Safety and Efficiency of Rotational Atherectomy in Chronic Total Coronary Occlusion—One-Year Clinical Outcomes of an Observational Registry
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Definitions
2.3. Follow-Up
2.4. Clinical Endpoints
2.5. Statistical Methods
3. Results
4. Discussion
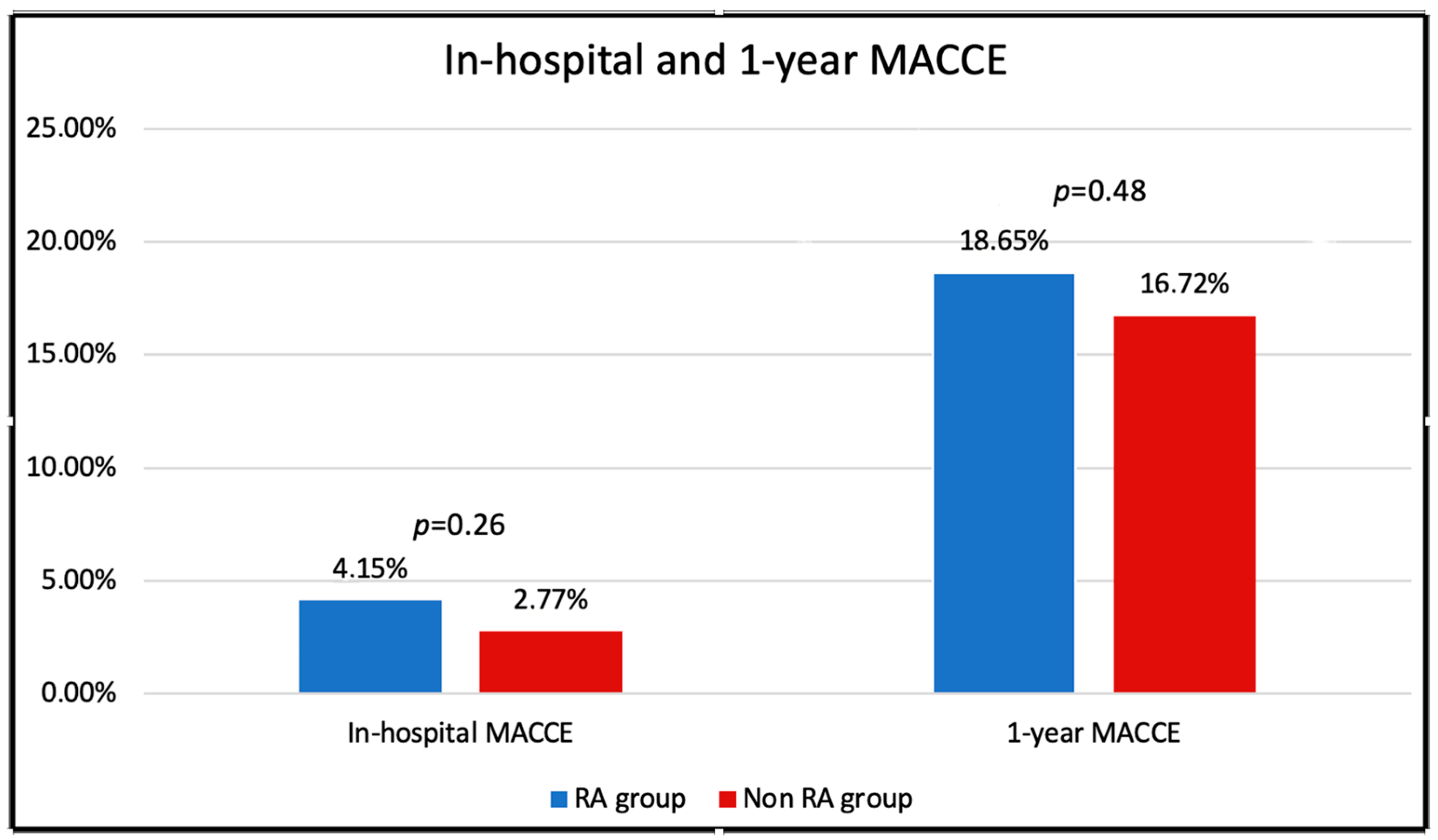
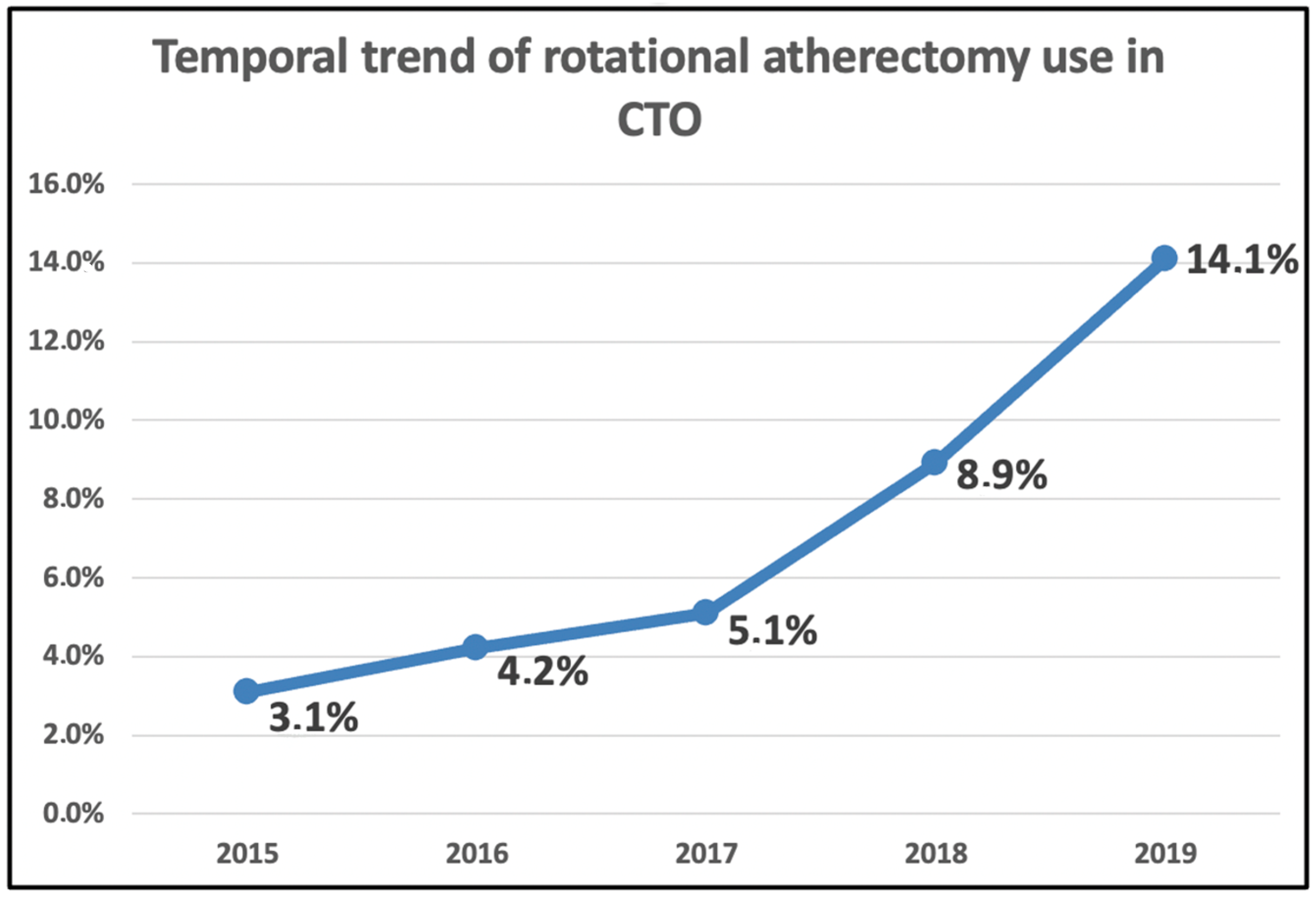
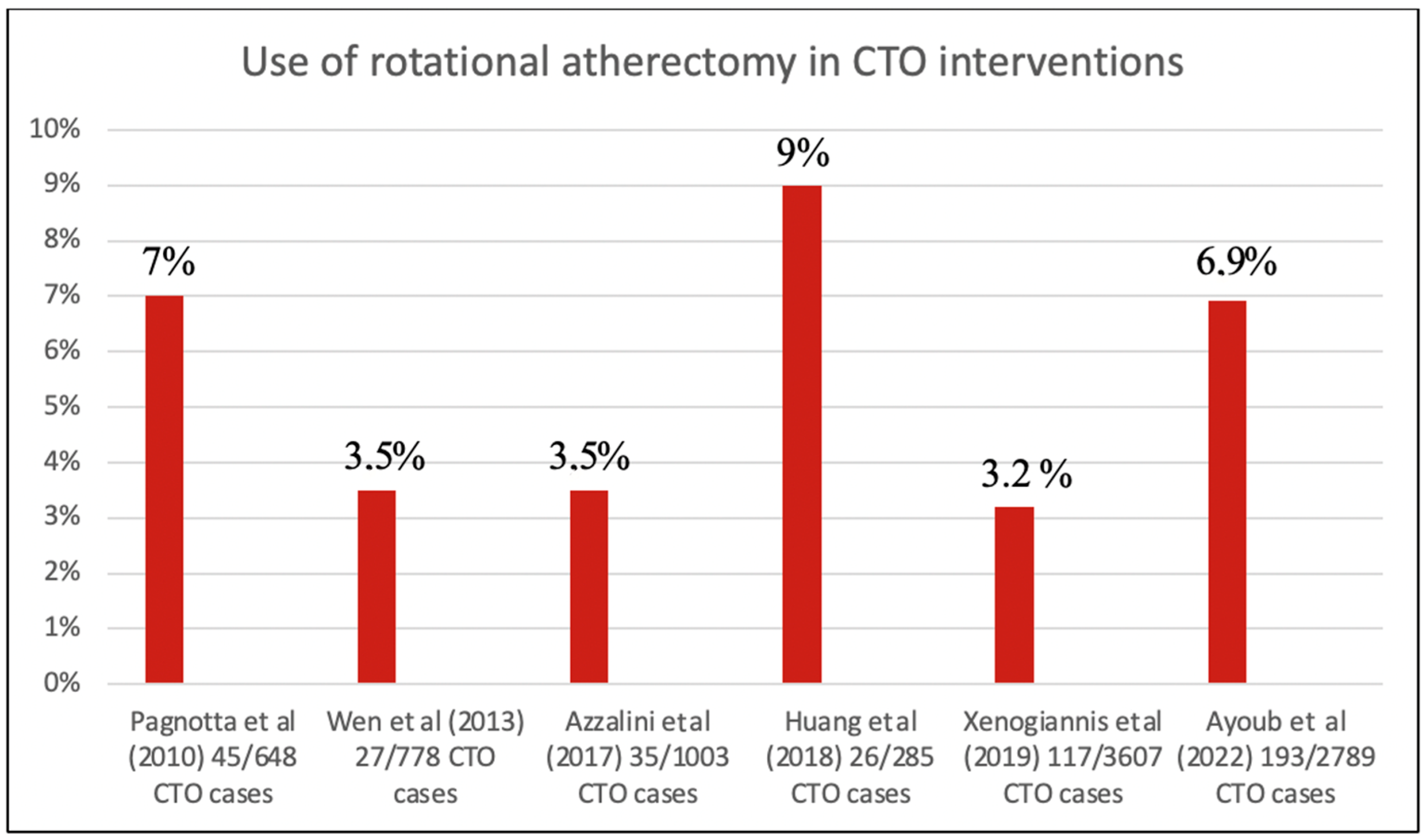
- RA is increasingly used in approximately 7% of our CTO cases in the last years, mainly for complex calcified lesions and in patients with prior CABG;
- RA is linked with a significantly higher rate of procedural and technical success;
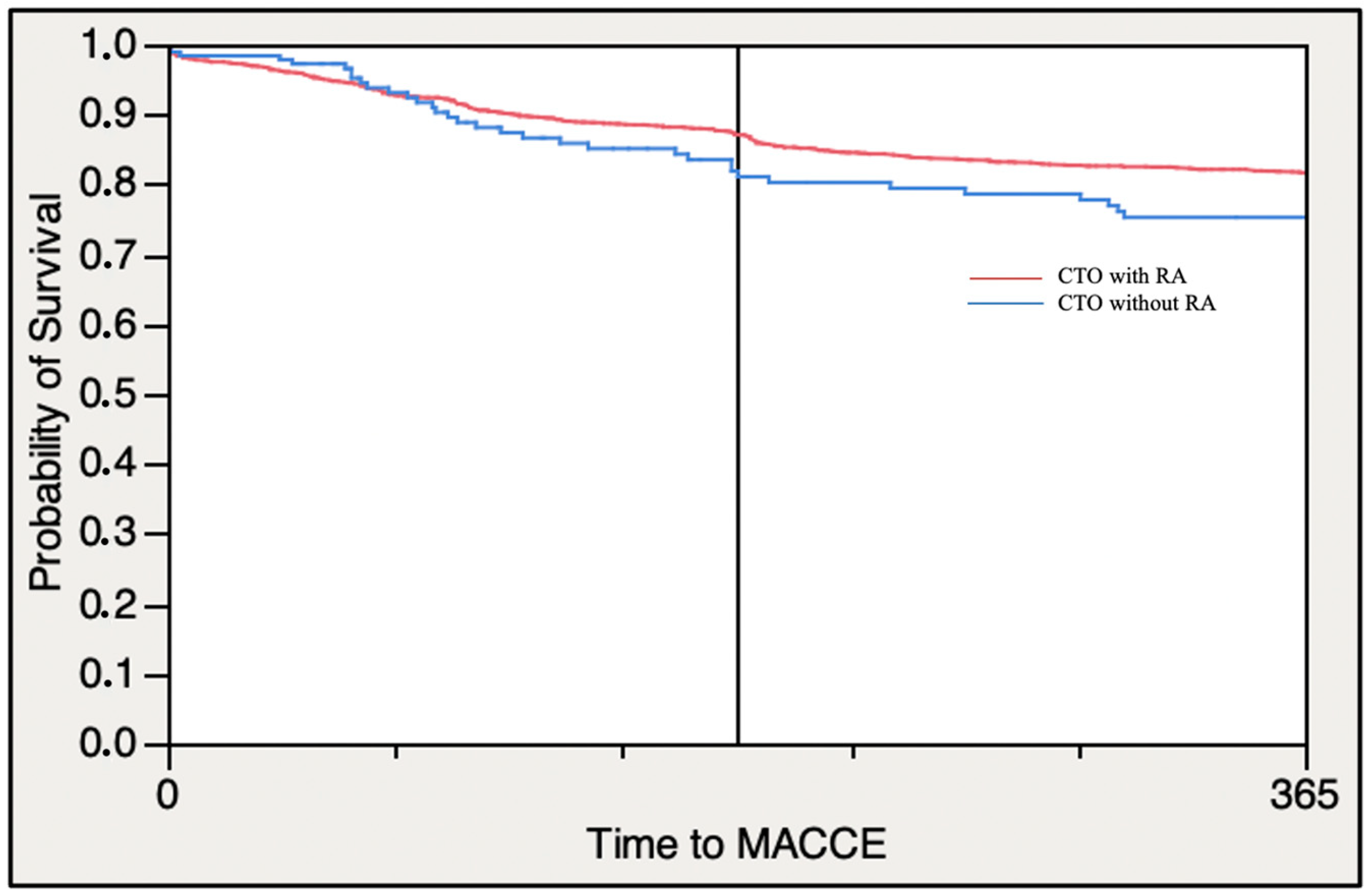
- Patients treated with RA showed similar in-hospital and one-year MACE rates despite a higher rate of tamponade and pericardiocentesis.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Williams, D.O.; Holubkov, R.; Yeh, W.; Bourassa, M.G.; Al-Bassam, M.; Block, P.C.; Coady, P.; Cohen, H.; Cowley, M.; Dorros, G.; et al. Percutaneous coronary intervention in the current era compared with 1985–1986: The National Heart, Lung, and Blood Institute Registries. Circulation 2000, 102, 2945–2951. [Google Scholar] [CrossRef] [PubMed]
- Anderson, H.V.; Shaw, R.E.; Brindis, R.G.; Hewitt, K.; Krone, R.J.; Block, P.C.; McKay, C.R.; Weintraub, W.S.; ACC–NCDR. A contemporary overview of percutaneous coronary interventions. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). J. Am. Coll. Cardiol. 2002, 39, 1096–1103. [Google Scholar] [CrossRef]
- Wilson, W.M.; Walsh, S.J.; Yan, A.T.; Hanratty, C.G.; Bagnall, A.J.; Egred, M.; Smith, E.; Oldroyd, K.G.; McEntegart, M.; Irving, J.; et al. Hybrid approach improves success of chronic total occlusion angioplasty. Heart 2016, 102, 1486–1493. [Google Scholar] [CrossRef]
