Role of Statins after Endovascular Repair of Abdominal Aortic Aneurysms: A Nationwide Population-Based Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
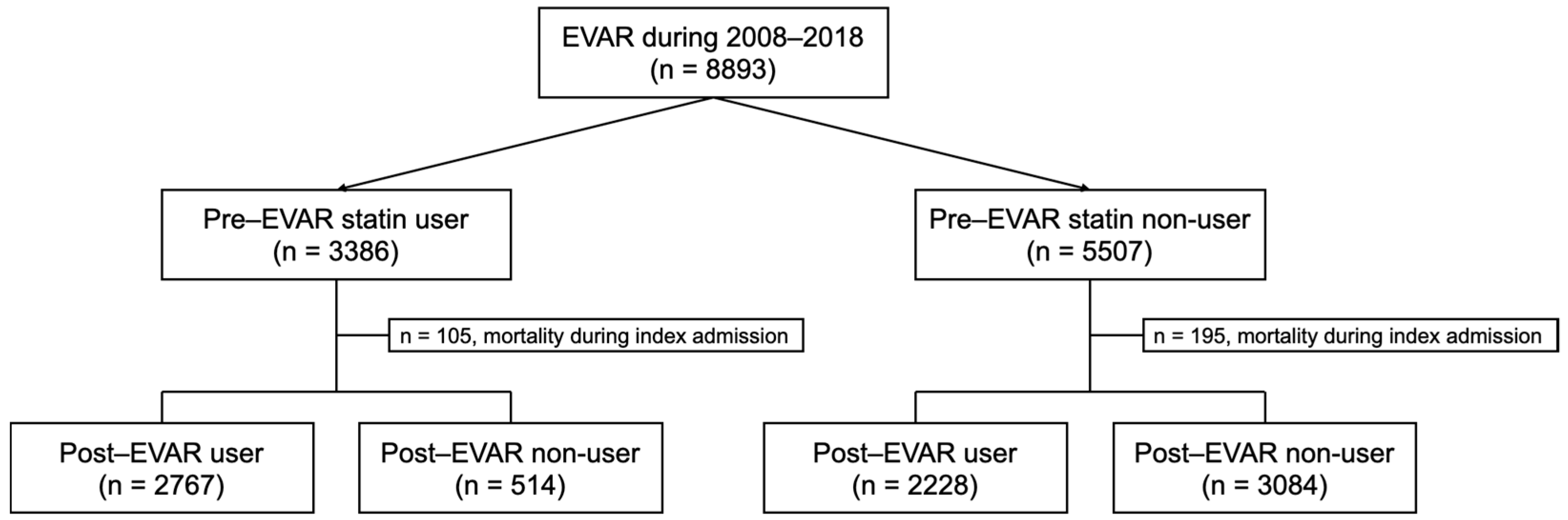
2.2. Study Population
2.3. Definition of Variables and Outcomes
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Outcomes According to Pre-Treatment Statin Use
3.3. Outcomes According to Post-Operative Statin Use
3.4. Subgroup Analysis
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Volodos, N.L.; Shekhanin, V.E.; Karpovich, I.P.; Troian, V.I.; Gur’ev Iu, A. A self-fixing synthetic blood vessel endoprosthesis. Vestn. Khir Im. II Grek. 1986, 137, 123–125. [Google Scholar]
- Parodi, J.C.; Palmaz, J.C.; Barone, H.D. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann. Vasc. Surg. 1991, 5, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Zhang, S.; Zhang, J.; Ji, C.; Eckstein, H.H. Outcomes of Endovascular Abdominal Aortic Aneurysm Repair in Octogenarians: Meta-analysis and Systematic Review. Eur. J. Vasc. Endovasc. Surg. 2017, 54, 454–463. [Google Scholar] [CrossRef]
- Ho, V.T.; Rothenberg, K.A.; George, E.L.; Lee, J.T.; Stern, J.R. Female sex is independently associated with in-hospital mortality after endovascular aortic repair for ruptured aortic aneurysm. Ann. Vasc. Surg. 2022, 81, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Khashram, M.; Williman, J.A.; Hider, P.N.; Jones, G.T.; Roake, J.A. Systematic Review and Meta-analysis of Factors Influencing Survival Following Abdominal Aortic Aneurysm Repair. Eur. J. Vasc. Endovasc. Surg. 2016, 51, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, A.; Laufs, U.; Liao, J.K. Pleiotropic Effects of Statins on the Cardiovascular System. Circ. Res. 2017, 120, 229–243. [Google Scholar] [CrossRef]
- Cholesterol Treatment Trialists, C.; Baigent, C.; Blackwell, L.; Emberson, J.; Holland, L.E.; Reith, C.; Bhala, N.; Peto, R.; Barnes, E.H.; Keech, A.; et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010, 376, 1670–1681. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e1082–e1143. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Pini, R.; Faggioli, G.; Mascoli, C.; Gallitto, E.; Freyrie, A.; Gargiulo, M.; Stella, A. Influence of statin therapy on type 2 endoleak evolution. Ann. Vasc. Surg. 2015, 29, 1167–1173. [Google Scholar] [CrossRef]
- Twine, C.P.; Williams, I.M. Systematic review and meta-analysis of the effects of statin therapy on abdominal aortic aneurysms. Br. J. Surg. 2011, 98, 346–353. [Google Scholar] [CrossRef]
