kim, D.Y.; Kang, M.I.; et al. Association of circulating dipeptidyl-peptidase 4 levels with osteoporotic fracture in postmenopausal women. Osteoporos. Int. 2017, 28, 1099–1108. [Google Scholar] [CrossRef]
- Zheng, T.; Yang, L.; Liu, Y.; Liu, H.; Yu, J.; Zhang, X.; Qin, S. Plasma DPP4 activities are associated with osteoporosis in postmenopausal women with normal glucose tolerance. J. Clin. Endocrinol. Metab. 2015, 100, 3862–3870. [Google Scholar] [CrossRef]
- Qiu, M.; Zhai, S.; Liu, D. DPP4 activities are associated with osteopenia/osteoporosis and fracture risk in newly diagnosed type 2 diabetes. Int. J. Endocrinol. 2020, 2020, 8874272. [Google Scholar] [CrossRef]
- Kirby, M.; Yu, D.M.T.; O’Connor, S.P.; Gorrell, M.D. Inhibitor selectivity in the clinical application of dipeptidyl peptidase-4 inhibition. Clin. Sci. 2010, 118, 31–41. [Google Scholar] [CrossRef]
- Olsen, C.; Wagtmann, N. Identification and characterization of human DPP9, a novel homologue of dipeptidyl peptidase IV. Gene 2002, 299, 185–193. [Google Scholar] [CrossRef]
- Zhang, H.; Chen, Y.; Keane, F.M.; Gorrell, M.D. Advances in understanding the expression and function of dipeptidyl peptidase 8 and 9. Mol. Cancer Res. 2013, 11, 1487–1496. [Google Scholar] [CrossRef] [PubMed]
- Cui, C.; Tian, X.; Wei, L.; Wang, Y.; Wang, K.; Fu, R. New insights into the role of dipeptidyl peptidase 8 and dipeptidyl peptidase 9 and their inhibitors. Front. Pharmacol. 2022, 13, 1002871. [Google Scholar] [CrossRef] [PubMed]
- Casado-Díaz, A.; Santiago-Mora, R.; Jiménez, R.; Caballero-Villarraso, J.; Herrera, C.; Torres, A.; Dorado, G.; Quesada-Gómez, J.M. Cryopreserved human bone marrow mononuclear cells as a source of mesenchymal stromal cells: Application in osteoporosis research. Cytotherapy 2008, 10, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Bjelke, J.R.; Christensen, J.; Nielsen, P.F.; Branner, S.; Kanstrup, A.B.; Wagtmann, N.; Rasmussen, H.B. Dipeptidyl peptidases 8 and 9: Specificity and molecular characterization compared with dipeptidyl peptidase IV. Biochem. J. 2006, 396, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Gürtler, A.; Kunz, N.; Gomolka, M.; Hornhardt, S.; Friedl, A.A.; McDonald, K.; Kohn, J.E.; Posch, A. Stain-Free technology as a normalization tool in Western blot analysis. Anal. Biochem. 2013, 433, 105–111. [Google Scholar] [CrossRef]
- Gilda, J.E.; Gomes, A.V. Stain-Free total protein staining is a superior loading control to b-actin for Western blots. Anal. Biochem. 2013, 440, 186–188. [Google Scholar] [CrossRef]
- Ambrosi, T.H.; Scialdone, A.; Graja, A.; Gohlke, S.; Jank, A.M.; Bocian, C.; Woelk, L.; Fan, H.; Logan, D.W.; Schürmann, A.; et al. Adipocyte Accumulation in the Bone Marrow during Obesity and Aging Impairs Stem Cell-Based Hematopoietic and Bone Regeneration. Cell Stem Cell 2017, 20, 771–784.e6. [Google Scholar] [CrossRef]
- De Paula, F.J.A.; Horowitz, M.C.; Rosen, C.J. Novel insights into the relationship between diabetes and osteoporosis. Diabetes Metab. Res. Rev. 2010, 26, 622–630. [Google Scholar] [CrossRef]