- Karacsonyi, J.; Stanberry, L.; Alaswad, K.; Krestyaninov, O.; Choi, J.W.; Rangan, B.V.; Nikolakopoulos, I.; Vemmou, E.; Ungi, I.; Brilakis, E.S. Predicting Technical Success of Chronic Total Occlusion Percutaneous Coronary Intervention: Comparison of 3 Scores. Circ. Cardiovasc. Interv. 2021, 14, e009860. [Google Scholar] [CrossRef] [PubMed]
- Kovacic, J.C.; Sharma, A.B.; Roy, S.; Li, J.R.; Narayan, R.; Kim, D.B.; Sharma, S.K.; Kini, A.S. GuideLiner mother-and-child guide catheter extension: A simple adjunctive tool in PCI for balloon un-crossable chronic total occlusions. J. Interv. Cardiol. 2013, 26, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.M.; Pokala, N.R.; Menon, R.V.; Kotsia, A.P.; Raja, V.; Christopoulos, G.; Michael, T.T.; Rangan, B.V.; Sherbet, D.; Patel, V.G.; et al. Prevalence and treatment of “balloon-uncrossable” coronary chronic total occlusions. J. Invasive Cardiol. 2015, 27, 78–84. [Google Scholar] [PubMed]
- Pagnotta, P.; Briguori, C.; Mango, R.; Visconti, G.; Focaccio, A.; Belli, G.; Presbitero, P. Rotational atherectomy in resistant chronic total occlusions. Catheter. Cardiovasc. Interv. 2010, 76, 366–371. [Google Scholar] [CrossRef]
- Tajti, P.; Karmpaliotis, D.; Alaswad, K.; Toma, C.; Choi, J.W.; Jaffer, F.A.; Doing, A.H.; Patel, M.; Mahmud, E.; Uretsky, B.; et al. Prevalence, Presentation and Treatment of ‘Balloon Undilatable’ Chronic Total Occlusions: Insights from a Multicenter US Registry. Catheter. Cardiovasc. Interv. 2018, 91, 657–666. [Google Scholar] [CrossRef]
- Brilakis, E.S.; Mashayekhi, K.; Tsuchikane, E.; Rafeh, N.A.; Alaswad, K.; Araya, M.; Avran, A.; Azzalini, L.; Babunashvili, A.M.; Bayani, B.; et al. Guiding Principles for Chronic Total Occlusion Percutaneous Coronary Intervention. Circulation 2019, 140, 420–433. [Google Scholar] [CrossRef]
