Manual Therapy Effects on Nonspecific Neck Pain Are Not Mediated by Mechanisms Related to Conditioned Pain Modulation: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
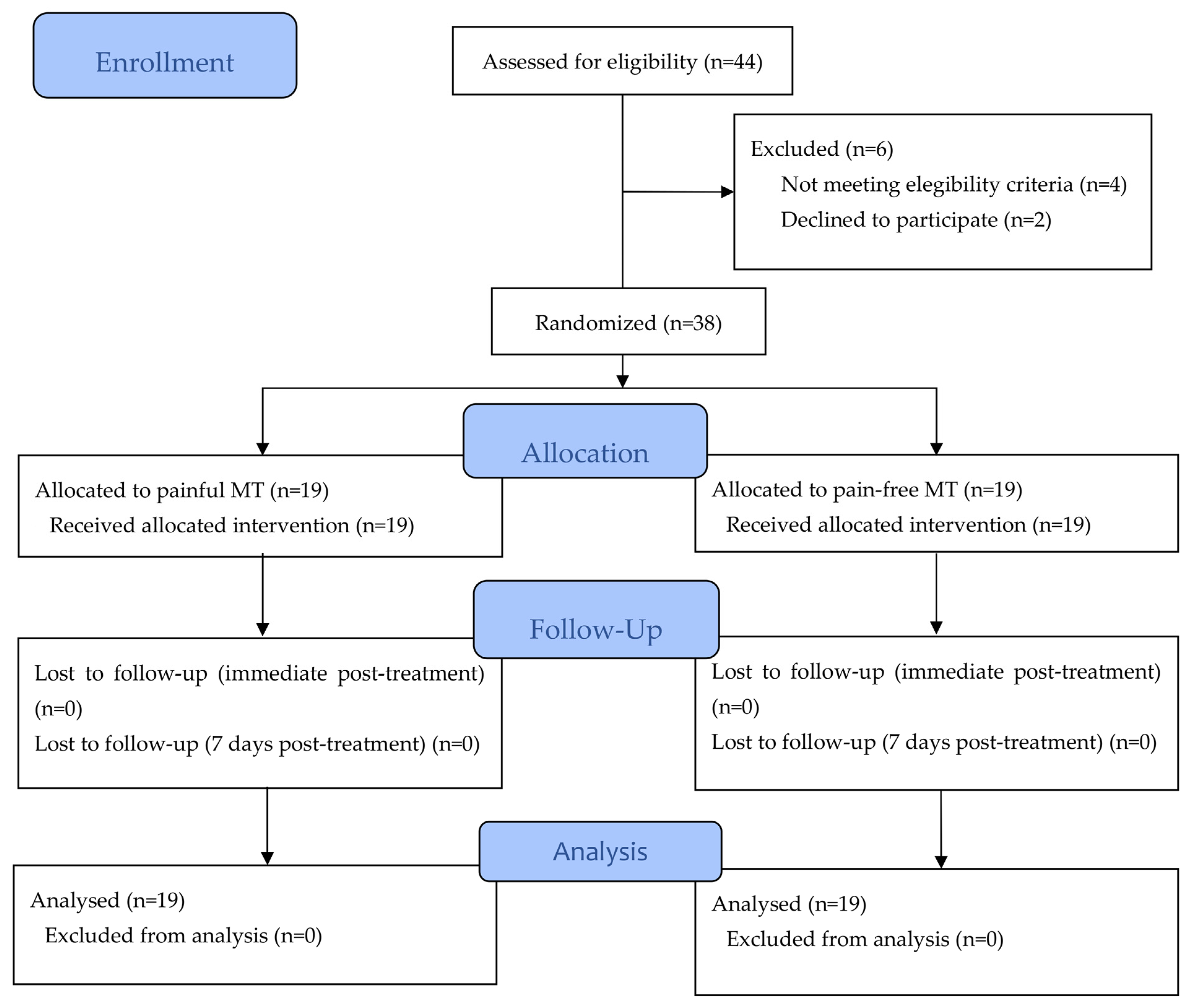
2.1. Design
2.2. Participants
2.3. Treatment
- Posteroanterior passive joint mobilization: The therapist placed the tip of their thumbs on the posterior surface of the spinous process, previously evaluated as the most painful, while gently resting the other fingers around the participant’s neck [31]. Oscillations were performed at a frequency of one oscillation per second for a total of nine minutes, divided into three sets of three minutes, with a one-minute rest interval.
- Pressure: The therapist applied digital ischemic compression on the point with the highest hyperalgesia [32] in each of the following regions: right upper trapezius, left upper trapezius, right paravertebral muscles and left paravertebral muscles. The pressure was maintained for one minute at each point.
- Massage: The therapist performed slow muscle fiber gliding techniques to control the pain being caused. The upper trapezius muscles were targeted for three minutes each, starting with the right side and then moving to the left, with passes from the acromion to the occipital region. Another three minutes were dedicated to the paravertebral musculature on each side, following the same order, with passes from the T1 vertebra to the occipital region.