- Klemann, C.; Wagner, L.; Stephan, M.; von Hörsten, S. Cut to the chase: A review of CD26/dipeptidyl peptidase-4′s (DPP4) entanglement in the immune system. Clin. Exp. Immunol. 2016, 185, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Lankas, G.R.; Leiting, B.; Roy, R.S.; Eiermann, G.J.; Beconi, M.G.; Biftu, T.; Chan, C.; Edmondson, S.; Feeney, W.P.; He, H.; et al. Dipeptidyl peptidase IV inhibition for the treatment of type 2 diabetes: Potential importance of selectivity over dipeptidyl peptidases 8 and 9. Diabetes 2005, 54, 2988–2994. [Google Scholar] [CrossRef] [PubMed]
- Burkey, B.F.; Hoffmann, P.K.; Hassiepen, U.; Trappe, J.; Juedes, M.; Foley, J.E. Adverse effects of dipeptidyl peptidases 8 and 9 inhibition in rodents revisited. Diabetes Obes. Metab. 2008, 10, 1057–1061. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.J.; Tang, H.K.; Yeh, T.K.; Chen, C.M.; Shy, H.S.; Chu, Y.R.; Chien, C.H.; Tsai, T.Y.; Huang, Y.C.; Huang, Y.L.; et al. Biochemistry, pharmacokinetics, and toxicology of a potent and selective DPP8/9 inhibitor. Biochem. Pharmacol. 2009, 78, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Minoux, M.; Piaia, A.; Kueng, B.; Gapp, B.; Weber, D.; Haller, C.; Barbieri, S.; Namoto, K.; Lorenz, T.; et al. DPP9 enzyme activity controls survival of mouse migratory tongue muscle progenitors and its absence leads to neonatal lethality due to suckling defect. Dev. Biol. 2017, 431, 297–308. [Google Scholar] [CrossRef] [PubMed]
- Gabrilovac, J.; Čupić, B.; Zapletal, E.; Kraus, O.; Jakić-Razumović, J. Dipeptidyl peptidase 9 (DPP9) in human skin cells. Immunobiology 2017, 222, 327–342. [Google Scholar] [CrossRef]
- Matheeussen, V.; Waumans, Y.; Martinet, W.; Van Goethem, S.; Van Der Veken, P.; Scharpé, S.; Augustyns, K.; De Meyer, G.R.Y.; De Meester, I. Dipeptidyl peptidases in atherosclerosis: Expression and role in macrophage differentiation, activation and apoptosis. Basic Res. Cardiol. 2013, 108, 350. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, F.; Wu, K.; Wu, W.; Wu, H.; Zhang, W. Targeting dipeptidyl peptidase 8 genes inhibits proliferation, migration and invasion by inhibition of cyclin D1 and MMP2MMP9 signal pathway in cervical cancer. J. Gene Med. 2018, 20, e3056. [Google Scholar] [CrossRef] [PubMed]
- Finger, Y.; Habich, M.; Gerlich, S.; Urbanczyk, S.; Logt, E.; Koch, J.; Schu, L.; Lapacz, K.J.; Ali, M.; Petrungaro, C.; et al. Proteasomal degradation induced by DPP9-mediated processing competes with mitochondrial protein import. EMBO J. 2020, 39, e103889. [Google Scholar] [CrossRef]
- Kim, H.; Lee, H.J.; Oh, Y.; Choi, S.G.; Hong, S.H.; Kim, H.J.; Lee, S.Y.; Choi, J.W.; Su Hwang, D.; Kim, K.S.; et al. The DUSP26 phosphatase activator adenylate kinase 2 regulates FADD phosphorylation and cell growth. Nat. Commun. 2014, 5, 3351. [Google Scholar] [CrossRef]
- Qian, S.W.; Li, X.; Zhang, Y.Y.; Huang, H.Y.; Liu, Y.; Sun, X.; Tang, Q.Q. Characterization of adipocyte differentiation from human mesenchymal stem cells in bone marrow. BMC Dev. Biol. 2010, 10, 47. [Google Scholar] [CrossRef] [PubMed]
- Gomathi, K.; Akshaya, N.; Srinaath, N.; Moorthi, A.; Selvamurugan, N. Regulation of Runx2 by post-translational modifications in osteoblast differentiation. Life Sci. 2020, 245, 117389. [Google Scholar] [CrossRef] [PubMed]
- Komori, T. Regulation of bone development and maintenance by Runx2. Front. Biosci. 2008, 13, 898–903. [Google Scholar] [CrossRef]
- Veis, A.; Dorvee, J.R. Biomineralization mechanisms: A new paradigm for crystal nucleation in organic matrices. Calcif. Tissue Int. 2013, 93, 307–315. [Google Scholar] [CrossRef]
