Anatomical Single-Bundle Anterior Cruciate Ligament Reconstruction Using a Calcium Phosphate-Hybridized Tendon Graft with More than an Average of 5 Years of Follow-Up: A Follow-Up Study of a Randomized Controlled Trial
Abstract
1. Introduction
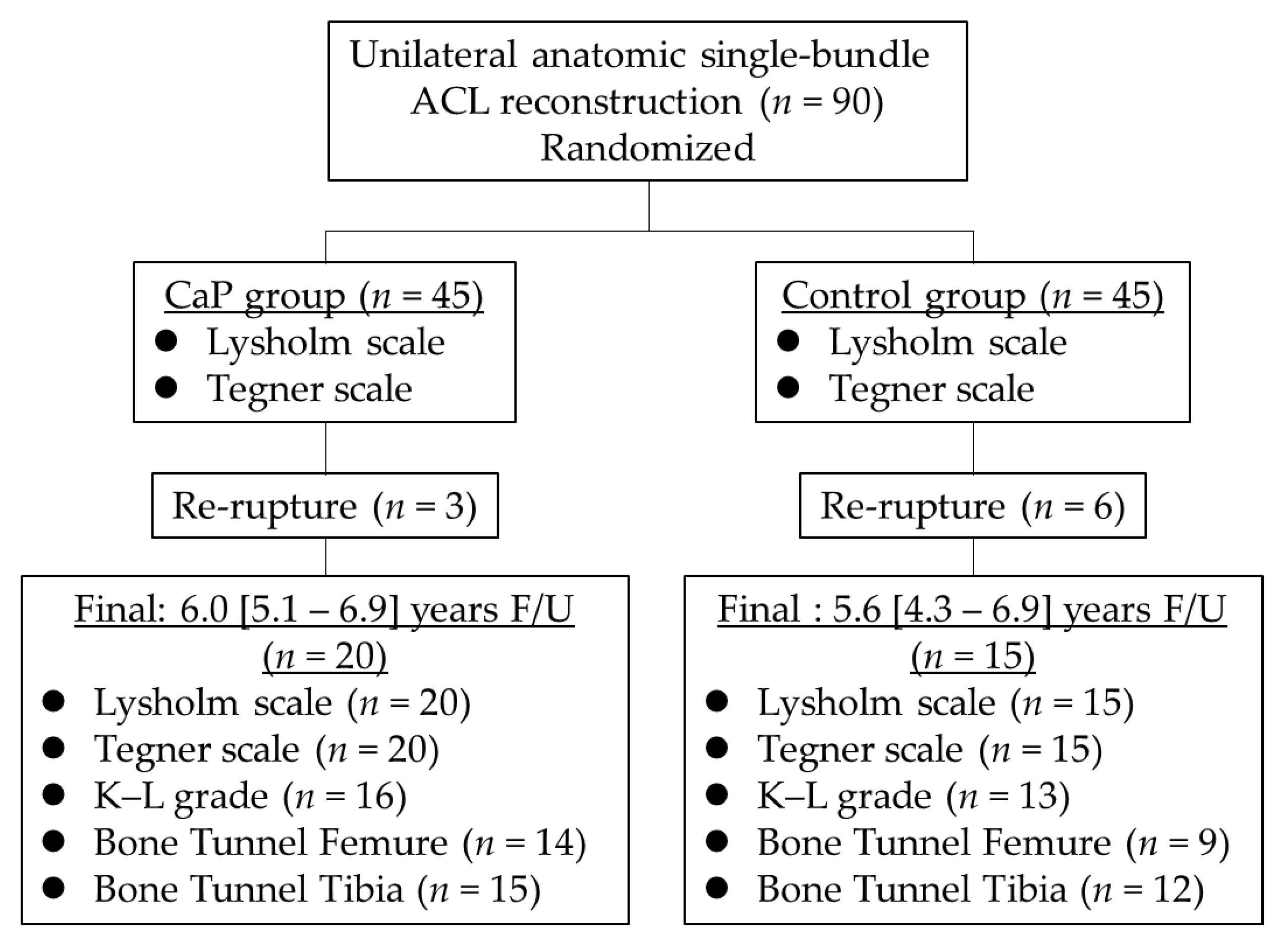
2. Materials and Methods
2.1. Clinical Evaluations
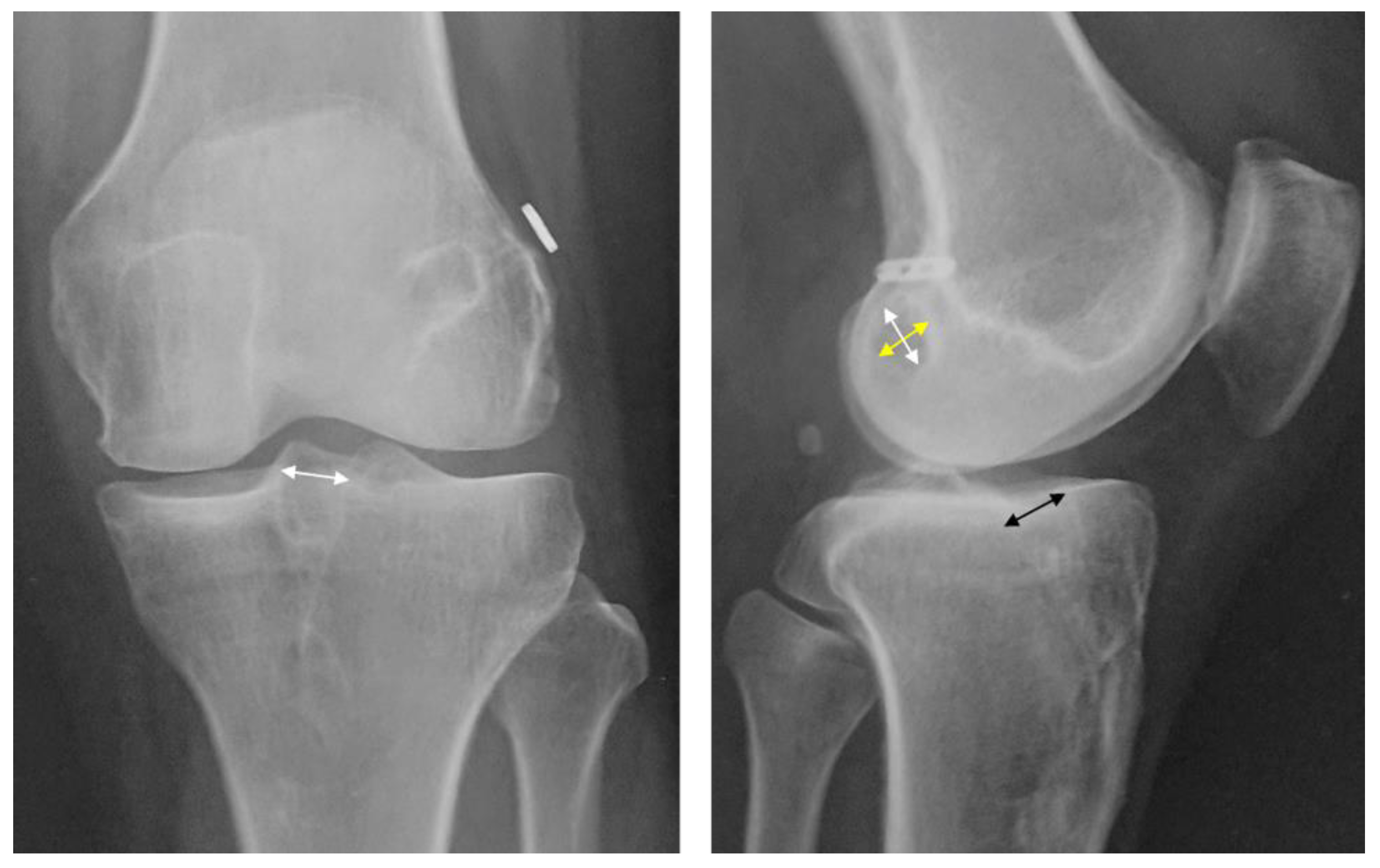
2.2. Radiograph Evaluations
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Woo, S.Y.L.; Maynard, J.; Butler, D.; Lyon, R.; Torzilli, P.; Akeson, W. Ligament, tendon, and joint capsule insertions to bone. In Injury and Repair of the Musculoskeletal Soft Tissues; Woo, S.L.Y., Buckwalter, J.A., Eds.; American Academy of Orthopaedic Surgeons: Park Ridge, IL, USA, 1988; pp. 133–166. [Google Scholar]
- Everhart, J.S.; Yalcin, S.; Spindler, K.P. Twenty-year outcomes after anterior cruciate ligament reconstruction: A systematic review of prospectively collected data. Am. J. Sports Med. 2022, 50, 2842–2852. [Google Scholar] [CrossRef] [PubMed]
- Haybäck, G.; Raas, C.; Rosenberger, R. Failure rates of common grafts used in ACL reconstructions: A systematic review of studies published in the last decade. Arch. Orthop. Trauma Surg. 2022, 142, 3293–3299. [Google Scholar] [CrossRef] [PubMed]
- Yue, L.; DeFroda, S.F.; Sullivan, K.; Garcia, D.; Owens, B.D. Mechanisms of bone tunnel enlargement following anterior cruciate ligament reconstruction. JBJS Rev. 2020, 8, e0120. [Google Scholar] [CrossRef] [PubMed]
- Stolarz, M.; Ficek, K.; Binkowski, M.; Wróbel, Z. Bone tunnel enlargement following hamstring anterior cruciate ligament reconstruction: A comprehensive review. Phys. Sportsmed. 2017, 45, 31–40. [Google Scholar] [CrossRef]
- Grana, W.A.; Egle, D.M.; Mahnken, R.; Goodhart, C.W. An analysis of autograft fixation after anterior cruciate ligament reconstruction in a rabbit model. Am. J. Sports Med. 1994, 22, 344–351. [Google Scholar] [CrossRef]
- Nebelung, W.; Becker, R.; Urbach, D.; Röpke, M.; Roessner, A. Histological findings of tendon-bone healing following anterior cruciate ligament reconstruction with hamstring grafts. Arch. Orthop. Trauma Surg. 2003, 123, 158–163. [Google Scholar] [CrossRef]
