Successful Preventive Treatment of Oncogenic Transforming HPV Infections in Low-Grade Cytology (ASC-US/LSIL) Patients with an Adsorptive and Antioxidant Vaginal Gel
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Group
2.2. Treatment
2.3. Methods
2.4. Data Evaluation and Statistics
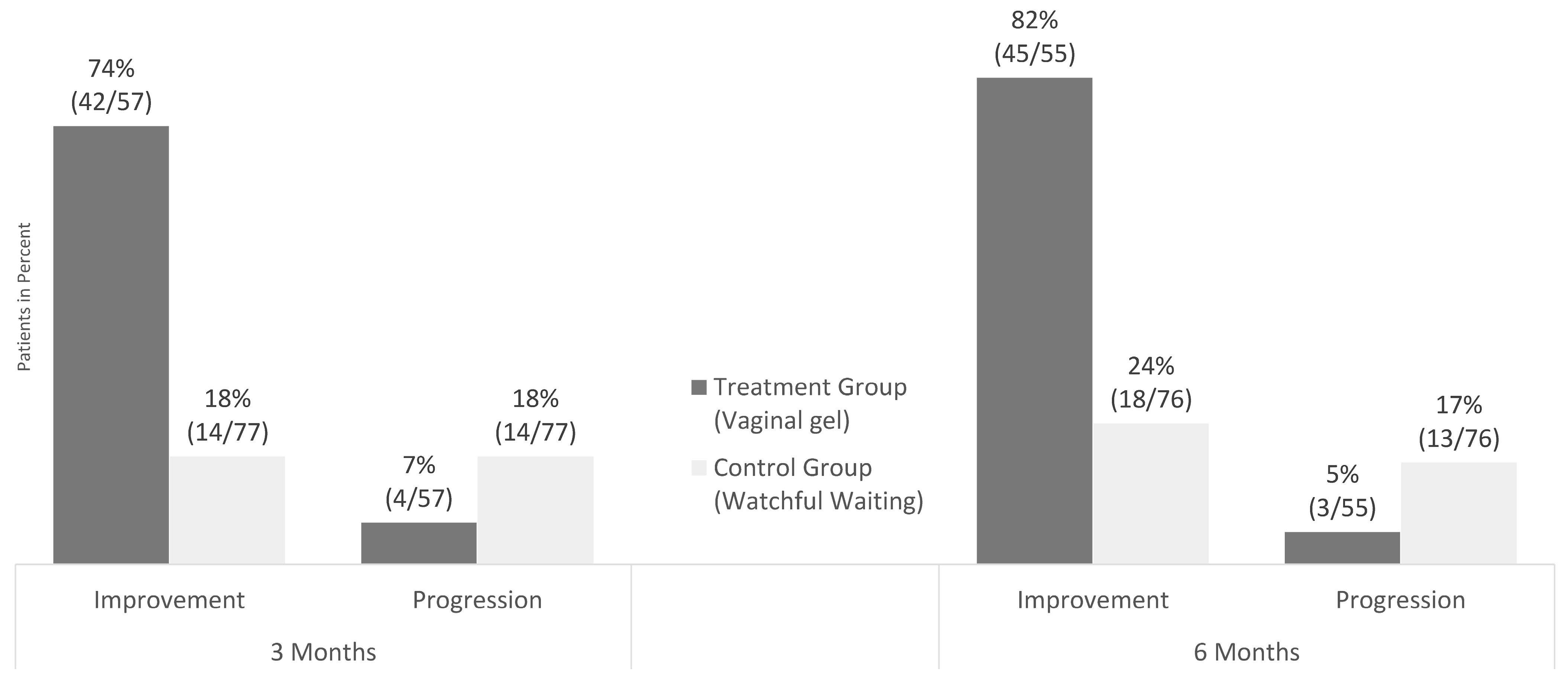
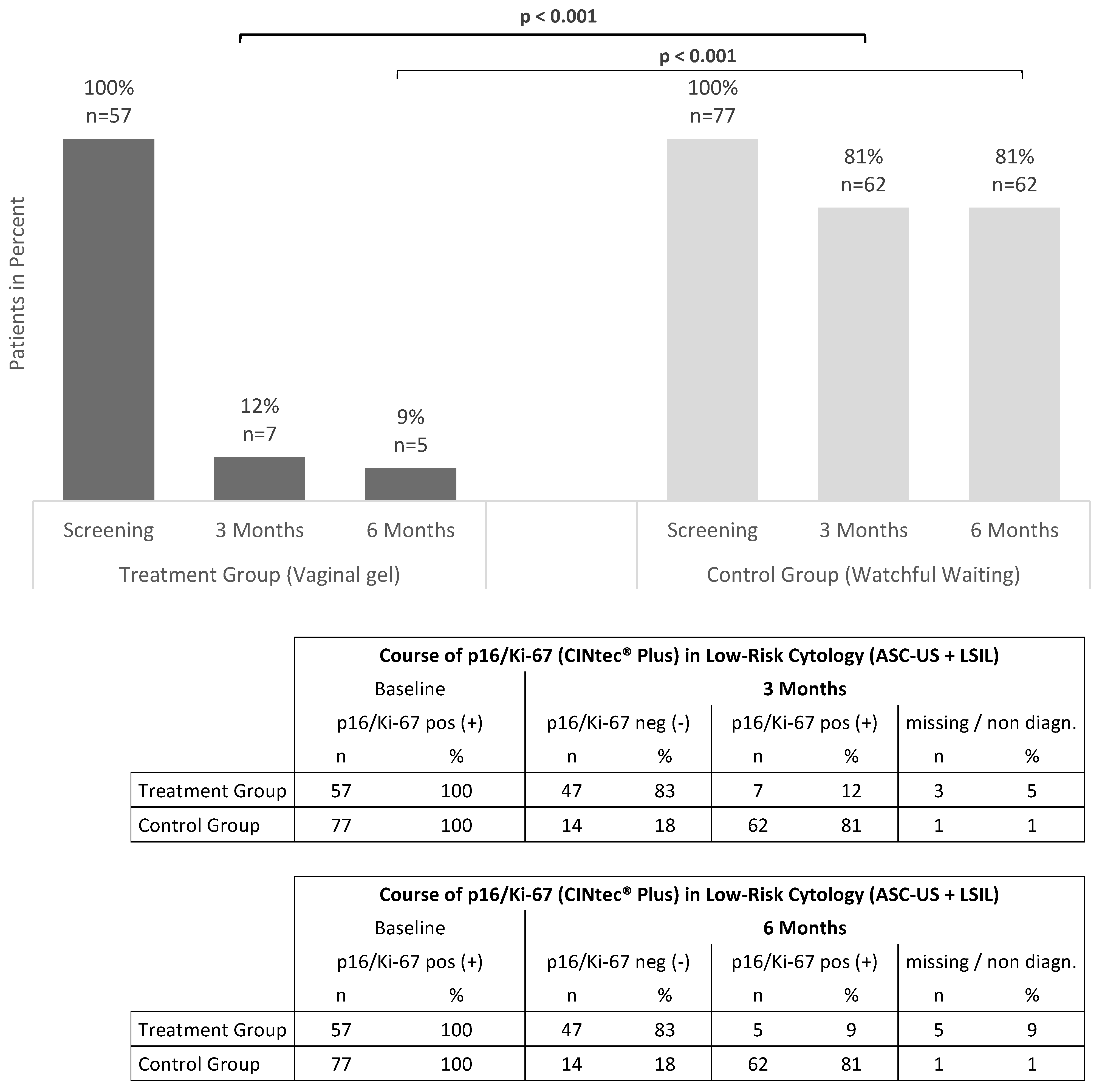
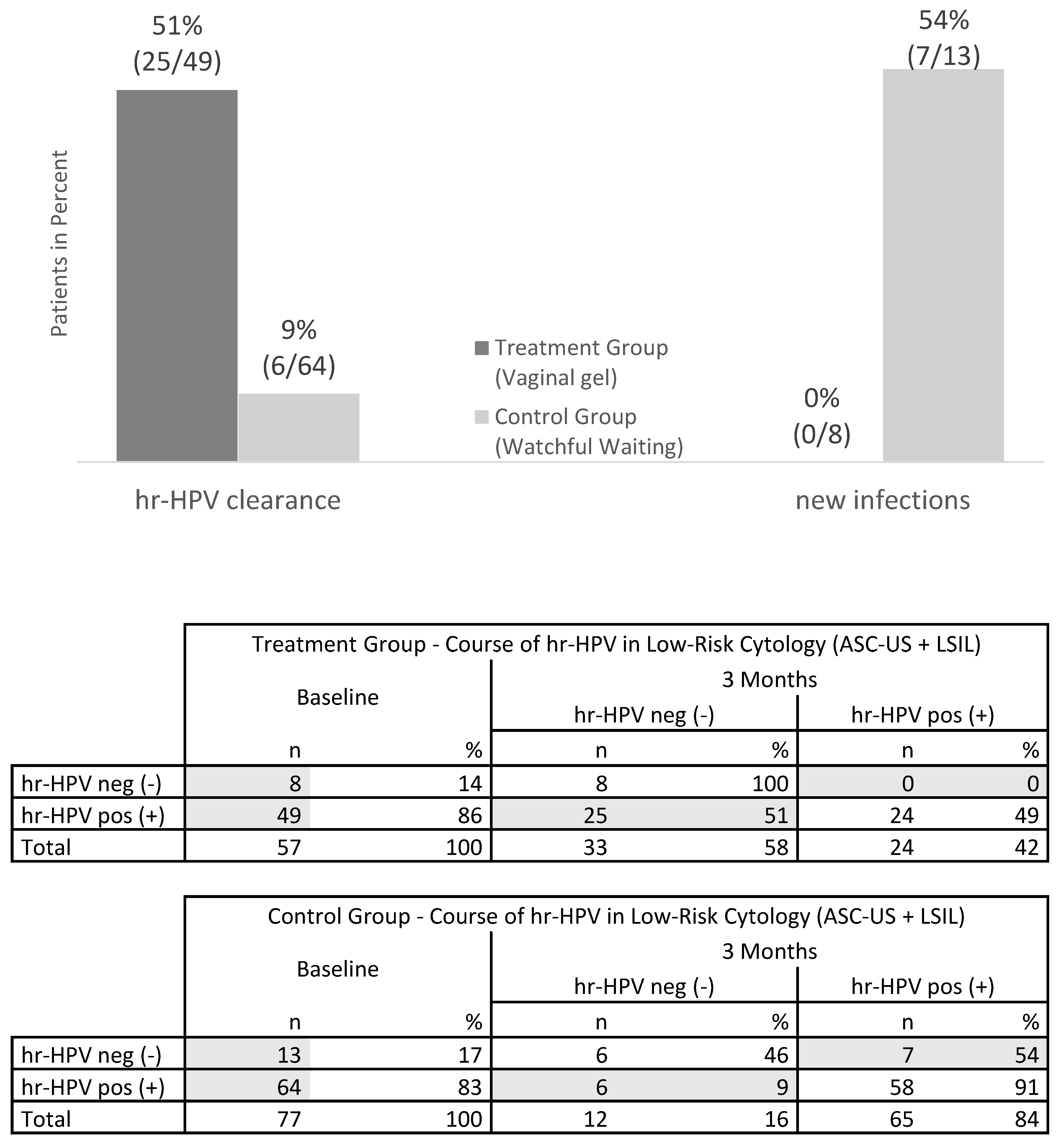
3. Results
4. Discussion
4.1. Summary of the Main Results
4.2. Results in the Context of Published Literature
4.3. Strengths and Weaknesses
4.4. Implications for Practice and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Okunade, K.S. Human papillomavirus and cervical cancer. J. Obstet. Gynaecol. 2020, 40, 602–608. [Google Scholar] [CrossRef]
- Vink, M.A.; Bogaards, J.A.; van Kemenade, F.J.; de Melker, H.E.; Meijer, C.J.; Berkhof, J. Clinical progression of high-grade cervical intraepithelial neoplasia: Estimating the time to preclinical cervical cancer from doubly censored national registry data. Am. J. Epidemiol. 2013, 178, 1161–1169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perkins, R.B.; Guido, R.S.; Castle, P.E.; Chelmow, D.; Einstein, M.H.; Garcia, F.; Huh, W.K.; Kim, J.J.; Moscicki, A.B.; Nayar, R.; et al. 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors. J. Low Genit. Tract Dis. 2020, 24, 102–131, Erratum in J. Low Genit. Tract Dis. 2020, 24, 427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogstad, K.E. The psychological impact of abnormal cytology and colposcopy. BJOG 2002, 109, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Williams, V.M.; Filippova, M.; Soto, U.; Duerksen-Hughes, P.J. HPV-DNA integration and carcinogenesis: Putative roles for inflammation and oxidative stress. Future Virol. 2011, 6, 45–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hudelist, G.; Manavi, M.; Pischinger, K.I.; Watkins-Riedel, T.; Singer, C.F.; Kubista, E.; Czerwenka, K.F. Physical state and expression of HPV DNA in benign and dysplastic cervical tissue: Different levels of viral integration are correlated with lesion grade. Gynecol. Oncol. 2004, 92, 873–880. [Google Scholar] [CrossRef]