2.4. Outcomes
2.4.1. Demographic and Clinical Characteristics
2.4.2. Psychophysical Variables
- Pressure Pain Thresholds (PPT)
- Conditioned pain modulation
- Temporal summation of pain
- Cold pain intensity
2.4.3. Intensity of Neck Pain
2.4.4. Self-Perceived Improvement by Global Rating of Change (GROC Scale)
2.4.5. Expectations
2.5. Statistical Analysis
2.6. Sample Size Calculation
3. Results
3.1. Effects on Psychophysical Variables
3.2. Effects on Intensity of Neck Pain
3.3. Self-Perceived Improvement
3.4. Association of Baseline CPM and TSP with the Effects of Treatments on PPTs, Pain Intensity and Self-Perceived Improvement
3.5. Association of Expectations with the Effects of Treatments on PPTs, Pain Intensity and Self-Perceived Improvement
3.6. Blinding Assessment
4. Discussion
- Clinical Relevance
- Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoy, D.; March, L.; Woolf, A.; Blyth, F.; Brooks, P.; Smith, E.; Vos, T.; Barendregt, J.; Blore, J.; Murray, C.; et al. The Global Burden of Neck Pain: Estimates from the Global Burden of Disease 2010 Study. Ann. Rheum. Dis. 2014, 73, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Kolahi, A.-A.; Hoy, D.; Buchbinder, R.; Mansournia, M.A.; Bettampadi, D.; Ashrafi-Asgarabad, A.; Almasi-Hashiani, A.; Smith, E.; Sepidarkish, M.; et al. Global, Regional, and National Burden of Neck Pain in the General Population, 1990–2017: Systematic Analysis of the Global Burden of Disease Study 2017. BMJ 2020, 368, m791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vasseljen, O.; Woodhouse, A.; Bjørngaard, J.H.; Leivseth, L. Natural Course of Acute Neck and Low Back Pain in the General Population: The HUNT Study. Pain 2013, 154, 1237–1244. [Google Scholar] [CrossRef]
- Farrell, S.F.; Smith, A.D.; Hancock, M.J.; Webb, A.L.; Sterling, M. Cervical Spine Findings on MRI in People with Neck Pain Compared with Pain-Free Controls: A Systematic Review and Meta-Analysis. J. Magn. Reson. Imaging 2019, 49, 1638–1654. [Google Scholar] [CrossRef]
- Carlesso, L.C.; Macdermid, J.C.; Gross, A.R.; Walton, D.M.; Santaguida, P.L. Treatment Preferences amongst Physical Therapists and Chiropractors for the Management of Neck Pain: Results of an International Survey. Chiropr. Man. Ther. 2014, 22, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K. Neck Pain: Revision 2017. J. Orthop. Sport. Phys. Ther. 2017, 47, A1–A83. [Google Scholar] [CrossRef] [Green Version]
- Bier, J.D.; Scholten-Peeters, W.G.M.; Staal, J.B.; Pool, J.; van Tulder, M.W.; Beekman, E.; Knoop, J.; Meerhoff, G.; Verhagen, A.P. Clinical Practice Guideline for Physical Therapy Assessment and Treatment in Patients with Nonspecific Neck Pain. Phys. Ther. 2018, 98, 162–171. [Google Scholar] [CrossRef] [Green Version]
- Corp, N.; Mansell, G.; Stynes, S.; Wynne-Jones, G.; Morsø, L.; Hill, J.C.; van der Windt, D.A. Evidence-Based Treatment Recommendations for Neck and Low Back Pain across Europe: A Systematic Review of Guidelines. Eur. J. Pain. 2021, 25, 275–295. [Google Scholar] [CrossRef]
- Fredin, K.; Lorås, H. Manual Therapy, Exercise Therapy or Combined Treatment in the Management of Adult Neck Pain—A Systematic Review and Meta-Analysis. Musculoskelet. Sci. Pract. 2017, 31, 62–71. [Google Scholar] [CrossRef]
- Coulter, I.D.; Crawford, C.; Vernon, H.; Hurwitz, E.L.; Khorsan, R.; Booth, M.S.; Herman, P.M. Manipulation and Mobilization for Treating Chronic Nonspecific Neck Pain: A Systematic Review and Meta-Analysis for an Appropriateness Panel. Pain Physician 2019, 22, E55–E70. [Google Scholar] [CrossRef]