- Shao, H.; Wu, R.; Cao, L.; Gu, H.; Chai, F. Trelagliptin stimulates osteoblastic differentiation by increasing runt-related transcription factor 2 (RUNX2): A therapeutic implication in osteoporosis. Bioengineered 2021, 12, 960–968. [Google Scholar] [CrossRef]
- Wang, Q.; Xie, X.; Zhang, D.; Mao, F.; Wang, S.; Liao, Y. Saxagliptin enhances osteogenic differentiation in MC3T3-E1 cells, dependent on the activation of AMP-activated protein kinase α (AMPKα)/runt-related transcription factor-2 (Runx-2). Bioengineered 2022, 13, 431–439. [Google Scholar] [CrossRef]
- Dong, C.; Yang, H.; Wang, Y.; Yan, X.; Li, D.; Cao, Z.; Ning, Y.; Zhang, C. Anagliptin stimulates osteoblastic cell differentiation and mineralization. Biomed. Pharmacother. 2020, 129, 109796. [Google Scholar] [CrossRef]
- Huan, Y.; Jiang, Q.; Liu, J.L.; Shen, Z.F. Establishment of a dipeptidyl peptidases (DPP) 8/9 expressing cell model for evaluating the selectivity of DPP4 inhibitors. J. Pharmacol. Toxicol. Methods 2015, 71, 8–12. [Google Scholar] [CrossRef]
- Sbaraglini, M.L.; Molinuevo, M.S.; Sedlinsky, C.; Schurman, L.; McCarthy, A.D. Saxagliptin affects long-bone microarchitecture and decreases the osteogenic potential of bone marrow stromal cells. Eur. J. Pharmacol. 2014, 727, 8–14. [Google Scholar] [CrossRef]
- Cortet, B.; Lucas, S.; Legroux-Gerot, I.; Penel, G.; Chauveau, C.; Paccou, J. Bone disorders associated with diabetes mellitus and its treatments. Jt. Bone Spine 2019, 86, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Hwang, J.S. Impact of Type 2 Diabetes Mellitus and Antidiabetic Medications on Bone Metabolism. Curr. Diabetes Rep. 2020, 20, 78. [Google Scholar] [CrossRef]
- Bunck, M.C.; Poelma, M.; Eekhoff, E.M.; Schweizer, A.; Heine, R.J.; Nijpels, G.; Foley, J.E.; Diamant, M. Effects of vildagliptin on postprandial markers of bone resorption and calcium homeostasis in recently diagnosed, well-controlled type 2 diabetes patients. J. Diabetes 2012, 4, 181–185. [Google Scholar] [CrossRef]
- Glorie, L.; D’Haese, P.C.; Verhulst, A. Boning up on DPP4, DPP4 substrates, and DPP4-adipokine interactions: Logical reasoning and known facts about bone related effects of DPP4 inhibitors. Bone 2016, 92, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.V. Diabetes, bone and glucose-lowering agents: Clinical outcomes. Diabetologia 2017, 60, 1170–1179. [Google Scholar] [CrossRef]
- Charoenphandhu, N.; Suntornsaratoon, P.; Sa-Nguanmoo, P.; Tanajak, P.; Teerapornpuntakit, J.; Aeimlapa, R.; Chattipakorn, N.; Chattipakorn, S. Dipeptidyl Peptidase-4 Inhibitor, Vildagliptin, Improves Trabecular Bone Mineral Density and Microstructure in Obese, Insulin-Resistant, Pre-Diabetic Rats. Can. J. Diabetes 2018, 42, 545–552. [Google Scholar] [CrossRef]
- Kanda, J.; Furukawa, M.; Izumo, N.; Shimakura, T.; Yamamoto, N.; Takahashi, H.E.; Wakabayashi, H. Effects of the linagliptin, dipeptidyl peptidase-4 inhibitor, on bone fragility induced by type 2 diabetes mellitus in obese mice. Drug Discov. Ther. 2020, 14, 218–225. [Google Scholar] [CrossRef]
- Ferrari, S.L.; Abrahamsen, B.; Napoli, N.; Akesson, K.; Chandran, M.; Eastell, R.; El-Hajj Fuleihan, G.; Josse, R.; Kendler, D.L.; Kraenzlin, M.; et al. Diagnosis and management of bone fragility in diabetes: An emerging challenge. Osteoporos. Int. 2018, 29, 2585–2596. [Google Scholar] [CrossRef] [PubMed]
