Evaluation of Ocular Perfusion in Patients with End-Stage Renal Disease Receiving Hemodialysis Using Optical Coherence Tomography Angiography
Abstract
1. Introduction
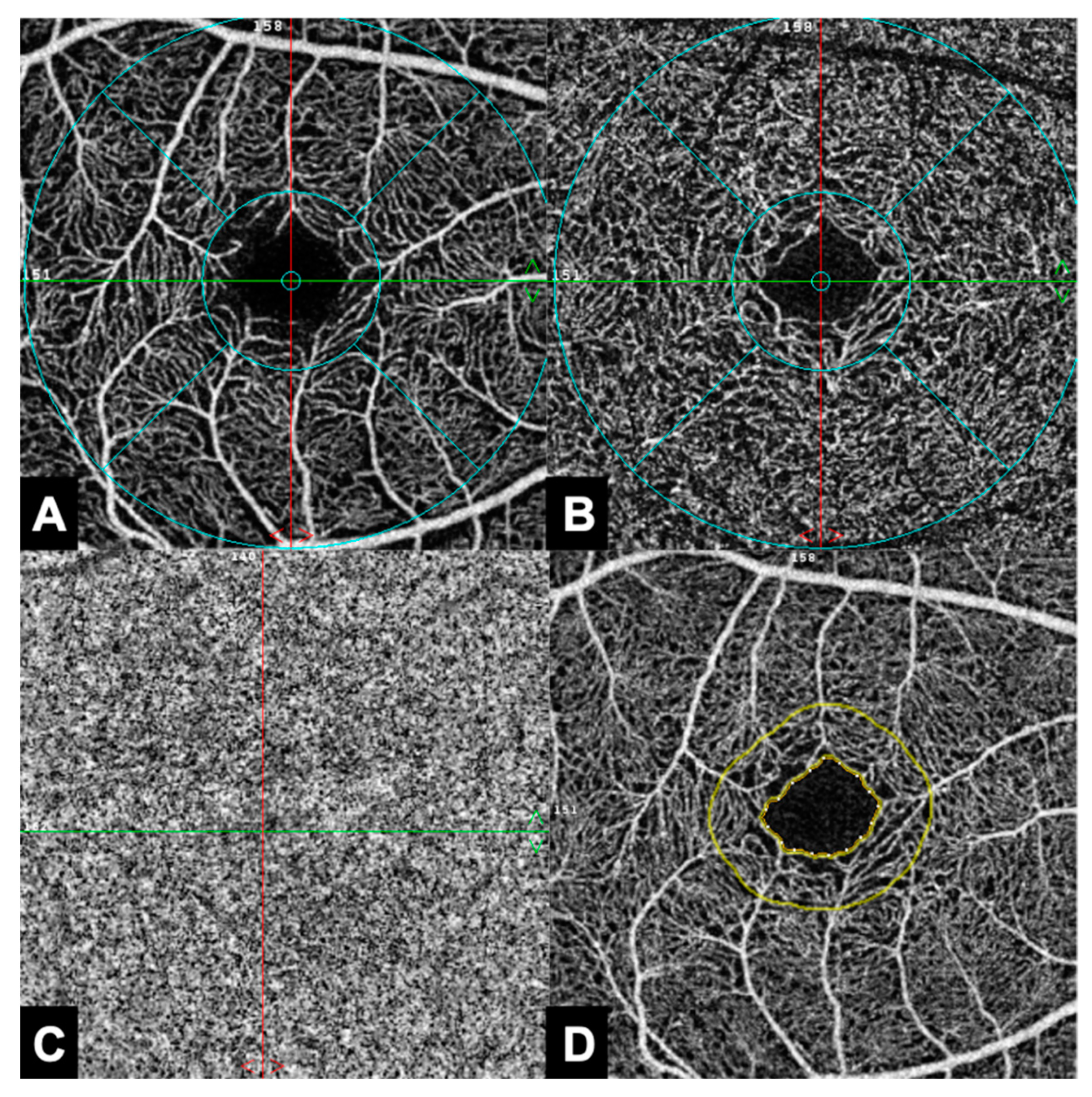
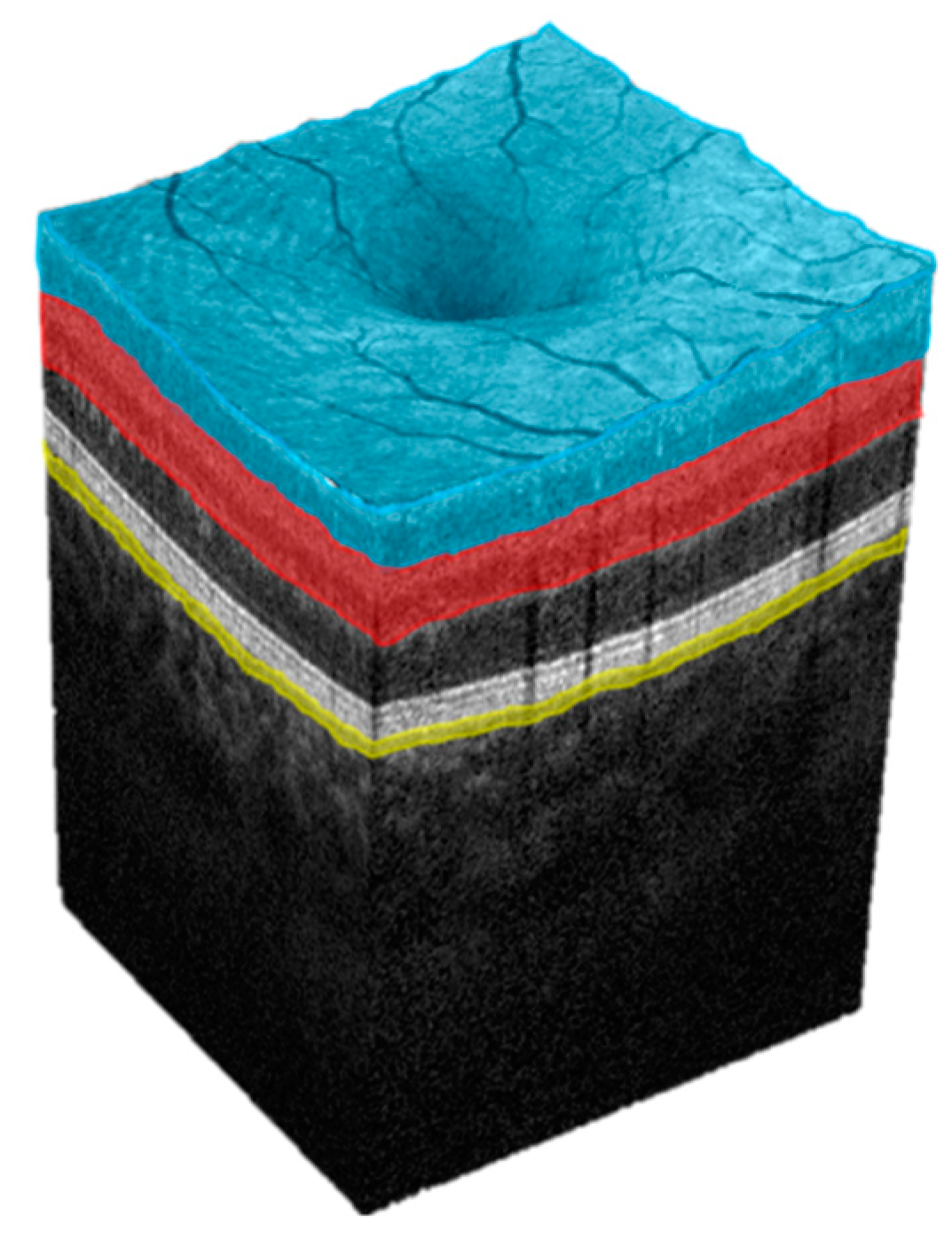
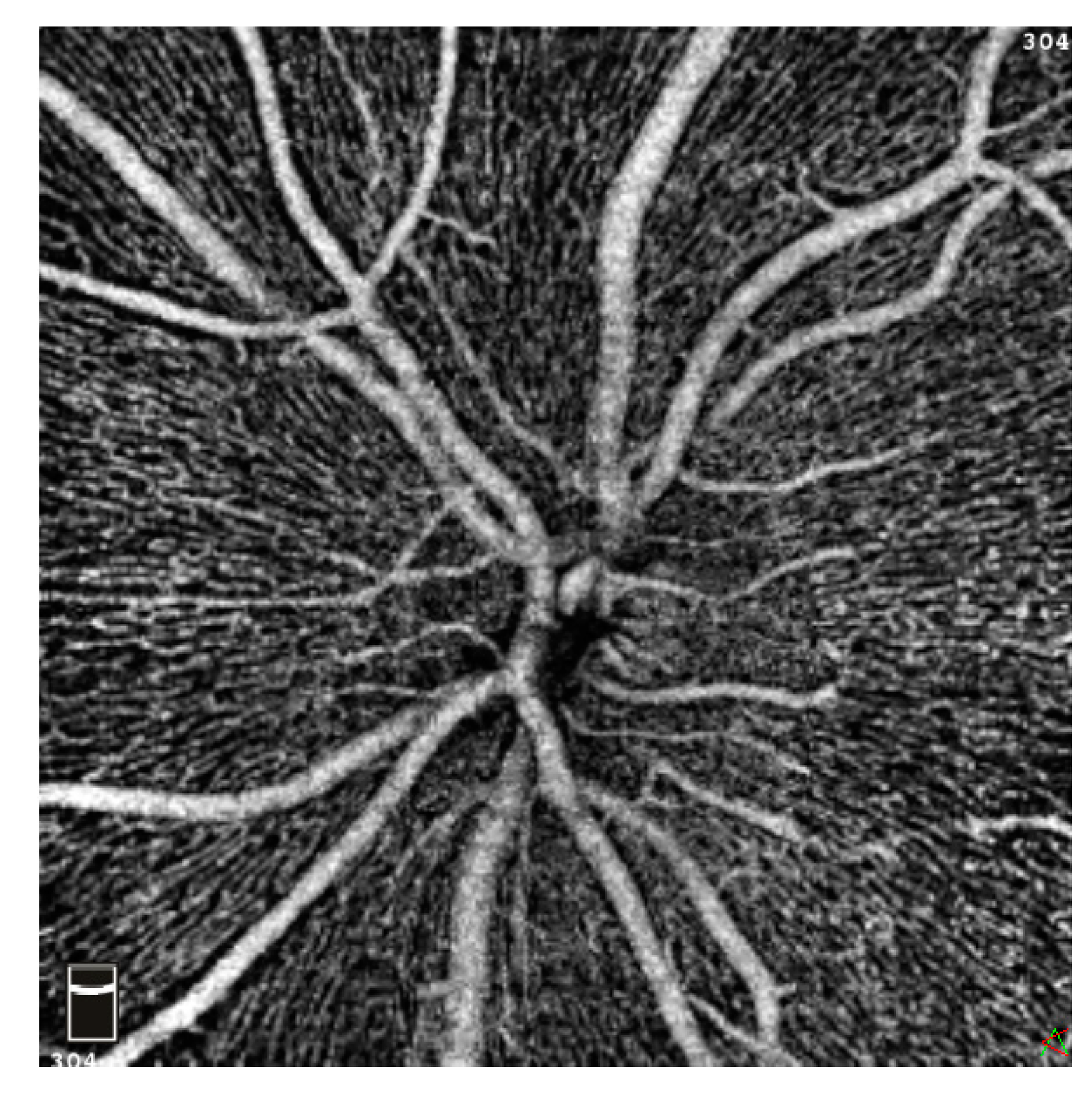
2. Materials and Methods
2.1. Design and Setting
2.2. Patient Examination
2.3. Comparison of Measurements
2.4. Statistical Analysis
3. Results
3.1. Primary Objective
3.2. Secondary Objective
3.3. Tertiary Objective
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Monteiro-Henriques, I.; Rocha-Sousa, A.; Barbosa-Breda, J. Optical Coherence Tomography Angiography Changes in Cardiovascular Systemic Diseases and Risk Factors: A Review. Acta Ophthalmol. 2022, 100, e1–e15. [Google Scholar] [CrossRef]
- Brücher, V.C.; Storp, J.J.; Eter, N.; Alnawaiseh, M. Optical Coherence Tomography Angiography-Derived Flow Density: A Review of the Influencing Factors. Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.W.; Wong, T.Y.; Cheng, C.-Y.; Sabanayagam, C. Kidney and Eye Diseases: Common Risk Factors, Etiological Mechanisms, and Pathways. Kidney Int. 2014, 85, 1290–1302. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.W.; Lamoureux, E.L.; Cheng, C.-Y.; Cheung, G.C.M.; Tai, E.S.; Wong, T.Y.; Sabanayagam, C. Increased Burden of Vision Impairment and Eye Diseases in Persons with Chronic Kidney Disease—A Population-Based Study. EBioMedicine 2016, 5, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Sarnak, M.J.; Foley, R.N. Cardiovascular Mortality in the General Population Versus Dialysis: A Glass Half Full or Empty? Am. J. Kidney Dis. 2011, 58, 4–6. [Google Scholar] [CrossRef]
- Kooman, J.P.; Kotanko, P.; Schols, A.M.W.J.; Shiels, P.G.; Stenvinkel, P. Chronic Kidney Disease and Premature Ageing. Nat. Rev. Nephrol. 2014, 10, 732–742. [Google Scholar] [CrossRef] [PubMed]
- London, G.M.; Safar, M.E.; Pannier, B. Aortic Aging in ESRD: Structural, Hemodynamic, and Mortality Implications. J. Am. Soc. Nephrol. JASN 2016, 27, 1837–1846. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-K.; Wang, Y.-Y.; Liu, C.; Shi, T.-T.; Lu, J.; Cao, X.; Yang, F.-Y.; Feng, J.-P.; Chen, C.; Ji, L.-N.; et al. Urine Proteome Specific for Eye Damage Can Predict Kidney Damage in Patients with Type 2 Diabetes: A Case-Control and a 5.3-Year Prospective Cohort Study. Diabetes Care 2017, 40, 253–260. [Google Scholar] [CrossRef]