- Gross, A.; Miller, J.; D’Sylva, J.; Burnie, S.J.; Goldsmith, C.H.; Graham, N.; Haines, T.; Brønfort, G.; Hoving, J.L. COG Manipulation or Mobilisation for Neck Pain: A Cochrane Review. Man. Ther. 2010, 15, 315–333. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.H.; Huang, G.C. Efficacy of Massage Therapy on Pain and Dysfunction in Patients with Neck Pain: A Systematic Review and Meta-Analysis. Evid. Based Complement. Alternat. Med. 2014, 2014, 204360. [Google Scholar] [CrossRef] [PubMed]
- Tsegay, G.S.; Gebregergs, G.B.; Weleslassie, G.G.; Hailemariam, T.T. Effectiveness of Thoracic Spine Manipulation on the Management of Neck Pain: A Systematic Review and Meta-Analysis of Randomized Control Trials. J. Pain Res. 2023, 16, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Bialosky, J.E.; Beneciuk, J.M.; Bishop, M.D.; Coronado, R.A.; Penza, C.W.; Simon, C.B.; George, S.Z. Unraveling the Mechanisms of Manual Therapy: Modeling an Approach. J. Orthop. Sports Phys. Ther. 2018, 48, 8–18. [Google Scholar] [CrossRef]
- Edwards, R.R.; Dworkin, R.H.; Turk, D.C.; Angst, M.S.; Dionne, R.; Freeman, R.; Hansson, P.; Haroutounian, S.; Arendt-Nielsen, L.; Attal, N.; et al. Patient Phenotyping in Clinical Trials of Chronic Pain Treatments: IMMPACT Recommendations. Pain 2016, 157, 1851–1871. [Google Scholar] [CrossRef]
- Bialosky, J.E.; Bishop, M.D.; Price, D.D.; Robinson, M.E.; George, S.Z. The Mechanisms of Manual Therapy in the Treatment of Musculoskeletal Pain: A Comprehensive Model. Man. Ther. 2009, 14, 531–538. [Google Scholar] [CrossRef] [Green Version]
- Arribas-Romano, A.; Fernández-Carnero, J.; Molina-Rueda, F.; Angulo-Diaz-Parreño, S.; Navarro-Santana, M.J. Efficacy of Physical Therapy on Nociceptive Pain Processing Alterations in Patients with Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Pain Med. 2020, 21, 2502–2517. [Google Scholar] [CrossRef]
- Martínez-Pozas, O.; Sánchez-Romero, E.A.; Beltran-Alacreu, H.; Arribas-Romano, A.; Cuenca-Martínez, F.; Villafañe, J.H.; Fernández-Carnero, J. Effects of Orthopedic Manual Therapy on Pain Sensitization in Patients with Chronic Musculoskeletal Pain: An Umbrella Review with Meta-Meta-Analysis. Am. J. Phys. Med. Rehabil. 2023. [Google Scholar] [CrossRef]
- Yarnitsky, D.; Arendt-Nielsen, L.; Bouhassira, D.; Edwards, R.R.; Fillingim, R.B.; Granot, M.; Hansson, P.; Lautenbacher, S.; Marchand, S.; Wilder-Smith, O. Recommendations on Terminology and Practice of Psychophysical DNIC Testing. Eur. J. Pain 2010, 14, 339. [Google Scholar] [CrossRef]
- Le Bars, D.; Dickenson, A.H.; Besson, J.-M. Diffuse Noxious Inhibitory Controls (DNIC). I. Effects on Dorsal Horn Convergent Neurones in the Rat. Pain 1979, 6, 283–304. [Google Scholar] [CrossRef]
- Sirucek, L.; Ganley, R.P.; Zeilhofer, H.U.; Schweinhardt, P. Diffuse Noxious Inhibitory Controls and Conditioned Pain Modulation: A Shared Neurobiology within the Descending Pain Inhibitory System? Pain 2023, 164, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Yarnitsky, D.; Bouhassira, D.; Drewes, A.M.; Fillingim, R.B.; Granot, M.; Hansson, P.; Landau, R.; Marchand, S.; Matre, D.; Nilsen, K.B.; et al. Recommendations on Practice of Conditioned Pain Modulation (CPM) Testing. Eur. J. Pain 2015, 19, 805–806. [Google Scholar] [CrossRef] [PubMed]
- Piché, M. Mechanistic Perspective on Conditioned Pain Modulation. Pain 2023, 164, e1–e2. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.T.; Riley, J.L.; Bishop, M.D.; Beneciuk, J.M.; Godza, M.; Cruz-Almeida, Y.; Bialosky, J.E. A Psychophysical Study Comparing Massage to Conditioned Pain Modulation: A Single Blind Randomized Controlled Trial in Healthy Participants. J. Bodyw. Mov. Ther. 2021, 27, 426–435. [Google Scholar] [CrossRef]
