A Peculiar CLL Case with Complex Chromosome 6 Rearrangements and Refinement of All Breakpoints at the Gene Level by Genomic Array: A Case Report
Abstract
:1. Introduction
2. Case Presentation
3. Genetic Investigations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Albiol, N.; Moreno, C. Autoimmune Cytopenia in CLL: Prognosis and Management in the Era of Targeted Therapies. Cancer J. 2021, 27, 286–296. [Google Scholar] [CrossRef]
- Vitale, C.; Montalbano, M.C.; Salvetti, C.; Boccellato, E.; Griggio, V.; Boccadoro, M.; Coscia, M. Autoimmune Complications in Chronic Lymphocytic Leukemia in the Era of Targeted Drugs. Cancers 2020, 12, 282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Autore, F.; Pasquale, R.; Innocenti, I.; Fresa, A.; Sora, F.; Laurenti, L. Autoimmune Hemolytic Anemia in Chronic Lymphocytic Leukemia: A Comprehensive Review. Cancers 2021, 13, 5804. [Google Scholar] [CrossRef]
- Hallek, M. Chronic lymphocytic leukemia: 2013 update on diagnosis, risk stratification and treatment. Am. J. Hematol. 2013, 88, 803–816. [Google Scholar] [CrossRef]
- Dameshek, W. Chronic lymphocytic leukemia—An accumulative disease of immunolgically incompetent lymphocytes. Blood 1967, 29, 566–584. [Google Scholar] [CrossRef] [Green Version]
- Hodgson, K.; Ferrer, G.; Montserrat, E.; Moreno, C. Chronic lymphocytic leukemia and autoimmunity: A systematic review. Haematologica 2011, 96, 752–761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiorazzi, N.; Rai, K.R.; Ferrarini, M. Chronic lymphocytic leukemia. N. Engl. J. Med. 2005, 352, 804–815. [Google Scholar] [CrossRef] [Green Version]
- Strati, P.; Caligaris-Cappio, F. A matter of debate in chronic lymphocytic leukemia: Is the occurrence of autoimmune disorders an indicator of chronic lymphocytic leukemia therapy? Curr. Opin. Oncol. 2011, 23, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Jachiet, V.; Mekinian, A.; Carrat, F.; Grignano, E.; Retbi, A.; Boffa, J.-J.; Ronco, P.; Rondeau, E.; Sellam, J.; Berenbaum, F.; et al. Autoimmune manifestations associated with lymphoma: Characteristics and outcome in a multicenter retrospective cohort study. Leuk. Lymphoma 2018, 59, 1399–1405. [Google Scholar] [CrossRef]
- Mauro, F.R.; Foa, R.; Cerretti, R.; Giannarelli, D.; Coluzzi, S.; Mandelli, F.; Girelli, G. Autoimmune hemolytic anemia in chronic lymphocytic leukemia: Clinical, therapeutic, and prognostic features. Blood 2000, 95, 2786–2792. [Google Scholar] [CrossRef]
- Zent, C.S.; Ding, W.; Schwager, S.M.; Reinalda, M.S.; Hoyer, J.D.; Jelinek, D.F.; Tschumper, R.C.; Bowen, D.A.; Call, T.G.; Shanafelt, T.D.; et al. The prognostic significance of cytopenia in chronic lymphocyti leukaemia/small lymphocytic lymphoma. Br. J. Haematol. 2008, 141, 615–621. [Google Scholar] [CrossRef] [Green Version]
