Mental Health of Children and Adolescents before and during the COVID-19 Pandemic: How Did the Lockdown Modify Psychiatric Emergencies in Tuscany, Italy?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
- Date of birth (day, month, year).
- Sex (male, female).
- Emergency room admission date (day, month, year).
- Psychiatric symptoms at admission (affective, anxiety, eating disorder, psychotic, psychomotor agitations, self-harm, suicide attempt, suicidal ideation, and somatic symptoms).
- New admissions versus relapse.
- None or previous psychiatric diagnosis according to the Diagnostic and Statistical Manual of Mental Disorder (DSM-5-TR) criteria.
- Outcome after psychiatry specialist evaluation (home discharge versus hospitalization) was used as the measure of clinical severity.
2.3. Lockdown Severity
- LS-1: no restrictions on social contacts, work activities, or travel, routine health care guaranteed, schools fully open.
- LS-2: restaurants open only during daytime, recreational activities not allowed, travel within the region is unrestricted, travel between regions not allowed, routine health care guaranteed, schools open only for students up to 14 years.
- LS-3: restaurants are closed, recreational activities not allowed, movement allowed only within the city of residence, social contacts limited to two people per day, routine health care guaranteed, secondary school students attend classes through distance learning, schools open only for students up to 11 years.
- LS-4: restaurants and non-essential commercial activities are closed, leisure activities not allowed, travel not allowed, 24 h curfew, home exit allowed only for essential activities, routine health care guaranteed, most schools are closed or use distance learning.