- Giles, K.A.; Schermerhorn, M.L.; O’Malley, A.J.; Cotterill, P.; Jhaveri, A.; Pomposelli, F.B.; Landon, B.E. Risk prediction for perioperative mortality of endovascular vs open repair of abdominal aortic aneurysms using the Medicare population. J. Vasc. Surg. 2009, 50, 256–262. [Google Scholar] [CrossRef]
- Wilt, T.J.; Bloomfield, H.E.; MacDonald, R.; Nelson, D.; Rutks, I.; Ho, M.; Larsen, G.; McCall, A.; Pineros, S.; Sales, A. Effectiveness of statin therapy in adults with coronary heart disease. Arch. Intern. Med. 2004, 164, 1427–1436. [Google Scholar] [CrossRef]
- London, M.J.; Schwartz, G.G.; Hur, K.; Henderson, W.G. Association of Perioperative Statin Use with Mortality and Morbidity After Major Noncardiac Surgery. JAMA Intern. Med. 2017, 177, 231–242. [Google Scholar] [CrossRef]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77. [Google Scholar] [CrossRef]
- Leurs, L.J.; Visser, P.; Laheij, R.J.; Buth, J.; Harris, P.L.; Blankensteijn, J.D. Statin use is associated with reduced all-cause mortality after endovascular abdominal aortic aneurysm repair. Vascular 2006, 14, 1–8. [Google Scholar] [CrossRef]
- Xiong, X.; Wu, Z.; Qin, X.; Huang, Q.; Wang, X.; Qin, J.; Lu, X. Meta-analysis suggests statins reduce mortality after abdominal aortic aneurysm repair. J. Vasc. Surg. 2022, 75, 356–362. [Google Scholar] [CrossRef]
- Toth, P.P.; Granowitz, C.; Hull, M.; Anderson, A.; Philip, S. Long-term statin persistence is poor among high-risk patients with dyslipidemia: A real-world administrative claims analysis. Lipids Health Dis. 2019, 18, 175. [Google Scholar] [CrossRef]
- Booth, J.N., 3rd; Colantonio, L.D.; Chen, L.; Rosenson, R.S.; Monda, K.L.; Safford, M.M.; Kilgore, M.L.; Brown, T.M.; Taylor, B.; Dent, R.; et al. Statin Discontinuation, Reinitiation, and Persistence Patterns Among Medicare Beneficiaries After Myocardial Infarction: A Cohort Study. Circ. Cardiovasc. Qual. Outcomes 2017, 10, e003626. [Google Scholar] [CrossRef]
- Nakayama, A.; Morita, H.; Miyata, T.; Hoshina, K.; Nagayama, M.; Takanashi, S.; Sumiyoshi, T.; Komuro, I.; Nagai, R. Predictors of mortality after emergency or elective repair of abdominal aortic aneurysm in a Japanese population. Heart Vessels 2014, 29, 65–70. [Google Scholar] [CrossRef]
- Sun, T.; Zhang, H.; Cheng, Y.; Wang, S.; Tao, Y.; Zhang, D.; Huang, J.; Zhang, J.; Li, Z. A two-year follow-up for Chinese patients with abdominal aortic aneurysm undergoing open/endovascular repair. Chin. Med. J. 2014, 127, 457–461. [Google Scholar]
- Liao, K.M.; Wang, S.W.; Lu, C.H.; Chen, C.Y.; Huang, Y.B. The influence of statins on aortic aneurysm after operation: A retrospective nationwide study. Medicine 2019, 98, e15368. [Google Scholar] [CrossRef]
