Long-Term Outcome and Athletic Level following Operative Treatment for Osteochondritis Dissecans of the Knee in Pediatric and Adolescent Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Defect Size, Depth, and Localization
2.2. Surgical Intervention and Revisions
2.3. Subjective Knee Scores and Sports Questionnaires
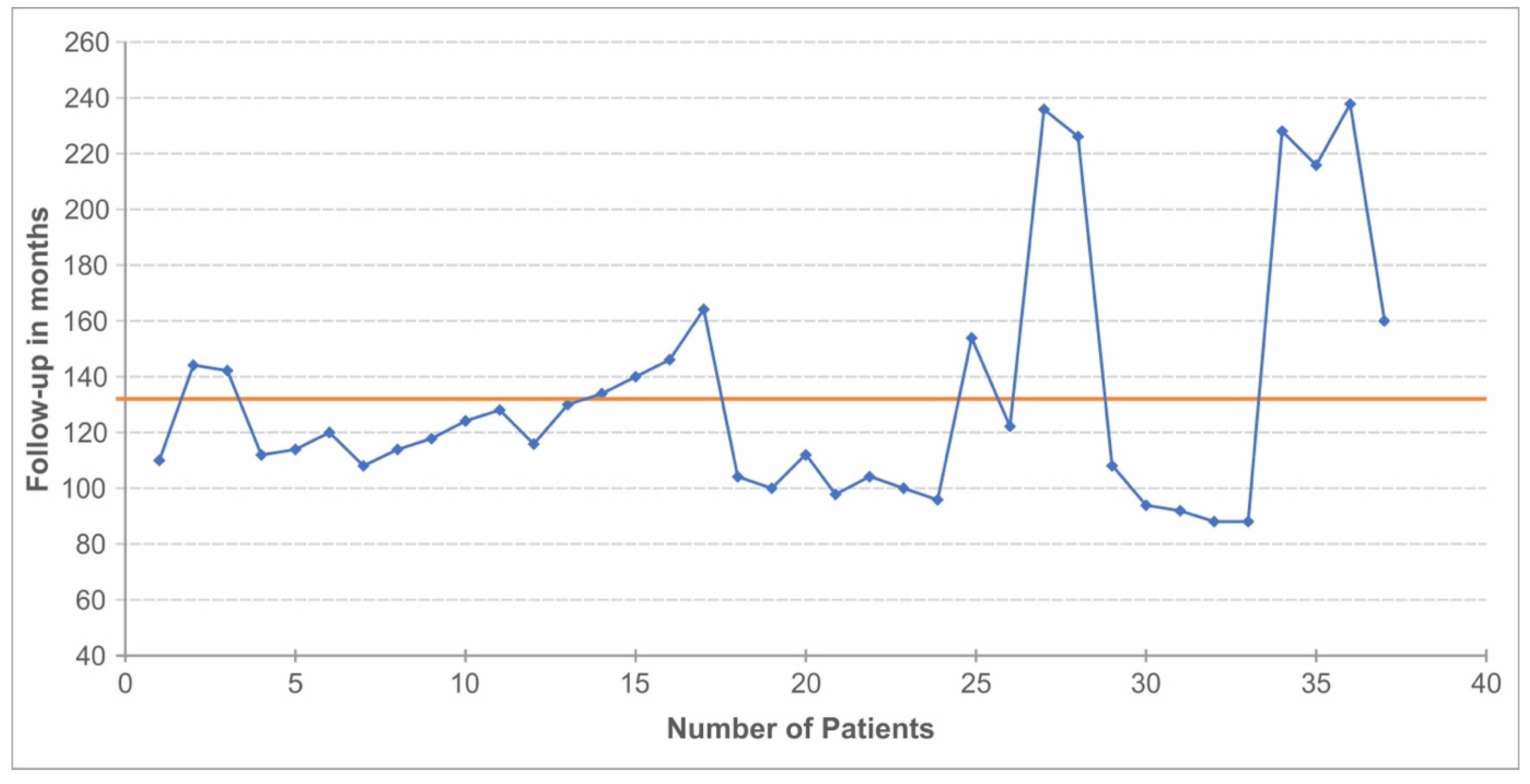
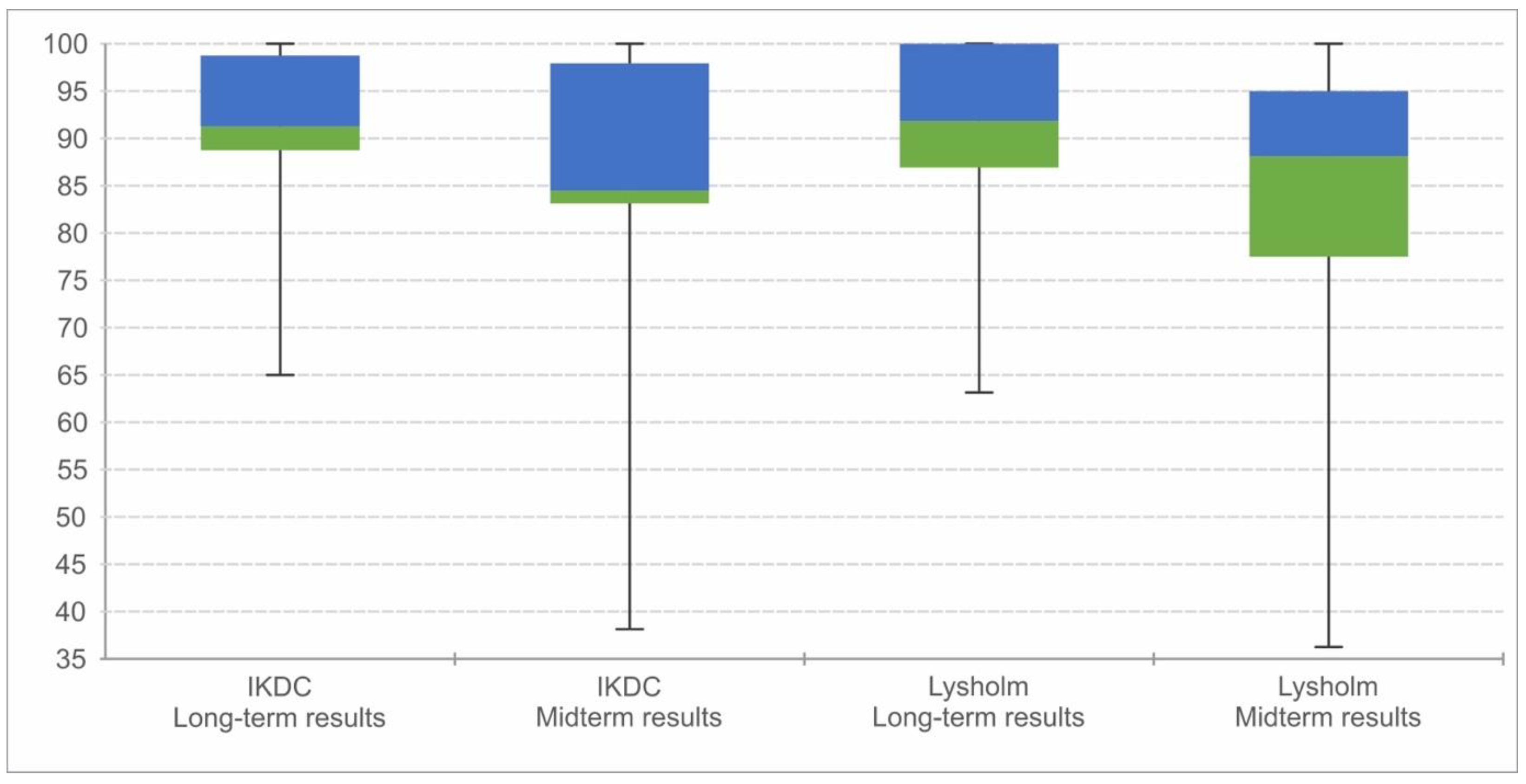
2.4. Statistical Analysis and Comparison with Midterm Data
3. Results
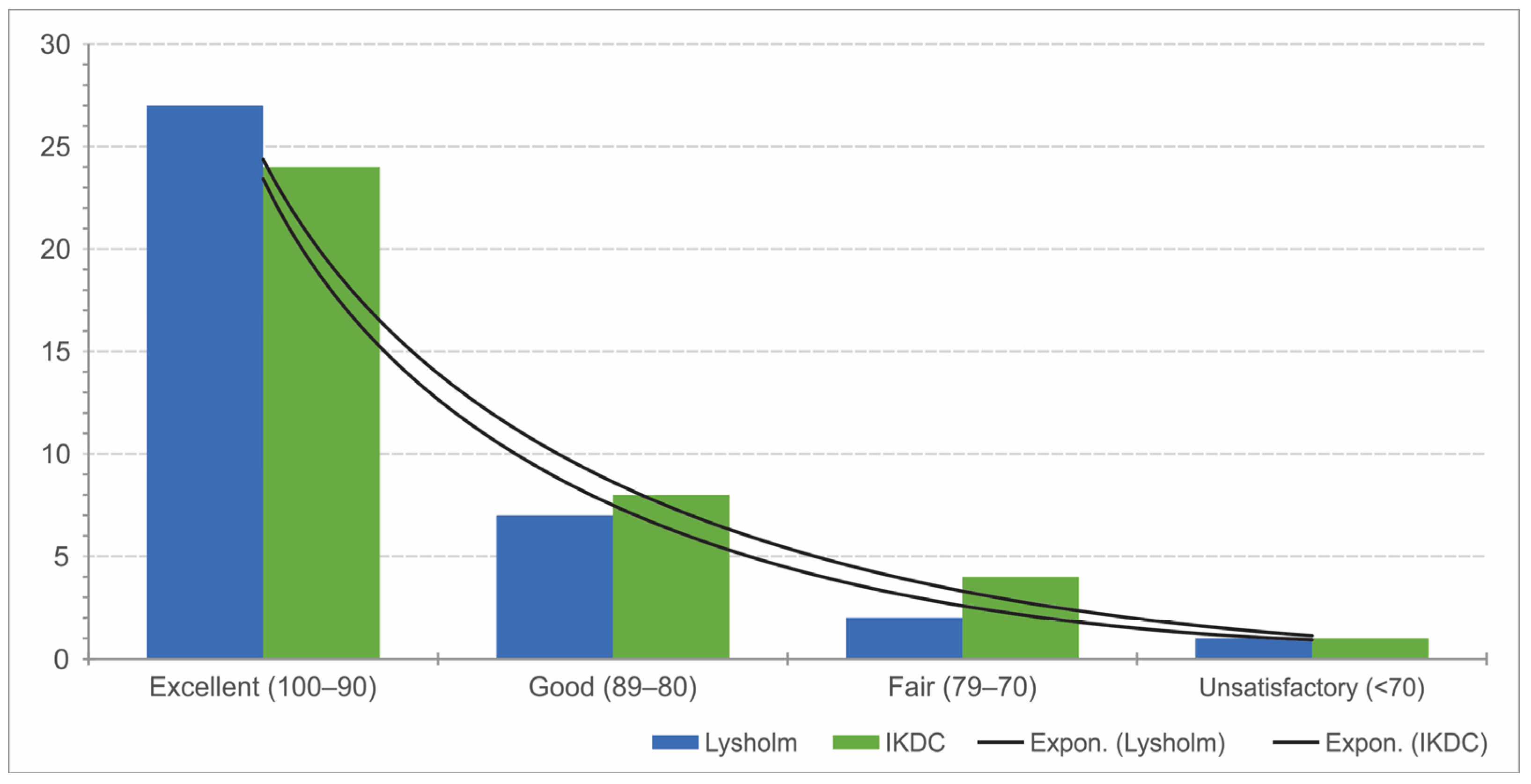
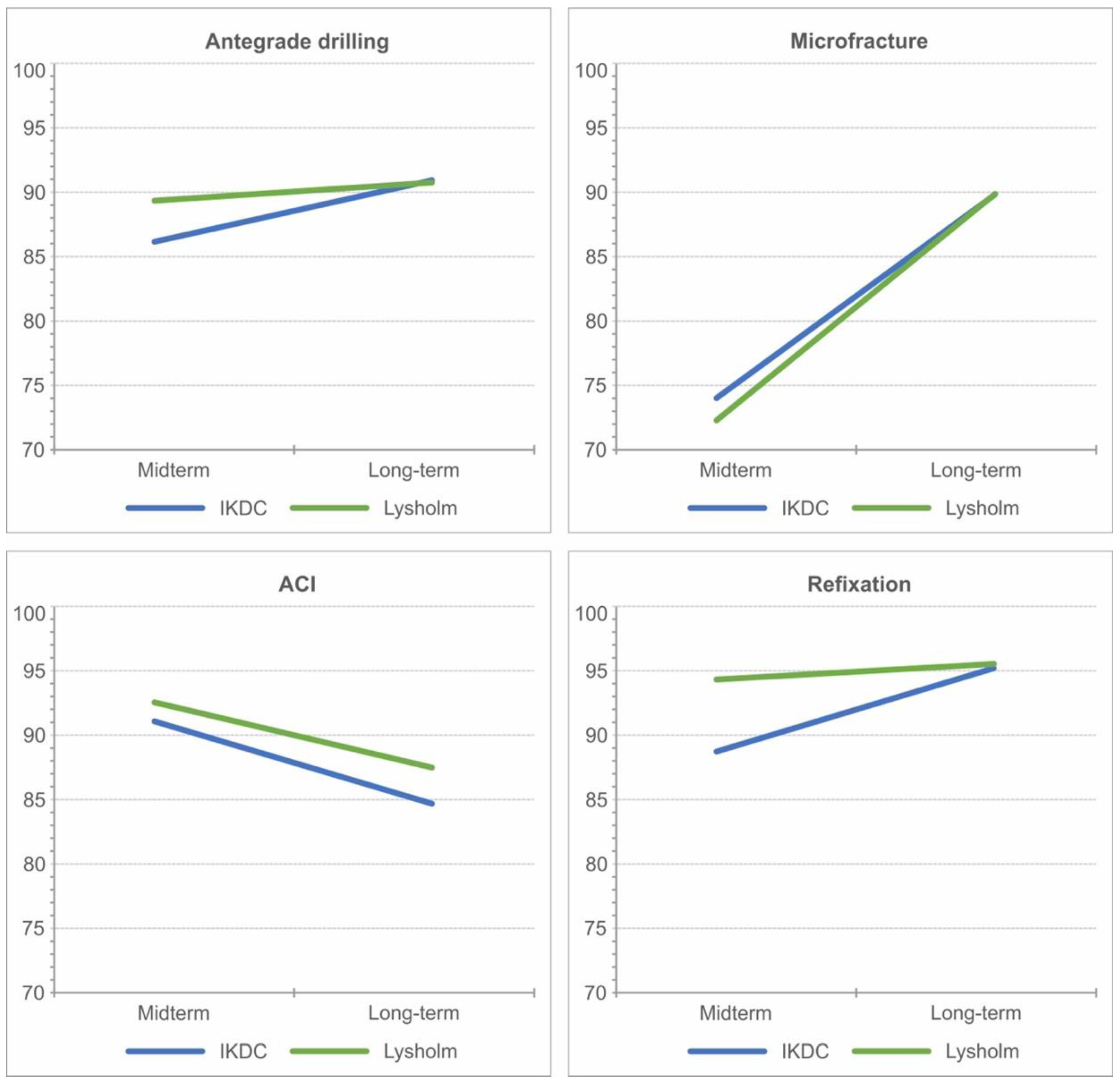
3.1. Subjective Scores of Knee Function
3.2. Results for OCDO and CODC
3.3. Results of Defect Size, Depth, and Localization
3.4. Results According to BMI
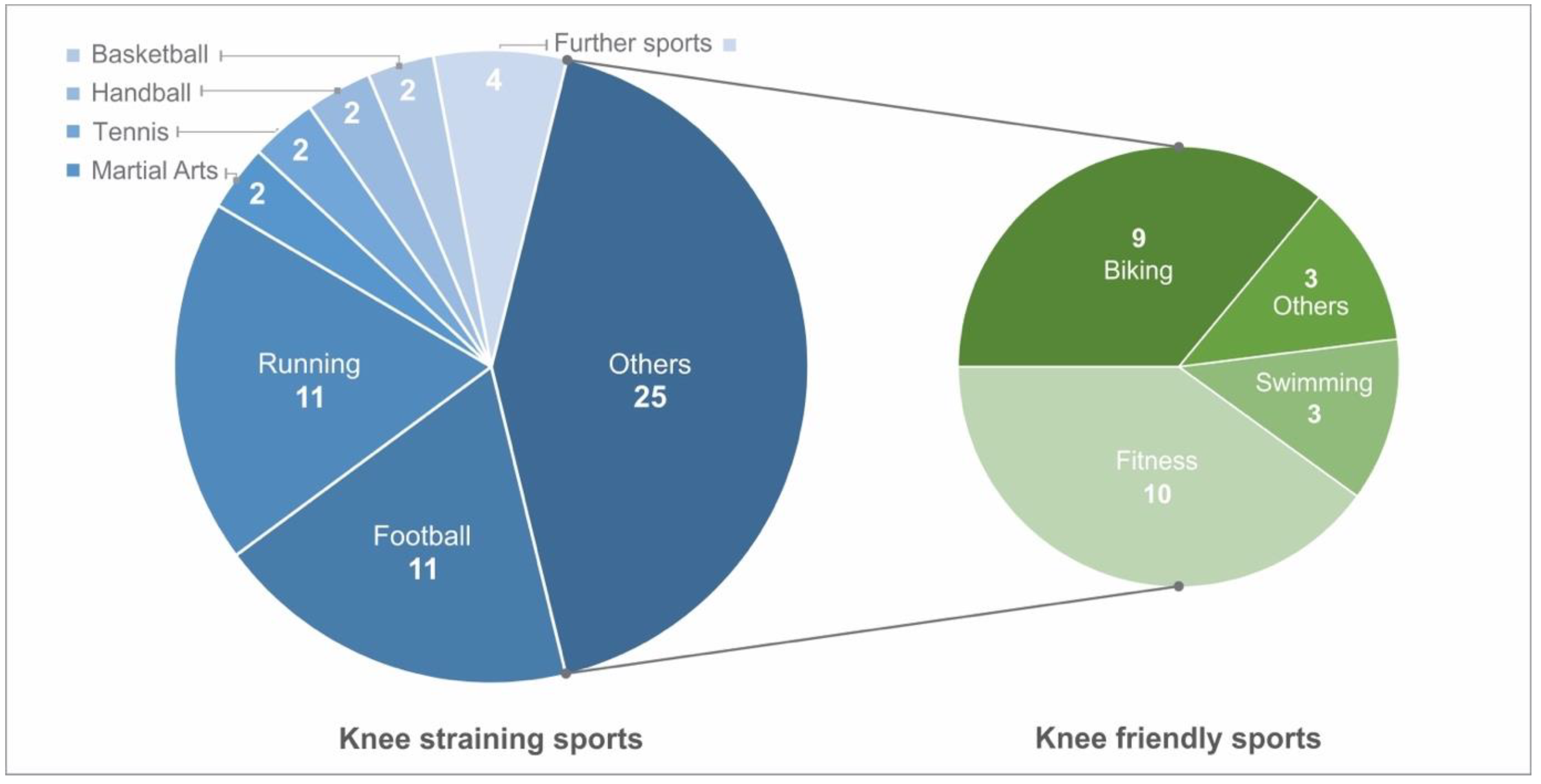
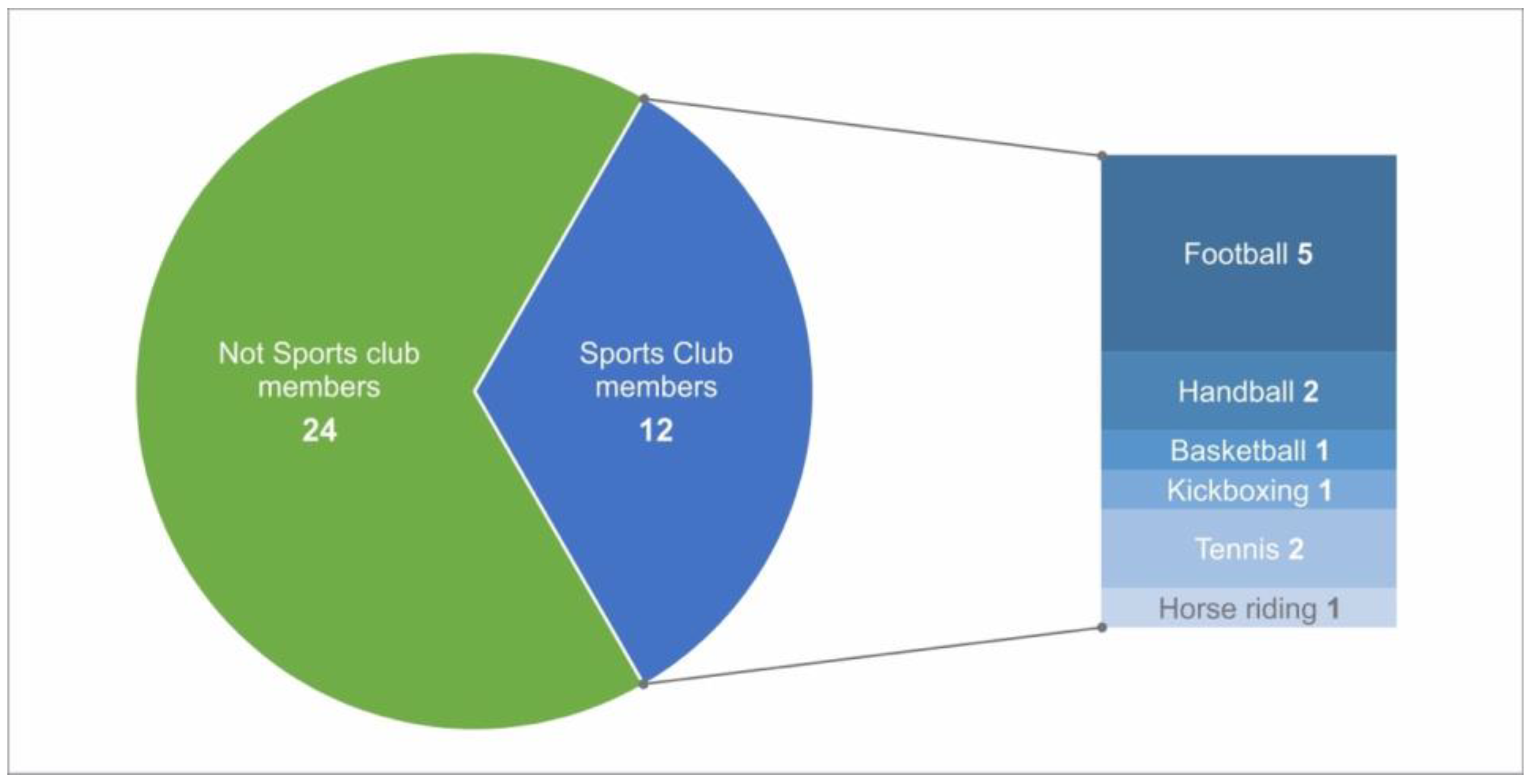
3.5. Sports
3.6. Results According to Surgical Intervention and after Revisions
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OCD | Osteochondrosis dissecans |
| OCDO | Osteochondritis dissecans with open physes |
| OCDC | Osteochondritis dissecans with closed physes |
| MFC | Medial femoral condyle |
| OATS | Osteochondral autograft transfer system |
| AD | Antegrade drilling |
| MF | Microfracture |
| MRI | Magnetic resonance imaging |
| ACI | Autologous chondrocyte implantation |
| TKA | Total knee arthroplasty |
References
- Bruns, J.; Werner, M.; Habermann, C. Osteochondritis Dissecans: Etiology, Pathology, and Imaging with a Special Focus on the Knee Joint. Cartilage 2018, 9, 346–362. [Google Scholar] [CrossRef] [PubMed]
- König, F. The Classic: On loose bodies in the joint. 1887. Clin. Orthop. Relat. Res. 2013, 471, 1107–1115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heyworth, B.E.; Kocher, M.S. Osteochondritis Dissecans of the Knee. JBJS Rev. 2015, 3, e1. [Google Scholar] [CrossRef]