- Goffaux, P.; Redmond, W.J.; Rainville, P.; Marchand, S. Descending Analgesia--When the Spine Echoes What the Brain Expects. Pain 2007, 130, 137–143. [Google Scholar] [CrossRef]
- Hermans, L.; Van Oosterwijck, J.; Goubert, D.; Goudman, L.; Crombez, G.; Calders, P.; Meeus, M. Inventory of Personal Factors Influencing Conditioned Pain Modulation in Healthy People: A Systematic Literature Review. Pain Pract. 2016, 16, 758–769. [Google Scholar] [CrossRef]
- Wilson, A.T.; Bishop, M.D.; Beneciuk, J.M.; Tilley, H.E.; Riley, J.L.; Cruz-Almeida, Y.; Bialosky, J.E. Expectations Affect Pain Sensitivity Changes during Massage. J. Man. Manip. Ther. 2023, 31, 84–92. [Google Scholar] [CrossRef]
- Bishop, M.D.; Mintken, P.E.; Bialosky, J.E.; Cleland, J.A. Patient Expectations of Benefit from Interventions for Neck Pain and Resulting Influence on Outcomes. J. Orthop. Sports Phys. Ther. 2013, 43, 457–465. [Google Scholar] [CrossRef] [Green Version]
- Ferreira-Valente, M.A.; Pais-Ribeiro, J.L.; Jensen, M.P. Validity of Four Pain Intensity Rating Scales. Pain 2011, 152, 2399–2404. [Google Scholar] [CrossRef]
- Guzmán Pavón, M.J.; Cavero Redondo, I.; Martínez Vizcaíno, V.; Ferri Morales, A.; Lorenzo García, P.; Álvarez Bueno, C. Comparative Effectiveness of Manual Therapy Interventions on Pain and Pressure Pain Threshold in Patients with Myofascial Trigger Points: A Network Meta-Analysis. Clin. J. Pain 2022, 38, 749–760. [Google Scholar] [CrossRef]
- Snodgrass, S.J.; Rivett, D.A.; Sterling, M.; Vicenzino, B. Dose Optimization for Spinal Treatment Effectiveness: A Randomized Controlled Trial Investigating the Effects of High and Low Mobilization Forces in Patients with Neck Pain. J. Orthop. Sports Phys. Ther. 2014, 44, 141–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagrale, A.V.; Glynn, P.; Joshi, A.; Ramteke, G. The Efficacy of an Integrated Neuromuscular Inhibition Technique on Upper Trapezius Trigger Points in Subjects with Non-Specific Neck Pain: A Randomized Controlled Trial. J. Man. Manip. Ther. 2010, 18, 37–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- James, K.E.; Bloch, D.A.; Lee, K.K.; Kraemer, H.C.; Fuller, R.K. An Index for Assessing Blindness in a Multi-Centre Clinical Trial: Disulfiram for Alcohol Cessation—A VA Cooperative Study. Stat. Med. 1996, 15, 1421–1434. [Google Scholar] [CrossRef]
- Bang, H.; Ni, L.; Davis, C.E. Assessment of Blinding in Clinical Trials. Control. Clin. Trials 2004, 25, 143–156. [Google Scholar] [CrossRef]
- Von Korff, M.; Ormel, J.; Keefe, F.J.; Dworkin, S.F. Grading the Severity of Chronic Pain. Pain 1992, 50, 133–149. [Google Scholar] [CrossRef]
- Smith, B.H.; Penny, K.I.; Purves, A.M.; Munro, C.; Wilson, B.; Grimshaw, J.; Chambers, W.A.; Smith, W.C. The Chronic Pain Grade Questionnaire: Validation and Reliability in Postal Research. Pain 1997, 71, 141–147. [Google Scholar] [CrossRef]
- Ferrer-Peña, R.; Gil-Martínez, A.; Pardo-Montero, J.; Jiménez-Penick, V.; Gallego-Izquierdo, T.; La Touche, R. Adaptation and Validation of the Spanish Version of the Graded Chronic Pain Scale. Reumatol. Clin. 2016, 12, 130–138. [Google Scholar] [CrossRef]
- Cuesta-Vargas, A.I.; Roldan-Jimenez, C.; Neblett, R.; Gatchel, R.J. Cross-Cultural Adaptation and Validity of the Spanish Central Sensitization Inventory. Springerplus 2016, 5, 1837. [Google Scholar] [CrossRef] [Green Version]
- Mayer, T.G.; Neblett, R.; Cohen, H.; Howard, K.J.; Choi, Y.H.; Williams, M.J.; Perez, Y.; Gatchel, R.J. The Development and Psychometric Validation of the Central Sensitization Inventory. Pain Pract. 2012, 12, 276–285. [Google Scholar] [CrossRef] [Green Version]