- LS-5: same as the previous level, plus all routine health is suspended because medical services have been limited to essential needs and urgent care, all schools are closed or use only distance learning.
2.4. Data Analysis
3. Results
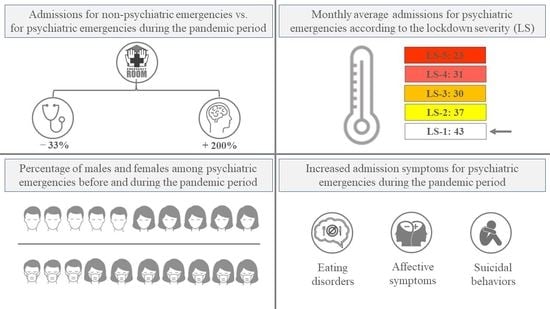
3.1. Total and Psychiatric Clinical Presentations Admissions
3.2. Demographic Variables of Admissions for Psychiatric Clinical Presentations
3.3. Monthly Average Admissions of Psychiatric Clinical Presentations
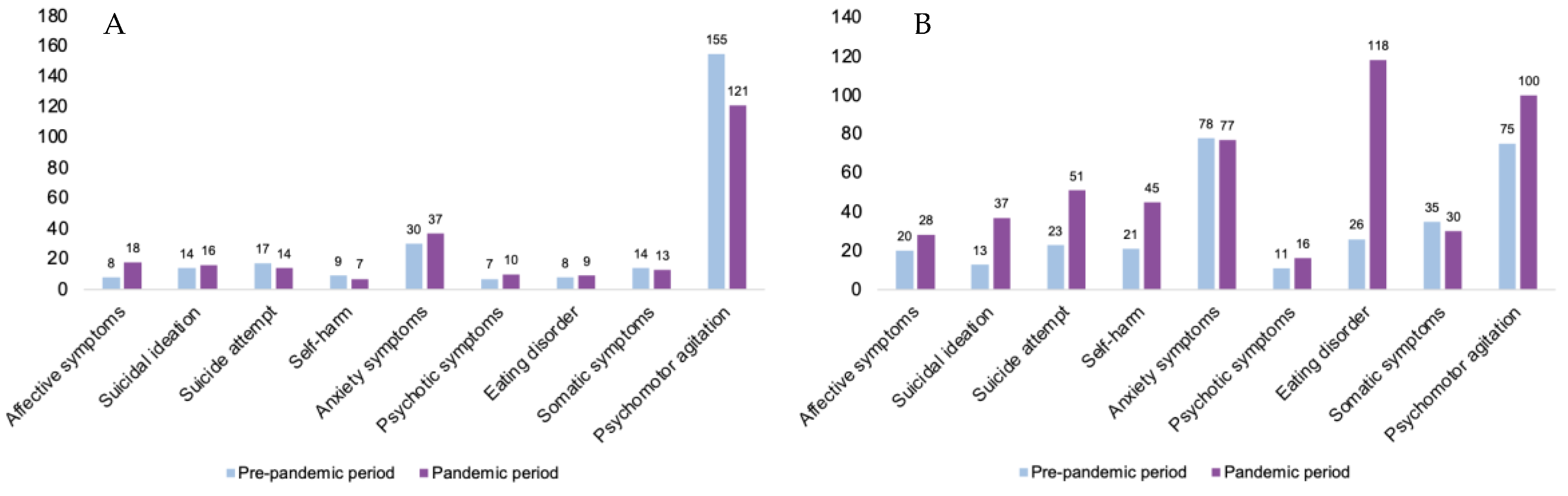
3.4. Admission Symptoms for Psychiatric Clinical Presentations in All Patients and Related to the Biological Sex
3.5. Symptoms and Diagnosis of Psychiatric Clinical Presentations Admissions
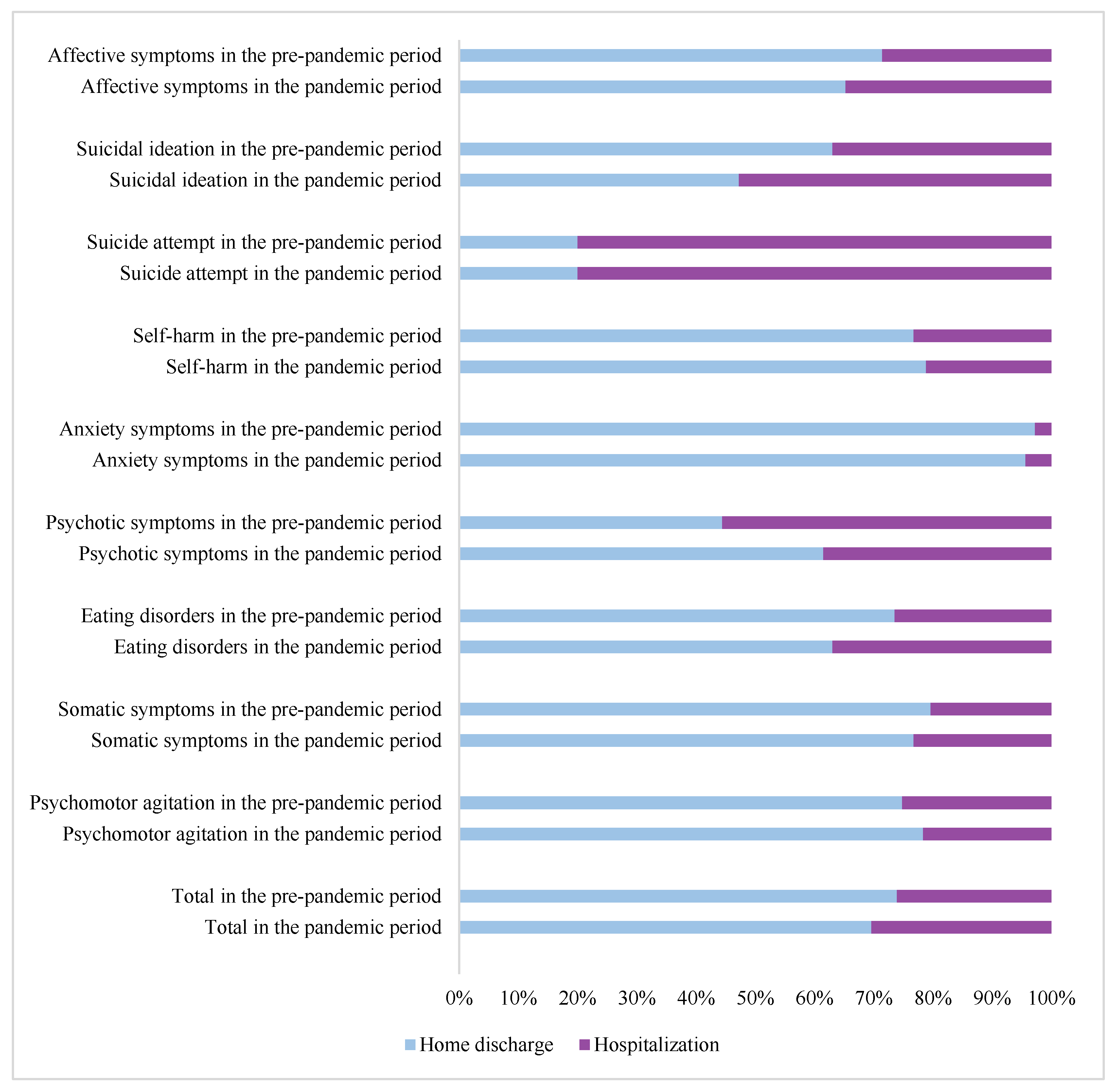
3.6. Admissions Outcome of Psychiatric Clinical Presentations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Comprehensive Mental Health Action Plan 2013–2030; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Dolan, M.A.; Fein, J.A. Committee on Pediatric Emergency Medicine. Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics 2011, 127, e1356–e1366. [Google Scholar] [CrossRef] [Green Version]
- Mahajan, P.; Alpern, E.R.; Grupp-Phelan, J.; Chamberlain, J.; Dong, L.; Holubkov, R.; Jacobs, E.; Stanley, R.; Tunik, M.; Sonnett, M.; et al. Epidemiology of Psychiatric-related Visits to Emergency Departments in a Multicenter Collaborative Research Pediatric Network. Pediatr. Emerg. Care 2009, 25, 715–720. [Google Scholar] [CrossRef] [Green Version]
- Tuite, A.R.; Ng, V.; Rees, E.; Fisman, D. Estimation of COVID-19 outbreak size in Italy. Lancet Infect. Dis. 2020, 20, 537. [Google Scholar] [CrossRef] [Green Version]
- Davico, C.; Ghiggia, A.; Marcotulli, D.; Ricci, F.; Amianto, F.; Vitiello, B. Psychological Impact of the COVID-19 Pandemic on Adults and Their Children in Italy. Front. Psychiatry 2021, 12, 572997. [Google Scholar] [CrossRef] [PubMed]