- Brilakis, E.S.; Grantham, J.A.; Rinfret, S.; Wyman, R.M.; Burke, M.N.; Karmpaliotis, D.; Lembo, N.; Pershad, A.; Kandzari, D.E.; Buller, C.E.; et al. A Percutaneous Treatment Algorithm for Crossing Coronary Chronic Total Occlusions. JACC Cardiovasc. Interv. 2012, 5, 367–379. [Google Scholar] [CrossRef]
- Levin, T.N.; Carroll, J.; Feldman, T. High-speed rotational atherectomy for chronic total coronary occlusions. Catheter. Cardiovasc. Diagn. 1996, (Suppl. 3), 34–39. [Google Scholar]
- Gruberg, L.; Mehran, R.; Dangas, G.; Hong, M.K.; Mintz, G.S.; Kornowski, R.; Lansky, A.J.; Kent, K.M.; Pichard, A.D.; Satler, L.F.; et al. Effect of plaque debulking and stenting on short- and long-term outcomes after revascularization of chronic total occlusions. J. Am. Coll. Cardiol. 2000, 35, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Brilakis, E.S. Manual of Chronic Total Occlusion Interventions a Step-by-Step Approach; Elsevier/Academic Press: London, UK; L.E.A. Press: Hrajel, Liban, 2018. [Google Scholar]
- Moliterno, D.J. Rotational atherectomy for resistant chronic total occlusions: Another spin for tough old problems. Catheter. Cardiovasc. Interv. 2010, 76, 372–373. [Google Scholar] [CrossRef] [PubMed]
- Xenogiannis, I.; Karmpaliotis, D.; Alaswad, K.; Jaffer, F.A.; Yeh, R.W.; Patel, M.; Mahmud, E.; Choi, J.W.; Burke, M.N.; Doing, A.H.; et al. Usefulness of Atherectomy in Chronic Total Occlusion Interventions (from the PROGRESS-CTO Registry). Am. J. Cardiol. 2019, 123, 1422–1428. [Google Scholar] [CrossRef] [PubMed]
- Wen, S.-Y.; Yu, H.-Y.; Wang, B.-Y.; Sun, Z.-Q.; Wang, M.-Q.; Liu, S.-Q.; Li, H. Feasibility and outcome of rotational atherectomy for treating resistant chronic total occlusions. Zhonghua Xin Xue Guan Bing Za Zhi 2013, 41, 466–469. [Google Scholar] [PubMed]