- Neblett, R.; Cohen, H.; Choi, Y.; Hartzell, M.M.; Williams, M.; Mayer, T.G.; Gatchel, R.J. The Central Sensitization Inventory (CSI): Establishing Clinically Significant Values for Identifying Central Sensitivity Syndromes in an Outpatient Chronic Pain Sample. J. Pain 2013, 14, 438–445. [Google Scholar] [CrossRef] [Green Version]
- Andrade Ortega, J.A.; Delgado Martínez, A.D.; Almécija Ruiz, R. Validation of the Spanish Version of the Neck Disability Index. Spine 2010, 35, E114–E118. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Walton, D.M.; Avery, S.; Blanchard, A.; Etruw, E.; McAlpine, C.; Goldsmith, C.H. Measurement Properties of the Neck Disability Index: A Systematic Review. J. Orthop. Sports Phys. Ther. 2009, 39, 400–417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García Campayo, J.; Rodero, B.; Alda, M.; Sobradiel, N.; Montero, J.; Moreno, S. Validation of the Spanish version of the Pain Catastrophizing Scale in fibromyalgia. Med. Clin. 2008, 131, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Pérez, L.; López-Martínez, A.E.; Ruiz-Párraga, G.T. Psychometric Properties of the Spanish Version of the Tampa Scale for Kinesiophobia (TSK). J. Pain 2011, 12, 425–435. [Google Scholar] [CrossRef]
- Solé, E.; Castarlenas, E.; Sánchez-Rodríguez, E.; Galán, S.; de la Vega, R.; Jensen, M.P.; Miró, J. The Reliability and Validity of the Spanish Version of the Fear of Pain Questionnaire. J. Health Psychol. 2019, 24, 1134–1144. [Google Scholar] [CrossRef]
- Sanz, J.; Perdigón, A.L.; Vázquez Valverde, C. Adaptación española del Inventario para la Depresión de Beck-II (BDI-II): 2. Propiedades psicométricas en población general. Clínica Salud 2003, 14, 249–280. [Google Scholar]
- Wiebe, J.S.; Penley, J.A. A Psychometric Comparison of the Beck Depression Inventory-II in English and Spanish. Psychol. Assess 2005, 17, 481–485. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [Green Version]
- Bumberry, W.; Oliver, J.M.; McClure, J.N. Validation of the Beck Depression Inventory in a University Population Using Psychiatric Estimate as the Criterion. J. Consult. Clin. Psychol. 1978, 46, 150–155. [Google Scholar] [CrossRef]
- Spielberger, C. Development of the Spanish Edition of the State-Trait Anxiety Inventory. Interam. J. Psychol 1971, 5, 145–158. [Google Scholar]
- Guillén-Riquelme, A.; Buela-Casal, G. Metaanálisis de Comparación de Grupos y Metaanálisis de Generalización de La Fiabilidad Del Cuestionario State-Trait Anxiety Inventory (STAI). Rev. Española Salud Pública 2014, 88, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Kabacoff, R.I.; Segal, D.L.; Hersen, M.; Van Hasselt, V.B. Psychometric Properties and Diagnostic Utility of the Beck Anxiety Inventory and the State-Trait Anxiety Inventory with Older Adult Psychiatric Outpatients. J. Anxiety Disord. 1997, 11, 33–47. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Zayfert, C.; Gross, R.T. The Pain Anxiety Symptoms Scale: Development and Validation of a Scale to Measure Fear of Pain. Pain 1992, 50, 67–73. [Google Scholar] [CrossRef] [PubMed]
- López-Martínez, A.; Esteve, R.; Ramírez-Maestre, C. The Spanish Version of the Pain Anxiety Symptoms Scale (PASS-20): Preliminary Data on Its Reliability, Validity and Factorial Structure. Eur. J. Pain Suppl. 2011, 5, 265. [Google Scholar] [CrossRef]
- Nussbaum, E.L.; Downes, L. Reliability of Clinical Pressure-Pain Algometric Measurements Obtained on Consecutive Days. Phys. Ther. 1998, 78, 160–169. [Google Scholar] [CrossRef]
- Bisset, L.M.; Evans, K.; Tuttle, N. Reliability of 2 Protocols for Assessing Pressure Pain Threshold in Healthy Young Adults. J. Manip. Physiol. Ther. 2015, 38, 282–287. [Google Scholar] [CrossRef]