- Ford, T.; John, A.; Gunnell, D. Mental health of children and young people during pandemic. BMJ 2021, 372, n614. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 2012, 53, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.; Yim, H.W.; Song, Y.J.; Ki, M.; Min, J.A.; Cho, J.; Chae, J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health 2016, 38, e2016048. [Google Scholar] [CrossRef] [Green Version]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Newlove-Delgado, T.; McManus, S.; Sadler, K.; Thandi, S.; Vizard, T.; Cartwright, C.; Ford, T. Mental Health of Children and Young People group. Child mental health in England before and during the COVID-19 lockdown. Lancet Psychiatry 2021, 8, 353–354. [Google Scholar] [CrossRef]
- Uccella, S.; De Grandis, E.; De Carli, F.; D’Apruzzo, M.; Siri, L.; Preiti, D.; Di Profio, S.; Rebora, S.; Cimellaro, P.; Biolcati Rinaldi, A.; et al. Impact of the COVID-19 Outbreak on the Behavior of Families in Italy: A Focus on Children and Adolescents. Front. Public Health 2021, 9, 608358. [Google Scholar] [CrossRef]
- Hill, R.M.; Rufino, K.; Kurian, S.; Saxena, J.; Saxena, K.; Williams, L. Suicide Ideation and Attempts in a Pediatric Emergency Department before and during COVID-19. Pediatrics 2021, 147, e2020029280. [Google Scholar] [CrossRef]
- Italian National Istitute of Statistics (ISTAT). Archive 2021. Available online: https://www.istat.it/en/archive/annual+report (accessed on 7 May 2023).
- Italian Ministry of Health. Emergency Indications for Welfare Activities and Prevention and Control Measures in the Departments of Mental Health and Child Neuropsychiatry Services of Childhood and Adolescence 2020. Official Gazette of the Italian Republic—Archive. 2020–2021. Available online: https://www.gazzettaufficiale.it/ (accessed on 7 May 2023).