- Kessler, J.I.; Nikizad, H.; Shea, K.G.; Jacobs, J.C.; Bebchuk, J.D.; Weiss, J.M. The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am. J. Sports Med. 2014, 42, 320–326. [Google Scholar] [CrossRef]
- Nissen, C.W.; Albright, J.C.; Anderson, C.N.; Busch, M.T.; Carlson, C.; Carsen, S.; Chambers, H.G.; Edmonds, E.W.; Ellermann, J.M.; Ellis, J.H.B.; et al. Descriptive Epidemiology From the Research in Osteochondritis Dissecans of the Knee (ROCK) Prospective Cohort. Am. J. Sports Med. 2022, 50, 118–127. [Google Scholar] [CrossRef]
- Turati, M.; Anghilieri, F.M.; Bigoni, M.; Rigamonti, L.; Tercier, S.; Nicolaou, N.; Accadbled, F. Osteochondritis dissecans of the knee: Epidemiology, etiology, and natural history. J. Child. Orthop. 2023, 17, 40. [Google Scholar] [CrossRef]
- Andriolo, L.; Candrian, C.; Papio, T.; Cavicchioli, A.; Perdisa, F.; Filardo, G. Osteochondritis Dissecans of the Knee—Conservative Treatment Strategies: A Systematic Review. Cartilage 2019, 10, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.L.; McCauley, J.C.; Gracitelli, G.C.; Bugbee, W.D. Osteochondritis Dissecans Lesion Location Is Highly Concordant With Mechanical Axis Deviation. Am. J. Sports Med. 2020, 48, 871–875. [Google Scholar] [CrossRef] [PubMed]
- Deie, M.; Ochi, M.; Sumen, Y.; Kawasaki, K.; Adachi, N.; Yasunaga, Y.; Ishida, O. Relationship between osteochondritis dissecans of the lateral femoral condyle and lateral menisci types. J. Pediatr. Orthop. 2006, 26, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Cruz, A.I.; Shea, K.G.; Ganley, T.J. Pediatric Knee Osteochondritis Dissecans Lesions. Orthop. Clin. North Am. 2016, 47, 763–775. [Google Scholar] [CrossRef]