- Niutta, A.; Spicci, D.; Barcaroli, I. Fluoroangiographic Findings in Hemodialyzed Patients. Ann. Ophthalmol. 1993, 25, 375–380. [Google Scholar]
- Mayali, H.; Altinisik, M.; Sarigul, C.; Toraman, A.; Turkoglu, M.S.; Kurt, E. Multimodal Ocular Evaluation in Hemodialysis Patients. Int. Ophthalmol. 2021, 41, 1799–1805. [Google Scholar] [CrossRef]
- Spaide, R.F.; Fujimoto, J.G.; Waheed, N.K.; Sadda, S.R.; Staurenghi, G. Optical Coherence Tomography Angiography. Prog. Retin. Eye Res. 2018, 64, 1–55. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.U.; Lee, D.E.; Kang, M.H.; Seong, M.; Yi, J.-H.; Han, S.-W.; Cho, H. Optical Coherence Tomography Angiography Analysis of Changes in the Retina and the Choroid after Haemodialysis. Sci. Rep. 2018, 8, 17184. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Weng, H.; Li, Q.; Wang, Z. Changes in Retina and Choroid after Haemodialysis Assessed Using Optical Coherence Tomography Angiography. Clin. Exp. Optom. 2018, 101, 674–679. [Google Scholar] [CrossRef]
- Coppolino, G.; Bolignano, D.; Presta, P.; Ferrari, F.F.; Lionetti, G.; Borselli, M.; Randazzo, G.; Andreucci, M.; Bonelli, A.; Errante, A.; et al. Acquisition of Optical Coherence Tomography Angiography Metrics during Hemodialysis Procedures: A Pilot Study. Front. Med. 2022, 9, 1057165. [Google Scholar] [CrossRef]
- Wang, W.; He, M.; Gong, X.; Wang, L.; Meng, J.; Li, Y.; Xiong, K.; Li, W.; Huang, W. Association of Renal Function with Retinal Vessel Density in Patients with Type 2 Diabetes by Using Swept-Source Optical Coherence Tomographic Angiography. Br. J. Ophthalmol. 2020, 104, 1768–1773. [Google Scholar] [CrossRef] [PubMed]
- Yong, M.H.; Ong, M.Y.; Tan, K.S.; Hussein, S.H.; Mohd Zain, A.; Mohd, R.; Mustafar, R.; Wan Abdul Halim, W.H. Retinal Optical Coherence Tomography Angiography Parameters Between Patients with Different Causes of Chronic Kidney Disease. Front. Cell. Neurosci. 2022, 16, 766619. [Google Scholar] [CrossRef]