- Lăzăroiu, G.; Horak, J.; Valaskova, K. Scaring ourselves to death in the time of COVID-19: Pandemic awareness, virus anxiety, and contagious fear. Linguist. Philos. Investig. 2020, 19, 114–120. [Google Scholar]
- Rodriguez, C.M.; Lee, S.J.; Ward, K.P.; Pu, D.F. The Perfect Storm: Hidden Risk of Child Maltreatment during the COVID-19 Pandemic. Child Maltreat. 2021, 26, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Raffaldi, I.; Castagno, E.; Fumi, I.; Bondone, C.; Ricceri, F.; Besenzon, L.; Brach Del Prever, A.; Capalbo, P.; Cosi, G.; Felici, E.; et al. ICOPER Study Group. Pediatric admissions to emergency departments of North-Western Italy during COVID-19 pandemic: A retrospective observational study. Lancet Reg. Health Eur. 2021, 5, 100081. [Google Scholar] [CrossRef] [PubMed]
- Lawson, M.; Piel, M.H.; Simon, M. Child Maltreatment during the COVID-19 Pandemic: Consequences of Parental Job Loss on Psychological and Physical Abuse Towards Children. Child Abus. Negl. 2020, 110 Pt 2, 104709. [Google Scholar] [CrossRef] [PubMed]
- Chadi, N.; Spinoso-Di Piano, C.; Osmanlliu, E.; Gravel, J.; Drouin, O. Mental Health-Related Emergency Department Visits in Adolescents before and during the COVID-19 Pandemic: A Multicentric Retrospective Study. J. Adolesc. Health 2021, 69, 847–850. [Google Scholar] [CrossRef]
- Dror, C.; Hertz-Palmor, N.; Barzilai, Y.; Gila, S.; Tali, B.Z.; Alex, G.; Tal, L.; Maya, K.L.; Talia, S.; Doron, G.; et al. Youth Psychiatric Hospitalization in Israel during COVID-19: A Multi-Center Study. Int. J. Environ. Res. Public Health 2022, 19, 9870. [Google Scholar] [CrossRef]
- Beaudry, G.; Drouin, O.; Gravel, J.; Smyrnova, A.; Bender, A.; Orri, M.; Geoffroy, M.C.; Chadi, N. A comparative analysis of pediatric mental health-related emergency department utilization in Montréal, Canada, before and during the COVID-19 pandemic. Ann. Gen. Psychiatry 2022, 21, 17. [Google Scholar] [CrossRef]
- Leeb, R.T.; Bitsko, R.H.; Radhakrishnan, L.; Martinez, P.; Njai, R.; Holland, K.M. Mental Health-Related Emergency Department Visits among Children Aged <18 Years during the COVID-19 Pandemic—United States, January 1–October 17, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1675–1680. [Google Scholar] [CrossRef]
- Davico, C.; Marcotulli, D.; Lux, C.; Calderoni, D.; Cammisa, L.; Bondone, C.; Rosa-Brusin, M.; Secci, I.; Porro, M.; Campanile, R.; et al. Impact of the COVID-19 Pandemic on Child and Adolescent Psychiatric Emergencies. J. Clin. Psychiatry 2021, 82, 20m13467. [Google Scholar] [CrossRef]
- Leff, R.A.; Setzer, E.; Cicero, M.X.; Auerbach, M. Changes in pediatric emergency department visits for mental health during the COVID-19 pandemic: A cross-sectional study. Clin. Child Psychol. Psychiatry 2021, 26, 33–38. [Google Scholar] [CrossRef]
- Penner, F.; Hernandez Ortiz, J.; Sharp, C. Change in Youth Mental Health during the COVID-19 Pandemic in a Majority Hispanic/Latinx US Sample. J. Am. Acad. Child Adolesc. Psychiatry 2021, 60, 513–523. [Google Scholar] [CrossRef] [PubMed]
- de Kloet, E.R.; Joëls, M.; Holsboer, F. Stress and the brain: From adaptation to disease. Nat. Rev. Neurosci. 2005, 6, 463–475. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Xu, D.; Wang, J.; Shen, Y.; Lin, Z.; Ruan, L.; Chen, Q. Gender differences in psychiatric outpatients: A before and during COVID-19 pandemic study in general hospitals from China. Ann. Gen. Psychiatry 2022, 21, 35. [Google Scholar] [CrossRef] [PubMed]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239.e3. [Google Scholar] [CrossRef] [PubMed]
- Oosterhoff, B.; Palmer, C.A.; Wilson, J.; Shook, N. Adolescents’ Motivations to Engage in Social Distancing during the COVID-19 Pandemic: Associations with Mental and Social Health. J. Adolesc. Health 2020, 67, 179–185. [Google Scholar] [CrossRef]
- Vitousek, K.B.; Hollon, S.D. The investigation of schematic content and processing in eating disorders. Cogn. Ther. Res. 1990, 14, 191–214. [Google Scholar] [CrossRef]
- ARS Tuscany. The Behaviours, Habits, and Lifestyles of the Tuscan Adolescent Population before and during the COVID-19 Pandemic, the Results of the Survey EDIT. 2022. Available online: https://www.ars.toscana.it/ (accessed on 7 May 2023).
