MELD-Na Alterations on the Liver Transplant Waiting List and Their Impact on Listing Outcome
Abstract
1. Background
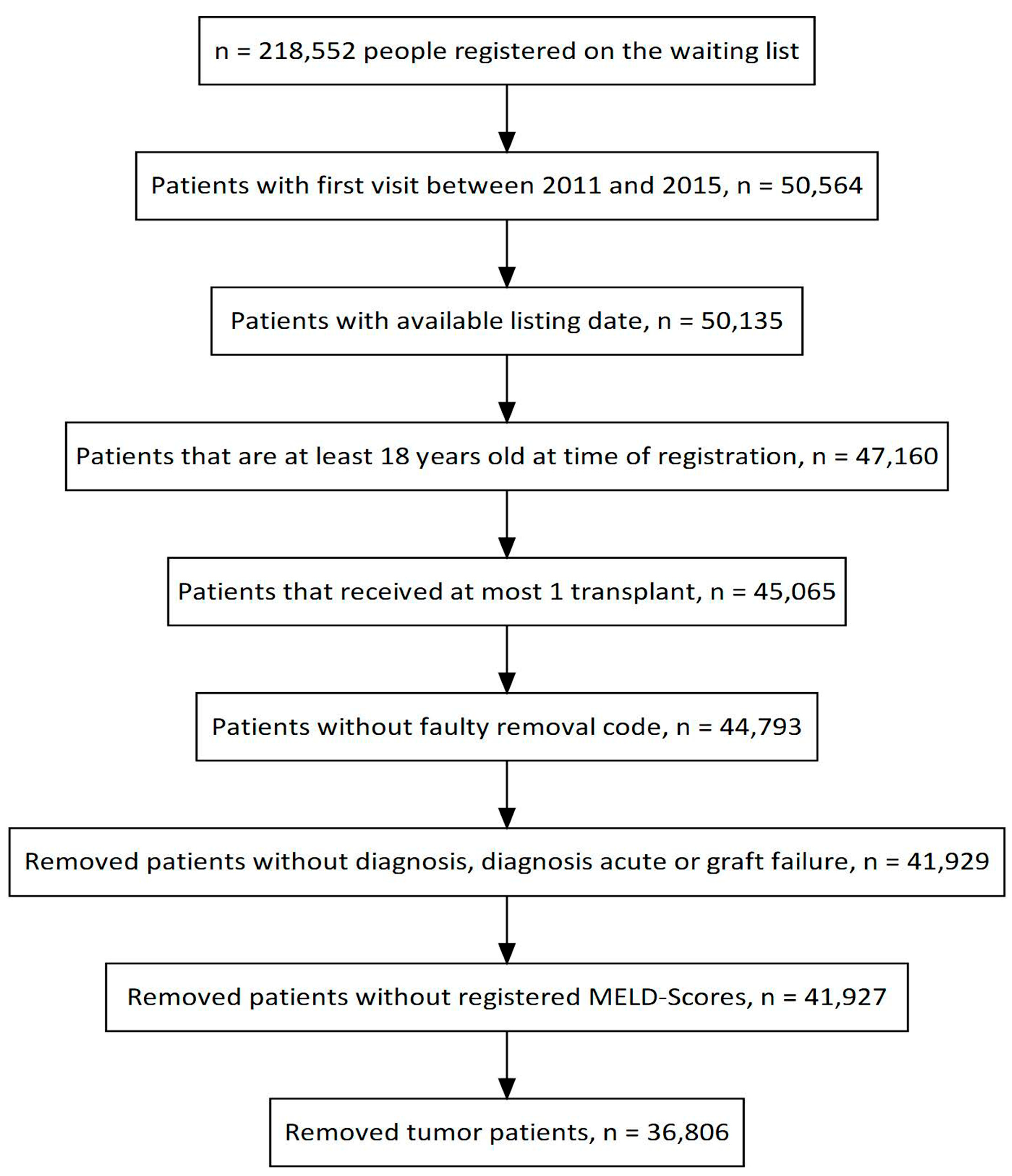
2. Methods
2.1. MELD Score Calculations
2.2. Statistics
3. Results
3.1. Waiting List Outcome
3.2. Waiting Time
3.3. MELD-Na Assessments
3.4. Meld-Na Values
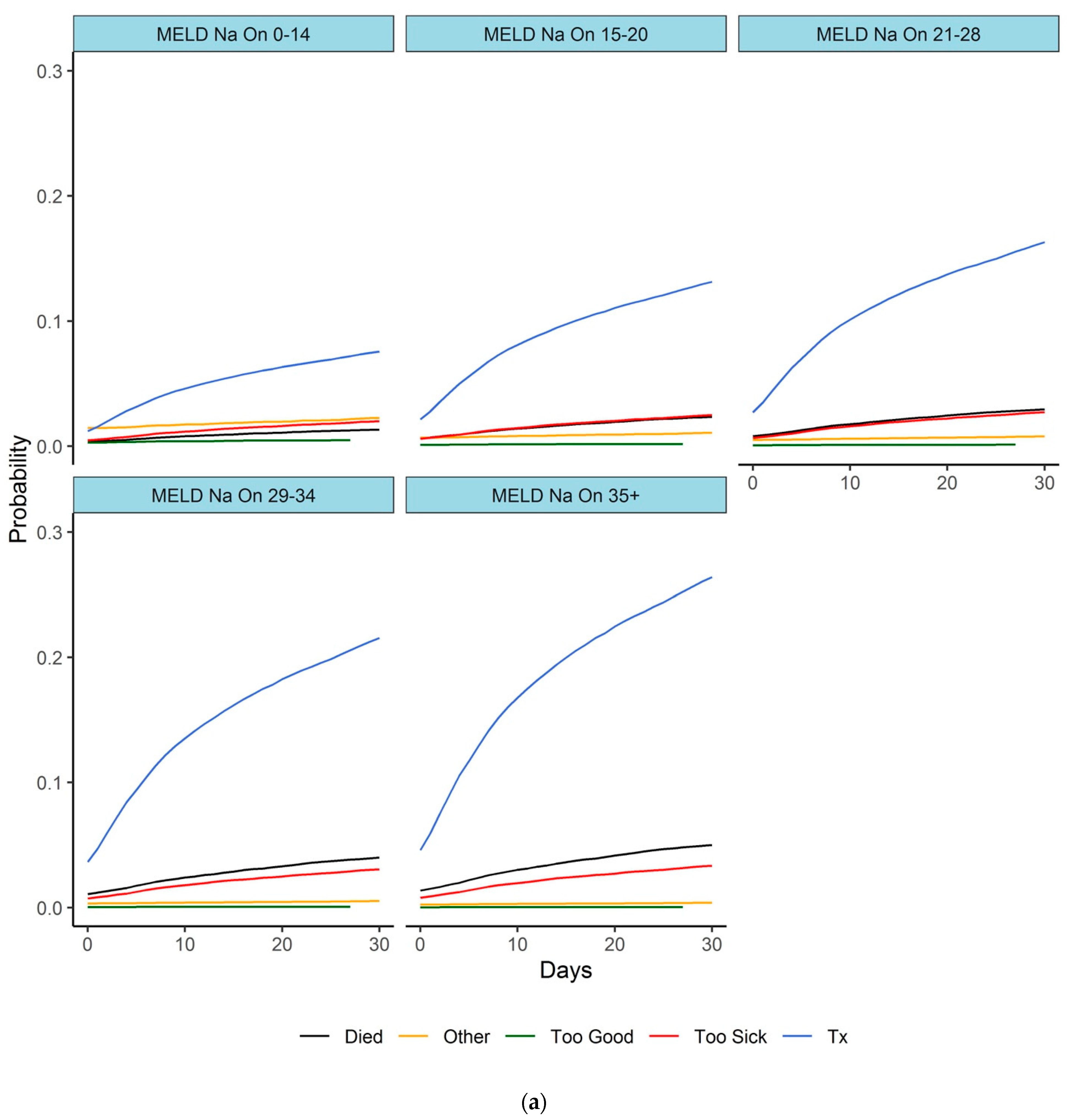
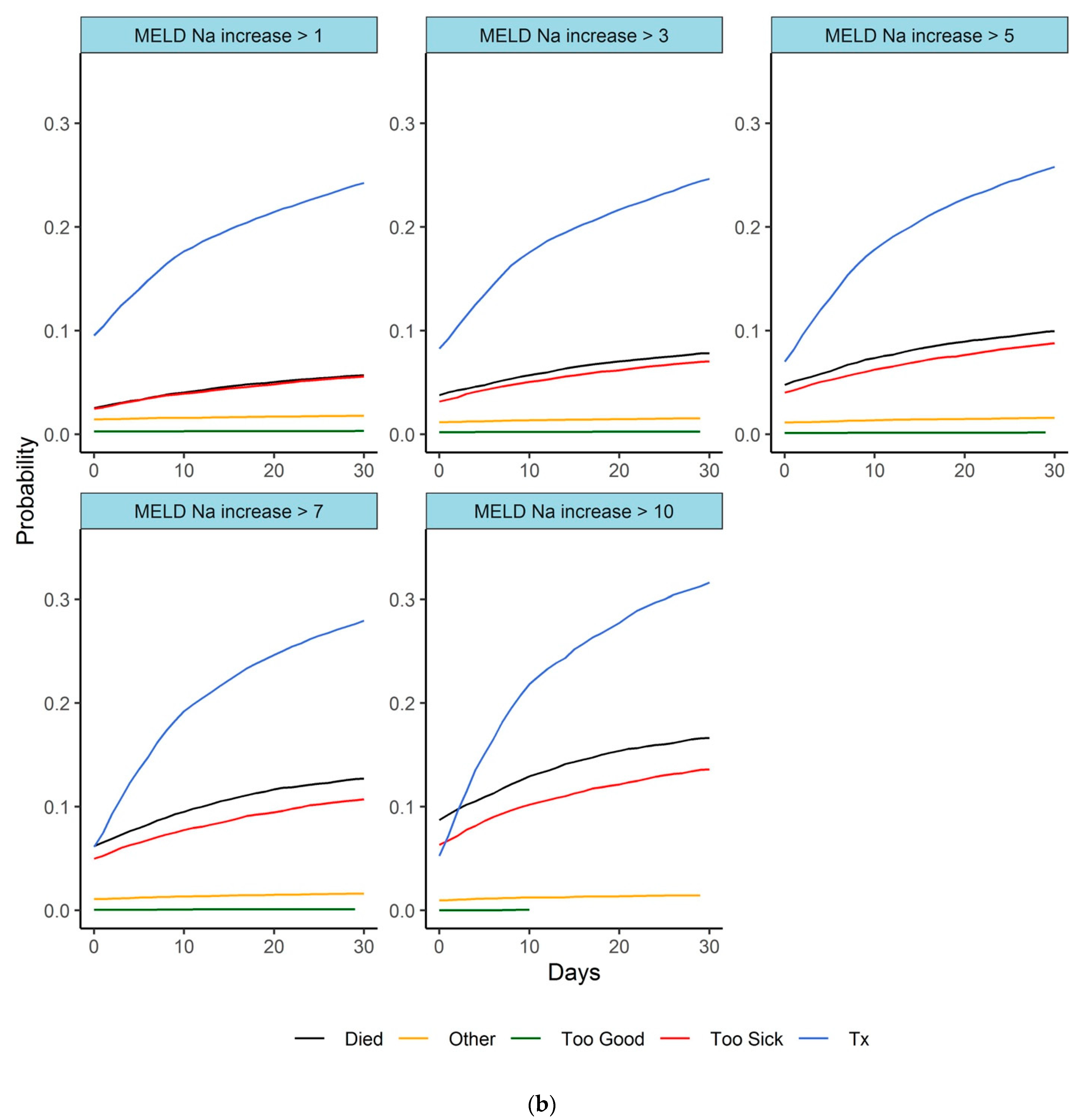
3.5. Subgroup Short Waiting Time (<30 Days)
3.6. Indications and MELD-Na Dynamics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MELD | model for end-stage liver disease |
| Delta MELD | dynamic MELD deterioration |
| Na | Sodium |