- Chen Wongworawat, Y.; Filippova, M.; Williams, V.M.; Filippov, V.; Duerksen-Hughes, P.J. Chronic oxidative stress increases the integration frequency of foreign DNA and human papillomavirus 16 in human keratinocytes. Am. J. Cancer Res. 2016, 6, 764–780. [Google Scholar] [PubMed]
- Sgambato, A.; Zannoni, G.F.; Faraglia, B.; Camerini, A.; Tarquini, E.; Spada, D.; Cittadini, A. Decreased expression of the CDK inhibitor p27Kip1 and increased oxidative DNA damage in the multistep process of cervical carcinogenesis. Gynecol. Oncol. 2004, 92, 776–783. [Google Scholar] [CrossRef]
- Georgescu, S.R.; Mitran, C.I.; Mitran, M.I.; Caruntu, C.; Sarbu, M.I.; Matei, C.; Nicolae, I.; Tocut, S.M.; Popa, M.I.; Tampa, M. New Insights in the Pathogenesis of HPV Infection and the Associated Carcinogenic Processes: The Role of Chronic Inflammation and Oxidative Stress. J. Immunol. Res. 2018, 2018, 5315816. [Google Scholar] [CrossRef] [Green Version]
- Sadler, L.; Saftlas, A.; Wang, W.; Exeter, M.; Whittaker, J.; McCowan, L. Treatment for cervical intraepithelial neoplasia and risk of preterm delivery. JAMA 2004, 291, 2100–2106. [Google Scholar] [CrossRef] [Green Version]
- Donnez, J. An update on uterine cervix pathologies related to infertility. Fertil. Steril. 2020, 113, 683–684. [Google Scholar] [CrossRef] [PubMed]
- Huber, J.; Mueller, A.; Sailer, M.; Regidor, P.A. Human papillomavirus persistence or clearance after infection in reproductive age. What is the status? Review of the literature and new data of a vaginal gel containing silicate dioxide, citric acid, and selenite. Womens Health 2021, 17, 17455065211020702. [Google Scholar] [CrossRef] [PubMed]
- Demarco, M.; Lorey, T.S.; Fetterman, B.; Cheung, L.C.; Guido, R.S.; Wentzensen, N.; Kinney, W.K.; Poitras, N.E.; Befano, B.; Castle, P.E.; et al. Risks of CIN 2+, CIN 3+, and Cancer by Cytology and Human Papillomavirus Status: The Foundation of Risk-Based Cervical Screening Guidelines. J. Low Genit. Tract Dis. 2017, 21, 261–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kjær, S.K.; Frederiksen, K.; Munk, C.; Iftner, T. Long-term absolute risk of cervical intraepithelial neoplasia