- Dalle Grave, R.; Calugi, S.; Sartirana, M. Cognitive Behavior Therapy for Adolescents with Eating Disorders (CBT-Ea); Positive Press: Verona, Italy, 2018. [Google Scholar]
- Otto, A.K.; Jary, J.M.; Sturza, J.; Miller, C.A.; Prohaska, N.; Bravender, T.; Van Huysse, J. Medical Admissions among Adolescents with Eating Disorders during the COVID-19 Pandemic. Pediatrics 2021, 148, e2021052201. [Google Scholar] [CrossRef]
- Mereu, A.; Fantoni, T.; Caini, S.; Monzali, F.; Roselli, E.; Taddei, S.; Lucarelli, S.; Pisano, T. Suicidality in adolescents with onset of anorexia nervosa. Eat. Weight Disord. 2022, 27, 2447–2457. [Google Scholar] [CrossRef]
- Liu, Q.; Zhou, Y.; Xie, X.; Xue, Q.; Zhu, K.; Wan, Z.; Wu, H.; Zhang, J.; Song, R. The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in china. J. Affect. Disord. 2021, 279, 412–416. [Google Scholar] [CrossRef]
- Liu, D.; Baumeister, R.F.; Zhou, Y. Mental health outcomes of coronavirus infection survivors: A rapid meta-analysis. J. Psychiatr. Res. 2021, 137, 542–553. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Liu, Y.; Liu, Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Res. 2020, 289, 113070. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Giannitto, N.; Squarcia, A.; Neglia, C.; Argentiero, A.; Minichetti, P.; Cotugno, N.; Principi, N. Development of Psychological Problems among Adolescents during School Closures Because of the COVID-19 Lockdown Phase in Italy: A Cross-Sectional Survey. Front. Pediatr. 2021, 8, 628072. [Google Scholar] [CrossRef]
- Yue, J.; Zang, X.; Le, Y.; An, Y. Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID-19) outbreak in China. Curr. Psychol. 2022, 41, 5723–5730. [Google Scholar] [CrossRef] [PubMed]
- Gassman-Pines, A.; Ananat, E.O.; Fitz-Henley, J., II. COVID-19 and Parent-Child Psychological Well-being. Pediatrics 2020, 146, e2020007294. [Google Scholar] [CrossRef] [PubMed]
- Patrick, S.W.; Henkhaus, L.E.; Zickafoose, J.S.; Lovell, K.; Halvorson, A.; Loch, S.; Letterie, M.; Davis, M.M. Well-being of Parents and Children during the COVID-19 Pandemic: A National Survey. Pediatrics 2020, 146, e2020016824. [Google Scholar] [CrossRef]
- Cancilliere, M.K.; Donise, K. A Comparison of Acute Mental Health Presentations to Emergency Services before and during the COVID-19 Pandemic. R. Isl. Med. J. 2022, 105, 9–15. [Google Scholar]
- Bratu, S. The fake news sociology of COVID-19 pandemic fear: Dangerously inaccurate beliefs, emotional contagion, and conspiracy ideation. Linguist. Philos. Investig. 2020, 19, 128–134. [Google Scholar]
| Decrees and Levels (2020) | Decrees and Levels (2021) |
|---|---|
| - | 14 January (LS-3) |
| - | 12, 23 February (LS-4) |
| 1, 4, 8, 11, 20, 22, 25 March 2020 (LS-5) | 2 March 2021 (LS-4) |
| 10, 23, 26 April 2020 (LS-5) | 22 April 2021 (LS5) |
| 17 May 2020 (LS-5) | 18 May 2021 (LS-2) |
| 11 June 2020 (LS-2) | No decrees (LS-2) |
| No decrees (LS-2) | 23 July 2021 (LS-1) |