- Yao, T.; He, Y.; Huang, L.; Chen, J.; Zhang, Z.; Yang, W.; Gao, X.; Dan, Y.; Huai, S.; Ou, S.; et al. Quantitative Vessel Density Analysis of Macular and Peripapillary Areas by Optical Coherence Tomography Angiography in Adults with Primary Nephrotic Syndrome. Microvasc. Res. 2022, 144, 104407. [Google Scholar] [CrossRef]
- Lahme, L.; Marchiori, E.; Panuccio, G.; Nelis, P.; Schubert, F.; Mihailovic, N.; Torsello, G.; Eter, N.; Alnawaiseh, M. Changes in retinal flow density measured by optical coherence tomography angiography in patients with carotid artery stenosis after carotid endarterectomy. Sci. Rep. 2018, 21, 17161. [Google Scholar] [CrossRef]
- Lahme, L.; Esser, E.L.; Mihailovic, N.; Schubert, F.; Lauermann, J.; Johnen, A.; Eter, N.; Duning, T.; Alnawaiseh, M. Evaluation of Ocular Perfusion in Alzheimer’s Disease Using Optical Coherence Tomography Angiography. J. Alzheimers Dis. 2018, 66, 1745–1752. [Google Scholar] [CrossRef]
- Tsokolas, G.; Tsaousis, K.T.; Diakonis, V.F.; Matsou, A.; Tyradellis, S. Optical Coherence Tomography Angiography in Neurodegenerative Diseases: A Review. Eye Brain. 2020, 14, 73–87. [Google Scholar] [CrossRef]
- Schmitz, B.; Nelis, P.; Rolfes, F.; Alnawaiseh, M.; Klose, A.; Krüger, M.; Eter, N.; Brand, S.-M.; Alten, F. Effects of High-Intensity Interval Training on Optic Nerve Head and Macular Perfusion Using Optical Coherence Tomography Angiography in Healthy Adults. Atherosclerosis 2018, 274, 8–15. [Google Scholar] [CrossRef]
- Li, X.; Xie, J.; Zhang, L.; Cui, Y.; Zhang, G.; Chen, X.; Wang, J.; Zhang, A.; Huang, T.; Meng, Q. Identifying Microvascular and Neural Parameters Related to the Severity of Diabetic Retinopathy Using Optical Coherence Tomography Angiography. Investig. Ophthalmol. Vis. Sci. 2020, 61, 39. [Google Scholar] [CrossRef]
- Cheng, B.-C.; Chen, P.-C.; Chen, P.-C.; Lu, C.-H.; Huang, Y.-C.; Chou, K.-H.; Li, S.-H.; Lin, A.-N.; Lin, W.-C. Decreased Cerebral Blood Flow and Improved Cognitive Function in Patients with End-Stage Renal Disease after Peritoneal Dialysis: An Arterial Spin-Labelling Study. Eur. Radiol. 2019, 29, 1415–1424. [Google Scholar] [CrossRef]