- Zent, C.S.; Ding, W.; Reinalda, M.S.; Schwager, S.M.; Hoyer, J.D.; Bowen, D.A.; Jelinek, D.F.; Tschumper, R.C.; Call, T.G.; Shanafelt, T.D.; et al. Autoimmune cytopenia in chronic lymphocytic leukemia/small lymphocytic lymphoma: Changes in clinical presentation and prognosis. Leuk. Lymphoma 2009, 50, 1261–1268. [Google Scholar] [CrossRef]
- Moreno, C.; Hodgson, K.; Ferrer, G.; Elena, M.; Filella, X.; Pereira, A.; Baumann, T.; Montserrat, E. Autoimmune cytopenia in chronic lymphocytic leukemia: Prevalence, clinical associations, and prognostic significance. Blood 2010, 116, 4771–4776. [Google Scholar] [CrossRef] [PubMed]
- Diehl, L.F.; Ketchum, L.H. Autoimmune disease and chronic lymphocytic leukemia: Autoimmune hemolytic anemia, pure red cell aplasia, and autoimmune thrombocytopenia. Semin. Oncol. 1998, 25, 80–97. [Google Scholar] [PubMed]
- Galton, D.A. The pathogenesis of chronic lymphocytic leukemia. Can. Med. Assoc. J. 1966, 94, 1005–1010. [Google Scholar]
- Barcellini, W.; Giannotta, J.A.; Fattizzo, B. Autoimmune Complications in Hematologic Neoplasms. Cancers 2021, 13, 1532. [Google Scholar] [CrossRef] [PubMed]
- Hill, Q.A.; Hill, A.; Berentsen, S. Defining autoimmune hemolytic anemia: A systematic review of the terminology used for diagnosis and treatment. Blood Adv. 2019, 3, 1897–1906. [Google Scholar] [CrossRef] [Green Version]
- Carli, G.; Visco, C.; Falisi, E.; Perbellini, O.; Novella, E.; Giaretta, I.; Ferrarini, I.; Sandini, A.; Alghisi, A.; Ambrosetti, A.; et al. Evans syndrome secondary to chronic lymphocytic leukaemia: Presentation, treatment, and outcome. Ann. Hematol. 2016, 95, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Maura, F.; Visco, C.; Falisi, E.; Reda, G.; Fabris, S.; Agnelli, L.; Tuana, G.; Lionetti, M.; Guercini, N.; Novella, E.; et al. B-cell receptor configuration and adverse cytogenetics are associated with autoimmune hemolytic anemia in chronic lymphocytic leukemia. Am. J. Hematol. 2013, 88, 32–36. [Google Scholar] [CrossRef]
- Vitale, C.; Salvetti, C.; Griggio, V.; Porrazzo, M.; Schiattone, L.; Zamprogna, G.; Visentin, A.; Vassallo, F.; Cassin, R.; Rigolin, G.M.; et al. Preexisting and treatment-emergent autoimmune cytopenias in patients with CLL treated with targeted drugs. Blood 2021, 137, 3507–3517. [Google Scholar] [CrossRef]
- Demir, C.; Ekinci, O. Clinical and serological autoimmune complications in chronic lymphocytic leukemia. Wien. Klin. Wochenschr. 2017, 129, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Atef, B.; Azmy, E.; Aladle, D.; Mabed, M. The prevalence and prognostic significance of autoimmune cytopenias in a cohort of Egyptian patients with chronic lymphocytic leukemia. Hematol. Oncol. Stem Cell Ther. 2019, 12, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Michalak, S.S.; Olewicz-Gawlik, A.; Rupa-Matysek, J.; Wolny-Rokicka, E.; Nowakowska, E.; Gil, L. Autoimmune hemolytic anemia: Current knowledge and perspectives. Immun. Ageing 2020, 17, 38. [Google Scholar] [CrossRef] [PubMed]