- Kocher, M.S.; Tucker, R.; Ganley, T.J.; Flynn, J.M. Management of Osteochondritis Dissecans of the Knee. Am. J. Sports Med. 2006, 34, 1181–1191. [Google Scholar] [CrossRef] [PubMed]
- Gomoll, A.H.; Flik, K.R.; Hayden, J.K.; Cole, B.J.; Bush-Joseph, C.A.; Bach, B.R. Internal fixation of unstable Cahill Type-2C osteochondritis dissecans lesions of the knee in adolescent patients. Orthopedics 2007, 30, 487–490. [Google Scholar]
- Accadbled, F.; Vial, J.; Sales de Gauzy, J. Osteochondritis dissecans of the knee. Orthop. Traumatol. Surg. Res. 2018, 104, S97–S105. [Google Scholar] [CrossRef]
- Wall, E.J.; Polousky, J.D.; Shea, K.G.; Carey, J.L.; Ganley, T.J.; Grimm, N.L.; Jacobs, J.C.; Edmonds, E.W.; Eismann, E.A.; Anderson, A.F.; et al. Novel radiographic feature classification of knee osteochondritis dissecans: A multicenter reliability study. Am. J. Sport. Med. 2015, 43, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Chau, M.M.; Tompkins, M.A. Osteochondritis Dissecans of the Knee in Young Athletes. Clin. Sports Med. 2022, 41, 579–594. [Google Scholar] [CrossRef]
- Weiss, J.M.; Shea, K.G.; Jacobs, J.C.; Cannamela, P.C.; Becker, I.; Portman, M.; Kessler, J.I. Incidence of Osteochondritis Dissecans in Adults. Am. J. Sports Med. 2018, 46, 1592–1595. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.H.; Williams, A.M. Osteochondritis dissecans of the knee: A practical guide for surgeons. Bone Jt. J. 2016, 98-B, 723–729. [Google Scholar] [CrossRef]
- Chau, M.M.; Klimstra, M.A.; Wise, K.L.; Ellermann, J.M.; Tóth, F.; Carlson, C.S.; Nelson, B.J.; Tompkins, M.A. Osteochondritis Dissecans: Current Understanding of Epidemiology, Etiology, Management, and Outcomes. J Bone Jt. Surg. Am. 2021, 103, 1132. [Google Scholar] [CrossRef]