- Isshiki, R.; Kobayashi, S.; Iwagami, M.; Tsutumi, D.; Mochida, Y.; Ishioka, K.; Oka, M.; Maesato, K.; Moriya, H.; Ohtake, T.; et al. Cerebral Blood Flow in Patients with Peritoneal Dialysis by an Easy Z-Score Imaging System for Brain Perfusion Single-Photon Emission Tomography. Ther. Apher. Dial. 2014, 18, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Kalirao, P.; Pederson, S.; Foley, R.N.; Kolste, A.; Tupper, D.; Zaun, D.; Buot, V.; Murray, A.M. Cognitive Impairment in Peritoneal Dialysis Patients. Am. J. Kidney Dis. 2011, 57, 612–620. [Google Scholar] [CrossRef]
- Weiner, D.E.; Dad, T. Stroke and Chronic Kidney Disease: Epidemiology, Pathogenesis, and Management Across Kidney Disease Stages. Semin. Nephrol. 2015, 35, 311–322. [Google Scholar] [CrossRef]
- Toyoda, K.; Ninomiya, T. Stroke and Cerebrovascular Diseases in Patients with Chronic Kidney Disease. Lancet Neurol. 2014, 13, 823–833. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.; Sims, D.; Ferro, C.J. Modulation of Stroke Risk in Chronic Kidney Disease. Clin. Kidney J. 2016, 9, 29–38. [Google Scholar] [CrossRef]
- Murray, A.M.; Seliger, S.; Lakshminarayan, K.; Herzog, C.A.; Solid, C.A. Incidence of Stroke Before and After Dialysis Initiation in Older Patients. J. Am. Soc. Nephrol. 2013, 24, 1166–1173. [Google Scholar] [CrossRef]
- London, G.M. Arterial Stiffness in Chronic Kidney Disease and End-Stage Renal Disease. Blood Purif. 2018, 45, 154–158. [Google Scholar] [CrossRef]
- Jablonski, K.L.; Chonchol, M. Vascular Calcification in End-Stage Renal Disease. Hemodial. Int. 2013, 17 (Suppl. S1), S17–S21. [Google Scholar] [CrossRef] [PubMed]
- Fursova, A.Z.; Vasil’eva, M.V.; Derbeneva, A.S.; Tarasov, M.S.; Chubar, N.V.; Nikulich, I.F.; Gusarevitch, O.G. Optical coherence tomography angiography in the diagnosis of retinal microvascular changes in chronic kidney disease (clinical observations). Vestn. Oftalmol. 2021, 137, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Vadalà, M.; Castellucci, M.; Guarrasi, G.; Terrasi, M.; La Blasca, T.; Mulè, G. Retinal and Choroidal Vasculature Changes Associated with Chronic Kidney Disease. Graefes Arch. Clin. Exp. Ophthalmol. 2019, 257, 1687–1698. [Google Scholar] [CrossRef] [PubMed]
