Comparative Study for Characteristics of Locomotive Syndrome in Patients with Lumbar Stenosis and Adult Spinal Deformity
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Radiographic Measurements
2.3. LS Screening Instrument
2.4. Physical Performance Tests
- (1)
- Two-step test: a measurement of the length of two strides of the participants, providing a general assessment of their walking ability including muscular strength, balance, and flexibility of the lower extremities. It is scored by normalizing the maximal length of two steps by the height. Two-Step Test scores < 0.9, <1.1, <1.3, and ≥1.3 points correspond to LS-3, LS-2, LS-1, and non-LS [7].
- (2)
- The stand-up test: a simple method of assessing the muscular strength of the lower extremities by having participants stand-up on one or both legs once from seats of different heights (40, 30, 20, and 10 cm). The test is scored as 0–8, with the scores defined as follows: 0 (unable to stand); 1–4 (able to stand—using both legs—from 40, 30, 20, and 10 cm, respectively); 5–8 (able to stand—using one leg—from 40, 30, 20, and 10 cm, respectively). Stand-Up Test scores of 0–1, 2, 3–4, and 5–8 points are equivalent to LS-3, LS-2, LS-1, and non-LS [7].
2.5. Statistical Analyses
3. Patient Population
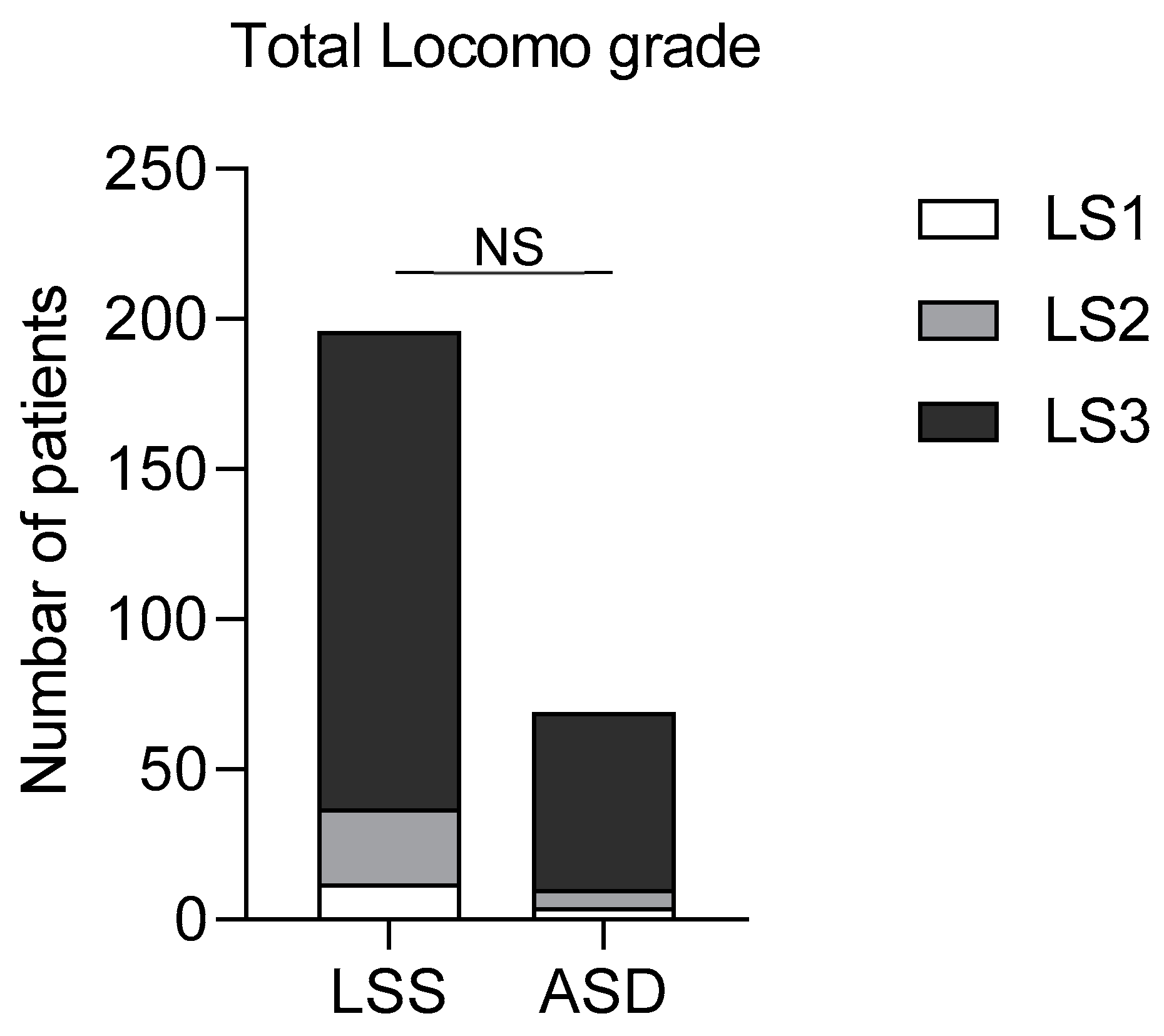
4. Frequency and Severity of Locomotive Dysfunction in Patients with LSS or ASD
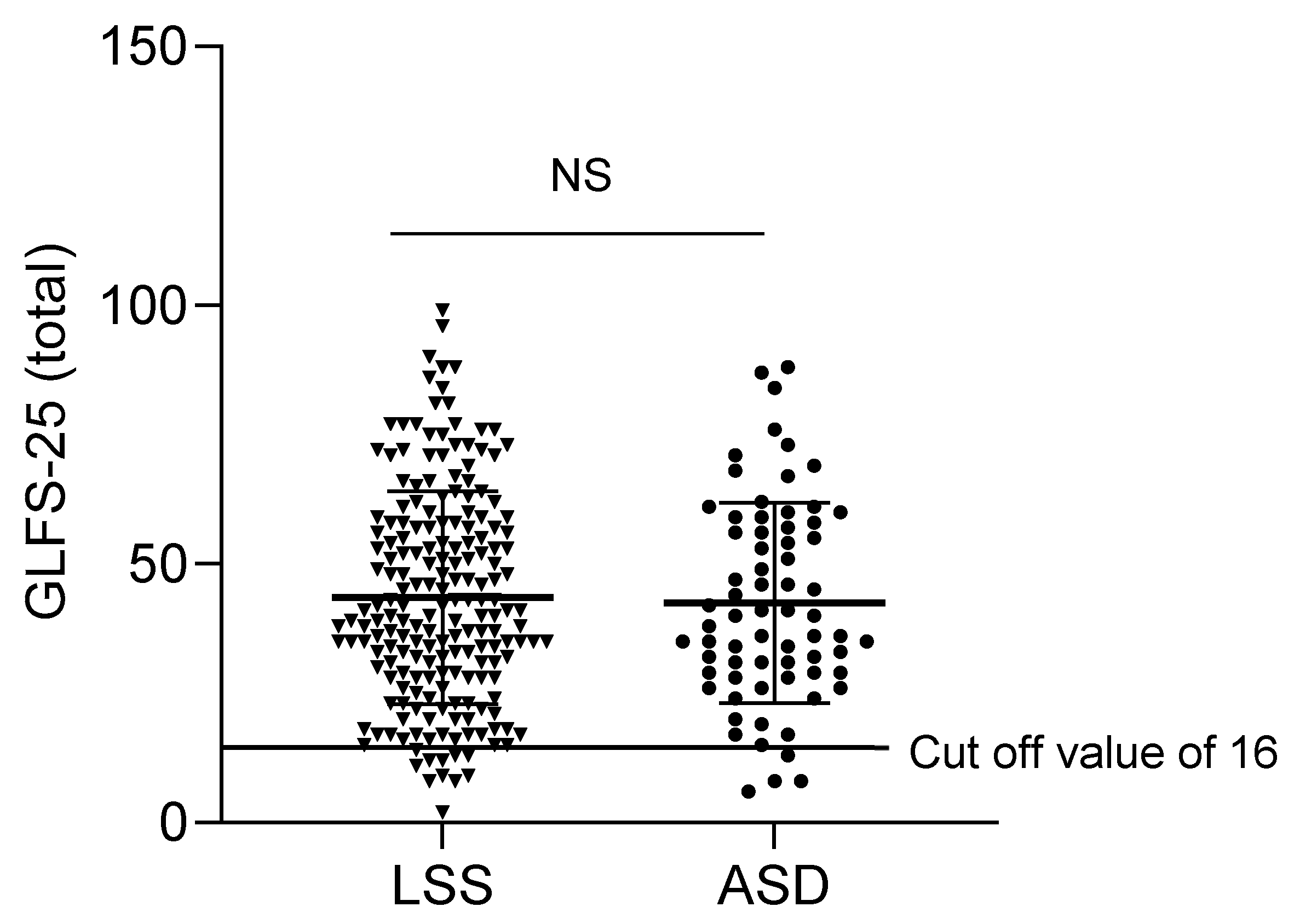
5. GLFS-25 Scores in Patients with LSS or ASD
6. Correlation between GLFS-Scores and Spinopelvic Parameters in ASD
7. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sandvik, L.; Erikssen, J.; Thaulow, E.; Erikssen, G.; Mundal, R.; Rodahl, K. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N. Engl. J. Med. 1993, 328, 533–537. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K. A “super-aged” society and the “locomotive syndrome”. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2008, 13, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Seichi, A.; Hoshino, Y.; Doi, T.; Akai, M.; Tobimatsu, Y.; Iwaya, T. Development of a screening tool for risk of locomotive syndrome in the elderly: The 25-question Geriatric Locomotive Function Scale. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2012, 17, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Shigematsu, H.; Tanaka, M.; Kawasaki, S.; Iwata, E.; Masuda, K.; Morimoto, Y.; Yamamoto, Y.; Tanaka, Y. Loco-check presents a useful tool to determine health-related quality of life in elderly people with lumbar spinal stenosis. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2019, 24, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Morozumi, M.; Ando, K.; Kobayashi, K.; Seki, T.; Ishizuka, S.; Machino, M.; Tanaka, S.; Ito, S.; Kanbara, S.; Inoue, T.; et al. Relationship between lumbopelvic discordance and locomotive syndrome in a middle-aged community-living population: The Yakumo study. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2019, 25, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, N.; Muraki, S.; Iidaka, T.; Oka, H.; Horii, C.; Kawaguchi, H.; Akune, T.; Nakamura, K.; Tanaka, S. Prevalence and co-existence of locomotive syndrome, sarcopenia, and frailty: The third survey of Research on Osteoarthritis/Osteoporosis Against Disability (ROAD) study. J. Bone Miner. Metab. 2019, 37, 1058–1066. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Morimoto, T.; Otani, K.; Mawatari, M. Locomotive Syndrome and Lumbar Spine Disease: A Systematic Review. J. Clin. Med. 2022, 11, 1304. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.R.; Park, J.; Ham, D.W.; Kwon, B.T.; Go, S.J.; Kim, H.J. functional mobility tests for evaluation of functionalities in patients with adult spinal deformity. BMC Musculoskelet. Disord. 2022, 23, 391. [Google Scholar] [CrossRef] [PubMed]
- Won, Y.I.; Kim, C.H.; Park, H.P.; Chung, S.G.; Yuh, W.T.; Kwon, S.W.; Yang, S.H.; Lee, C.H.; Choi, Y.; Park, S.B.; et al. A cost-utility analysis between decompression only and fusion surgery for elderly patients with lumbar spinal stenosis and sagittal imbalance. Sci. Rep. 2022, 12, 20408. [Google Scholar] [CrossRef] [PubMed]