- Kennedy, D.L.; Kemp, H.I.; Ridout, D.; Yarnitsky, D.; Rice, A.S.C. Reliability of Conditioned Pain Modulation: A Systematic Review. Pain 2016, 157, 2410–2419. [Google Scholar] [CrossRef] [Green Version]
- Flood, A.; Waddington, G.; Cathcart, S. Examining the Relationship between Endogenous Pain Modulation Capacity and Endurance Exercise Performance. Res. Sports Med. 2017, 25, 300–312. [Google Scholar] [CrossRef]
- Vaegter, H.B.; Handberg, G.; Graven-Nielsen, T. Similarities between Exercise-Induced Hypoalgesia and Conditioned Pain Modulation in Humans. Pain 2014, 155, 158–167. [Google Scholar] [CrossRef]
- Cathcart, S.; Winefield, A.H.; Rolan, P.; Lushington, K. Reliability of Temporal Summation and Diffuse Noxious Inhibitory Control. Pain Res. Manag. 2009, 14, 433–438. [Google Scholar] [CrossRef] [Green Version]
- Nie, H.; Arendt-Nielsen, L.; Andersen, H.; Graven-Nielsen, T. Temporal Summation of Pain Evoked by Mechanical Stimulation in Deep and Superficial Tissue. J. Pain 2005, 6, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, S.; Sterling, M. An Investigation of the Use of a Numeric Pain Rating Scale with Ice Application to the Neck to Determine Cold Hyperalgesia. Man. Ther. 2013, 18, 172–174. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M.; Jull, G.; Vicenzino, B.; Kenardy, J. Sensory Hypersensitivity Occurs Soon after Whiplash Injury and Is Associated with Poor Recovery. Pain 2003, 104, 509–517. [Google Scholar] [CrossRef]
- Cleland, J.A.; Childs, J.D.; Whitman, J.M. Psychometric Properties of the Neck Disability Index and Numeric Pain Rating Scale in Patients with Mechanical Neck Pain. Arch. Phys. Med. Rehabil. 2008, 89, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Stratford, P.W.; Binkley, J.; Solomon, P.; Gill, C.; Finch, E. Assessing Change over Time in Patients with Low Back Pain. Phys. Ther. 1994, 74, 528–533. [Google Scholar] [CrossRef]
- Jaeschke, R.; Singer, J.; Guyatt, G.H. Measurement of Health Status. Ascertaining the Minimal Clinically Important Difference. Control. Clin. Trials 1989, 10, 407–415. [Google Scholar] [CrossRef]
- Kamper, S.J.; Maher, C.G.; Mackay, G. Global Rating of Change Scales: A Review of Strengths and Weaknesses and Considerations for Design. J. Man. Manip. Ther. 2009, 17, 163–170. [Google Scholar] [CrossRef] [Green Version]
- Field, A. Discovering Statistics with IBM SPSS Statistics; Sage: Newbury Park, CA, USA, 2013. [Google Scholar]
- Van Breukelen, G.J.P. ANCOVA versus Change from Baseline: More Power in Randomized Studies, More Bias in Nonrandomized Studies [Corrected]. J. Clin. Epidemiol. 2006, 59, 920–925. [Google Scholar] [CrossRef]
- Zabala Mata, J.; Lascurain-Aguirrebena, I.; Dominguez Lopez, E.; Jatsu Azkue, J. Enhanced Pronociceptive and Disrupted Antinociceptive Mechanisms in Nonspecific Chronic Neck Pain. Phys. Ther. 2021, 101, pzaa223. [Google Scholar] [CrossRef]
- Walton, D.M.; Macdermid, J.C.; Nielson, W.; Teasell, R.W.; Chiasson, M.; Brown, L. Reliability, Standard Error, and Minimum Detectable Change of Clinical Pressure Pain Threshold Testing in People with and without Acute Neck Pain. J. Orthop. Sports Phys. Ther. 2011, 41, 644–650. [Google Scholar] [CrossRef] [Green Version]
- Xie, Y.; Jun, D.; Thomas, L.; Coombes, B.K.; Johnston, V. Comparing Central Pain Processing in Individuals with Non-Traumatic Neck Pain and Healthy Individuals: A Systematic Review and Meta-Analysis. J. Pain 2020, 21, 1101–1124. [Google Scholar] [CrossRef] [PubMed]