grade 3 or worse following human papillomavirus infection: Role of persistence. J. Natl. Cancer Inst. 2010, 102, 1478–1488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, D.C.; Goncalves, A.K.; Cobucci, R.N.; Mendonca, R.C.; Lima, P.H.; Cavalcanti, G.J. Immunohistochemical Expression of P16, Ki-67 and P53 in Cervical Lesions-A Systematic Review. Pathol. Res. Pract. 2017, 213, 723–729. [Google Scholar] [CrossRef]
- Vousden, K.H. Regulation of the cell cycle by viral oncoproteins. Semin. Cancer Biol. 1995, 6, 109–116. [Google Scholar] [CrossRef] [PubMed]
- von Keyserling, H.; Kuhn, W.; Schneider, A.; Bergmann, T.; Kaufmann, A.M. P16ink(4)a and P14arf mRNA Expression in Pap Smears Is Age-Related. Mod. Pathol. 2012, 25, 465–470. [Google Scholar] [CrossRef] [Green Version]
- Major, A.L.; Dvořák, V.; Schwarzová, J.; Skřivánek, A.; Malík, T.; Pluta, M.; Mayboroda, I.; Grandjean, E.M. Efficacy and safety of an adsorbent and anti-oxidative vaginal gel on CIN1 and 2, on high-risk HPV, and on p16/Ki-67: A randomized controlled trial. Arch. Gynecol. Obstet. 2021, 303, 501–511. [Google Scholar] [CrossRef]
- Major, A.L.; Skřivánek, A.; Grandjean, E.M.; Dvořák, V.; Malík, T.; Pluta, M.; Mayboroda, I. An Adsorptive and Antioxidant Vaginal Gel Clears High-Risk HPV- and p16/Ki-67-Associated Abnormal Cytological Cervical Findings: A post-hoc Subgroup Analysis of a Prospective Randomized Controlled Trial on CIN2 and p16 Positive CIN1. Front. Med. 2021, 8, 645559. [Google Scholar] [CrossRef]
- Liu, W.; Gong, J.; Xu, H.; Zhang, D.; Xia, N.; Li, H.; Song, K.; Lv, T.; Chen, Y.; Diao, Y.; et al. Good Performance of p16/Ki-67 Dual-Stain Cytology for Detection and Post-Treatment Surveillance of High-Grade CIN/VAIN in a Prospective, Cross-Sectional Study. Diagn. Cytopathol. 2020, 48, 635–644. [Google Scholar] [CrossRef]
- Zhu, Y.; Ren, C.; Yang, L.; Zhang, X.; Liu, L.; Wang, Z. Performance of p16/Ki67 immunostaining, HPV E6/E7 mRNA testing, and HPV DNA assay to detect high-grade cervical dysplasia in women with ASCUS. BMC Cancer 2019, 19, 271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wentzensen, N.; Schwartz, L.; Zuna, R.E.; Smith, K.; Mathews, C.; Gold, M.A.; Allen, R.A.; Zhang, R.; Dunn, S.T.; Walker, J.L.; et al. Performance of p16/Ki-67 Immunostaining to Detect Cervical Cancer Precursors in a Colposcopy Referral Population. Clin. Cancer Res. 2012, 18, 4154–4162. [Google Scholar] [CrossRef] [Green Version]