- Mutsuzaki, H.; Sakane, M.; Fujie, H.; Hattori, S.; Kobayashi, H.; Ochiai, N. Effect of calcium phosphate–hybridized tendon graft on biomechanical behavior in anterior cruciate ligament reconstruction in a goat model: Novel technique for improving tendon-bone healing. Am. J. Sports Med. 2011, 39, 1059–1066. [Google Scholar] [CrossRef]
- Belk, J.W.; Kraeutler, M.J.; Carver, T.J.; McCarty, E.C. Knee osteoarthritis after anterior cruciate ligament reconstruction with bone-patellar tendon-bone versus hamstring tendon autograft: A systematic review of randomized controlled trials. Arthroscopy 2018, 34, 1358–1365. [Google Scholar] [CrossRef]
- Taguchi, T.; Kishida, A.; Akashi, M. Hydroxyapatite formation on/in hydrogels using a novel alternate soaking process. Chem. Lett. 1998, 8, 711–712. [Google Scholar] [CrossRef]
- Mutsuzaki, H.; Sakane, M.; Nakajima, H.; Ito, A.; Hattori, S.; Miyanaga, Y.; Ochiai, N.; Tanaka, J. Calcium-phosphate-hybridized tendon directly promotes regeneration of tendon-bone insertion. J. Biomed. Mater. Res. A 2004, 70, 319–327. [Google Scholar] [CrossRef]
- Mutsuzaki, H.; Sakane, M.; Ito, A.; Nakajima, H.; Hattori, S.; Miyanaga, Y.; Tanaka, J.; Ochiai, N. The interaction between osteoclast-like cells and osteoblasts mediated by nanophase calcium phosphate-hybridized tendons. Biomaterials 2005, 26, 1027–1034. [Google Scholar] [CrossRef]
- Mutsuzaki, H.; Fujie, H.; Nakajima, H.; Fukagawa, M.; Nomura, S.; Sakane, M. Effect of calcium phosphate-hybridized tendon graft in anatomicalal single-bundle ACL reconstruction in goats. Orthop. J. Sports Med. 2016, 4, 2325967116662653. [Google Scholar] [CrossRef]
- Mutsuzaki, H.; Kinugasa, T.; Ikeda, K.; Sakane, M. Calcium phosphate-hybridized tendon grafts reduce femoral bone tunnel enlargement in anatomical single-bundle ACL reconstruction. Knee Surg. Sport. Traumatol. Arthrosc. 2018, 26, 500–507. [Google Scholar] [CrossRef]
- Mutsuzaki, H.; Kinugasa, T.; Ikeda, K.; Sakane, M. Anatomical single-bundle anterior cruciate ligament reconstruction using a calcium phosphate-hybridized tendon graft: A randomized controlled trial with 2 years of follow-up. J. Orthop. Surg. Res. 2018, 13, 327. [Google Scholar] [CrossRef]
- Mutsuzaki, H.; Kinugasa, T.; Ikeda, K.; Sakane, M. Morphological changes in the femoral and tibial bone tunnels after anatomical single-bundle anterior cruciate ligament reconstruction using a calcium phosphate-hybridized tendon graft in 2 years of follow-up. Orthop. Traumatol. Surg. Res. 2019, 105, 653–660. [Google Scholar] [CrossRef]