- Huang, W.-C.; Teng, H.-I.; Chan, W.-L.; Lu, T.-M. Short-term and long-term clinical outcomes of rotational atherectomy in resistant chronic total occlusion. J. Interv. Cardiol. 2018, 31, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Azzalini, L.; Dautov, R.; Ojeda, S.; Serra, A.; Benincasa, S.; Bellini, B.; Giannini, F.; Chavarría, J.; Gheorghe, L.L.; Pan, M.; et al. Long-term outcomes of rotational atherectomy for the percutaneous treatment of chronic total occlusions. Catheter. Cardiovasc. Interv. 2017, 89, 820–828. [Google Scholar] [CrossRef]
- Mintz, G.S.; Popma, J.J.; Pichard, A.D.; Kent, K.M.; Satler, L.F.; Chuang, Y.C.; Ditrano, C.J.; Leon, M.B. Patterns of calcification in coronary artery disease. A statistical analysis of intravascular ultrasound and coronary angiography in 1155 lesions. Circulation 1995, 91, 1959–1965. [Google Scholar] [CrossRef]
- Valgimigli, M.; Bueno, H.; Byrne, R.A.; Collet, J.P.; Costa, F.; Jeppsson, A.; Jüni, P.; Kastrati, A.; Kolh, P.; Mauri, L.; et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2018, 39, 213–260. [Google Scholar]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018, 138, e618–e651. [Google Scholar] [CrossRef]
- de Labriolle, A.; Bonello, L.; Roy, P.; Lemesle, G.; Steinberg, D.H.; Xue, Z.; Kaneshige, K.; Suddath, W.O.; Satler, L.F.; Kent, K.M.; et al. Comparison of safety, efficacy, and outcome of successful versus unsuccessful percutaneous coronary intervention in “true” chronic total occlusions. Am. J. Cardiol. 2008, 102, 1175–1181. [Google Scholar] [CrossRef] [PubMed]