- Debono, S.; Nash, J.; Tambyraja, A.L.; Newby, D.E.; Forsythe, R.O. Endovascular repair for abdominal aortic aneurysms. Heart 2021, 107, 1783–1789. [Google Scholar] [CrossRef] [PubMed]
- Alshaikh, H.N.; Bohsali, F.; Gani, F.; Nejim, B.; Malas, M. Statin intensity and postoperative mortality following open repair of intact abdominal aortic aneurysm. BJS Open. 2018, 2, 411–418. [Google Scholar] [CrossRef]

| Pre-EVAR Statin User (n = 3121) | Pre-EVAR Statin Non-User (n = 3121) | SMD | p-Value 1 | |
|---|---|---|---|---|
| Age (years ± SD) | 72.9 ± 7.7 | 73.0 ± 8.7 | 0.003 | 0.905 |
| Sex (male, n (%)) | 2585 (82.8) | 2573 (82.4) | 0.010 | 0.689 |
| MPRS | 6.5 ± 6.0 | 6.5 ± 6.0 | 0.027 | 0.993 |
| Low risk | 1075 (34.4) | 1062 (34.0) | ||
| Intermediate risk | 1432 (45.9) | 1475 (47.3) | ||
| High risk | 614 (19.7) | 584 (18.7) | ||
| Comorbidities | ||||
| Hypertension | 2729 (87.4) | 2753 (88.2) | 0.024 | 0.353 |
| Diabetes mellitus | 675 (21.6) | 645 (20.7) | 0.024 | 0.304 |
| Heart failure | 614 (19.7) | 582 (18.6) | 0.026 | 0.304 |
| Ischemic heart disease | 1616 (51.8) | 1599 (51.2) | 0.011 | 0.667 |
| Myocardial infarction | 423 (13.6) | 259 (8.3) | 0.169 | <0.001 |
| Atrial fibrillation | 253 (8.1) | 247 (7.9) | 0.007 | 0.780 |
| COPD | 391 (12.5) | 375 (12.0) | 0.016 | 0.537 |
| Peripheral artery disease | 454 (14.5) | 472 (15.1) | 0.016 | 0.522 |
| Chronic kidney disease | 77 (2.5) | 80 (2.6) | 0.006 | 0.808 |
| Cerebrovascular disease | 845 (27.1) | 852 (27.3) | 0.005 | 0.842 |
| Pre-EVAR Statin User (n = 3121) | Pre-EVAR Statin Non-User (n = 3121) | HR | 95% CI | p-Value | |||
|---|---|---|---|---|---|---|---|
| No. of Events | Incidence Rate 1 | No. of Events | Incidence Rate 1 | ||||
| 30-day mortality | 82 | 2.7 | 71 | 2.3 | 1.15 | (0.84–1.58) | 0.376 |
| Overall mortality | 985 | 83.9 | 1104 | 98.9 | 0.85 | (0.78–0.92) | <0.001 |
| Cardiovascular mortality | 95 | 8.1 | 132 | 11.8 | 0.66 | (0.51–0.86) | 0.002 |
| Reintervention | 223 | 19.8 | 238 | 22.3 | 0.89 | (0.74–1.06) | 0.189 |
| Myocardial infarction | 61 | 5.3 | 62 | 5.6 | 0.85 | (0.60–1.20) | 0.362 |
| Major bleeding | 99 | 8.6 | 99 | 9.0 | 0.95 | (0.72–1.25) | 0.697 |
| Any stroke | 434 | 39.8 | 421 | 40.4 | 1.01 | (0.88–1.15) | 0.915 |
| Hemorrhagic stroke | 105 | 9.1 | 123 | 11.1 | 0.83 | (0.64–1.07) | 0.147 |
| Ischemic stroke | 340 | 30.8 | 299 | 28.4 | 1.12 | (0.95–1.30) | 0.171 |