| TX | Transplantation |
| DOL | Died on list |
| UNOS | United Network of Organ Sharing |
References
- Wiesner, R.; Edwards, E.; Freeman, R.; Harper, A.; Kim, R.; Kamath, P.; Kremers, W.; Lake, J.; Howard, T.; Merion, R.M.; et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 2003, 124, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Wiesner, R.H.; McDiarmid, S.V.; Kamath, P.S.; Edwards, E.B.; Malinchoc, M.; Kremers, W.K.; Krom, R.A.; Kim, W.R. MELD and PELD: Application of survival models to liver allocation. Liver Transpl. 2001, 7, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Heuman, D.M.; Mihas, A.A.; Habib, A.; Gilles, H.S.; Stravitz, R.T.; Sanyal, A.J.; Fisher, R.A. MELD-XI: A rational approach to “sickest first” liver transplantation in cirrhotic patients requiring anticoagulant therapy. Liver Transpl. 2007, 13, 30–37. [Google Scholar] [CrossRef] [PubMed]
- De, A.; Singh, A.; Kumari, S.; Singh, V. Has the time come for using MELD-Sarcopenia score? J. Hepatol. 2018, 68, 1324. [Google Scholar] [CrossRef] [PubMed]
- Organ Procurement and Transplantation Network Liver and Intestine Committee. Allocation of Livers and Liverintestines. Effective 1 September 2018. Available online: https://optn.transplant.hrsa.gov/policies-bylaws/policies/ (accessed on 18 May 2023).