| No decrees (LS-2) | 6 August 2021 (LS-1) |
| 7 September 2020 (LS-2) | No decrees (LS-1) |
| 13, 18, 24 October 2020 (LS-3) | 8 October 2021 (LS-1) |
| 3 November 2020 (LS-5) | No decrees (LS-1) |
| 2, 3 December 2020 (LS-5) | 24 December 2021 (LS-2) |
| Year | Total Admissions in ER | MH Admissions (N and Percentage of Total) | New MH (N and Percentage of Total) | Relapses MH (N and Percentage of Total) |
|---|---|---|---|---|
| 2018–2021 | 143,909 | 1311/143,909 (0.91%) | 384/1311 (29.3%) | 927 (70.7%) |
| 2018 | 42,923 | 226/42,923 (0.53%) | 79/226 (35%) | 147 (65%) |
| 2019 | 43,111 | 290/4311 (0.67%) | 73/290 (25.2%) | 217 (74.8%) |
| 2020 | 24,906 | 258/24,906 (1.04%) | 76/258 (29.5%) | 182 (70.5%) |
| 2021 | 32,969 | 537/32,969 (1.63%) | 156/537 (29.1%) | 381 (70.9%) |
| Pandemic Period (March 2020–December 2021) | ||||
|---|---|---|---|---|
| / | 2020 | 2021 | ||
| Month | Levels | Admissions | Levels | Admissions |
| January | / | / | LS-3 | 39 |
| February | / | / | LS-4 | 28 |
| March | LS-5 | 9 | LS-4 | 34 |
| April | LS-5 | 17 | LS-5 | 47 |
| May | LS-5 | 20 | LS-2 | 64 |
| June | LS-2 | 16 | LS-2 | 49 |
| July | LS-2 | 21 | LS-1 | 36 |
| August | LS-2 | 21 | LS-1 | 42 |
| September | LS-2 | 35 | LS-1 | 42 |
| October | LS-3 | 22 | LS-1 | 37 |
| November | LS-5 | 20 | LS-1 | 61 |
| December | LS-5 | 29 | LS-2 | 58 |
| Admission Symptoms for Psychiatric Clinical Presentations | Pre-Pandemic Period (January 2018–February 2020) | Pandemic Period (March 2020–December 2021) | ||
|---|---|---|---|---|
| Psychomotor agitation | 230 | 40.8% | 221 | 29.5% |
| Anxiety symptoms | 108 | 19.1% | 114 | 15.3% |
| Somatic symptoms | 49 | 8.7% | 43 | 5.7% |
| Suicide attempt | 40 | 7.1% | 65 | 8.7% |
| Eating disorder | 34 | 6.1% | 127 | 17% |
| Self-harm | 30 | 5.3% | 52 | 7.1% |
| Affective symptoms | 28 | 4.9% | 46 | 6.1% |
| Suicidal ideation | 27 | 4.8% | 53 | 7.1% |
| Psychotic symptoms | 18 | 3.2% | 26 | 3.5% |
| Admission Symptoms for Psychiatric Clinical Presentations | Pre-Pandemic Period (January 2018–February 2020) | Admission Symptoms for Psychiatric Clinical Presentations | Pandemic Period (March 2020–December 2021) | ||||
|---|---|---|---|---|---|---|---|
| Affective symptoms | DD (52.2%) | FEDs (8.7%) | DIC (8.7%) | Affective symptoms | DD (72.2%) | DIC (8.3%) | FEDs (8.3%) |
| Suicidal ideation | DD (65%) | ID (15%) | Bipolar disorders (10%) | Suicidal ideation | DD (61%) | FEDs (14.6%) | Bipolar disorders (7.3%) |
| Suicide attempt | DD (53.6%) | FEDs (17.9%) | Anxiety disorders (7.1%) | Suicide attempt | DD (66.7%) | FEDs (16.7%) | Schizophrenia (4.2%) |
| Self-harm | DD (34.8%) | FEDs (17.4%) | Bipolar disorders (8.7%) | Self-harm | DD (45.7%) | FEDs (17.1%) | Anxiety disorders (8.6%) |
| Anxiety symptoms | Anxiety disorders (53.1%) | DD (12.2%) | None (10.02%) | Anxiety symptoms | Anxiety disorders (62.1%) | DD (17.2%) | None (10.3%) |