- Michael, J.W.P.; Wurth, A.; Eysel, P.; König, D.P. Long-term results after operative treatment of osteochondritis dissecans of the knee joint—30 year results. Int. Orthop. 2008, 32, 217. [Google Scholar] [CrossRef] [Green Version]
- Cahill, B.R.; Berg, B.C. 99m-Technetium phosphate compound joint scintigraphy in the management of juvenile osteochondritis dissecans of the femoral condyles. Am. J. Sport. Med. 1983, 11, 329–335. [Google Scholar] [CrossRef]
- Langley, G.B.; Sheppeard, H.; RheumdoLng, Y. Clinical and Experimental Investigations The visual analogue scale: Its use in pain measurement. Rheumatol. Int. 1985, 5, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Higgins, L.D.; Taylor, M.K.; Park, D.; Ghodadra, N.; Marchant, M.; Pietrobon, R.; Cook, C. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Jt. Bone Spine 2007, 74, 594–599. [Google Scholar] [CrossRef] [PubMed]
- Lysholm, J.; Gillquist, J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am. J. Sports Med. 1982, 10, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Vannini, F.; Spalding, T.; Andriolo, L.; Berruto, M.; Denti, M.; Espregueira-Mendes, J.; Menetrey, J.; Peretti, G.; Seil, R.; Filardo, G. Sport and early osteoarthritis: The role of sport in aetiology, progression and treatment of knee osteoarthritis. Knee Surg. Sport. Traumatol. Arthrosc. 2016, 24, 1786–1796. [Google Scholar] [CrossRef]
- John, R.; Dhillon, M.S.; Syam, K.; Prabhakar, S.; Behera, P.; Singh, H. Epidemiological profile of sports-related knee injuries in northern India: An observational study at a tertiary care centre. J. Clin. Orthop. Trauma 2016, 7, 