One-Year and Five-Year Outcomes of Transcatheter Aortic Valve Replacement or Surgical Aortic Valve Replacement in a Taiwanese Elderly Population
Abstract
:1. Introduction
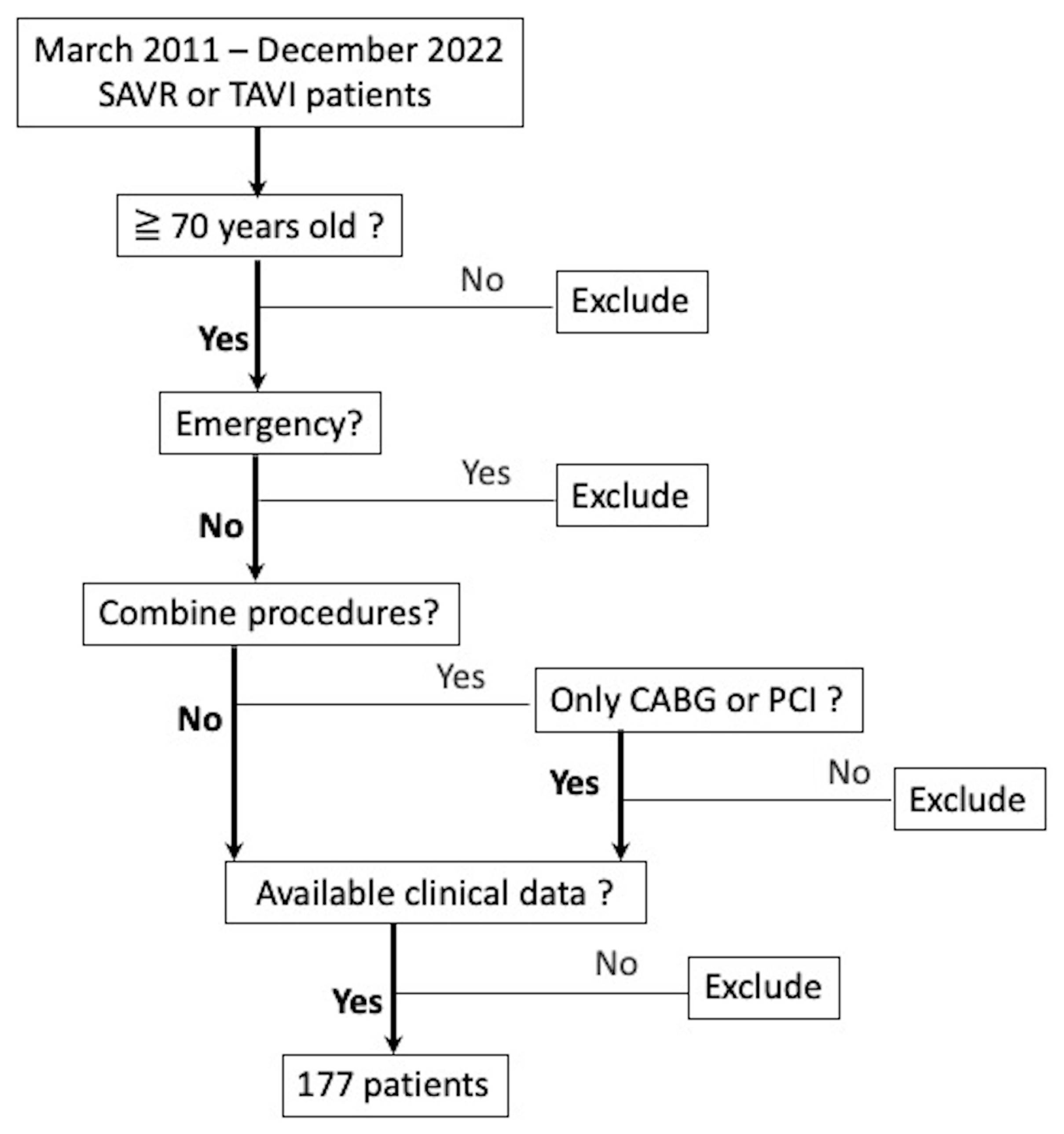
2. Materials and Methods
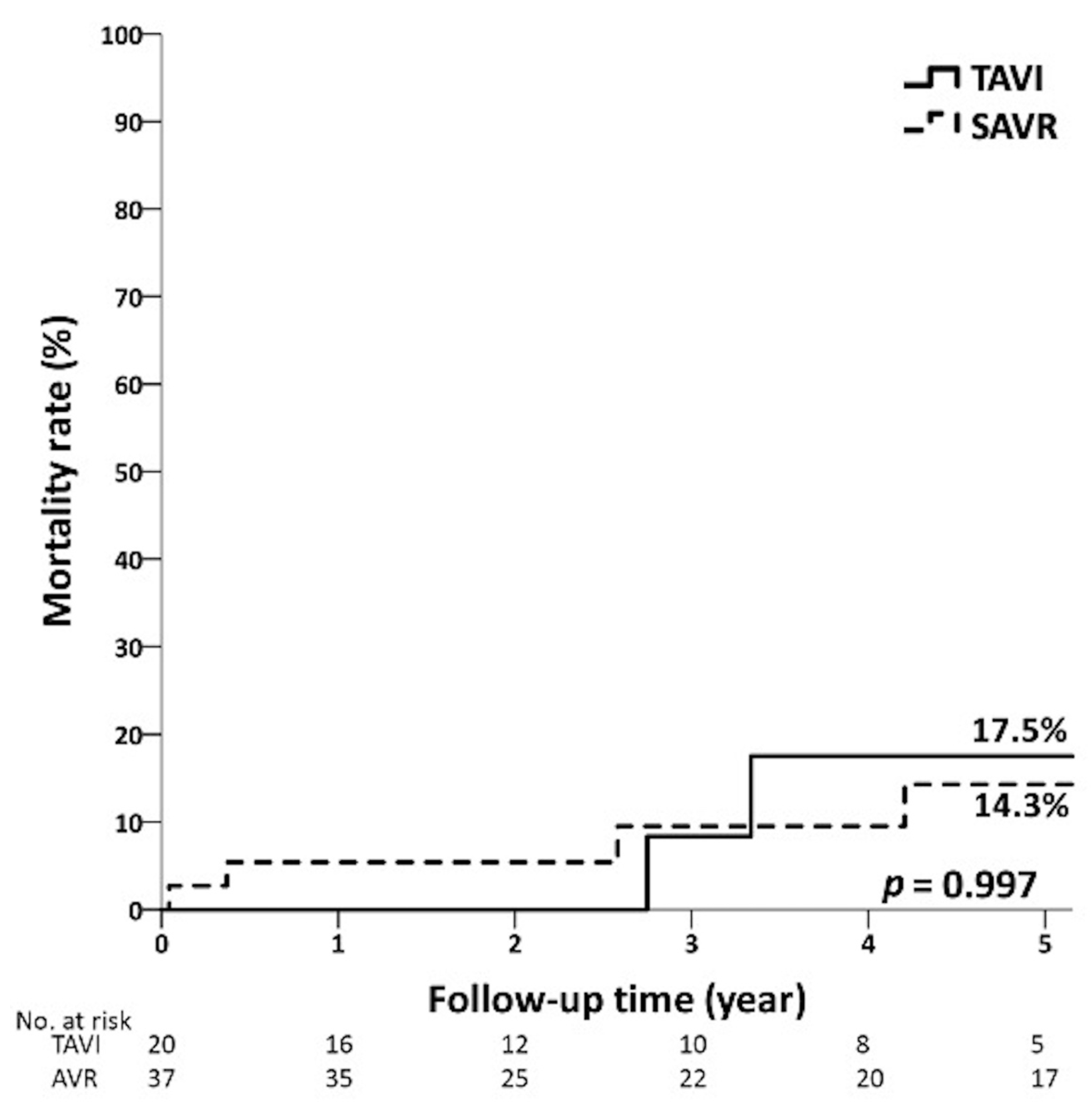
3. Results
4. Discussion
4.1. Body Mass Index
4.2. Diabetes Mellitus
4.3. Peripheral Arterial Obstructive Disease
4.4. Acute Kidney Injury
4.5. Research Contributions
4.6. Study Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Voigtländer, L.; Twerenbold, R.; Schäfer, U.; Conradi, L.; Balaban, Ü.; Bekeredjian, R.; Ensminger, S.; Walther, T.; Beckmann, A.; Frerker, C.; et al. Prognostic Impact of Underweight (Body Mass Index < 20 kg/m2) in Patients With Severe Aortic Valve Stenosis Undergoing Transcatheter Aortic Valve Implantation or Surgical Aortic Valve Replacement (from the German Aortic Valve Registry [GARY]). Am. J. Cardiol. 2020, 129, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Winter, J.E.; MacInnis, R.J.; Wattanapenpaiboon, N.; Nowson, C.A. BMI and all-cause mortality in older adults: A meta-analysis. Am. J. Clin. Nutr. 2014, 99, 875–890. [Google Scholar] [CrossRef] [PubMed]
- Takeji, Y.; Taniguchi, T.; Morimoto, T.; Saito, N.; Ando, K.; Shirai, S.; Sakaguchi, G.; Arai, Y.; Fuku, Y.; Kawase, Y.; et al. Transcatheter Aortic Valve Implantation vs. Surgical Aortic Valve Replacement for Severe Aortic Stenosis in Real-World Clinical Practice. Circ. J. 2020, 84, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Makkar, R.R.; Thourani, V.H.; Mack, M.J.; Kodali, S.K.; Kapadia, S.; Webb, J.G.; Yoon, S.-H.; Trento, A.; Svensson, L.G.; Herrmann, H.C.; et al. Five-Year Outcomes of Transcatheter or Surgical Aortic-Valve Replacement. N. Engl. J. Med. 2020, 382, 799–809. [Google Scholar] [CrossRef] [PubMed]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705. [Google Scholar] [CrossRef] [PubMed]