- Alnawaiseh, M.; Brand, C.; Bormann, E.; Sauerland, C.; Eter, N. Quantification of Macular Perfusion Using Optical Coherence Tomography Angiography: Repeatability and Impact of an Eye-Tracking System. BMC Ophthalmol. 2018, 18, 123. [Google Scholar] [CrossRef] [PubMed]
- Mihailovic, N.; Brand, C.; Lahme, L.; Schubert, F.; Bormann, E.; Eter, N.; Alnawaiseh, M. Repeatability, Reproducibility and Agreement of Foveal Avascular Zone Measurements Using Three Different Optical Coherence Tomography Angiography Devices. PLoS ONE 2018, 13, e0206045. [Google Scholar] [CrossRef]
- Spaide, R.F.; Curcio, C.A. Evaluation of Segmentation of the Superficial and Deep Vascular Layers of the Retina by Optical Coherence Tomography Angiography Instruments in Normal Eyes. JAMA Ophthalmol. 2017, 135, 259–262. [Google Scholar] [CrossRef]
- Al-Sheikh, M.; Ghasemi Falavarjani, K.; Akil, H.; Sadda, S.R. Impact of Image Quality on OCT Angiography Based Quantitative Measurements. Int. J. Retina Vitr. 2017, 3, 13. [Google Scholar] [CrossRef]
- Fenner, B.J.; Tan, G.S.W.; Tan, A.C.S.; Yeo, I.Y.S.; Wong, T.Y.; Cheung, G.C.M. Identification of Imaging Features That Determine Quality and Repeatability of Retinal Capillary Plexus Density Measurements in OCT Angiography. Br. J. Ophthalmol. 2018, 102, 509–514. [Google Scholar] [CrossRef]
- Zong, Y.; Xu, H.; Yu, J.; Jiang, C.; Kong, X.; He, Y.; Sun, X. Retinal Vascular Autoregulation during Phase IV of the Valsalva Maneuver: An Optical Coherence Tomography Angiography Study in Healthy Chinese Adults. Front. Physiol. 2017, 8, 553. [Google Scholar] [CrossRef]
- Kornfield, T.E.; Newman, E.A. Regulation of Blood Flow in the Retinal Trilaminar Vascular Network. J. Neurosci. 2014, 34, 11504–11513. [Google Scholar] [CrossRef]
- Maharshak, I.; Hecht, I.; Mankuta, L.; Achiron, A.; Spierer, O.; Burgansky, Z.; Bar, A.; Grossbard, A.; Katkov, A.; Cernes, R.; et al. The Effect of Hemodialysis on Individual Retinal Layer Thickness. Int. Ophthalmol. 2021, 41, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Kal, A.; Kal, O.; Eroglu, F.C.; Öner, O.; Kucukerdonmez, C.; Yılmaz, G. Evaluation of Choroidal and Retinal Thickness Measurements in Adult Hemodialysis Patients Using Spectral-Domain Optical Coherence Tomography. Arq. Bras. Oftalmol. 