- Wentzensen, N.; Clarke, M.A.; Bremer, R.; Poitras, N.; Tokugawa, D.; Goldhoff, P.E.; Castle, P.E.; Schiffman, M.; Kingery, J.D.; Grewal, K.K.; et al. Clinical Evaluation of Human Papillomavirus Screening With p16/Ki-67 Dual Stain Triage in a Large Organized Cervical Cancer Screening Program. JAMA Intern. Med. 2019, 179, 881–888. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rezwan, K.; Meier, L.P.; Gauckler, L.J. Lysozyme and bovine serum albumin adsorption on uncoated silica and AlOOH-coated silica particles: The influence of positively and negatively charged oxide surface coatings. Biomaterials 2005, 26, 4351–4357. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.G.; Johnston, C.; Oberdorster, G.; Finkelstein, J.N. Silica binds serum proteins resulting in a shift of the dose-response for silica-induced chemokine expression in an alveolar type II cell line. Toxicol. Appl. Pharmacol. 1999, 161, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.P.; Laband, S.J. Degradation of poliovirus by adsorption on inorganic surfaces. Appl. Environ. Microbiol. 1979, 37, 480–486. [Google Scholar] [CrossRef] [Green Version]
- Gordienko, A.S.; Kurdish, I.K. Electrical properties and interaction with silicon dioxide particles of Bacillus subtilis cells. Biofizika 2007, 52, 314–317. [Google Scholar] [CrossRef]
- Kuklinski, B.; Kössler, P.; Fuchs, N. Use of Selenite-Containing Compounds to be Topically or Buccally Administered. WO2003047604A, 13 August 2008. European Patent Office, EP No. 1 450 825 B1. [Google Scholar]
- Short, R.V. New ways of preventing HIV infection: Thinking simply, simply thinking. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2006, 361, 811–820. [Google Scholar] [CrossRef] [Green Version]