- Hill, Q.A.; Stamps, R.; Massey, E.; Grainger, J.D.; Provan, D.; Hill, A.; Haematology, T.B.S.F. The diagnosis and management of primary autoimmune haemolytic anaemia. Br. J. Haematol. 2017, 176, 395–411. [Google Scholar] [CrossRef] [PubMed]
- Barcellini, W.; Fattizzo, B. How I treat warm autoimmune hemolytic anemia. Blood 2021, 137, 1283–1294. [Google Scholar] [CrossRef]
- Berentsen, S. How I manage patients with cold agglutinin disease. Br. J. Haematol. 2018, 181, 320–330. [Google Scholar] [CrossRef] [Green Version]
- Go, R.S.; Winters, J.L.; Kay, N.E. How I treat autoimmune hemolytic anemia. Blood 2017, 129, 2971–2979. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dearden, C.; Wade, R.; Else, M.; Richards, S.; Milligan, D.; Hamblin, T.; Catovsky, D.; for the UK National Cancer Research Institute (NCRI) Haematological Oncology Clinical Studies Group and NCRI CLL Working Group. The prognostic significance of a positive direct antiglobulin test in chronic lymphocytic leukemia: A beneficial effect of the combination of fludarabine and cyclophosphamide on the incidence of hemolytic anemia. Blood 2008, 111, 1820–1826. [Google Scholar] [CrossRef] [Green Version]
- De Back, T.R.; Kater, A.; Tonino, S.H. Autoimmune cytopenias in chronic lymphocytic leukemia: A concise review and treatment recommendations. Expert. Rev. Hematol. 2018, 11, 613–624. [Google Scholar] [CrossRef]
- Barcellini, W.; Fattizzo, B.; Zaninoni, A.; Radice, T.; Nichele, I.; Di Bona, E.; Lunghi, M.; Tassinari, C.; Alfinito, F.; Ferrari, A.; et al. Clinical heterogeneity and predictors of outcome in primary autoimmune hemolytic anemia: A GIMEMA study of 308 patients. Blood 2014, 124, 2930–2936. [Google Scholar] [CrossRef]
- Fattizzo, B.; Barcellini, W. Autoimmune Cytopenias in Chronic Lymphocytic Leukemia: Focus on Molecular Aspects. Front. Oncol. 2019, 9, 1435. [Google Scholar] [CrossRef] [PubMed]
- Jager, U.; Barcellini, W.; Broome, C.M.; Gertz, M.A.; Hill, A.; Hill, Q.A.; Jilma, B.; Kuter, D.J.; Michel, M.; Montillo, M.; et al. Diagnosis and treatment of autoimmune hemolytic anemia in adults: Recommendations from the First International Consensus Meeting. Blood Rev. 2020, 41, 100648. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo, C.; Rajapakse, S.; Gooneratne, L. Rituximab in the treatment of autoimmune haemolytic anaemia. Br. J. Clin. Pharm. 