No Success without Effort: Follow-Up at Six Years after Implementing a Benchmarking and Feedback Concept for Postoperative Pain after Total Hip Arthroplasty
Abstract
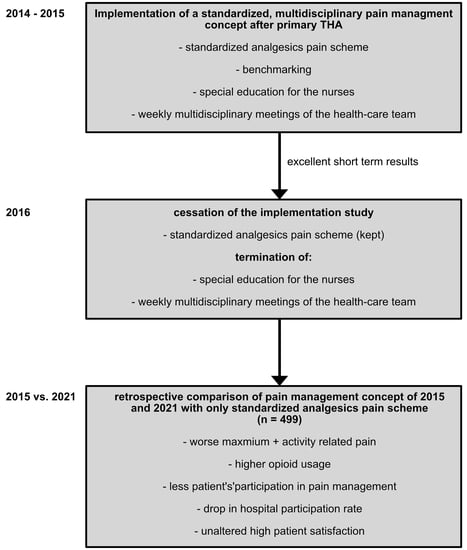
1. Introduction
Aim of This Study
2. Methods
2.1. Initially Established Pain Management Concept
2.2. Cessation of the Implementation Study
2.3. QUIPS Project—Benchmarking and Feedback Concept
2.4. Statistical Analysis
3. Results
3.1. Postoperative Pain Development
3.2. Postoperative PONV Prophylaxis and Analgesics Consumption
3.3. Occurrence of Side Effects
3.4. Functional Outcome after Surgery
3.5. Comparison among 24 Anonymized Hospitals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rawal, N. Current issues in postoperative pain management. Eur. J. Anaesthesiol. 2016, 33, 160–171. [Google Scholar] [CrossRef] [PubMed]
- Glare, P.; Aubrey, K.R.; Myles, P.S. Transition from acute to chronic pain after surgery. Lancet 2019, 393, 1537–1546. [Google Scholar] [CrossRef] [PubMed]
- Li, J.W.; Ma, Y.S.; Xiao, L.K. Postoperative Pain Management in Total Knee Arthroplasty. Orthop. Surg. 2019, 11, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Lo, L.W.T.; Suh, J.; Chen, J.Y.; Liow, M.H.L.; Allen, J.C.; Lo, N.N.; Yeo, S.J.; Howe, T.S.; Koh, J.S.B. Early Postoperative Pain after Total Knee Arthroplasty Is Associated with Subsequent Poorer Functional Outcomes and Lower Satisfaction. J. Arthroplast. 2021, 36, 2466–2472. [Google Scholar] [CrossRef]
- Gerbershagen, H.J.; Pogatzki-Zahn, E.; Aduckathil, S.; Peelen, L.M.; Kappen, T.H.; van Wijck, A.J.M.; Kalkman, C.J.; Meissner, W. Procedure-specific risk factor analysis for the development of severe postoperative pain. Anesthesiology 2014, 120, 1237–1245. [Google Scholar] [CrossRef]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020–2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef]
- Halawi, M.J.; Jongbloed, W.; Baron, S.; Savoy, L.; Williams, V.J.; Cote, M.P. Patient Dissatisfaction After Primary Total Joint Arthroplasty: The Patient Perspective. J. Arthroplast. 2019, 34, 1093–1096. [Google Scholar] [CrossRef]
- Heath, E.L.; Ackerman, I.N.; Cashman, K.; Lorimer, M.; Graves, S.E.; Harris, I.A. Patient-reported outcomes after hip and knee arthroplasty: Results from a large national registry. Bone Jt. Open. 2021, 2, 422–432. [Google Scholar] [CrossRef]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Tang, S.; Jin, Y.; Hou, Y.; Wang, W.; Zhang, J.; Zhu, W.; Zhang, W.; Gu, X.; Ma, Z. Predictors of chronic pain in elderly patients undergoing total knee and hip arthroplasty: A prospective observational study. J. Arthroplast. 2023. [Google Scholar] [CrossRef]
- Fletcher, D.; Stamer, U.M.; Pogatzki-Zahn, E.; Zaslansky, R.; Tanase, N.V.; Perruchoud, C.; Kranke, P.; Komann, M.; Lehman, T.; Meissner, W.; et al. Chronic postsurgical pain in Europe: An observational study. Eur. J. Anaesthesiol. 2015, 32, 725–734. [Google Scholar] [CrossRef] [PubMed]
- Gentry, W.; Stambough, J.B.; Porter, A.; Barnes, C.L., 3rd; Stronach, B.M.; Mears, S.C. Surgical Approach Does Not Affect Chronic Opioid Usage After Total Hip Arthroplasty. J. Arthroplast. 2023. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J.; Habib, A.S.; Miller, T.E.; White, W.; Apfelbaum, J.L. Incidence, patient satisfaction, and perceptions of post-surgical pain: Results from a US national survey. Curr. Med. Res. Opin. 2014, 30, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Q.; Zhou, Z. Perioperative pain management of total hip arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2019, 33, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Meissner, W.; Ullrich, K.; Zwacka, S. Benchmarking as a tool of continuous quality improvement in postoperative pain management. Eur. J. Anaesthesiol 2006, 23, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Benditz, A.; Greimel, F.; Auer, P.; Zeman, F.; Göttermann, A.; Grifka, J.; Meissner, W.; von Kunow, F. Can consistent benchmarking within a standardized pain management concept decrease postoperative pain after total hip arthroplasty? A prospective cohort study including 367 patients. J. Pain Res. 2016, 9, 1205–1213. [Google Scholar] [CrossRef]