- Kim, W.R.; Biggins, S.W.; Kremers, W.K.; Wiesner, R.H.; Kamath, P.S.; Benson, J.T.; Edwards, E.; Therneau, T.M. Hyponatremia and mortality among patients on the liver-transplant waiting list. N. Engl. J. Med. 2008, 359, 1018–1026. [Google Scholar] [CrossRef] [PubMed]
- Nagai, S.; Chau, L.C.; Schilke, R.E.; Safwan, M.; Rizzari, M.; Collins, K.; Yoshida, A.; Abouljoud, M.S.; Moonka, D. Effects of Allocating Livers for Transplantation Based on Model for End-Stage Liver Disease-Sodium Scores on Patient Outcomes. Gastroenterology 2018, 155, 1451–1462.e1453. [Google Scholar] [CrossRef] [PubMed]
- Gyori, G.P.; Silberhumer, G.R.; Rahmel, A.; de Vries, E.; Soliman, T.; Zehetmayer, S.; Rogiers, X.; Berlakovich, G.A.; Eurotransplant. Impact of dynamic changes in meld score on survival after liver transplantation—A eurotransplant registry analysis. Liver Int. 2016, 36, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Gyori, G.P.; Silberhumer, G.R.; Zehetmayer, S.; Kern, B.; Hetz, H.; Soliman, T.; Steininger, R.; Muhlbacher, F.; Berlakovich, G.A. Dynamic changes in MELD score not only predict survival on the waiting list but also overall survival after liver transplantation. Transpl. Int. 2012, 25, 935–940. [Google Scholar] [CrossRef] [PubMed]
- Kamath, P.S.; Wiesner, R.H.; Malinchoc, M.; Kremers, W.; Therneau, T.M.; Kosberg, C.L.; D’Amico, G.; Dickson, E.R.; Kim, W.R. A model to predict survival in patients with end-stage liver disease. Hepatology 2001, 33, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Silberhumer, G.R.; Hetz, H.; Rasoul-Rockenschaub, S.; Peck-Radosavljevic, M.; Soliman, T.; Steininger, R.; Muehlbacher, F.; Berlakovich, G.A. Is MELD score sufficient to predict not only death on waiting list, but also post-transplant survival? Transpl. Int. 2006, 19, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Bambha, K.; Kim, W.R.; Kremers, W.K.; Therneau, T.M.; Kamath, P.S.; Wiesner, R.; Rosen, C.B.; Thostenson, J.; Benson, J.T.; Dickson, E.R. Predicting survival among patients listed for liver transplantation: An assessment of serial MELD measurements. Am. J. Transplant. 2004, 4, 1798–1804. [Google Scholar] [CrossRef] [PubMed]
- Merion, R.M.; Wolfe, R.A.; Dykstra, D.M.; Leichtman, A.B.; Gillespie, B.; Held, P.J. Longitudinal assessment of mortality risk among candidates for liver transplantation. Liver Transpl. 2003, 9, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.Y.; Ohri, N.; Kabarriti, R.; Aparo, S.; Chuy, J.; Goel, S.; Schwartz, J.M.; Kinkhabwala, M.; Kaubisch, A.; Guha, C. Model for End-Stage Liver Disease and Sodium Velocity Predicts Overall Survival in Nonmetastatic Hepatocellular Carcinoma Patients. Can. J. Gastroenterol. Hepatol. 2018, 2018, 5681979. [Google Scholar] [CrossRef] [PubMed]