207–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hefti, F.; Beguiristain, J.; Krauspe, R.; Möller-Madsen, B.; Riccio, V.; Tschauner, C.; Reinhard, W.; Reinhard, Z. Osteochondritis dissecans: A multicenter study of the European Pediatric Orthopedic Society. J. Pediatr. Orthop. B 1999, 8, 231–245. [Google Scholar] [PubMed]
- Bruns, J.; Rayf, M.; Steinhagen, J. Longitudinal long-term results of surgical treatment in patients with osteochondritis dissecans of the femoral condyles. Knee Surg. Sport. Traumatol. Arthrosc. 2008, 16, 436–441. [Google Scholar] [CrossRef]
- Goebel, S.; Steinert, A.; Rucker, A.; Rudert, M.; Barthel, T. Minimal-invasive retrograde Anbohrung der Osteochondrosis dissecans des Femurkondylus mit einem speziellen Zielinstrumentarium. Oper. Orthopädie Traumatol. 2011, 23, 111–120. [Google Scholar] [CrossRef]
- Louisia, S.; Beaufils, P.; Katabi, M.; Robert, H. Transchondral drilling for osteochondritis dissecans of the medial condyle of the knee. Knee Surg. Sport. Traumatol. Arthrosc. 2003, 11, 33–39. [Google Scholar] [CrossRef]
- Husen, M.; Van der Weiden, G.S.; Custers, R.J.H.; Poudel, K.; Stuart, M.J.; Krych, A.J.; Saris, D.B. Internal Fixation of Unstable Osteochondritis Dissecans of the Knee: Long-term Outcomes in Skeletally Immature and Mature Patients. Am. J. Sport. Med. 2023, 51, 1403–1413. [Google Scholar] [CrossRef] [PubMed]
- Komnos, G.; Iosifidis, M.; Papageorgiou, F.; Melas, I.; Metaxiotis, D.; Hantes, M. Juvenile Osteochondritis Dissecans of the Knee Joint: Midterm Clinical and MRI Outcomes of Arthroscopic Retrograde Drilling and Internal Fixation with Bioabsorbable Pins. Cartilage 2021, 13, 1228S. [Google Scholar] [CrossRef]