- Meissner, W.; Mescha, S.; Rothaug, J.; Zwacka, S.; Goettermann, A.; Ulrich, K.; Schleppers, A. Quality improvement in postoperative pain management: Results from the QUIPS project. Dtsch. Arztebl. Int. 2008, 105, 865–870. [Google Scholar] [CrossRef]
- Bertin, K.C.; Röttinger, H. Anterolateral mini-incision hip replacement surgery: A modified Watson-Jones approach. Clin. Orthop. Relat. Res. 2004, 429, 248–255. [Google Scholar] [CrossRef]
- Farrar, J.T.; Young, J.P.; LaMoreaux, L., Jr.; Werth, J.L.; Poole, M.R. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001, 94, 149–158. [Google Scholar] [CrossRef]
- Noth, U.; Geiser, T.; Kranich, T.; von Rottkay, E.; Reichert, J.C.; Reyle-Hahn, M. Fast track strategies in hip arthroplasty. Orthopade 2019, 48, 330–336. [Google Scholar] [CrossRef]
- Streb, T.; Schneider, A.; Wiesmann, T.; Riecke, J.; Schubert, A.-K.; Dinges, H.-C.; Volberg, C. Rebound pain-From definition to treatment. Anaesthesiologie 2022, 71, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Stone, A.; Lirk, P.; Vlassakov, K. Rebound pain after peripheral nerve blockade-bad timing or rude awakening? Anesthesiol. Clin. 2022, 40, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Barry, G.S.; Bailey, J.G.; Sardinha, J.; Brousseau, P.; Uppal, V. Factors associated with rebound pain after peripheral nerve block for ambulatory surgery. Br. J. Anaesth. 2021, 126, 862–871. [Google Scholar] [CrossRef] [PubMed]
- Dawson, S.; Loewenstein, S.N. Severe rebound pain after peripheral nerve block for ambulatory extremity surgery is an underappreciated problem. Comment on Br J Anaesth 2021; 126: 862-71. Br. J. Anaesth. 2021, 126, e204–e205. [Google Scholar] [CrossRef]
- Sunderland, S.; Yarnold, C.H.; Head, S.J.; Osborn, J.A.; Purssell, A.; Peel, J.K.; Schwarz, S.K.W. Regional versus general anesthesia and the incidence of unplanned health care resource utilization for postoperative pain after wrist fracture surgery: Results from a retrospective quality improvement project. Reg. Anesth. Pain Med. 2016, 41, 22–27. [Google Scholar] [CrossRef]
- den Hartog, Y.M.; Hannink, G.; van Dasselaar, N.T.; Mathijssen, N.M.; Vehmeijer, S.B. Which patient-specific and surgical characteristics influence postoperative pain after THA in a fast-track setting? BMC Musculoskelet. Disord. 2017, 18, 363. [Google Scholar] [CrossRef]
- Kehlet, H. Fast-track hip and knee arthroplasty. Lancet 2013, 381, 1600–1602. [Google Scholar] [CrossRef]
- Greimel, F.; Maderbacher, G.; Zeman, F.; Grifka, J.; Meissner, W.; Benditz, A. No Clinical Difference Comparing General, Regional, and Combination Anesthesia in Hip Arthroplasty: A Multicenter Cohort-Study Regarding Perioperative Pain Management and Patient Satisfaction. J. Arthroplast. 2017, 32, 3429–3433. [Google Scholar] [CrossRef]
- Lung, B.E.; Le, R.; McLellan; Callan, K.; Donnelly, M.; Yi, J.; Birring, P.; McMaster, W.C.; Yang, S.; So, D.H. Repeat High-Dose Dexamethasone May Improve Recovery 48 Hours after Total Hip Arthroplasty. Arch. Bone Jt. Surg. 2023, 11, 188–196. [Google Scholar] [CrossRef]
- Farì, G.; de Sire, A.; Fallea, C.; Albano, M.; Grossi, G.; Bettoni, E.; Di Paolo, S.; Agostini, F.; Bernetti, A.; Puntillo, F.; et al. Efficacy of Radiofrequency as Therapy and Diagnostic Support in the Management of Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Diagnostics 2022, 12, 600. [Google Scholar] [CrossRef]

| 2015 (n = 201) | 2021 (n = 290) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Median ± IQR | Range | Median ± IQR | Range | p-Value | |||||
| Age (yrs.) | 65 ± 20 | 35–85 | 65 ± 20 | 35–85 | 0.762 | ||||