- Mack, M.J.; Leon, M.B.; Smith, C.R.; Miller, D.C.; Moses, J.W.; Tuzcu, E.M.; Webb, J.G.; Douglas, P.S.; Anderson, W.N.; Blackstone, E.H.; et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): A randomised controlled trial. Lancet 2015, 385, 2477–2484. [Google Scholar] [CrossRef]
- Sannino, A.; Schiattarella, G.G.; Toscano, E.; Gargiulo, G.; Giugliano, G.; Galderisi, M.; Losi, M.-A.; Stabile, E.; Cirillo, P.; Imbriaco, M.; et al. Meta-Analysis of Effect of Body Mass Index on Outcomes After Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2017, 119, 308–316. [Google Scholar] [CrossRef]
- Mariscalco, G.; Wozniak, M.; Dawson, A.G.; Serraino, G.F.; Porter, R.; Nath, M.; Klersy, C.; Kumar, T.; Murphy, G.J. Body Mass Index and Mortality Among Adults Undergoing Cardiac Surgery: A Nationwide Study With a Systematic Review and Meta-Analysis. Circulation 2017, 135, 850–863. [Google Scholar] [CrossRef]
- Burns, D.J.; Rapetto, F.; Angelini, G.D.; Benedetto, U.; Caputo, M.; Ciulli, F.; Vohra, H.A. Body mass index and early outcomes following mitral valve surgery for degenerative disease. J. Thorac. Cardiovasc. Surg. 2021, 161, 1765–1773.e2. [Google Scholar] [CrossRef]
- Gao, M.; Sun, J.; Young, N.; Boyd, D.; Atkins, Z.; Li, Z.; Ding, Q.; Diehl, J.; Liu, H. Impact of Body Mass Index on Outcomes in Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2016, 30, 1308–1316. [Google Scholar] [CrossRef]
- Al-Sarraf, N.; Raza, A.; Rowley, S.; Hughes, A.; Tolan, M.; Young, V.; McGovern, E. Short-term and long-term outcome in low body mass index patients undergoing cardiac surgery. Gen. Thorac. Cardiovasc. Surg. 2009, 57, 87–93. [Google Scholar] [CrossRef]
- Batsis, J.A.; Zagaria, A.B. Addressing Obesity in Aging Patients. Med. Clin. N. Am. 2018, 102, 65–85. [Google Scholar] [CrossRef]