- Clarke, M.A.; Rodriguez, A.C.; Gage, J.C.; Herrero, R.; Hildesheim, A.; Wacholder, S.; Burk, R.; Schiffman, M. A large, population-based study of age-related associations between vaginal pH and human papillomavirus infection. BMC Infect. Dis. 2012, 12, 33. [Google Scholar] [CrossRef] [Green Version]
- Faro, S. Vaginitis: Diagnosis and management. Int. J. Fertil. Menopausal Stud. 1996, 41, 115–123. [Google Scholar]
- Katki, H.A.; Gage, J.C.; Schiffman, M.; Castle, P.E.; Fetterman, B.; Poitras, N.E.; Lorey, T.; Cheung, L.C.; Raine-Bennett, T.; Kinney, W.K. Follow-up testing after colposcopy: Five-year risk of CIN 2+ after a colposcopic diagnosis of CIN 1 or less. J. Low Genit. Tract Dis. 2013, 17 (Suppl. S1), 69–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huber, J.; Pötsch, B.; Gantschacher, M.; Templ, M. Routine Treatment of Cervical Cytological Cell Changes: Diagnostic Standard, Prevention and Routine Treatment of Cervical Cytological Cell Changes-An Assessment of Primary and Secondary Prevention and Routine Treatment Data in the Context of an Anonymous Data Collection from Practicing Gynaecologists; an Academic, Non-Interventional Study. Geburtshilfe Frauenheilkd. 2016, 76, 1086–1091. [Google Scholar] [PubMed] [Green Version]
- White, C.; Bakhiet, S.; Bates, M.; Keegan, H.; Pilkington, L.; Ruttle, C.; Sharp, L.; O’ Toole, S.; Fitzpatrick, M.; Flannelly, G.; et al. Triage of LSIL/ASC-US With p16/Ki-67 Dual Staining and Human Papillomavirus Testing: A 2-year Prospective Study. Cytopathology 2016, 27, 269–276. [Google Scholar] [CrossRef] [Green Version]
- Clarke, M.A.; Cheung, L.C.; Castle, P.E.; Schiffman, M.; Tokugawa, D.; Poitras, N.; Lorey, T.; Kinney, W.; Wentzensen, N. Five-Year Risk of Cervical Precancer Following p16/Ki-67 Dual-Stain Triage of HPV-Positive Women. JAMA Oncol. 2019, 5, 181–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melnikow, J.; Henderson, J.T.; Burda, B.U.; Senger, C.A.; Durbin, S.; Weyrich, M.S. Screening for Cervical Cancer With High-Risk Human Papillomavirus Testing: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2018, 320, 687–705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grimm, C.; Polterauer, S.; Natter, C.; Rahhal, J.; Hefler, L.; Tempfer, C.B.; Heinze, G.; Stary, G.; Reinthaller, A.; Speiser, P. Treatment of cervical intraepithelial neoplasia with topical imiquimod: A randomized controlled trial. Obstet. Gynecol. 2012, 120, 152–159. [Google Scholar] [CrossRef] [Green Version]
