Differences between Novice and Expert Raters Assessing Trunk Control Using the Trunk Control Measurement Scale Spanish Version (TCMS-S) in Children with Cerebral Palsy
Abstract
1. Introduction
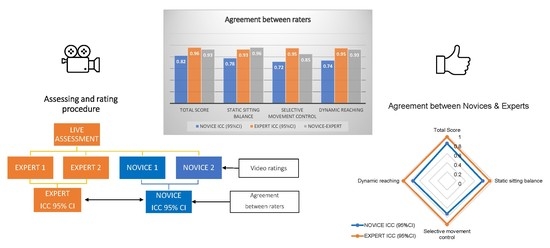
2. Materials and Methods
2.1. Study Design, Setting and Participants
2.2. Trunk Control Measurement Scale-S
2.3. Study Procedures
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child. Neurol. Suppl. 2007, 109, 8–14. [Google Scholar]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.-C.; et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Gorter, J.W.; Rosenbaum, P.L.; Hanna, S.E.; Palisano, R.J.; Bartlett, D.J.; Russell, D.J.; Walter, S.D.; Raina, P.; Galuppi, B.E.; Wood, E. Limb distribution, motor impairment, and functional classification of cerebral palsy. Dev. Med. Child Neurol. 2007, 46, 461–467. [Google Scholar] [CrossRef]
- Schiariti, V.; Mahdi, S.; Bölte, S. International Classification of Functioning, Disability and Health Core Sets for cerebral palsy, autism spectrum disorder, and attention-deficit–hyperactivity disorder. Dev. Med. Child Neurol. 2018, 60, 933–941. [Google Scholar] [CrossRef] [PubMed]
- Schiariti, V.; Longo, E.; Shoshmin, A.; Kozhushko, L.; Besstrashnova, Y.; Król, M.; Campos, T.N.C.; Ferreira, H.N.C.; Verissimo, C.; Shaba, D.; et al. Implementation of the international classification of functioning, disability, and health (ICF) core sets for children and youth with cerebral palsy: Global initiatives promoting optimal functioning. Int. J. Environ. Res. Public Health 2018, 15, 1899. [Google Scholar] [CrossRef] [PubMed]
- Jackman, M.; Sakzewski, L.; Morgan, C.; Boyd, R.N.; Brennan, S.E.; Langdon, K.; Toovey, R.A.M.; Greaves, S.; Thorley, M.; Novak, I. Interventions to improve physical function for children and young people with cerebral palsy: International clinical practice guideline. Dev. Med. Child Neurol. 2021, 64, 536–549. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Mc Namara, M.; Paton, M.C.; Popat, H.; et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef]
- Brogren, E.; Hadders-Algra, M. Postural dysfunction in children with cerebral palsy: Some implications for therapeutic guidance. Neural. Plast. 2005, 12, 640328. [Google Scholar] [CrossRef]
- van Balen, L.C.; Dijkstra, L.J.; Hadders-Algra, M. Development of postural adjustments during reaching in typically developing infants from 4 to 18 months. Exp. Brain Res. 2012, 220, 109–119. [Google Scholar] [CrossRef]
- Saether, R.; Helbostad, J.L.; Adde, L.; Braendvik, S.; Lydersen, S.; Vik, T.; Sæther, R.; Brændvik, S. The relationship between trunk control in sitting and during gait in children and adolescents with cerebral palsy. Dev. Med. Child Neurol. 2015, 57, 344–350. [Google Scholar] [CrossRef]