- Ham, C.H.; Park, Y.K.; Kim, J.H.; Kwon, W.K.; Kim, D.W.; Moon, H.J. Characteristics of Sagittal Spinopelvic Alignment Changes After Symptom Relief After Simple Lumbar Decompression. Neurosurgery 2022, 91, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Comer, C.; Ammendolia, C.; Battié, M.C.; Bussières, A.; Fairbank, J.; Haig, A.; Melloh, M.; Redmond, A.; Schneider, M.J.; Standaert, C.J.; et al. Consensus on a standardised treatment pathway algorithm for lumbar spinal stenosis: An international Delphi study. BMC Musculoskelet. Disord. 2022, 23, 550. [Google Scholar] [CrossRef] [PubMed]
- Saimon, Y.; Goh, A.C.; Momose, K.; Ryuzaki, D.; Akahane, H.; Oba, A.; Mukaiyama, K. Correlation between radiographic sagittal alignment, range of motion, muscle strength, and quality of life in adults with spinal deformities. J. Phys. Ther. Sci. 2020, 32, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Endo, T.; Ohba, T.; Oba, H.; Oda, K.; Tanaka, N.; Haro, H. Prevalence and Key Radiographic Spinal Malalignment Parameters Associated with the Risk of Pulmonary Function Impairment in Patients Treated Surgically to Correct Adult Spinal Deformity. Spine Surg. Relat. Res. 2020, 4, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Ohba, T.; Ebata, S.; Oba, H.; Oda, K.; Tanaka, N.; Koyama, K.; Haro, H. Prevalence and key radiographic spinal malalignment parameters that influence the risk for gastroesophageal reflux disease in patients treated surgically for adult spinal deformity. BMC Gastroenterol. 2018, 18, 8. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, Y.; Miyakoshi, N.; Kobayashi, T.; Abe, T.; Kijima, H.; Abe, E.; Shimada, Y. Activities of daily living and patient satisfaction after long fusion for adult spinal deformity: A retrospective study. Eur. Spine J. 2019, 28, 1670–1677. [Google Scholar] [CrossRef] [PubMed]