- Polterauer, S.; Reich, O.; Widschwendter, A.; Hadjari, L.; Bogner, G.; Reinthaller, A.; Joura, E.; Trutnovsky, G.; Ciresa-Koenig, A.; Ganhoer-Schimboeck, J.; et al. Topical imiquimod compared with conization to treat cervical high-grade squamous intraepithelial lesions: Multicenter, randomized controlled trial. Gynecol. Oncol. 2022, 165, 23–29. [Google Scholar] [CrossRef]
- Koeneman, M.M.; Kruse, A.J.; Kooreman, L.F.; Zur Hausen, A.; Hopman, A.H.; Sep, S.J.; Van Gorp, T.; Slangen, B.F.; van Beekhuizen, H.J.; van de Sande, A.J.; et al. Preliminary stop of the TOPical Imiquimod treatment of high-grade Cervical intraepithelial neoplasia (TOPIC) trial. BMC Cancer 2017, 17, 110. [Google Scholar] [CrossRef] [Green Version]
- Wouters, T.; Hendriks, N.; Koeneman, M.; Kruse, A.J.; van de Sande, A.; van Beekhuizen, H.J.; Gerestein, K.G.; Bekkers, R.L.M.; Piek, J.M.J. Systemic adverse events in imiquimod use for cervical intraepithelial neoplasia–A case series. Case Rep. Womens Health 2019, 21, e00105. [Google Scholar] [CrossRef]
- Wang, H.; Ma, Y.; Li, R.; Chen, X.; Wan, L.; Zhao, W. Associations of Cervicovaginal Lactobacilli With High-Risk Human Papillomavirus Infection, Cervical Intraepithelial Neoplasia, and Cancer: A Systematic Review and Meta-Analysis. J. Infect. Dis. 2019, 220, 1243–1254. [Google Scholar] [CrossRef]
- Norenhag, J.; Du, J.; Olovsson, M.; Verstraelen, H.; Engstrand, L.; Brusselaers, N. The vaginal microbiota, human papillomavirus and cervical dysplasia: A systematic review and network meta-analysis. BJOG 2020, 127, 171–180. [Google Scholar] [CrossRef] [PubMed]
| Treatment Group (n = 57) | Control Group (n = 77) | p | ||||
|---|---|---|---|---|---|---|
| Age (years) Mean ± SD | 32.98 | ±6.78 | 35.16 | ±8.60 | 0.152 + | |
| Relevant gynecological history ** | 2 | 3.51% | 16 | 20.78% | 0.004 x | |
| Smoking | 18 | 31.58% | 17 | 22.08% | 0.237 x | |
| HPV vaccination | 10 | 17.54% | 12 | 15.58% | 0.816 x | |