2015, 79, 709–719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birgens, H.; Frederiksen, H.; Hasselbalch, H.C.; Rasmussen, I.H.; Nielsen, O.J.; Kjeldsen, L.; Larsen, H.; Mourits-Andersen, T.; Plesner, T.; Rønnov-Jessen, D.; et al. A phase III randomized trial comparing glucocorticoid monotherapy versus glucocorticoid and rituximab in patients with autoimmune haemolytic anaemia. Br. J. Haematol. 2013, 163, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Michel, M.; Terriou, L.; Roudot-Thoraval, F.; Hamidou, M.; Ebbo, M.; Le Guenno, G.; Galicier, L.; Audia, S.; Royer, B.; Morin, A.-S.; et al. A randomized and double-blind controlled trial evaluating the safety and efficacy of rituximab for warm auto-immune hemolytic anemia in adults (the RAIHA study). Am. J. Hematol. 2017, 92, 23–27. [Google Scholar] [CrossRef]
- D’Arena, G.; Laurenti, L.; Capalbo, S.; D’Arco, A.M.; De Filippi, R.; Marcacci, G.; Di Renzo, N.; Storti, S.; Califano, C.; Vigliotti, M.L.; et al. Rituximab therapy for chronic lymphocytic leukemia-associated autoimmune hemolytic anemia. Am. J. Hematol. 2006, 81, 598–602. [Google Scholar] [CrossRef]
- Nikitin, E.; Kislova, M.; Morozov, D.; Belyakova, V.; Suvorova, A.; Sveshnikova, J.; Vyscub, G.; Matveeva, I.; Shirokova, M.; Shipaeva, A.; et al. Ibrutinib in combination with rituximab is highly effective in treatment of chronic lymphocytic leukemia patients with steroid refractory and relapsed autoimmune cytopenias. Leukemia 2023, 1–10. [Google Scholar] [CrossRef]
- Rack, K.A.; Van Den Berg, E.; Haferlach, C.; Beverloo, H.B.; Costa, D.; Espinet, B.; Foot, N.; Jeffries, S.; Martin, K.; O’Connor, S.; et al. European recommendations and quality assurance for cytogenomic analysis of haematological neoplasms. Leukemia 2019, 33, 1851–1867. [Google Scholar] [CrossRef]
- Rack, K.A.; Berg, E.V.D.; Haferlach, C.; Beverloo, H.B.; Costa, D.; Espinet, B.; Foot, N.; Jeffries, S.; Martin, K.; O’connor, S.; et al. European recommendations and quality assurance for cytogenomic analysis of haematological neoplasms: Reponse to the comments from the Francophone Group of Hematological Cytogenetics (GFCH). Leukemia 2020, 34, 2262–2264. [Google Scholar] [CrossRef] [Green Version]
- Pellestor, F.; Gaillard, J.B.; Schneider, A.; Puechberty, J.; Gatinois, V. Chromoanagenesis, the mechanisms of a genomic chaos. Semin. Cell Dev. Biol. 2022, 123, 90–99. [Google Scholar] [CrossRef]
- Zhang, C.Z.; Leibowitz, M.L.; Pellman, D. Chromothripsis and beyond: Rapid genome evolution from complex chromosomal rearrangements. Genes. Dev. 2013, 27, 2513–2530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, M.M. Chromoplexy: A new category of complex rearrangements in the cancer genome. Cancer Cell 2013, 23, 567–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, D.; Granada, I.; Espinet, B.; Collado, R.; Ruiz-Xivillé, N.; Puiggros, A.; Uribe, M.; Arias, A.; Gómez, C.; Delgado, J.; et al. Balanced and unbalanced translocations in a multicentric series of 2843 patients with chronic lymphocytic leukemia. Genes Chromosom. Cancer 2022, 61, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Gozzetti, A.; Calabrese, S.; Crupi, R.; Zaja, F.; Tozzuoli, D.; Tassi, M.; Raspadori, D.; Lenoci, M.; Lauria, F. Trisomy 8 in chronic lymphocytic leukemia: A report of two cases. Cancer Genet. Cytogenet. 