- Kallem Seyyar, G.; Aras, B.; Aras, O. Trunk control and functionality in children with spastic cerebral palsy. Dev. Neurorehabilit. 2019, 22, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Marsico, P.; Mitteregger, E.; Balzer, J.; van Hedel, H.J.A. The Trunk Control Measurement Scale: Reliability and discriminative validity in children and young people with neuromotor disorders. Dev. Med. Child Neurol. 2017, 59, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Wallard, L.; Bril, B.; Dietrich, G.; Kerlirzin, Y.; Bredin, J. The role of head stabilization in locomotion in children with cerebral palsy. Ann. Phys. Rehabil. Med. 2012, 55, 590–600. [Google Scholar] [CrossRef] [PubMed]
- Wallard, L.; Dietrich, G.; Kerlirzin, Y.; Bredin, J. Balance control in gait children with cerebral palsy. Gait Posture 2014, 40, 43–47. [Google Scholar] [CrossRef]
- Pierret, J.; Caudron, S.; Paysant, J.; Beyaert, C. Impaired postural control of axial segments in children with cerebral palsy. Gait Posture 2021, 86, 266–272. [Google Scholar] [CrossRef]
- Pierret, J.; Beyaert, C.; Vasa, R.; Rumilly, E.; Paysant, J.; Caudron, S. Rehabilitation of Postural Control and Gait in Children with Cerebral Palsy: The Beneficial Effects of Trunk-Focused Postural Activities. Dev. Neurorehabil. 2023, 26, 180–192. [Google Scholar] [CrossRef]
- Talgeri, A.J.; Nayak, A.; Karnad, S.D.; Jain, P.; Tedla, J.S.; Reddy, R.S.; Sangadala, D.R. Effect of Trunk Targeted Interventions on Functional Outcomes in Children with Cerebral Palsy—A Systematic Review. Dev. Neurorehabil. 2023, 26, 193–205. [Google Scholar] [CrossRef]
- Heyrman, L.; Molenaers, G.; Desloovere, K.; Verheyden, G.; De Cat, J.; Monbaliu, E.; Feys, H. A clincal tool to measure trunk control in children with cerebral palsy: The trunk Control Measurement Scale. Res. Dev. Disabil. 2011, 32, 2624–2635. [Google Scholar] [CrossRef]
- Mitteregger, E.; Marsico, P.; Balzer, J.; van Hedel, H.J.A. Translation and construct validity of the Trunk Control Measurement Scale in children and youths with brain lesions. Res. Dev. Disabil. 2015, 45–46, 343–352. [Google Scholar] [CrossRef]
- Jeon, J.-Y.; Shin, W.-S. Reliability and validity of the Korean version of the Trunk Control Measurement Scale (TCMS-K) for children with cerebral palsy. Res. Dev. Disabil. 2014, 35, 581–590. [Google Scholar] [CrossRef]
- Ozal, C.; Ari, G.; Gunel, M.K. Inter–intra observer reliability and validity of the Turkish version of Trunk Control Measurement Scale in children with cerebral palsy. Acta Orthop. Traumatol. Turc. 2019, 53, 381–384. [Google Scholar] [CrossRef] [PubMed]
- Ravizzotti, E.; Vercelli, S.; Pellicciari, L.; Furmanek, M.P.; Zagnoni, G.; Piscitelli, D. Reliability and Validity of the Trunk Control Measurement Scale Among Children and Adolescents With Cerebral Palsy in Tanzania. Percept. Mot. Ski. 2020, 128, 731–745. [Google Scholar] [CrossRef] [PubMed]
- Desloovere, K.; Heyrman, L. Trunk control in children with cerebral palsy: Where are we now? Dev. Med. Child Neurol. 2015, 57, 310–311. [Google Scholar] [CrossRef] [PubMed]
- Heo, J.-Y.; Shin, H.-K. Reliability analysis of the Korean version of the trunk control measurement scale in cerebral palsy. J. Phys. Ther. Sci. 2018, 30, 1–4. [Google Scholar] [CrossRef]
- López-Ruiz, J.; Estrada-Barranco, C.; Martín-Gómez, C.; Egea-Gámez, R.M.; Valera-Calero, J.A.; Martín-Casas, P.; López-De-Uralde-Villanueva, I. Trunk Control Measurement Scale (TCMS): Psychometric Properties of Cross-Cultural Adaptation and Validation of the Spanish Version. Int. J. Environ. Res. Public Health 2023, 20, 5144. [Google Scholar] [CrossRef]