2016, 79, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Ulaş, F.; Doğan, Ü.; Keleş, A.; Ertilav, M.; Tekçe, H.; Çelebi, S. Evaluation of Choroidal and Retinal Thickness Measurements Using Optical Coherence Tomography in Non-Diabetic Haemodialysis Patients. Int. Ophthalmol. 2013, 33, 533–539. [Google Scholar] [CrossRef]
- Theodossiadis, P.G.; Theodoropoulou, S.; Neamonitou, G.; Grigoropoulos, V.; Liarakos, V.; Triantou, E.; Theodossiadis, G.P.; Vlahakos, D.V. Hemodialysis-Induced Alterations in Macular Thickness Measured by Optical Coherence Tomography in Diabetic Patients with End-Stage Renal Disease. Ophthalmologica 2012, 227, 90–94. [Google Scholar] [CrossRef]
- Chrapko, B.E.; Bednarek-Skublewska, A.; Stas’kiewicz, G.; Ksiazek, A. Relationship of Haemodialysis Therapy Duration and Cardiac Adrenergic System Function Assessed by Iodine-123 Metaiodobenzylguanidine Imaging in Haemodialysed Nondiabetic Patients. Nucl. Med. Commun. 2012, 33, 155. [Google Scholar] [CrossRef]
- Arnould, L.; Guenancia, C.; Azemar, A.; Alan, G.; Pitois, S.; Bichat, F.; Zeller, M.; Gabrielle, P.H.; Bron, A.M.; Creuzot-Garcher, C.; et al. The EYE-MI Pilot Study: A Prospective Acute Coronary Syndrome Cohort Evaluated With Retinal Optical Coherence Tomography Angiography. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4299–4306. [Google Scholar] [CrossRef]
- Alnawaiseh, M.; Eckardt, F.; Mihailovic, N.; Frommeyer, G.; Diener, R.; Rosenberger, F.; Eckardt, L.; Eter, N.; Lahme, L.; Lange, P.S. Ocular perfusion in patients with reduced left ventricular ejection fraction measured by optical coherence tomography angiography. Graefes Arch. Clin. Exp. Ophthalmol. 2021, 259, 3605–3611. [Google Scholar] [CrossRef] [PubMed]
| Study Group | Control Group | p Value | |
|---|---|---|---|
| Patients (n) | 24 | 24 | |
| Eyes (n) | 24 | 24 | |
| Age (years) | 56.11 (49.77; 64.40) | 56.86 (48.92; 65.71) | 0.97 |
| Gender (m: f) | 13: 11 | 13: 11 | |
| Laterality (r: l) | 7: 17 | 9: 15 | |
| Patients with arterial hypertension (treated; n; %) | 21 (84%) | 16 (67%) | |
| Patients with arterial hypertension (untreated; n; %) | 0 (0%) | 0 (0%) | |