2007, 175, 175–176. [Google Scholar] [CrossRef] [PubMed]
- Edelmann, J.; Holzmann, K.; Miller, F.; Winkler, D.; Bühler, A.; Zenz, T.; Bullinger, L.; Kühn, M.W.M.; Gerhardinger, A.; Bloehdorn, J.; et al. High-resolution genomic profiling of chronic lymphocytic leukemia reveals new recurrent genomic alterations. Blood 2012, 120, 4783–4794. [Google Scholar] [CrossRef] [Green Version]
- Gunnarsson, R.; Mansouri, L.; Isaksson, A.; Göransson, H.; Cahill, N.; Jansson, M.; Rasmussen, M.; Lundin, J.; Norin, S.; Buhl, A.M.; et al. Array-based genomic screening at diagnosis and during follow-up in chronic lymphocytic leukemia. Haematologica 2011, 96, 1161–1169. [Google Scholar] [CrossRef] [Green Version]
- Urbankova, H.; Papajik, T.; Plachy, R.; Holzerova, M.; Balcarkova, J.; Divoka, M.; Prochazka, V.; Pikalova, Z.; Indrak, K.; Jarosova, M. Array-based karyotyping in chronic lymphocytic leukemia (CLL) detects new unbalanced abnormalities that escape conventional cytogenetics and CLL FISH panel. Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc Czech Repub. 2014, 158, 56–64. [Google Scholar] [CrossRef] [Green Version]
- Tausch, E.; Schneider, C.; Robrecht, S.; Zhang, C.; Dolnik, A.; Bloehdorn, J.; Bahlo, J.; Al-Sawaf, O.; Ritgen, M.; Fink, A.-M.; et al. Prognostic and predictive impact of genetic markers in patients with CLL treated with obinutuzumab and venetoclax. Blood 2020, 135, 2402–2412. [Google Scholar] [CrossRef]
- Schweighofer, C.D.; Coombes, K.R.; Majewski, T.; Barron, L.L.; Lerner, S.; Sargent, R.L.; O’Brien, S.; Ferrajoli, A.; Wierda, W.G.; Czerniak, B.A.; et al. Genomic variation by whole-genome SNP mapping arrays predicts time-to-event outcome in patients with chronic lymphocytic leukemia: A comparison of CLL and HapMap genotypes. J. Mol. Diagn. 2013, 15, 196–209. [Google Scholar] [CrossRef] [Green Version]
- Tsimberidou, A.M.; Wen, S.; O’Brien, S.; McLaughlin, P.; Wierda, W.G.; Ferrajoli, A.; Faderl, S.; Manning, J.; Lerner, S.; Mai, C.V.; et al. Assessment of chronic lymphocytic leukemia and small lymphocytic lymphoma by absolute lymphocyte counts in 2126 patients: 20 years of experience at the University of Texas M.D. Anderson Cancer Center. J. Clin. Oncol. 2007, 25, 4648–4656. [Google Scholar] [CrossRef] [Green Version]