| Histology § | CIN1 | 35 | 61.40% | 71 | 92.21% | <0.001 x |
| CIN2 | 22 | 38.60% | 6 | 7.79% | ||
| Total | 57 | 100.00% | 77 | 100.00% | ||
| Cytology | ASC-US | 17 | 22.70% | 20 | 20.60% | 0.697 * |
| LSIL | 40 | 53.30% | 57 | 58.80% | ||
| Total | 57 | 100.00% | 77 | 100.00% | ||
| High-risk HPV §§ | Yes | 49 | 85.96% | 64 | 83.12% | 0.811 x |
| No | 8 | 14.04% | 13 | 16.88% | ||
| Total | 57 | 100.00% | 77 | 100.00% | ||
| p16/Ki-67 §§§ (CINtec® Plus) | CIN1 | 35 | 61.40% | 71 | 92.21% | <0.001 x |
| CIN2 | 22 | 38.60% | 6 | 7.79% | ||
| Total | 57 | 100.00% | 77 | 100.00% | ||
| IHC p16 §§§§ | CIN1 | 30/35 | 85.71% | 37/71 | 52.11% | <0.001 * |
| CIN2 | 22/22 | 100.00% | 6/6 | 100.00% | ||
| Total | 52/57 | 91.23% | 43/77 | 55.84% | ||
| High-Risk HPV | CIN1 | 29/35 | 82.86% | 58/71 | 81.69% | n.a. |
| CIN2 | 20/22 | 90.91% | 6/6 | 100.00% | ||
| Total | 49/57 | 85.96% | 64/77 | 83.12% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Major, A.L.; Mayboroda, I.; Riger, A. Successful Preventive Treatment of Oncogenic Transforming HPV Infections in Low-Grade Cytology (ASC-US/LSIL) Patients with an Adsorptive and Antioxidant Vaginal Gel. J. Clin. Med. 2023, 12, 4142. https://doi.org/10.3390/jcm12124142
Major AL, Mayboroda I, Riger A. Successful Preventive Treatment of Oncogenic Transforming HPV Infections in Low-Grade Cytology (ASC-US/LSIL) Patients with an Adsorptive and Antioxidant Vaginal Gel. Journal of Clinical Medicine. 2023; 12(12):4142. https://doi.org/10.3390/jcm12124142
Chicago/Turabian StyleMajor, Attila Louis, Ivanna Mayboroda, and Alexandra Riger. 2023. "Successful Preventive Treatment of Oncogenic Transforming HPV Infections in Low-Grade Cytology (ASC-US/LSIL) Patients with an Adsorptive and Antioxidant Vaginal Gel" Journal of Clinical Medicine 12, no. 12: 4142. https://doi.org/10.3390/jcm12124142
APA StyleMajor, A. L., Mayboroda, I., & Riger, A. (2023). Successful Preventive Treatment of Oncogenic Transforming HPV Infections in Low-Grade Cytology (ASC-US/LSIL) Patients with an Adsorptive and Antioxidant Vaginal Gel. Journal of Clinical Medicine, 12(12), 4142. https://doi.org/10.3390/jcm12124142