- Olivari, Z.; Rubartelli, P.; Piscione, F.; Ettori, F.; Fontanelli, A.; Salemme, L.; Giachero, C.; Di Mario, C.; Gabrielli, G.; Spedicato, L.; et al. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: Data from a multicenter, prospective, observational study (TOAST-GISE). J. Am. Coll. Cardiol. 2003, 41, 1672–1678. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.; Rihal, C.S.; Lennon, R.J.; Wiste, H.J.; Singh, M.; Holmes, D.R. Trends in outcomes after percutaneous coronary intervention for chronic total occlusions: A 25-year experience from the Mayo Clinic. J. Am. Coll. Cardiol. 2007, 49, 1611–1618. [Google Scholar] [CrossRef] [PubMed]
- Suero, J.A.; Marso, S.P.; Jones, P.G.; Laster, S.B.; Huber, K.C.; Giorgi, L.V.; Johnson, W.L.; Rutherford, B.D. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: A 20-year experience. J. Am. Coll. Cardiol. 2001, 38, 409–414. [Google Scholar] [CrossRef]
- Park, T.K.; Lee, S.H.; Choi, K.H.; Lee, J.M.; Yang, J.H.; Bin Song, Y.; Hahn, J.; Choi, J.; Gwon, H.; Lee, S.H.; et al. Late Survival Benefit of Percutaneous Coronary Intervention Compared With Medical Therapy in Patients With Coronary Chronic Total Occlusion: A 10-Year Follow-Up Study. J. Am. Hear. Assoc. 2021, 10, e019022. [Google Scholar] [CrossRef]
- Li, H.; Ai, H.; Li, L.; Zheng, N.; Tang, G.; Yang, G.; Zhao, Y.; Sun, F.; Zhang, H. The therapeutic effects of excimer laser coronary atherectomy therapy for in-stent restenosis chronic total occlusions. BMC Cardiovasc. Disord. 2021, 21, 399. [Google Scholar] [CrossRef]
| Patient Characteristics | CTO without RA (n = 2596) | CTO with RA (n = 193) | p Value |
|---|---|---|---|
| Age (years) | 65.73 ± 10.84 | 70.33 ± 8.97 | <0.0001 * |
| Men | 82.55% | 80.83% | 0.56 |
| BMI (kg/m2) | 28.44 ± 4.66 | 28.19 ± 4.47 | 0.45 |
| eGFR, mL/min/1.73 m2 | 72.43 | 66.18 | <0.0001 * |
| CAD presentation | 0.37 | ||
| ACS | 12.79% | 10.36% | |
| No ACS | 87.21% | 89.64% | |
| Diabetes mellitus | 29.85% | 43.41% | 0.0002 * |
| Dyslipidemia | 89.89% | 92.27% | 0.37 |
| Hypertension | 85.86% | 92.51% | 0.0081 * |