- Pareek, A.; Sanders, T.L.; Wu, I.T.; Larson, D.R.; Saris, D.B.F.; Krych, A.J. Incidence of symptomatic osteochondritis dissecans lesions of the knee: A population-based study in Olmsted County. Osteoarthr. Cartil. 2017, 25, 1663–1671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shea, K.G.; Jacobs, B.S.J.C., Jr.; Carey, J.L.; Anderson, A.F.; Oxford, J.T.; Jacobs, J.C., Jr. Osteochondritis dissecans knee histology studies have variable findings and theories of etiology. Clin. Orthop. Relat. Res. 2013, 471, 1127–1136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanders, T.L.; Pareek, A.; Obey, M.R.; Johnson, N.R.; Carey, J.L.; Stuart, M.J.; Krych, A.J. High Rate of Osteoarthritis After Osteochondritis Dissecans Fragment Excision Compared With Surgical Restoration at a Mean 16-Year Follow-up. Am. J. Sport. Med. 2017, 45, 1799–1805. [Google Scholar] [CrossRef]
- Zarzycki, W. Evaluation of treatment results for osteochondritis dissecans of the knee joint. Chir. Narz. Ruch. Ortop. Pol. 2001, 66, 61–66. [Google Scholar]
- Hevesi, M.; Sanders, T.L.; Pareek, A.; Milbrandt, T.A.; Levy, B.A.; Stuart, M.J.; Saris, D.B.F.; Krych, A.J. Osteochondritis Dissecans in the Knee of Skeletally Immature Patients: Rates of Persistent Pain, Osteoarthritis, and Arthroplasty at Mean 14-Years’ Follow-Up. Cartilage 2020, 11, 291–299. [Google Scholar] [CrossRef]
- Carey, J.L.; Shea, K.G.; Lindahl, A.; Vasiliadis, H.S.; Lindahl, C.; Peterson, L. Autologous Chondrocyte Implantation as Treatment for Unsalvageable Osteochondritis Dissecans: 10- to 25-Year Follow-up. Am. J. Sport. Med. 2020, 48, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Krych, A.J.; Harnly, H.W.; Rodeo, S.A.; Williams, R.J. Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: A retrospective comparative study. J. Bone Jt. Surg Am. 2012, 94, 971–978. [Google Scholar] [CrossRef]