- Jarosova, M.; Hruba, M.; Oltova, A.; Plevova, K.; Kruzova, L.; Kriegova, E.; Fillerova, R.; Koritakova, E.; Doubek, M.; Lysak, D.; et al. Chromosome 6q deletion correlates with poor prognosis and low relative expression of FOXO3 in chronic lymphocytic leukemia patients. Am. J. Hematol. 2017, 92, E604–E607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Houldsworth, J.; Guttapalli, A.; Thodima, V.; Yan, X.J.; Mendiratta, G.; Zielonka, T.; Nanjangud, G.; Chen, W.; Patil, S.; Mato, A.; et al. Genomic imbalance defines three prognostic groups for risk stratification of patients with chronic lymphocytic leukemia. Leuk. Lymphoma 2014, 55, 920–928. [Google Scholar] [CrossRef] [PubMed]
- Dalsass, A.; Mestichelli, F.; Ruggieri, M.; Gaspari, P.; Pezzoni, V.; Vagnoni, D.; Angelini, M.; Angelini, S.; Bigazzi, C.; Falcioni, S.; et al. 6q deletion detected by fluorescence in situ hybridization using bacterial artificial chromosome in chronic lymphocytic leukemia. Eur. J. Haematol. 2013, 91, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Gunnarsson, R.; Isaksson, A.; Mansouri, M.; Göransson, H.; Jansson, M.; Cahill, N.; Rasmussen, M.; Staaf, J.; Lundin, J.; Norin, S.; et al. Large but not small copy-number alterations correlate to high-risk genomic aberrations and survival in chronic lymphocytic leukemia: A high-resolution genomic screening of newly diagnosed patients. Leukemia 2010, 24, 211–215. [Google Scholar] [CrossRef]
- Zavacka, K.; Plevova, K. Chromothripsis in Chronic Lymphocytic Leukemia: A Driving Force of Genome Instability. Front. Oncol. 2021, 11, 771664. [Google Scholar] [CrossRef]





| 30 September 2022 | 15 October 2022 | 24 October 2022 | 9 December 2022 | 16–23 December 2022 | 8 March 2022 | Normal Range | SI | |
|---|---|---|---|---|---|---|---|---|
| WBC | 143,960 | 4130 | 4020 | 6770 | 4000–9500 | 109/L | ||
| Hb | 52 | 69 | 91 | 136 | 130–170 | g/L | ||
| MCV | 119.6 | 128.8 | 125.4 | 93.0 | 80.0–95.0 | fL | ||
| PLT | 149,000 | 120,000 | 104,000 | 215,000 | 130,000–400,000 | 109/L | ||
| ANC | 4600 | 1970 | 2400 | 4080 | 109/L | |||
| ALC | 129,320 | 2010 | 1410 | 2220 | 109/L | |||
| AMC | 9480 | 110 | 200 | 430 | 109/L | |||
| HP | <20.00 | 50–150 | mG/dL | |||||
| sCr | 1.10 | 0.86 | 0.94 | <1.25 | mG/dL | |||
| TBILI | 3.70 | 0.50 | 0.20–1.30 | mG/dL | ||||
| IBILI | 3.40 | mG/dL | ||||||
| LDH | 337 | 355 | 120–246 | IU/mL | ||||
| CRP | 5.00 | 5.00 | <10 | mG/L | ||||
| Ret | 142.2 | 109/L | ||||||
| Treatment Administration | Corticosteroid | Rituximab | Rituximab interruption for COVID Positivity (20 October 2022–2 December 2022) | Rituximab | Rituximab | Acalabrutinib |
| Peripheral Blood | Bone Marrow | |
|---|---|---|
| CD5+ | CD5+ | |
| CD20+dim | CD20+ | |
| CD23+ | CD23+ | |
| CD19+ | CD3- | |
| LAMBDA+ | LEF1+ | |
| CYCLIN D1- | ||
| Conclusion | CLL-type mature B-cell lymphoproliferative neoplasia | Medullary localization of CLL |