- Franki, I.; Van den Broeck, C.; De Cat, J.; Molenaers, G.; Vanderstraeten, G.; Desloovere, K. A study of whether video scoring is a reliable option for blinded scoring of the Gross Motor Function Measure-88. Clin. Rehabil. 2015, 29, 809–815. [Google Scholar] [CrossRef]
- Carballo-Fazanes, A.; Rey, E.; Valentini, N.C.; Rodríguez-Fernández, J.E.; Varela-Casal, C.; Rico-Díaz, J.; Barcala-Furelos, R.; Abelairas-Gómez, C. Intra-Rater (Live vs. Video Assessment) and Inter-Rater (Expert vs. Novice) Reliability of the Test of Gross Motor Development-Third Edition. Int. J. Environ. Res. Public Health 2021, 18, 1652. [Google Scholar] [CrossRef]
- Palmer, K.K.; Brian, A. Test of Gross Motor Development-2 Scores Differ Between Expert and Novice Coders. J. Mot. Learn. Dev. 2016, 4, 142–151. [Google Scholar] [CrossRef]
- Kuo, K.T.; Hunter, B.C.; Obayashi, M.; Lider, J.; Teramoto, M.; Cortez, M.; Hansen, C. Novice vs. expert inter-rater reliability of the balance error scoring system in children between the ages of 5 and 14. Gait Posture 2021, 86, 13–16. [Google Scholar] [CrossRef]
- Haakonsen Dahl, S.S.; Jørgensen, L. Intra- and Inter-Rater Reliability of the Mini-Balance Evaluation Systems Test in Individuals with Stroke. Int. J. Phys. Med. Rehabil. 2013, 2, 1. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Prinsen, C.A.C.; Bouter, L.M.; de Vet, H.C.W.; Terwee, C.B. The COnsensus-based standards for the selection of health measurement INstruments (COSMIN) and how to select an outcome measurement instrument. Braz. J. Phys. Ther. 2016, 20, 105–113. [Google Scholar] [CrossRef]
- Shrout, P.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- López-De-Uralde-Villanueva, I.; Acuyo-Osorio, M.; Prieto-Aldana, M.; La Touche, R. Reliability and minimal detectable change of a modified passive neck flexion test in patients with chronic nonspecific neck pain and asymptomatic subjects. Musculoskelet. Sci. Pract. 2017, 28, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Ramiscal, L.S.; Bolgla, L.A.; Cook, C.E.; Magel, J.S.; Parada, S.A.; Chong, R. Reliability of the scapular dyskinesis test yes-no classification in asymptomatic individuals between students and expert physical therapists. Clin. Shoulder Elb. 2022, 25, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.M.; Carlin, J.B.; Reddihough, D.S. Using the Gross Motor Function Classification System to describe patterns of motor severity in cerebral palsy. Dev. Med. Child Neurol. 2011, 53, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Heyrman, L.; Desloovere, K.; Molenaers, G.; Verheyden, G.; Klingels, K.; Monbaliu, E.; Feys, H. Clinical characteristics of impaired trunk control in children with spastic cerebral palsy. Res. Dev. Disabil. 2013, 34, 327–334. [Google Scholar] [CrossRef]