| Patients who were active smokers at Time of study enrolment (n, %) | 4 (16%) | 3 (12%) | |
| Patients who were former smokers at Time of study enrolment (n, %) | 2 (8%) | 1 (4%) | |
| Patients with diabetes (n, %) | 5 (20%) | 5 (20%) | |
| Duration of HD treatment at time of OCTA imaging (months) | 46.0 (31.0; 84.0) | ||
| QI (macula) | 8.00 (7.00; 8.00) | 8.00 (7.00; 8.25) | 0.33 |
| SSI (macula) | 64.53 (59.41; 67.89) | 65.95 (62.34; 69.22) | 0.11 |
| QI (optic disc) | 8.00 (7.00; 8.00) | 8.00 (7.00; 8.00) | 0.52 |
| SSI (optic disc) | 64.53 (59.41; 67.89) | 65.39 (59.74; 68.94) | 0.10 |
| Visual acuity (LogMAR) | 0.1 (0.0; 0.1) | 0.1 (0.0; 0.1) | 0.77 |
| Spherical equivalent | 0 (−1.59; 0.09) | 0 (−0.69; 1.28) | 0.32 |
| Location | Parameter | Study Group | Control Group | p Values |
|---|---|---|---|---|
| SCP (%) | Whole en face | 41.41 (38.92; 44.39) | 45.00 (43.45; 47.15) | <0.01 |
| Fovea | 16.29 (14.11; 19.61) | 17.24 (14.86; 22.00) | 0.29 | |
| Para fovea | 43.98 (40.82; 46.32) | 47.74 (46.36; 49.91) | <0.01 | |
| DCP (%) | Whole en face | 48.19 (45.49; 51.69) | 49.23 (47.21; 51.34) | 0.33 |
| Fovea | 31.43 (26.74; 36.67) | 33.71 (29.23; 38.41) | 0.13 | |
| Para fovea | 49.77 (48.26; 53.03) | 51.02 (48.63; 53.39) | 0.42 | |
| CC (%) | Whole en face | 65.96 (64.55; 68.82) | 69.12 (65.81; 71.97) | 0.05 |
| Fovea | 65.51 (58.02; 69.22) | 68.58 (66.38; 71.64) | 0.01 | |
| Para fovea | 65.38 (63.65; 68.35) | 68.47 (65.08; 71.74) | 0.05 | |
| FAZ | FAZ area (mm2) | 0.29 (0.20; 0.35) | 0.28 (0.19; 0.32) | 0.42 |
| Perimeter (mm) | 2.11 (1.87; 2.40) | 2.09 (1.68; 2.34) | 0.38 | |
| Acircularity index | 1.17 (1.11; 1.18) | 1.13 (1.10; 1.21) | 0.41 | |
| FD-300 area density | 48.13 (43.90; 48.89) | 48.68 (46.96; 49.82) | 0.08 | |
| FD-300 length density | 16.38 (14.69; 17.42) | 17.32 (16.54; 17.99) | <0.01 | |
| RPC (%) | Whole en face | 54.20 (50.90; 56.14) | 55.45 (53.80; 57.15) | 0.09 |
| Inside disc | 57.99 (55.74; 62.94) | 59.88 (55.88; 61.95) | 0.90 | |
| Peripapillary | 55.76 (51.59; 58.76) | 57.45 (56.02; 60.10) | 0.07 |
| Location | Parameter | Duration of HD Treatment at Time of OCTA Imaging | |
|---|---|---|---|
| r Spearman | p-Value | ||