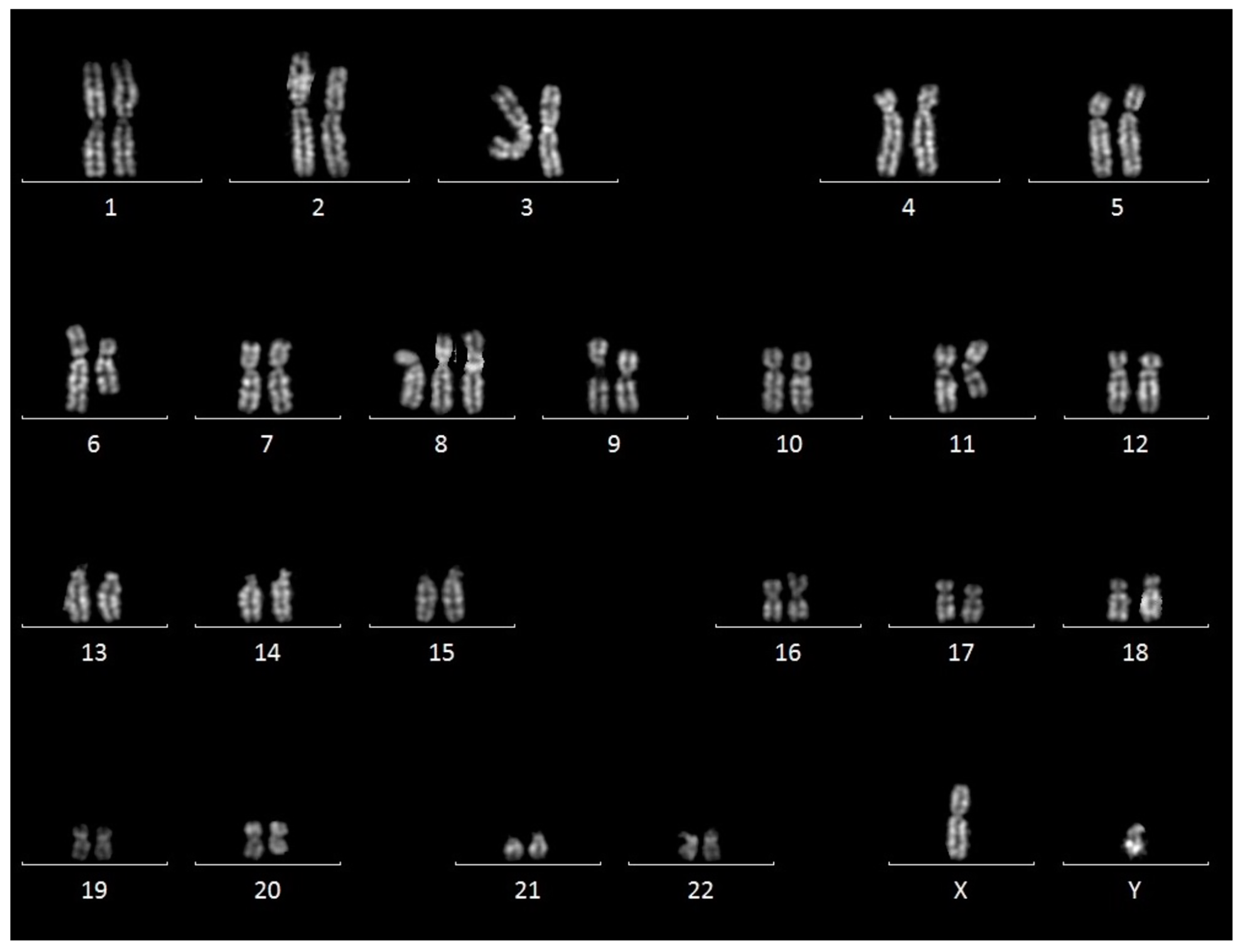
| Karyotyping | 47,XY,+8,der(6)t(6;11)(p12;q24)del(6)(q14q22),der(11)t(6;11)(p12;q24)del(11)(q13q24)[19]/ 46,XY,der(6)t(6;11)(p12;q24)del(6)(q14q22),der(11)t(6;11)(p12;q24)del(11)(q13q24)[1] | |
| FISH | Monoallelic deletion of ATM in 90% of nuclei | |
| Retained signal of TP53, 13q14, centromere 12 | ||
| Sequencing | TP53 and IGHV wild type | |
| Array-CGH result arr[GRCh37] | Copy number variation | Size (Mb) |
| 6p21.1p12.3(42530647_47909775) × 1 | 5.4 Mb | |
| 6p12.3(48415298_48509357) × 1 | 0.1 Mb | |
| 6p12.3(49041219_49391971) × 1 | 0.35 Mb | |
| 6q14.2(84136451_84871569) × 1 | 0.73 Mb | |
| 6q14.3q21(85872402_105528935) × 1 | 19.6 Mb | |
| 6q22.1(114960420_116038498) × 1 | 1 Mb | |
| 6q22.1q22.31(117082970_125486670) × 1 | 8.4 Mb | |
| 6q24.2q25.2(144831439_154339818) × 1 | 9.5 Mb | |
| 6q25.3(155552589_155880666) × 1 | 0.33 Mb | |
| arr[GRCh37] (8) × 3 | arr[GRCh37] (8) × 3 | |
| 11q14.1q14.3(81540019_89188979) × 1 | 7.65 Mb | |
| 11q14.3q21(92716797_92927742) × 1 | 0.21 Mb | |
| 11q22.3q23.2(106853105_113669303) × 1 | 6.8 Mb | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cennamo, M.; Sirocchi, D.; Giudici, C.; Giagnacovo, M.; Petracco, G.; Ferrario, D.; Garganigo, S.; Papa, A.; Veniani, E.; Squizzato, A.; et al. A Peculiar CLL Case with Complex Chromosome 6 Rearrangements and Refinement of All Breakpoints at the Gene Level by Genomic Array: A Case Report. J. Clin. Med. 2023, 12, 4110. https://doi.org/10.3390/jcm12124110
Cennamo M, Sirocchi D, Giudici C, Giagnacovo M, Petracco G, Ferrario D, Garganigo S, Papa A, Veniani E, Squizzato A, et al. A Peculiar CLL Case with Complex Chromosome 6 Rearrangements and Refinement of All Breakpoints at the Gene Level by Genomic Array: A Case Report. Journal of Clinical Medicine. 2023; 12(12):4110. https://doi.org/10.3390/jcm12124110
Chicago/Turabian StyleCennamo, Michele, Davide Sirocchi, Carolina Giudici, Marzia Giagnacovo, Guido Petracco, Daniela Ferrario, Simona Garganigo, Angela Papa, Emanuela Veniani, Alessandro Squizzato, and et al. 2023. "A Peculiar CLL Case with Complex Chromosome 6 Rearrangements and Refinement of All Breakpoints at the Gene Level by Genomic Array: A Case Report" Journal of Clinical Medicine 12, no. 12: 4110. https://doi.org/10.3390/jcm12124110
APA StyleCennamo, M., Sirocchi, D., Giudici, C., Giagnacovo, M., Petracco, G., Ferrario, D., Garganigo, S., Papa, A., Veniani, E., Squizzato, A., Del Vecchio, L., Patriarca, C., Partenope, M., & Modena, P. (2023). A Peculiar CLL Case with Complex Chromosome 6 Rearrangements and Refinement of All Breakpoints at the Gene Level by Genomic Array: A Case Report. Journal of Clinical Medicine, 12(12), 4110. https://doi.org/10.3390/jcm12124110