- Xun, Y.H.; Shi, J.P.; Li, C.Q.; Li, D.; Shi, W.Z.; Pan, Q.C.; Guo, J.C.; Zang, G.Q. Prognostic performance of a series of model for end-stage liver disease and respective Delta scores in patients with hepatitis B acute-on-chronic liver failure. Mol. Med. Rep. 2014, 9, 1559–1568. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, V.; Moreau, R.; Jalan, R.; Gines, P.; Study, E.-C.C.C. Acute-on-chronic liver failure: A new syndrome that will re-classify cirrhosis. J. Hepatol. 2015, 62 (Suppl. 1), S131–S143. [Google Scholar] [CrossRef] [PubMed]
- Finkenstedt, A.; Nachbaur, K.; Zoller, H.; Joannidis, M.; Pratschke, J.; Graziadei, I.W.; Vogel, W. Acute-on-chronic liver failure: Excellent outcomes after liver transplantation but high mortality on the wait list. Liver Transpl. 2013, 19, 879–886. [Google Scholar] [CrossRef] [PubMed]
| DOL | Too Poor | Active | Too Good | TX | Other | ALL | |
|---|---|---|---|---|---|---|---|
| Alcoholic | 1323 (12.3) | 1162 (10.8) | 2251 (21.0) | 398 (3.7) | 4743 (44.2) | 862 (8.0) | 10,739 (100.0) |
| Biliary | 329 (11.5) | 262 (9.1) | 584 (20.4) | 66 (2.3) | 1540 (53.7) | 87 (3.0) | 2868 (100.0) |
| Hepatitis | 1455 (11.1) | 1452 (11.1) | 2330 (17.8) | 337 (2.6) | 6682 (51.0) | 842 (6.4) | 13,098 (100.0) |
| Metabolic | 77 (10.8) | 56 (7.9) | 97 (13.7) | 8 (1.1) | 451 (63.4) | 22 (3.1) | 711 (100.0) |
| NASH | 744 (13.6) | 668 (12.2) | 1160 (21.2) | 98 (1.8) | 2538 (46.4) | 262 (4.8) | 5470 (100.0) |
| Other | 475 (12.1) | 485 (12.4) | 846 (21.6) | 143 (3.7) | 1762 (44.9) | 209 (5.3) | 3920 (100.0) |
| ALL | 4403 (12.0) | 4085 (11.1) | 7268 (19.7) | 1050 (2.9) | 17,716 (48.1) | 2284 (6.2) | 36,806 (100.0) |
| a. | |
| Indications | Waiting Time |
| Alcoholic | 152 (24:432) |
| Biliary | 192 (53:492) |
| Hepatitis | 183 (40:436) |
| Metabolic | 90 (10:310) |
| NASH | 168 (39:419) |
| Other | 147 (24:453) |
| b. | |
| MELD-Na ON | Waiting Time |
| <15 | 310 (122:600) |
| 15–20 | 270 (115:549) |
| 21–28 | 103 (34:267) |
| 30–34 | 17 (6:48) |
| 35> | 5 (2:12) |
| c. | |
| Outcome | Waiting Time |
| TX | 90 (16:260) |
| Too sick | 144 (34:363) |
| DOL | 123 (28:344) |
| Active | 469 (217:908) |
| Too good | 531 (277:868) |
| Other | 256 (91:513) |
| Number of Patients | MELD-Na ON | MELD-Na OFF | Delta | Delta Max | Delta Last | |
|---|---|---|---|---|---|---|
| TX | 17,716 | 21.6 ± 9.1 | 24.6 ± 9.8 | 3.0 ± 6.3 | 6.6 ± 6.1 | −0.3 ± 3.9 |
| Too sick | 4085 | 21.5 ± 8.5 | 27.6 ± 10.1 | 6.1 ± 8.0 | 9.3 ± 7.3 | 2.0 ± 5.7 |
| DOL | 4403 | 22.5 ± 8.0 | 29.3 ± 9.1 | 6.8 ± 8.4 | 10.0 ± 7.6 | 2.8 ± 6.4 |
| active | 7268 | 15.4 ± 5.2 | 15.3 ± 5.7 | −0.1 ± 5.2 | 6.7 ± 5.1 | −0.2 ± 3.5 |
| Too good | 1050 | 15.5 ± 6.3 | 12.3 ± 4.7 | −3.4 ± 5.8 | 6.7 ± 5.5 | −1.1 ± 3.9 |
| Other | 2284 | 16.9 ± 6.5 | 17.5 ± 7.3 | 0.6 ± 5.6 | 5.9 ± 5.1 | 0.5 ± 4.3 |