- Cole, B.J.; Deberardino, T.; Brewster, R.; Farr, J.; Levine, D.W.; Nissen, C.; Roaf, P.; Zaslav, K. Outcomes of autologous chondrocyte implantation in study of the treatment of articular repair (STAR) patients with osteochondritis dissecans. Am. J. Sports Med. 2012, 40, 2015–2022. [Google Scholar] [CrossRef]
- Dhillon, J.; Decilveo, A.P.; Kraeutler, M.J.; Belk, J.W.; McCulloch, P.C.; Scillia, A.J. Third-Generation Autologous Chondrocyte Implantation (Cells Cultured Within Collagen Membrane) Is Superior to Microfracture for Focal Chondral Defects of the Knee Joint: Systematic Review and Meta-analysis. Arthrosc. J. Arthrosc. Relat. Surg. 2022, 38, 2579–2586. [Google Scholar] [CrossRef]


| N | Mean | SD | Minimum | Maximum | p-Value | ||
|---|---|---|---|---|---|---|---|
| Localisation | Typical | 24 | 92.6 | 9.8 | 64.7 | 100 | 0.283 |
| IKDC | Atypical | 13 | 89.1 | 6.2 | 78.2 | 100 | |
| Localisation | Typical | 24 | 93.3 | 9.6 | 63.0 | 100 | 0.251 |
| Lysholm | Atypical | 13 | 89.4 | 7.5 | 75.0 | 100 | |
| Defect size | <4 cm2 | 21 | 90.6 | 9.7 | 64.7 | 100 | 0.92 |
| IKDC | ≥4 cm2 | 9 | 92.4 | 8.9 | 73.6 | 100 | |
| Defect size | <4 cm2 | 21 | 91.5 | 10.5 | 63.0 | 100 | 0.71 |
| Lysholm | ≥4 cm2 | 9 | 92.6 | 8.3 | 80.0 | 100 | |
| Defect depth | <0.8 cm2 | 15 | 94.5 | 5.8 | 79.3 | 100 | 0.023 * |
| IKDC | ≥0.8 cm2 | 14 | 87.1 | 11.1 | 64.7 | 100 | |
| Defect depth | <0.8 cm2 | 15 | 95.5 | 5.3 | 83.0 | 100 | 0.015 * |
| Lysholm | ≥0.8 cm2 | 14 | 87.2 | 11.8 | 63.0 | 100 |
| Surgical Method | N | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Antegrade drilling | 10 | ||||
| IKDC | 91.3 | 10.3 | 65 | 100 | |