- Muhsen, A.; Moss, P.; Gibson, W.; Walker, B.; Jacques, A.; Schug, S.; Wright, A. The Association between Conditioned Pain Modulation and Manipulation-Induced Analgesia in People with Lateral Epicondylalgia. Clin. J. Pain 2019, 35, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M.; Pedler, A.; Chan, C.; Puglisi, M.; Vuvan, V.; Vicenzino, B. Cervical Lateral Glide Increases Nociceptive Flexion Reflex Threshold but Not Pressure or Thermal Pain Thresholds in Chronic Whiplash Associated Disorders: A Pilot Randomised Controlled Trial. Man. Ther. 2010, 15, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Pozsgai, M.; Udvarácz, K.; Péter, I.A.; Than, P.; Nusser, N. Effect of Single End-Range and Not End-Range Maitland Mobilization on Pressure Pain Threshold and Functional Measures in Knee Osteoarthritis: Randomised, Controlled Clinical Trial. Eur. J. Phys. Rehabil. Med. 2022, 58, 774–783. [Google Scholar] [CrossRef] [PubMed]
- Geurts, J.W.; Willems, P.C.; Lockwood, C.; van Kleef, M.; Kleijnen, J.; Dirksen, C. Patient Expectations for Management of Chronic Non-Cancer Pain: A Systematic Review. Health Expect. 2017, 20, 1201–1217. [Google Scholar] [CrossRef] [Green Version]

| Painful MT (n = 19) | Pain-Free MT (n = 19) | Statistic | Between Group p | |
|---|---|---|---|---|
| Sex | 15/4 | 15/4 | ||
| Female, No. (%) | 15 (79) | 15 (79) | Chi2 = 0.00 | 1.000 |
| Male, No. (%) | 4 (21) | 4 (21) | ||
| Age (y) b | 24 (20, 27) | 23 (20, 27) | Z = 0.04 | 0.965 |
| Height (m) a | 1.67 (0.08) | 1.66 (0.11) | t = 0.54 | 0.590 |
| Weight (kg) b | 62 (58, 70) | 57 (54, 70) | Z = 1.20 | 0.231 |
| BMI (kg/m2) b | 22.5 (20.2, 25.1) | 21.7 (20.8, 23.2) | Z = 0.32 | 0.748 |
| Pain duration (mo) b | 36 (36, 84) | 36 (14, 72) | Z = 0.987 | 0.324 |
| Pain intensity (NPRS 0–10) | ||||
| Current a | 3.84 (1.47) | 3.74 (1.55) | t = 0.21 | 0.831 |
| Mean in the last week a | 4.92 (1.36) | 4.42 (1.36) | t = 0.18 | 0.860 |
| Worst in the last week b | 6.5 (6, 8) | 7 (5, 7) | Z = 0.19 | 0.846 |
| Graded Chronic Pain Scale a | 26.7 (9.6) | 31.1 (10.7) | t = −1.34 | 0.189 |
| Central Sensitization Inventory a | 39.5 (10.9) | 36.4 (11.6) | t = 0.85 | 0.401 |
| Neck Disability Index a | 10.4 (3.3) | 10.6 (4.9) | t = −0.19 | 0.847 |
| Pain Catastrophizing Scale (0–52) b | 6 (3, 11) | 9.89 (9.84) | Z = −0.19 | 0.849 |
| Tampa Scale for Kinesophobia (0–44) a | 18.95 (4.2) | 20.6 (5.33) | t = −1.08 | 0.286 |
| Pain Anxiety Symptoms Scale-20 (0–100) a | 22.3 (13) | 28.9 (17.1) | t = −1.35 | 0.187 |
| State Anxiety Inventory (0–60) a | 24.6 (4.4) | 24.3 (4.7) | t = 0.18 | 0.860 |
| Beck Depression Inventory-II (0–63) a | 9.53 (5.34) | 10.3 (9.15) | t = −0.32 | 0.748 |
| Expectations | ||||
| Positive, No. (%) | 17 (89%) | 6 (32%) | Chi2 = 13.62 | 0.001 * |
| Neutral, No. (%) | 1 (5%) | 10 (53%) | ||
| Negative, No. (%) | 1 (5%) | 3 (16%) |
| Variables | Painful MT (n = 19) | Pain-Free MT (n = 19) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline Mean (SD) | Post-Treatment Mean (SD) | Diff. Intra-Group (Post-Base) Diff (95% CI) | Baseline Mean (SD) | Post-Treatment Mean (SD) | Diff. Intra-Group (Post-Base) Diff (95% CI) | Test | p-Value | |
| PPT C7 | 3.09 (1.26) | 3.03 (1.10) | −0.06 (−0.47; 0.35) | 3.51 (1.44) | 3.14 (1.14) | −0.37 (−0.89; 0.16) | t = 0.48 | 0.632 |
| PPT trapezius | 2.08 (0.77) | 2.26 (0.74) | 0.18 (−0.15; 0.51) | 2.16 (0.91) | 2.26 (0.97) | 0.10 (−0.10; 0.31) | z = 0.32 | 0.749 |
| PPT extensor ulnaris | 4.77 (1.31) | 4.49 (1.16) | −0.28 (−0.59; 0.25) | 4.22 (1.38) | 4.26 (1.39) | 0.04 (−0.39; 0.46) | t = −0.85 | 0.403 |
| PPT tibialis anterior | 6.78 (2.55) | 6.59 (1.95) | −0.18 (−0.81; 0.45) | 6.29 (2.50) | 6.16 (2.13) | −0.13 (−0.53; 0.27) | t = 0.26 | 0.793 |
| Parallel CPM | 0.98 (1.23) | 0.43 (0.92) | −0.55 (−1.23; 0.14) | 1.20 (0.92) | 0.58 (1.42) | −0.62 (−1.30; 0.06) | t = −0.25 | 0.805 |