| Smoking (current) | 20.01% | 10.99% | 0.0024 * |
| LVEF (%) | 0.29 | ||
| >51% | 62.24% | 58.89% | |
| 41–51% | 20.31% | 25.56% | |
| 30–40% | 10.89% | 11.11% | |
| 0–29% | 6.56% | 4.44% | |
| Family History of CAD | 43.58% | 37.18% | 0.13 |
| Prior Myocardial Infarction | 38.35% | 34.50% | 0.33 |
| Prior CABG | 16.06% | 33.52% | <0.0001 * |
| Prior CVD | 11.6% | 12.3% | 0.87 |
| LDL max. | 104.75 ± 41.39 | 91.78 ± 35.71 | <0.0001 * |
| CTO without RA (n = 2596) | CTO with RA (n = 193) | p Value | |
|---|---|---|---|
| Target vessel | <0.0001 * | ||
| 50.35% | 55.96% | |
| 21.34% | 19.17% | |
| 26.93% | 20.73% | |
| 0.7% | 0.0% | |
| Number of treated vessels | 1.35 ± 0.58 | 1.41 ± 0.59 | 0.14 |
| Number of treated segments | 6.63 ± 5.41 | 5.67 ± 4.94 | 0.009 * |
| Lesion length (mm) | 0.15 | ||
| 2.93% | 0.52% | 0.22 |
| 18.09% | 17.28% | |
| 78.98% | 82.20% | |
| Ostial lesion | 6.69% | 7.2% | 0.32 |
| Calcification | <0.0001 * | ||
| 6.49% | 0.52% | |
| 28.42% | 2.07% | |
| 28.80% | 11.40% | |
| 36.29% | 86.01% | |
| Eccentric calcification | 53.12% | 49.41% | 0.35 |
| Tortuosity | 20.74% | 23.83% | 0.31 |
| Relevant side brunch | 29.58% | 23.40% | 0.072 * |
| Intra-lesion Angulation | 0.13 | ||
| 11.98% | 11.92% | |
| 36.47% | 30.05% | |
| 45.12% | 48.19% | |
| 6.43% | 9.84% | <0.0001 * |
| CTO without RA (n = 2596) | CTO with RA (n = 193) | p Value | |
|---|---|---|---|
| Balloon diameter pre-dilatation, mm | 2.50 ± 1.23 | 2.99 ± 2.74 | <0.0001 * |
| Maximum inflation pressure pre-dilatation, atm | 17.63 ± 5.37 | 22.65 ± 18.59 | <0.0001 * |
| Number of stents implanted | 1.73 ± 1.20 | 2.19 ± 1.15 | <0.0001 * |
| Diameter of implanted stent, max., mm | 3.17 ± 0.04 | 4.16 ± 0.53 | 0.05 * |
| Overall stent length, mm | 54.18 ± 32.5 | 50.55 ± 30.21 | 0.23 |