- Han, R.; Wang, X.; Bachovchin, W.; Zukowska, Z.; Osborn, J.W. Inhibition of dipeptidyl peptidase 8/9 impairs preadipocyte differentiation. Sci. Rep. 2015, 5, 12348. [Google Scholar] [CrossRef] [PubMed]
- Powell, D.R.; Revelli, J.P.; Doree, D.D.; Dacosta, C.M.; Desai, U.; Shadoan, M.K.; Rodriguez, L.; Mullens, M.; Yang, Q.M.; Ding, Z.M.; et al. High-throughput screening of mouse gene knockouts identifies established and novel high body fat phenotypes. Diabetes Metab. Syndr. Obes. 2021, 14, 3753–3785. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Maqsudi, S.; Rainczuk, A.; Duffield, N.; Lawrence, J.; Keane, F.M.; Justa-Schuch, D.; Geiss-Friedlander, R.; Gorrell, M.D.; Stephens, A.N. Identification of novel dipeptidyl peptidase 9 substrates by two-dimensional differential in-gel electrophoresis. FEBS J. 2015, 282, 3737–3757. [Google Scholar] [CrossRef]
- Hatzmann, F.M.; Großmann, S.; Waldegger, P.; Wiegers, G.J.; Mandl, M.; Rauchenwald, T.; Pierer, G.; Zwerschke, W. Dipeptidyl peptidase-4 cell surface expression marks an abundant adipose stem/progenitor cell population with high stemness in human white adipose tissue. Adipocyte 2022, 11, 601–615. [Google Scholar] [CrossRef]
- Zilleßen, P.; Celner, J.; Kretschmann, A.; Pfeifer, A.; Racké, K.; Mayer, P. Metabolic role of dipeptidyl peptidase 4 (DPP4) in primary human (pre)adipocytes. Sci. Rep. 2016, 6, 23074. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Gall, M.G.; Zhang, H.; Keane, F.M.; McCaughan, G.W.; Yu, D.M.T.; Gorrell, M.D. Dipeptidyl peptidase 9 enzymatic activity influences the expression of neonatal metabolic genes. Exp. Cell Res. 2016, 342, 72–82. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Long, F. Notch signaling suppresses glucose metabolism in mesenchymal progenitors to restrict osteoblast differentiation. J. Clin. Investig. 2018, 128, 5573–5586. [Google Scholar] [CrossRef] [PubMed]
- Casado-Díaz, A.; Anter, J.; Müller, S.; Winter, P.; Quesada-Gómez, J.M.; Dorado, G. Transcriptomic Analyses of Adipocyte Differentiation From Human Mesenchymal Stromal-Cells (MSC). J. Cell Physiol. 2017, 232, 771–784. [Google Scholar] [CrossRef]
- Yuan, Z.; Li, Q.; Luo, S.; Liu, Z.; Luo, D.; Zhang, B.; Zhang, D.; Rao, P.; Xiao, J. PPARγ; and Wnt Signaling in Adipogenic and Osteogenic Differentiation of Mesenchymal Stem Cells. Curr. Stem Cell Res. Ther. 2016, 11, 216–225. [Google Scholar] [CrossRef]
- de Winter, T.J.J.; Nusse, R. Running Against the Wnt: How Wnt/β-Catenin Suppresses Adipogenesis. Front. Cell Dev. Biol. 2021, 9, 627429. [Google Scholar] [CrossRef]
- Clevers, H.; Nusse, R. Wnt/β-Catenin Signaling and Disease. Cell 2012, 149, 1192–1205. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.L.; Khoo, P.L.; de Young, R.A.; Steiner, K.; Wilcock, C.; Mukhopadhyay, M.; Westphal, H.; Jamieson, R.V.; Robb, L.; Tam, P.P.L. Dkk1 and Wnt3 interact to control head morphogenesis in the mouse. Development 2008, 135, 1791–1801. [Google Scholar] [CrossRef]
- Ren, X.; Zhu, R.; Liu, G.; Xue, F.; Wang, Y.; Xu, J.; Zhang, W.; Yu, W.; Li, R. Effect of sitagliptin on tubulointerstitial Wnt/β-catenin signalling in diabetic nephropathy. Nephrology 2019, 24, 1189–1197. [Google Scholar] [CrossRef]