| Sequential CPM | 0.21 (0.99) | 0.01 (0.77) | −0.20 (−0.83; 0.43) | 0.49 (0.67) | 0.14 (1.08) | −0.35 (−0.90; 0.20) | z = −0.31 | 0.760 |
| TSP | 3.5 (1.97) | 3.58 (2.19) | 0.08 (−0.73; 0.88) | 2.5 (2.58) | 3.03 (1.87) | 0.53 (−0.77; 1.82) | t = 0.22 | 0.827 |
| Cold pain intensity | 4.74 (1.96) | 4.44 (1.90) | −0.30 (−0.90; 0.31) | 6.05 (1.78) | 5.5 (1.93) | −0.55 (−1.17; 0.07) | t = −0.05 | 0.959 |
| Follow-Up | Painful MT (n = 19) | Pain-Free MT (n = 19) | Group Diff. (Adj. by Baseline) Mean Diff. (99% CI) | ||
|---|---|---|---|---|---|
| Mean (SD) | Diff. with Baseline Mean Diff. (99% CI) | Mean (SD) | Diff. with Baseline Mean Diff. (99% CI) | ||
| Baseline | 3.94 (1.52) | 3.74 (1.55) | |||
| Post-treatment | 3.59 (1.50) | −0.35 (−1.58, 0.87) | 1.82 (1.12) | −1.92 (−3.08, −0.77) * | 1.74 (0.54, 2.95) * |
| 4 h | 2.91 (2.40) | −1.03 (−2.54, 0.48) | 2.03 (1.62) | −1.71 (−3.13, −0.29) * | 0.83 (−1.01, 2.67) |
| 1 day | 3.35 (1.73) | −0.59 (−1.90, 0.72) | 2.79 (1.74) | −0.95 (−2.19, 0.29) | 0.50 (−1.05, 2.05) |
| 2 days | 3.12 (1.68) | −0.82 (−2.14, 0.49) | 2.55 (1.94) | −1.18 (−2.43, 0.06) | 0.49 (−1.12, 2.10) |
| 3 days | 2.56 (1.68) | −1.38 (−2.78, 0.01) | 2.58 (2.14) | −1.16 (−2.48, 0.16) | −0.09 (−1.82, 1.63) |
| 4 days | 2.82 (1.67) | −1.12 (−2.38, 0.142) | 2.68 (1.92) | −1.05 (−2.24, 0.14) | 0.05 (−1.51, 1.62) |
| 5 days | 2.88 (1.65) | −1.06 (−2.42, 0.30) | 2.63 (1.93) | −1.11 (−2.39, 0.18) | 0.19 (−1.43, 1.81) |
| 6 days | 2.88 (1.87) | −1.06 (−2.40, 0.29) | 2.68 (1.76) | −1.05 (−2.33, 0.22) | 0.13 (−1.49, 1.75) |
| 7 days | 2.35 (1.94) | −1.59 (−2.73, −0.45) * | 2.64 (1.66) | −0.97 (−2.05, 0.11) | −0.53 (−2.01, 0.95) |
| Painful MT (n = 19) Median (IQR) | Pain-Free MT (n = 19) Median (IQR) | Difference (95% CI) | Between Group p | |
|---|---|---|---|---|
| GROC post-treatment | 4 (2–5) | 3 (1–5) | 1 (−1, 2) | 0.308 |
| GROC post-7 days | 3 (1–4) | 1 (0–3) | 1 (0, 3) | 0.149 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arribas-Romano, A.; Fernández-Carnero, J.; González-Zamorano, Y.; Rodríguez-Lagos, L.; Alguacil-Diego, I.M.; Molina-Álvarez, M.; Tejera, D.M.; Mercado-Romero, F. Manual Therapy Effects on Nonspecific Neck Pain Are Not Mediated by Mechanisms Related to Conditioned Pain Modulation: A Randomized Clinical Trial. J. Clin. Med. 2023, 12, 3894. https://doi.org/10.3390/jcm12123894
Arribas-Romano A, Fernández-Carnero J, González-Zamorano Y, Rodríguez-Lagos L, Alguacil-Diego IM, Molina-Álvarez M, Tejera DM, Mercado-Romero F. Manual Therapy Effects on Nonspecific Neck Pain Are Not Mediated by Mechanisms Related to Conditioned Pain Modulation: A Randomized Clinical Trial. Journal of Clinical Medicine. 2023; 12(12):3894. https://doi.org/10.3390/jcm12123894
Chicago/Turabian StyleArribas-Romano, Alberto, Josué Fernández-Carnero, Yeray González-Zamorano, Leonardo Rodríguez-Lagos, Isabel María Alguacil-Diego, Miguel Molina-Álvarez, David Morales Tejera, and Francisco Mercado-Romero. 2023. "Manual Therapy Effects on Nonspecific Neck Pain Are Not Mediated by Mechanisms Related to Conditioned Pain Modulation: A Randomized Clinical Trial" Journal of Clinical Medicine 12, no. 12: 3894. https://doi.org/10.3390/jcm12123894
APA StyleArribas-Romano, A., Fernández-Carnero, J., González-Zamorano, Y., Rodríguez-Lagos, L., Alguacil-Diego, I. M., Molina-Álvarez, M., Tejera, D. M., & Mercado-Romero, F. (2023). Manual Therapy Effects on Nonspecific Neck Pain Are Not Mediated by Mechanisms Related to Conditioned Pain Modulation: A Randomized Clinical Trial. Journal of Clinical Medicine, 12(12), 3894. https://doi.org/10.3390/jcm12123894