- Muramoto, A.; Imagama, S.; Ito, Z.; Hirano, K.; Ishiguro, N.; Hasegawa, Y. Spinal sagittal balance substantially influences locomotive syndrome and physical performance in community-living middle-aged and elderly women. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2016, 21, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Ohba, T.; Oba, H.; Koyama, K.; Oda, K.; Tanaka, N.; Fujita, K.; Haro, H. Locomotive syndrome: Prevalence, surgical outcomes, and physical performance of patients treated to correct adult spinal deformity. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2020, 26, 678–683. [Google Scholar] [CrossRef] [PubMed]
- Machino, M.; Ando, K.; Kobayashi, K.; Nakashima, H.; Kanbara, S.; Ito, S.; Inoue, T.; Yamaguchi, H.; Koshimizu, H.; Seki, T.; et al. Influence of Global Spine Sagittal Balance and Spinal Degenerative Changes on Locomotive Syndrome Risk in a Middle-Age and Elderly Community-Living Population. BioMed Res. Int. 2020, 2020, 3274864. [Google Scholar] [CrossRef] [PubMed]
- Yurube, T.; Ito, M.; Takeoka, T.; Watanabe, N.; Inaoka, H.; Kakutani, K.; Kuroda, R.; Nishida, K. Possible Improvement of the Sagittal Spinopelvic Alignment and Balance through “Locomotion Training” Exercises in Patients with “Locomotive Syndrome”: A Literature Review. Adv. Orthop. 2019, 2019, 6496901. [Google Scholar] [CrossRef] [PubMed]
| Variable | LSS (N = 196) | ASD (N = 69) | p |
|---|---|---|---|
| Age (y) | 74.6 ± 9.4 | 72.8 ± 7.3 | 0.13 |
| Female/male gender (n) | 172/24 | 62/7 | 0.83 |
| BMI (kg/m2) | 24.2 ± 2.1 | 23.8 ± 3.1 | 0.42 |
| Test | |||
| 2-step test (points) | 0.95 ± 0.4 | 1.04 ± 0.3 | 0.11 |
| Stand-up test (points) | 2.69 ± 1.5 | 2.86 ± 1.5 | 0.43 |
| Domain | Item | LSS | ASD | p * |
|---|---|---|---|---|
| Pain | 1 | 0.96 ± 1.2 | 1.06 ± 1.1 | 0.51 |
| 2 | 2.4 ± 1.0 | 2.4 ± 1.1 | 0.76 | |
| 3 | 2.3 ± 1.2 | 1.4 ± 1.3 | <0.05 | |
| 4 | 2.2 ± 1.0 | 2.3 ± 0.9 | 0.63 | |
| Mobility | 5 | 1.4 ± 1.1 | 1.4 ± 1.0 | 0.80 |
| 6 | 1.2 ± 1.2 | 1.3 ± 1.2 | 0.73 | |
| 7 | 1.2 ± 1.2 | 1.4 ± 0.97 | 0.13 | |
| Self-care | 8 | 0.57 ± 0.86 | 0.84 ± 0.92 | <0.05 |
| 9 | 1.3 ± 1.1 | 1.2 ± 1.1 | 0.43 | |
| 10 | 0.93 ± 1.1 | 0.79 ± 0.96 | 0.37 | |
| 11 | 0.8 ± 0.96 | 1.2 ± 1.1 | <0.05 | |
| Mobility | 12 | 2.1 ± 1.2 | 2.0 ± 1.2 | 0.69 |
| 13 | 2.5 ± 1.2 | 2.4 ± 1.1 | 0.76 | |