| Balloon diameter post-dilatation, mm | 3.64 ± 2.13 | 3.96 ± 3.08 | <0.0001 * |
| Post-dilatation pressure, atm | 20.12 ± 7.04 | 21.98 ± 6.92 | <0.0001 * |
| Burr Size used | |||
| 33.14% | ||
| 47.34% | ||
| 16.57% | ||
| 2.96% | ||
| TIMI flow post PCI | 0.0063 * | ||
| 12.2% | 5.79% | |
| 1.48% | 1.05% | |
| 86.33% | 93.16% | |
| Access site | 0.0027 * | ||
| 31.08% | 20.32% | |
| 68.60% | 78.61% | |
| Guiding catheter size, Fr | <0.0001 * | ||
| 62.82% | 32.13% | |
| 34.25% | 60.62% | |
| 2.93% | 7.25% | |
| CTO technique | 0.29 | ||
| 73.42% | 69.95% | |
| 26.58% | 30.05% | |
| Procedural time (minutes) | 81 (33–126) | 127 (94–186) | <0.0001 * |
| Fluoroscopy time (minutes) | 35 (20–60) | 54 (35–80) | <0.0001 * |
| Fluoroscopic Dose Area Product (cGy*cm2) | 9710 (5388–16,398) | 12,881 (4347–20,632) | <0.0001 * |
| Contrast volume used (mL) | 260 (190–390) | 310 (200–400) | 0.0002 * |
| CTO without RA (n = 2596) | CTO with RA (n = 193) | p Value | |
|---|---|---|---|
| one-year MACCE | 16.72% (434) | 18.65% (36) | 0.48 |
| one-year Mortality | 3.70% (96) | 5.7% (11) | 0.16 |
| one-year MI | 1.2% (31) | 1.04% (2) | 0.84 |
| one-year TVR | 16.26% (422) | 18.65% (36) | 0.39 |
| one-year Stroke | 0.65% (17) | 0,00% (0) | 0.63 |
| one-year TLR | 14.33% (372) | 18.13% (35) | 0.16 |
| In-hospital MACCE | 2.77% (72) | 4.15% (8) | 0.26 |
| Mortality | 1.04% (27) | 1.04% (2) | 1.0 |
| MI Type 4a | 5.5% (142) | 12.5% (24) | <0.0004 * |
| TVR | 16.35% (475) | 18.52% (40) | 0.40 |
| Stroke | 0.19% (5) | 0% (0) | 1.0 |
| Technical success | 87.87% (2281) | 97.41% (188) | <0.0001 * |
| Procedural success | 85.10% (2209) | 93.26% (180) | 0.0002 * |
| Procedural time (min) | 81 (33.6, 126) | 127 (94, 186) | <0.0001 * |
| Fluoroscopy time (min) | 35 (20, 60) | 54 (35, 80) | <0.0001 * |