- Balzer, J.; Marsico, P.; Mitteregger, E.; Van Der Linden, M.L.; Mercer, T.H.; van Hedel, H.J.A. Influence of trunk control and lower extremity impairments on gait capacity in children with cerebral palsy. Disabil. Rehabil. 2018, 40, 3164–3170. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.; Kim, M. Reliability and responsiveness of the gross motor function measure-88 in children with cerebral palsy. Phys. Ther. 2013, 93, 393–400. [Google Scholar] [CrossRef]
- Nordmark, E.; Hägglund, G.; Jarnlo, G.B. Reliability of the gross motor function measure in cerebral palsy. Scand. J. Rehabil. Med. 1997, 29, 25–28. [Google Scholar]
- Kwon, Y.; Kim, J.-W.; Heo, J.-H.; Jeon, H.-M.; Choi, E.-B.; Eom, G.-M. The effect of sitting posture on the loads at cervico-thoracic and lumbosacral joints. Technol. Health Care 2018, 26, 409–418. [Google Scholar] [CrossRef]
- Krumlinde-Sundholm, L.; Holmefur, M.; Kottorp, A.; Eliasson, A.-C. The Assisting Hand Assessment: Current evidence of validity, reliability, and responsiveness to change. Dev. Med. Child Neurol. 2007, 49, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Holmefur, M.; Krumlinde-Sundholm, L.; Eliasson, A.-C. Interrater and intrarater reliability of the Assisting Hand Assessment. Am. J. Occup. Ther. 2007, 61, 79–84. [Google Scholar] [CrossRef]
- Romeo, D.M.; Ricci, D.; Brogna, C.; Mercuri, E. Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: A critical review of the literature. Dev. Med. Child Neurol. 2016, 58, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Dewar, R.; Claus, A.P.; Tucker, K.; Ware, R.; Johnston, L.M. Reproducibility of the Balance Evaluation Systems Test (BESTest) and the Mini-BESTest in school-aged children. Gait Posture 2017, 55, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Ferre-Fernández, M.P.; Murcia-González, M.A.P.; Ríos-Díaz, J.P. Intra- and Interrater Reliability of the Spanish Version of the Gross Motor Function Measure (GMFM-SP-88). Pediatr. Phys. Ther. 2022, 34, 193–200. [Google Scholar] [CrossRef] [PubMed]
- de Vet, H.C.W.; Terwee, C.B.; Knol, D.L.; Bouter, L.M. When to use agreement versus reliability measures. J. Clin. Epidemiol. 2006, 59, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
| GMFCS | Unilateral | Diparesis | Tetraparesis | Ataxic | Total | |
|---|---|---|---|---|---|---|
| Age range 6–12 | I | 10 | 5 | 1 | 0 | 16 |
| II | 6 | 12 | 3 | 0 | 21 | |
| III | 0 | 1 | 5 | 1 | 7 | |
| IV | 0 | 0 | 2 | 1 | 3 | |
| TOTAL | 16 | 18 | 11 | 2 | 47 | |
| Unilateral | Diparesis | Tetraparesis | Ataxic | Total | ||
| Age range 12–18 | I | 13 | 7 | 0 | 0 | 20 |
| II | 7 | 6 | 2 | 3 | 18 | |
| III | 0 | 2 | 4 | 0 | 6 | |
| IV | 0 | 0 | 4 | 1 | 5 | |
| TOTAL | 20 | 15 | 10 | 4 | 49 |
| TCMS-S | GMFCS I (n = 36) | GMFCS II (n = 39) | GMFCS III (n = 13) | GMFCS IV (n = 8) | ||||
|---|---|---|---|---|---|---|---|---|
| Novice | Expert | Novice | Expert | Novice | Expert | Novice | Expert | |
| Total score (x/58) | 45.80 ±4.29 | 51.73 ±3.96 | 40.05 ±4.92 | 43.47 ±6.18 | 32.92 ±8.82 | 32.3 ±10.72 | 20.14 ±9.39 | 20.64 ±12.5 |
| Static sitting balance (x/20) | 18.87 ±1.25 | 19.16 ±1.17 | 17.87 ±1.57 | 17.87 ±2.06 | 14.84 ±4.57 | 14 ±4.69 | 10.71 ±4.32 | 9.5 ±5.55 |