- Tegner, Y.; Lysholm, J. Rating systems in the evaluation of knee ligament injuries. Clin. Orthop. Relat. Res. 1985, 198, 43–49. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef]
- Devitt, B.M.; Maes, M.; Feller, J.A.; Webster, K.E. No long-term tunnel enlargement following anterior cruciate ligament reconstruction using autograft hamstring tendon with dual suspensory fixation. Knee Surg Sports Traumatol. Arthrosc. 2020, 28, 2157–2162. [Google Scholar] [CrossRef]
- Zhao, D.; Pan, J.K.; Lin, F.Z.; Luo, M.H.; Liang, G.H.; Zeng, L.F.; Huang, H.T.; Han, Y.H.; Xu, N.J.; Yang, W.Y.; et al. Risk Factors for revision or rerupture after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am. J. Sports Med. 2022, 3, 3635465221119787. [Google Scholar] [CrossRef]
- Ekeland, A.; Engebretsen, L.; Fenstad, A.M.; Heir, S. Similar risk of ACL graft revision for alpine skiers, football and handball players: The graft revision rate is influenced by age and graft choice. Br. J. Sports Med. 2020, 54, 33–37. [Google Scholar] [CrossRef]
- Lee, R.; Kean, W.F. Obesity and knee osteoarthritis. Inflammopharmacology 2012, 20, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Examination Committee of Criteria for ‘Obesity Disease’ in Japan. New criteria for ‘obesity disease’ in Japan. Circ. J. 2002, 66, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Rodeo, S.A.; Kawamura, S.; Kim, H.J.; Dynybil, C.; Ying, L. Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: An effect of graft-tunnel motion? Am. J. Sports Med. 2006, 34, 1790–1800. [Google Scholar] [CrossRef] [PubMed]
- Rodeo, S.A.; Kawamura, S.; Ma, C.B.; Deng, X.H.; Sussman, P.S.; Hays, P.; Ying, L. The effect of osteoclast activity on tendon-to-bone healing: An experimental study in rabbits. J. Bone Jt. Surg. 2007, 89, 2250–2259. [Google Scholar]
- Berg, E.E.; Pollard, M.E.; Kang, Q. Interarticular bone tunnel healing. Arthroscopy 2001, 17, 189–195. [Google Scholar] [CrossRef]
- Feller, J.A.; Webster, K.E. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am. J. Sports Med. 2003, 31, 564–573. [Google Scholar] [CrossRef]
- Paessler, H.H.; Mastrokalos, D.S. Anterior cruciate ligament reconstruction using semitendinosus and gracilis tendons, bone patellar tendon, or quadriceps tendon-graft with press-fit fixation without hardware. A new and innovative procedure. Orthop. Clin. N. Am. 2003, 34, 49–64. [Google Scholar] [CrossRef]