| Lysholm | 91 | 10.8 | 63 | 100 | |
| Microfracture | 8 | ||||
| IKDC | 89.4 | 11.5 | 73 | 100 | |
| Lysholm | 89.4 | 12.4 | 70 | 100 | |
| ACI | 6 | ||||
| IKDC | 85.2 | 8.3 | 74 | 97 | |
| Lysholm | 87.3 | 8.2 | 81 | 100 | |
| Refixation | 9 | ||||
| IKDC | 94.8 | 4.1 | 87 | 100 | |
| Lysholm | 95.7 | 3.2 | 93 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bangert, Y.; Zarembowicz, P.; Engelleiter, K.; Gkarilas, E.; Schmitt, H.; Renkawitz, T.; Jaber, A. Long-Term Outcome and Athletic Level following Operative Treatment for Osteochondritis Dissecans of the Knee in Pediatric and Adolescent Patients. J. Clin. Med. 2023, 12, 4140. https://doi.org/10.3390/jcm12124140
Bangert Y, Zarembowicz P, Engelleiter K, Gkarilas E, Schmitt H, Renkawitz T, Jaber A. Long-Term Outcome and Athletic Level following Operative Treatment for Osteochondritis Dissecans of the Knee in Pediatric and Adolescent Patients. Journal of Clinical Medicine. 2023; 12(12):4140. https://doi.org/10.3390/jcm12124140
Chicago/Turabian StyleBangert, Yannic, Patrick Zarembowicz, Karoly Engelleiter, Evangelos Gkarilas, Holger Schmitt, Tobias Renkawitz, and Ayham Jaber. 2023. "Long-Term Outcome and Athletic Level following Operative Treatment for Osteochondritis Dissecans of the Knee in Pediatric and Adolescent Patients" Journal of Clinical Medicine 12, no. 12: 4140. https://doi.org/10.3390/jcm12124140
APA StyleBangert, Y., Zarembowicz, P., Engelleiter, K., Gkarilas, E., Schmitt, H., Renkawitz, T., & Jaber, A. (2023). Long-Term Outcome and Athletic Level following Operative Treatment for Osteochondritis Dissecans of the Knee in Pediatric and Adolescent Patients. Journal of Clinical Medicine, 12(12), 4140. https://doi.org/10.3390/jcm12124140