| Selective movement control (x/28) | 17.59 ±3.34 | 22.86 ±3.18 | 13.29 ±3.69 | 16.24 ±4.73 | 10.92 ±3.83 | 11.38 ±5.12 | 4.78 ±3.88 | 6.21 ±.5.40 |
| Dynamic reaching (x/10) | 9.33 ±0.98 | 9.7 ±0.82 | 8.88 ±0.89 | 9.35 ±0.7 | 7.15 ±1.51 | 6.92 ±2.26 | 4.64 ±2.47 | 4.92 ±3.19 |
| EXPERT RATERS | |||||
|---|---|---|---|---|---|
| TMCS-S | ER1 | ER2 | ICC (95% CI) | SEM | MDC95 |
| Total Score | 42.1 ± 11.8 | 44.0 ± 11.9 | 0.96 (0.88 to 0.98) | 2.0 | 5.7 |
| Static sitting balance | 16.7 ± 4.1 | 17.4 ± 4.2 | 0.93 (0.87 to 0.96) | 1.0 | 2.7 |
| Selective movement control | 16.6 ± 6.7 | 17.8 ± 7.0 | 0.95 (0.85 to 0.96) | 1.6 | 4.5 |
| Dynamic reaching | 8.8 ± 2.1 | 8.8 ± 2.0 | 0.95 (0.92 to 0.96) | 0.5 | 1.3 |
| NOVICE RATERS | |||||
| TMCS-S | N1 | N2 | ICC (95% CI) | SEM | MDC95 |
| Total Score | 40.0 ± 10.6 | 39.0 ± 9.2 | 0.82 (0.74 to 0.88) | 4.2 | 11.6 |
| Static sitting balance | 16.9 ± 3.7 | 17.4 ± 3.8 | 0.78 (0.68 to 0.85) | 1.7 | 4.9 |
| Selective movement control | 14.4 ± 6.2 | 13.3 ± 4.6 | 0.72 (0.60 to 0.81) | 2.8 | 7.8 |
| Dynamic reaching | 8.7 ± 1.9 | 8.2 ± 2.0 | 0.74 (0.63 to 0.83) | 0.9 | 2.6 |
| EXPERT RATERS vs. NOVICE RATERS | |||||
| TMCS-S | Novice 1–2 | Experts 3–4 | ICC (95% CI) | SEM | MDC95 |
| Total Score | 39.5 ± 9.5 | 43.0 ± 11.8 | 0.93 (0.71 to 0.97) | 3.1 | 8.7 |
| Static sitting balance | 17.2 ± 3.5 | 17.1 ± 4.1 | 0.96 (0.95 to 0.98) | 1.0 | 2.8 |
| Selective movement control | 13.9 ± 5.1 | 17.2 ± 6.8 | 0.85 (0.20 to 0.95) | 2.3 | 6.3 |
| Dynamic reaching | 8.4 ± 1.8 | 8.8 ± 2.0 | 0.93 (0.89 to 0.96) | 0.6 | 1.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Ruiz, J.; Estrada-Barranco, C.; Giménez-Mestre, M.J.; Villarroya-Mateos, I.; Martín-Casas, P.; López-de-Uralde-Villanueva, I. Differences between Novice and Expert Raters Assessing Trunk Control Using the Trunk Control Measurement Scale Spanish Version (TCMS-S) in Children with Cerebral Palsy. J. Clin. Med. 2023, 12, 3568. https://doi.org/10.3390/jcm12103568
López-Ruiz J, Estrada-Barranco C, Giménez-Mestre MJ, Villarroya-Mateos I, Martín-Casas P, López-de-Uralde-Villanueva I. Differences between Novice and Expert Raters Assessing Trunk Control Using the Trunk Control Measurement Scale Spanish Version (TCMS-S) in Children with Cerebral Palsy. Journal of Clinical Medicine. 2023; 12(10):3568. https://doi.org/10.3390/jcm12103568
Chicago/Turabian StyleLópez-Ruiz, Javier, Cecilia Estrada-Barranco, Maria José Giménez-Mestre, Isabel Villarroya-Mateos, Patricia Martín-Casas, and Ibai López-de-Uralde-Villanueva. 2023. "Differences between Novice and Expert Raters Assessing Trunk Control Using the Trunk Control Measurement Scale Spanish Version (TCMS-S) in Children with Cerebral Palsy" Journal of Clinical Medicine 12, no. 10: 3568. https://doi.org/10.3390/jcm12103568
APA StyleLópez-Ruiz, J., Estrada-Barranco, C., Giménez-Mestre, M. J., Villarroya-Mateos, I., Martín-Casas, P., & López-de-Uralde-Villanueva, I. (2023). Differences between Novice and Expert Raters Assessing Trunk Control Using the Trunk Control Measurement Scale Spanish Version (TCMS-S) in Children with Cerebral Palsy. Journal of Clinical Medicine, 12(10), 3568. https://doi.org/10.3390/jcm12103568