| Sex (male:female) | 95:105 | 138:151 | 0.99 | ||||||
| Duration of surgery (min) | 66.5 ± 23 | 32–152 | 64 ± 18 | 36–145 | 0.46 | ||||
| ASA Score - Frequency (%) | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | |
| 16.9 | 54.2 | 28.9 | 0 | 17.6 | 66.6 | 15.9 | 0 | 0.014 | |
| - Absolute number | 34 | 109 | 58 | 0 | 51 | 193 | 46 | 0 | 0.014 |
| Pain before surgery | |||||||||
| Chronic pain >3 months preoperatively % (number) | 92 (185/201) | 98.6 (286/290) | <0.001 | ||||||
| - Operated region (%) | 94.1 (174/185) | 94.8 (271/286) | 0.772 | ||||||
| - Operated + 1 other region % (number) | 5.9 (11/185) | 4.9 (14/286) | 0.772 | ||||||
| Preoperative opioid consumption % (number) | 0 (0/201) | 2.1 (6/290) | 0.086 | ||||||
| NRS chronic pain | 7 ± 2 | 3–10 | 7 ± 3 | 2–9 | 0.017 | ||||
| 2015 (n = 201) | 2021 (n = 290) | ||||
|---|---|---|---|---|---|
| Median ± IQR | Range | Median ± IQR | Range | p-Value | |
| NRS minimum | 0 ± 0 | 0–1 | 0 ± 0 | 0–1 | 0.069 |
| NRS maximum | 3 ± 3 | 0–9 | 5 ± 2 | 0–9 | <0.001 |
| NRS activity-related | 1 ± 2 | 0–5 | 3 ± 2 | 0–6 | <0.001 |
| Participation in pain management | 10 ± 0 | 9–10 | 10 ± 0 | 8–10 | <0.001 |
| Satisfaction with pain management | 10 ± 0 | 7–10 | 10 ± 0 | 3–10 | 0.849 |
| 2015 (n = 201) | 2021 (n = 290) | ||
|---|---|---|---|
| Relative Frequencies | Relative Frequencies | p-Value | |
| PONV prophylaxis % (number) | 53.7 (108/201) | 53.1 (153/288) | 0.927 |
| IMC non-opioid % (number) | 94 (189/201) | 97.9 (284/290) | 0.024 |
| IMC opioid % (number) | 33.8 (68/201) | 85.2 (247/290) | <0.001 |
| ward non-opioid % (number) | 100 (201/201) | 100 (288/288) | 0.99 |
| ward opioid % (number) | 34.8 (70/201) | 46.9 (135/288) | 0.009 |
| 2015 (n = 201) | 2021 (n = 290) | ||
|---|---|---|---|
| Relative Frequencies | Relative Frequencies | p-Value | |
| Nausea % (number) | 28.4 (57/201) | 26.9 (78/290) | 0.756 |
| Dizziness % (number) | 19.9 (40/201) | 30.0 (87/290) | 0.016 |
| Tiredness % (number) | 33.8 (68/201) | 22.8 (66/290) | 0.007 |
| 2015 (n = 201) | 2021 (n = 290) | ||
|---|---|---|---|
| Relative Frequencies | Relative Frequencies | p-Value | |
| Pain affected ability to move % (number) | 28.9 (58/201) | 25.5 (74/290) | 0.469 |
| Pain affected ability to cough/deep breath % (number) | 4.5 (9/201) | 4.8 (14/290) | 0.99 |
| Pain affected ability to sleep % (number) | 13.4 (27/201) | 9.3 (27/290) | 0.186 |
| Pain affected mood % (number) | 1.0 (2/201) | 1.4 (4/290) | 0.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reinhard, J.; Pulido, L.C.; Schindler, M.; Schraag, A.; Greimel, F.; Grifka, J.; Benditz, A. No Success without Effort: Follow-Up at Six Years after Implementing a Benchmarking and Feedback Concept for Postoperative Pain after Total Hip Arthroplasty. J. Clin. Med. 2023, 12, 4577. https://doi.org/10.3390/jcm12144577
Reinhard J, Pulido LC, Schindler M, Schraag A, Greimel F, Grifka J, Benditz A. No Success without Effort: Follow-Up at Six Years after Implementing a Benchmarking and Feedback Concept for Postoperative Pain after Total Hip Arthroplasty. Journal of Clinical Medicine. 2023; 12(14):4577. https://doi.org/10.3390/jcm12144577
Chicago/Turabian StyleReinhard, Jan, Loreto C. Pulido, Melanie Schindler, Amadeus Schraag, Felix Greimel, Joachim Grifka, and Achim Benditz. 2023. "No Success without Effort: Follow-Up at Six Years after Implementing a Benchmarking and Feedback Concept for Postoperative Pain after Total Hip Arthroplasty" Journal of Clinical Medicine 12, no. 14: 4577. https://doi.org/10.3390/jcm12144577
APA StyleReinhard, J., Pulido, L. C., Schindler, M., Schraag, A., Greimel, F., Grifka, J., & Benditz, A. (2023). No Success without Effort: Follow-Up at Six Years after Implementing a Benchmarking and Feedback Concept for Postoperative Pain after Total Hip Arthroplasty. Journal of Clinical Medicine, 12(14), 4577. https://doi.org/10.3390/jcm12144577