| Psychotic symptoms | Schizophrenia (50%) | ID (12.5%) | Depressive disorders (12.5%) | Psychotic symptoms | Schizophrenia (30%) | DD (20%) | DIC (10%) |
| Eating disorder | FEDs (72.7%) | None (13.6%) | Intellectual disabilities (9.1%) | Eating disorder | FEDs (88.8%) | DD (3.7%) | Anxiety disorders (1.2%) |
| Somatic symptoms | Somatic disorders (60%) | ID (10%) | ADHD (10%) | Somatic symptoms | Somatic disorders (33.3%) | None (18.5%) | DD (14.8%) |
| Psychomotor agitation | DD (33.2%) | ID (15.8%) | ASD (10.2%) | Psychomotor agitation | DIC (29.7%) | ID (17.1%) | ADHD (12.6%) |
| OR | 95% CI | p-Value | |
|---|---|---|---|
| Psychomotor agitation | |||
| Age (+1 year) | 1.18 | 1.08–1.30 | <0.001 |
| Anxiety symptoms | |||
| Previous access | |||
| No | 1.00 | ||
| Yes, and this is a relapse | 10.28 | 1.01–105.12 | 0.049 |
| Yes, but this is not a relapse | - | - | - |
| Treatment: educational (yes vs. no) | 83.27 | 4.15–1670.55 | 0.004 |
| Eating disorder | |||
| Previous access | |||
| No | 100 | ||
| Yes, and this is a relapse | 0.33 | 0.10–1.11 | 0.074 |
| Yes, but this is not a relapse | 0.10 | 0.01–1.22 | 0.071 |
| Treatment: psychotherapy (yes vs. no) | 0.31 | 0.14–0.072 | 0.006 |
| Somatic symptoms | |||
| Sex | |||
| Female | 1.00 | ||
| Male | 0.08 | 0.01–0.72 | 0.024 |
| Treatment: drugs (yes vs. no) | 0.18 | 0.04–0.77 | 0.021 |
| Treatment: psychotherapy (yes vs. no) | 9.92 | 2.54–38.72 | 0.001 |
| Affective symptoms | |||
| Age (+1 year) | 1.64 | 1.11–2.42 | 0.013 |
| Psychotic symptoms | |||
| Previous access | |||
| No | 1.00 | ||
| Yes, and this is a relapse | 0.20 | 0.05–0.79 | 0.022 |
| Yes, but this is not a relapse | 0.30 | 0.02–2.42 | 0.260 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tavano, S.; Caini, S.; Sforzi, I.; Silvestri, C.; Voller, F.; Pisano, T. Mental Health of Children and Adolescents before and during the COVID-19 Pandemic: How Did the Lockdown Modify Psychiatric Emergencies in Tuscany, Italy? J. Clin. Med. 2023, 12, 4154. https://doi.org/10.3390/jcm12124154
Tavano S, Caini S, Sforzi I, Silvestri C, Voller F, Pisano T. Mental Health of Children and Adolescents before and during the COVID-19 Pandemic: How Did the Lockdown Modify Psychiatric Emergencies in Tuscany, Italy? Journal of Clinical Medicine. 2023; 12(12):4154. https://doi.org/10.3390/jcm12124154
Chicago/Turabian StyleTavano, Simone, Saverio Caini, Idanna Sforzi, Caterina Silvestri, Fabio Voller, and Tiziana Pisano. 2023. "Mental Health of Children and Adolescents before and during the COVID-19 Pandemic: How Did the Lockdown Modify Psychiatric Emergencies in Tuscany, Italy?" Journal of Clinical Medicine 12, no. 12: 4154. https://doi.org/10.3390/jcm12124154
APA StyleTavano, S., Caini, S., Sforzi, I., Silvestri, C., Voller, F., & Pisano, T. (2023). Mental Health of Children and Adolescents before and during the COVID-19 Pandemic: How Did the Lockdown Modify Psychiatric Emergencies in Tuscany, Italy? Journal of Clinical Medicine, 12(12), 4154. https://doi.org/10.3390/jcm12124154