| Self-care | 14 | 0.81 ± 1.0 | 1.2 ± 1.0 | <0.05 |
| Mobility | 15 | 2.7 ± 1.2 | 2.8 ± 1.2 | 0.63 |
| Interpersonal interactions | 16 | 1.6 ± 1.3 | 1.6 ± 1.2 | 0.76 |
| Mobility | 17 | 1.9 ± 1.4 | 2.0 ± 1.4 | 0.49 |
| 18 | 1.7 ± 1.4 | 2.1 ± 1.3 | 0.06 | |
| Domestic life | 19 | 1.5 ± 1.2 | 1.6 ± 1.9 | 0.35 |
| 20 | 2.1 ± 1.3 | 2.6 ± 1.1 | <0.05 | |
| Community | 21 | 2.9 ± 1.1 | 3.0 ± 1.1 | 0.69 |
| Interpersonal interactions | 22 | 1.6 ± 1.4 | 1.5 ± 1.3 | 0.79 |
| Community | 23 | 2.2 ± 1.5 | 2.2 ± 1.4 | 0.91 |
| Anxiety | 24 | 1.3 ± 1.3 | 1.3 ± 1.1 | 0.69 |
| 25 | 2.0 ± 1.3 | 2.0 ± 1.2 | 0.89 |
| Variable | Preoperative | r-Value (Q20) | p-Value |
|---|---|---|---|
| PT (°) | 37.4 ± 10.6 | 0.69 | |
| SS (°) | 15.1 ± 13.4 | 0.33 | |
| LL (°) | 9.1 ± 21.7 | 0.60 | |
| PI–LL (°) | 42.1 ± 21.4 | 0.52 * | <0.05 |
| SVA (mm) | 124.8 ± 69.9 | 0.53 | |
| GT (°) | 53.2 ± 17.5 | 0.85 | |
| TPA (°) | 41.7 ± 14.9 | 0.90 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohba, T.; Goto, G.; Oda, K.; Tanaka, N.; Yokomichi, H.; Haro, H. Comparative Study for Characteristics of Locomotive Syndrome in Patients with Lumbar Stenosis and Adult Spinal Deformity. J. Clin. Med. 2023, 12, 4345. https://doi.org/10.3390/jcm12134345
Ohba T, Goto G, Oda K, Tanaka N, Yokomichi H, Haro H. Comparative Study for Characteristics of Locomotive Syndrome in Patients with Lumbar Stenosis and Adult Spinal Deformity. Journal of Clinical Medicine. 2023; 12(13):4345. https://doi.org/10.3390/jcm12134345
Chicago/Turabian StyleOhba, Tetsuro, Go Goto, Kotaro Oda, Nobuki Tanaka, Hiroshi Yokomichi, and Hirotaka Haro. 2023. "Comparative Study for Characteristics of Locomotive Syndrome in Patients with Lumbar Stenosis and Adult Spinal Deformity" Journal of Clinical Medicine 12, no. 13: 4345. https://doi.org/10.3390/jcm12134345
APA StyleOhba, T., Goto, G., Oda, K., Tanaka, N., Yokomichi, H., & Haro, H. (2023). Comparative Study for Characteristics of Locomotive Syndrome in Patients with Lumbar Stenosis and Adult Spinal Deformity. Journal of Clinical Medicine, 12(13), 4345. https://doi.org/10.3390/jcm12134345