- Li, B.; Luo, Y.R.; Zhang, Q.; Fu, S.H.; Chen, Y.D.; Tian, J.W.; Guo, Y. Sitagliptin, a dipeptidyl peptidase-4 inhibitor, attenuates apoptosis of vascular smooth muscle cells and reduces atherosclerosis in diabetic apolipoprotein E–deficient mice. Vasc. Pharmacol. 2021, 140, 106854. [Google Scholar] [CrossRef] [PubMed]
- Bagchi, D.P.; Nishii, A.; Li, Z.; DelProposto, J.B.; Corsa, C.A.; Mori, H.; Hardij, J.; Learman, B.S.; Lumeng, C.N.; MacDougald, O.A. Wnt/β-catenin signaling regulates adipose tissue lipogenesis and adipocyte-specific loss is rigorously defended by neighboring stromal-vascular cells. Mol. Metab. 2020, 42, 101078. [Google Scholar] [CrossRef] [PubMed]


| Gene | Primer Sequence (5′→3′) | Amplicon (bp) |
|---|---|---|
| Runt-related transcription factor 2 (RUNX2) | TGGTTAATCTCCGCAGGTCAC ACTGTGCTGAAGAGGCTGTTTG | 143 |
| Osterix (SP7) | AGCCAGAAGCTGTGAAACCTC AGCTGCAAGCTCTCCATAACC | 163 |
| Collagen, type I, alpha I (COL1A1) | CGCTGGCCCCAAAGGATCTCCTG GGGGTCCGGGAACACCTCGCTC | 263 |
| Integrin-binding sialoprotein (IBSP) | AGGGCAGTAGTGACTCATCCG CGTCCTCTCCATAGCCCAGTGTTG | 171 |
| Peroxisome proliferator-activated receptor gamma 2 (PPARG2) | GCGATTCCTTCACTGATACACTG GAGTGGGAGTGGTCTTCCATTAC | 136 |
| Patatin-like phospholipase domain containing 2 (ATGL) | CCAACACCAGCATCCAGTTCA ATCCCTGCTTGCACATCTCTC | 102 |
| Lipoprotein lipase (LPL) | AAGAAGCAGCAAAATGTACCTGAAG CCTGATTGGTATGGGTTTCACTC | 113 |
| Catenin beta 1 (CTNNB1) | AGCTGGTGGGCTGCAGAAAATG ACAATAGCCGGCTTATTACTAGAGC | 249 |
| Dickkopf1 (DKK1) | ATGCGTCACGCTATGTGCT GGAATACCCATCCAAGGTGCTA | 144 |
| LDL receptor-related protein 5 (LRP5) | TACTGGACAGACTGGCAGACC GTGTAGAAAGGCTCGCTTGG | 209 |
| LDL receptor-related protein 6 (LRP6) | TACTGGCCAAATGGACTGACT TGTTGCAAGCCAAAATGGAGT | 211 |
| Polymerase (RNA; DNA directed) II polypeptide A (POLR2A) | TTTTGGTGACGACTTGAACTGC CCATCTTGTCCACCACCTCTTC | 125 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torrecillas-Baena, B.; Camacho-Cardenosa, M.; Quesada-Gómez, J.M.; Moreno-Moreno, P.; Dorado, G.; Gálvez-Moreno, M.Á.; Casado-Díaz, A. Non-Specific Inhibition of Dipeptidyl Peptidases 8/9 by Dipeptidyl Peptidase 4 Inhibitors Negatively Affects Mesenchymal Stem Cell Differentiation. J. Clin. Med. 2023, 12, 4632. https://doi.org/10.3390/jcm12144632
Torrecillas-Baena B, Camacho-Cardenosa M, Quesada-Gómez JM, Moreno-Moreno P, Dorado G, Gálvez-Moreno MÁ, Casado-Díaz A. Non-Specific Inhibition of Dipeptidyl Peptidases 8/9 by Dipeptidyl Peptidase 4 Inhibitors Negatively Affects Mesenchymal Stem Cell Differentiation. Journal of Clinical Medicine. 2023; 12(14):4632. https://doi.org/10.3390/jcm12144632
Chicago/Turabian StyleTorrecillas-Baena, Bárbara, Marta Camacho-Cardenosa, José Manuel Quesada-Gómez, Paloma Moreno-Moreno, Gabriel Dorado, María Ángeles Gálvez-Moreno, and Antonio Casado-Díaz. 2023. "Non-Specific Inhibition of Dipeptidyl Peptidases 8/9 by Dipeptidyl Peptidase 4 Inhibitors Negatively Affects Mesenchymal Stem Cell Differentiation" Journal of Clinical Medicine 12, no. 14: 4632. https://doi.org/10.3390/jcm12144632
APA StyleTorrecillas-Baena, B., Camacho-Cardenosa, M., Quesada-Gómez, J. M., Moreno-Moreno, P., Dorado, G., Gálvez-Moreno, M. Á., & Casado-Díaz, A. (2023). Non-Specific Inhibition of Dipeptidyl Peptidases 8/9 by Dipeptidyl Peptidase 4 Inhibitors Negatively Affects Mesenchymal Stem Cell Differentiation. Journal of Clinical Medicine, 12(14), 4632. https://doi.org/10.3390/jcm12144632