| All | 36,806 | 20.0 ± 8.5 | 22.9 ± 10.2 | 2.8 ± 7.0 | 7.3 ± 6.3 | 0.4 ± 4.6 |
| MELD-Na ON | MELD-Na OFF | Delta | Delta Max | Delta Last | ||
| Too sick | 0.2 | <0.01 | <0.01 | <0.01 | <0.01 | |
| DOL | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | |
| Too good | <0.01 | <0.01 | <0.01 | 0.8 | <0.01 |
| Number of Patients | MELD ON | MELD OFF | Delta | Delta Max | |
|---|---|---|---|---|---|
| TX | 5744 | 29.3 (8.8) | 30.1 (9.0) | 0.7 (4.3) | 3.4(3.8) |
| Too sick | 961 | 29.4 (9.5) | 31.8 (10.0) | 2.5 (5.2) | 4.0 (4.8) |
| DOL | 1117 | 29.7 (8.6) | 31.8 (9.1) | 2.1 (4.8) | 3.6 (4.6) |
| Too good | 62 | 18.1 (9.7) | 16.2 (8.2) | −1.9 (4.7) | 2.9 (5.0) |
| active | 716 | 12.1 (4.7) | 12.1 (4.7) | 0.0 (0.9) | 0.1 (0.9) |
| other | 313 | 18.5 (9.0) | 18.5 (8.9) | 0.0 (2.4) | 1.3 (2.5) |
| All | 8913 | 27.5 (10.0) | 28.5 (10.4) | 1.0 (4.3) | 3.1 (4.0) |
| MELD-Na ON | MELD-Na OFF | Delta | Delta Max | ||
| Too sick | 1 | <0.01 | <0.01 | <0.01 | |
| DOL | 0.2 | <0.01 | 0.2 | <0.01 |
| MELD ON | MELD OFF | Delta | Delta Max | Delta Last | |
|---|---|---|---|---|---|
| Alcoholic | 22.1 (8.5) | 23.8 (10.0) | 1.7 (6.8) | 7.1 (5.9) | 0.1 (4.5) |
| Biliary | 19.2 (7.9) | 23.5 (10.0) | 4.3 (7.6) | 8.9 (6.9) | 0.2 (4.8) |
| Hepatitis | 18.1 (8.3) | 21.0 (10.4) | 3.0 (6.9) | 6.8 (6.4) | 0.6 (4.6) |
| Metabolic | 22.0 (9.1) | 25.6 (7.1) | 3.5 (7.1) | 7.2 (6.5) | 0.1 (4.7) |
| NASH | 20.0 (7.7) | 23.8 (9.5) | 3.8 (7.0) | 7.9 (6.4) | 0.5 (4.6) |
| Other | 21.2 (8.5) | 24.2 (10.1) | 3.0 (7.3) | 7.8 (6.6) | 0.3 (4.5) |
| MELD-Na ON | MELD-Na OFF | Delta | Delta Max | Delta Last | |
| <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silberhumer, G.R.; Györi, G.; Brugger, J.; Baumann, L.; Zehetmayer, S.; Soliman, T.; Berlakovich, G. MELD-Na Alterations on the Liver Transplant Waiting List and Their Impact on Listing Outcome. J. Clin. Med. 2023, 12, 3763. https://doi.org/10.3390/jcm12113763
Silberhumer GR, Györi G, Brugger J, Baumann L, Zehetmayer S, Soliman T, Berlakovich G. MELD-Na Alterations on the Liver Transplant Waiting List and Their Impact on Listing Outcome. Journal of Clinical Medicine. 2023; 12(11):3763. https://doi.org/10.3390/jcm12113763
Chicago/Turabian StyleSilberhumer, Gerd R., Georg Györi, Jonas Brugger, Lukas Baumann, Sonja Zehetmayer, Thomas Soliman, and Gabriela Berlakovich. 2023. "MELD-Na Alterations on the Liver Transplant Waiting List and Their Impact on Listing Outcome" Journal of Clinical Medicine 12, no. 11: 3763. https://doi.org/10.3390/jcm12113763
APA StyleSilberhumer, G. R., Györi, G., Brugger, J., Baumann, L., Zehetmayer, S., Soliman, T., & Berlakovich, G. (2023). MELD-Na Alterations on the Liver Transplant Waiting List and Their Impact on Listing Outcome. Journal of Clinical Medicine, 12(11), 3763. https://doi.org/10.3390/jcm12113763