| Contrast volume used (mL) | 260 (190, 390) | 310 (200, 400) | <0.0002 * |
| Fluoroscopic Dose Area Product (cGy*cm2) | 9710 (5388–16,398) | 12,881 (4347–20,632) | <0.0001 * |
| Major Complication % (n) | |||
| Perforation | 1.99% (51) | 7.94% (15) | <0.0001 * |
| Pericardiocentesis | 0.5% (13) | 3.11% (6) | 0.0013 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayoub, M.; Corpataux, N.; Behnes, M.; Schupp, T.; Forner, J.; Akin, I.; Neumann, F.-J.; Westermann, D.; Rudolph, V.; Mashayekhi, K. Safety and Efficiency of Rotational Atherectomy in Chronic Total Coronary Occlusion—One-Year Clinical Outcomes of an Observational Registry. J. Clin. Med. 2023, 12, 3510. https://doi.org/10.3390/jcm12103510
Ayoub M, Corpataux N, Behnes M, Schupp T, Forner J, Akin I, Neumann F-J, Westermann D, Rudolph V, Mashayekhi K. Safety and Efficiency of Rotational Atherectomy in Chronic Total Coronary Occlusion—One-Year Clinical Outcomes of an Observational Registry. Journal of Clinical Medicine. 2023; 12(10):3510. https://doi.org/10.3390/jcm12103510
Chicago/Turabian StyleAyoub, Mohamed, Noé Corpataux, Michael Behnes, Tobias Schupp, Jan Forner, Ibrahim Akin, Franz-Josef Neumann, Dirk Westermann, Volker Rudolph, and Kambis Mashayekhi. 2023. "Safety and Efficiency of Rotational Atherectomy in Chronic Total Coronary Occlusion—One-Year Clinical Outcomes of an Observational Registry" Journal of Clinical Medicine 12, no. 10: 3510. https://doi.org/10.3390/jcm12103510
APA StyleAyoub, M., Corpataux, N., Behnes, M., Schupp, T., Forner, J., Akin, I., Neumann, F.-J., Westermann, D., Rudolph, V., & Mashayekhi, K. (2023). Safety and Efficiency of Rotational Atherectomy in Chronic Total Coronary Occlusion—One-Year Clinical Outcomes of an Observational Registry. Journal of Clinical Medicine, 12(10), 3510. https://doi.org/10.3390/jcm12103510