- Maak, T.G.; Voos, J.E.; Wickiewicz, T.L.; Warren, R.F. Tunnel widening in revision anterior cruciate ligament reconstruction. J. Am. Acad. Orthop. Surg. 2010, 18, 695–706. [Google Scholar] [CrossRef]
- Bystrova, A.V.; Dekhtyar, Y.D.; Popov, A.I.; Coutinho, J.; Bystrov, V.S. Modified hydroxyapatite structure and properties: Modeling and synchrotron data analysis of modified hydroxyapatite structure. Ferroelectrics 2015, 475, 135–147. [Google Scholar] [CrossRef]
- Hübner, W.; Blume, A.; Pushnjakova, R.; Dekhtyar, Y.; Hein, H.J. The influence of X-ray radiation on the mineral/organic matrix interaction of bone tissue: An FT-IR microscopic investigation. Int. J. Artif. Organs 2005, 28, 66–73. [Google Scholar] [CrossRef]
- Sinusaite, L.; Antuzevics, A.; Popov, A.I.; Rogulis, U.; Misevicius, M.; Katelnikovas, A.; Kareiva, A.; Zarkov, A. Synthesis and luminescent properties of Mn-doped alpha-tricalcium phosphate. Ceram. Int. 2021, 47, 5335–5340. [Google Scholar] [CrossRef]
- Webster, K.E.; Chiu, J.J.; Feller, J.A. Impact of measurement error in the analysis of bone tunnel enlargement after anterior cruciate ligament reconstruction. Am. J. Sports Med. 2005, 33, 1680–1687. [Google Scholar] [CrossRef]
| CaP Group (n = 20) | Control Group (n = 15) | p Value | |
|---|---|---|---|
| Age (years) | 32.0 (24.4–37.5) | 25.9 (19.0–32.9) | 0.165 |
| Sex (male/female) | 8/12 | 10/5 | 0.189 |
| Height (cm) | 165.1 (161.8–168.4) | 169.5 (165.4–173.6) | 0.104 |
| Weight (kg) | 62.1 (57.0–67.2) | 70.4 (64.8–76.0) | 0.041 * |
| BMI (kg/m2) | 22.7 (21.2–24.2) | 24.5 (22.6–26.5) | 0.142 |
| Operative findings of meniscal injury (MM/LM) | 7/7 | 4/5 | 0.269 |
| Duration from injury to operation (months) | 15.1 (2.6–27.6) | 2.6 (1.5–3.8) | 0.082 |
| Follow-up period (years) | 6.0 (5.1–6.9) | 5.6 (4.3–6.9) | 0.764 |
| Preoperative (Preinjury) | Final | Fixed Effect | Model Fit Criteria | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CaP Group | Conventional Method | CaP Group | Conventional Method | Time | Group | Time × Group | Sex | Age | BMI | AICc | BIC | MCID | |
| Lysholm scale | 54.5 (50.5–58.5) | 49.2 (44.5–53.9) | 95.5 (91.5–99.5) | 97.0 (92.3–101.7) | <0.001 | 0.095 | 0.111 | 0.873 | 0.548 | 0.206 | 487.287 | 491.374 | 9.23 |