| Pre- and Post-User (n = 2767) | Pre-User But Post-Non-User (n = 514) | Pre-Non-User But Post-User (n = 2228) | Pre- and Post-Non-User (n = 3084) | p-Value 1 | |
|---|---|---|---|---|---|
| Age (years ± SD) | 72.7 ± 7.7 | 72.7 ± 7.6 | 72.8 ± 8.3 | 73.0 ± 9.2 | 0.905 |
| Sex (male, n (%)) | 2309 (83.4) | 420 (81.7) | 1896 (85.1) | 2594 (84.1) | 0.689 |
| MPRS | 6.6 ± 6.0 | 6.1 ± 5.8 | 5.8 ± 5.7 | 6.0 ± 5.8 | 0.993 |
| Low risk | 935 (33.8) | 187 (36.4) | 861 (38.6) | 1176 (38.1) | |
| Intermediate risk | 1283 (46.4) | 239 (46.5) | 1035 (46.5) | 1427 (46.3) | |
| High risk | 549 (19.8) | 88 (17.1) | 332 (14.9) | 481 (15.6) | |
| Comorbidities | |||||
| Hypertension | 2450 (88.5) | 446 (86.8) | 1643 (73.7) | 2155 (69.9) | 0.353 |
| Diabetes mellitus | 681 (24.6) | 130 (25.3) | 343 (15.4) | 394 (12.8) | 0.304 |
| Heart failure | 607 (21.9) | 96 (18.7) | 295 (13.2) | 395 (12.8) | 0.304 |
| IHD | 1556 (56.2) | 259 (50.4) | 893 (40.1) | 900 (29.2) | 0.667 |
| MI | 399 (14.4) | 64 (12.5) | 157 (7.0) | 143 (4.6) | <0.001 |
| Atrial fibrillation | 236 (8.5) | 45 (8.8) | 133 (6.0) | 209 (6.8) | 0.780 |
| COPD | 341 (12.3) | 66 (12.8) | 271 (12.2) | 423 (13.7) | 0.537 |
| PAD | 414 (15.0) | 68 (13.2) | 316 (14.2) | 427 (13.8) | 0.522 |
| CKD | 69 (2.5) | 8 (1.6) | 37 (1.7) | 63 (2.0) | 0.808 |
| CVD | 761 (27.5) | 173 (33.7) | 458 (20.6) | 623 (20.20) | 0.842 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, G.C.; Lee, K.Y.; Choo, E.H.; Hwang, B.-H.; Chung, W.S.; You, S.-J.; Jeon, J.; Kwon, S.; Chang, K. Role of Statins after Endovascular Repair of Abdominal Aortic Aneurysms: A Nationwide Population-Based Study. J. Clin. Med. 2023, 12, 3737. https://doi.org/10.3390/jcm12113737
Oh GC, Lee KY, Choo EH, Hwang B-H, Chung WS, You S-J, Jeon J, Kwon S, Chang K. Role of Statins after Endovascular Repair of Abdominal Aortic Aneurysms: A Nationwide Population-Based Study. Journal of Clinical Medicine. 2023; 12(11):3737. https://doi.org/10.3390/jcm12113737
Chicago/Turabian StyleOh, Gyu Chul, Kwan Yong Lee, Eun Ho Choo, Byung-Hee Hwang, Wook Sung Chung, So-Jeong You, JinKyung Jeon, Sol Kwon, and Kiyuk Chang. 2023. "Role of Statins after Endovascular Repair of Abdominal Aortic Aneurysms: A Nationwide Population-Based Study" Journal of Clinical Medicine 12, no. 11: 3737. https://doi.org/10.3390/jcm12113737
APA StyleOh, G. C., Lee, K. Y., Choo, E. H., Hwang, B.-H., Chung, W. S., You, S.-J., Jeon, J., Kwon, S., & Chang, K. (2023). Role of Statins after Endovascular Repair of Abdominal Aortic Aneurysms: A Nationwide Population-Based Study. Journal of Clinical Medicine, 12(11), 3737. https://doi.org/10.3390/jcm12113737