| SCP | Whole en face | −0.47 | <0.01 |
| Fovea | −0.26 | 0.08 | |
| Para fovea | −0.52 | <0.01 | |
| DCP | Whole en face | −0.21 | 0.15 |
| Fovea | −0.31 | 0.03 | |
| Para fovea | −0.16 | 0.28 | |
| CC | Whole en face | −0.39 | 0.01 |
| Fovea | −0.30 | 0.04 | |
| Para fovea | −0.40 | 0.01 | |
| FAZ | FAZ area (mm2) | 0.22 | 0.14 |
| Perimeter (mm) | 0.25 | 0.09 | |
| Acircularity index | 0.21 | 0.16 | |
| FD-300 area density | −0.29 | 0.05 | |
| FD-300 length Density | −0.41 | <0.01 | |
| RPC | Whole en face all | −0.37 | 0.01 |
| Inside disc all | −0.09 | 0.55 | |
| Peripapillary all | −0.37 | 0.01 | |
| Parameter | Study Group | Control Group | p Values |
|---|---|---|---|
| Total RT (µm) | 295.90 (285.20; 310.00) | 312.44 (304.90; 328.80) | <0.01 |
| Total RV (mm3) | 2.67 (2.58; 2.80) | 2.85 (2.82; 2.96) | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lahme, L.; Storp, J.J.; Marchiori, E.; Esser, E.; Eter, N.; Mihailovic, N.; Alnawaiseh, M. Evaluation of Ocular Perfusion in Patients with End-Stage Renal Disease Receiving Hemodialysis Using Optical Coherence Tomography Angiography. J. Clin. Med. 2023, 12, 3836. https://doi.org/10.3390/jcm12113836
Lahme L, Storp JJ, Marchiori E, Esser E, Eter N, Mihailovic N, Alnawaiseh M. Evaluation of Ocular Perfusion in Patients with End-Stage Renal Disease Receiving Hemodialysis Using Optical Coherence Tomography Angiography. Journal of Clinical Medicine. 2023; 12(11):3836. https://doi.org/10.3390/jcm12113836
Chicago/Turabian StyleLahme, Larissa, Jens Julian Storp, Elena Marchiori, Eliane Esser, Nicole Eter, Natasa Mihailovic, and Maged Alnawaiseh. 2023. "Evaluation of Ocular Perfusion in Patients with End-Stage Renal Disease Receiving Hemodialysis Using Optical Coherence Tomography Angiography" Journal of Clinical Medicine 12, no. 11: 3836. https://doi.org/10.3390/jcm12113836
APA StyleLahme, L., Storp, J. J., Marchiori, E., Esser, E., Eter, N., Mihailovic, N., & Alnawaiseh, M. (2023). Evaluation of Ocular Perfusion in Patients with End-Stage Renal Disease Receiving Hemodialysis Using Optical Coherence Tomography Angiography. Journal of Clinical Medicine, 12(11), 3836. https://doi.org/10.3390/jcm12113836