| Tegner scale | 5.9 (5.4–6.5) | 6.9 (6.2–7.6) | 5.5 (5.0–6.1) | 5.9 (5.2–6.6) | 0.012 | 0.049 | 0.239 | 0.459 | <0.001 | 0.811 | 239.875 | 243.961 | 0.70 |
| K–L grade | 1.1 (0.8–1.41) | 0.4 (0.1–0.8) | 1.8 (1.5–2.1) | 1.2 (0.8–1.5) | <0.001 | 0.015 | 0.686 | 0.571 | 0.002 | 0.150 | 112.622 | 116.236 | 0.33 |
| Group | Main Effect | Model Fit Criteria | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CaP Group | Control Method | Group | Sex | Age | BMI | AIC | BIC | MCID | |
| Femur | |||||||||
| APD (%) | 7.9 (−1.1–16.8) | 29.2 (17.9–40.5) | 0.004 | 0.708 | 0.927 | 0.284 | 207.398 | 214.211 | 16.05 |
| PDD (%) | 7.9 (−1.9–17.8) | 22.8 (10.9–34.7) | 0.062 | 0.936 | 0.668 | 0.819 | 201.346 | 207.892 | 15.00 |
| Tibia | |||||||||
| APD (%) | 8.9 (−3.0–20.8) | 22.9 (10.0–35.8) | 0.128 | 0.219 | 0.764 | 0.781 | 246.473 | 254.022 | 18.88 |
| MLD (%) | 21.0 (13.5–28.6) | 13.6 (5.1–22.2) | 0.217 | 0.142 | 0.455 | 0.253 | 233.175 | 240.950 | 22.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mutsuzaki, H.; Kinugasa, T. Anatomical Single-Bundle Anterior Cruciate Ligament Reconstruction Using a Calcium Phosphate-Hybridized Tendon Graft with More than an Average of 5 Years of Follow-Up: A Follow-Up Study of a Randomized Controlled Trial. J. Clin. Med. 2023, 12, 4437. https://doi.org/10.3390/jcm12134437
Mutsuzaki H, Kinugasa T. Anatomical Single-Bundle Anterior Cruciate Ligament Reconstruction Using a Calcium Phosphate-Hybridized Tendon Graft with More than an Average of 5 Years of Follow-Up: A Follow-Up Study of a Randomized Controlled Trial. Journal of Clinical Medicine. 2023; 12(13):4437. https://doi.org/10.3390/jcm12134437
Chicago/Turabian StyleMutsuzaki, Hirotaka, and Tomonori Kinugasa. 2023. "Anatomical Single-Bundle Anterior Cruciate Ligament Reconstruction Using a Calcium Phosphate-Hybridized Tendon Graft with More than an Average of 5 Years of Follow-Up: A Follow-Up Study of a Randomized Controlled Trial" Journal of Clinical Medicine 12, no. 13: 4437. https://doi.org/10.3390/jcm12134437
APA StyleMutsuzaki, H., & Kinugasa, T. (2023). Anatomical Single-Bundle Anterior Cruciate Ligament Reconstruction Using a Calcium Phosphate-Hybridized Tendon Graft with More than an Average of 5 Years of Follow-Up: A Follow-Up Study of a Randomized Controlled Trial. Journal of Clinical Medicine, 12(13), 4437. https://doi.org/10.3390/jcm12134437