- Lin, Y.-K.; Wang, C.-C.; Yen, Y.-F.; Chen, L.-J.; Ku, P.-W.; Chen, C.-C.; Lai, Y.-J. Association of body mass index with all-cause mortality in the elderly population of Taiwan: A prospective cohort study. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Forgie, K.; Bozso, S.J.; Hong, Y.; Norris, C.M.; Ishaque, A.; Gill, R.S.; Freed, D.H.; Moon, M.C.; Nagendran, J.; Nagendran, J. The effects of body mass index on outcomes for patients undergoing surgical aortic valve replacement. BMC Cardiovasc. Disord. 2020, 20, 255. [Google Scholar] [CrossRef]
- Conrotto, F.; D’Ascenzo, F.; Giordana, F.; Salizzoni, S.; Tamburino, C.; Tarantini, G.; Presbitero, P.; Barbanti, M.; Gasparetto, V.; Mennuni, M.; et al. Impact of Diabetes Mellitus on Early and Midterm Outcomes After Transcatheter Aortic Valve Implantation (from a Multicenter Registry). Am. J. Cardiol. 2014, 113, 529–534. [Google Scholar] [CrossRef]
- Tokarek, T.; Dziewierz, A.; Wiktorowicz, A.; Bagienski, M.; Rzeszutko, L.; Sorysz, D.; Kleczynski, P.; Dudek, D. Effect of diabetes mellitus on clinical outcomes and quality of life after transcatheter aortic valve implantation for severe aortic valve stenosis. Hell. J. Cardiol. 2018, 59, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Chorin, E.; Finkelstein, A.; Banai, S.; Aviram, G.; Barkagan, M.; Barak, L.; Keren, G.; Steinvil, A. Impact of Diabetes Mellitus and Hemoglobin A1C on Outcome After Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2015, 116, 1898–1903. [Google Scholar] [CrossRef] [PubMed]
- Natorska, J. Diabetes mellitus as a risk factor for aortic stenosis: From new mechanisms to clinical implications. Kardiol. Pol. 2021, 79, 1060–1067. [Google Scholar] [CrossRef]
- Abramowitz, Y.; Jilaihawi, H.; Chakravarty, T.; Mangat, G.; Maeno, Y.; Kazuno, Y.; Takahashi, N.; Kawamori, H.; Cheng, W.; Makkar, R.R. Impact of Diabetes Mellitus on Outcomes After Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2016, 117, 1636–1642. [Google Scholar] [CrossRef]
- Puls, M.; Bleckmann, A.; Jacobshagen, C.; Danner, B.C.; Hasenfuß, G.; Seipelt, R.; Schillinger, W. Diabetes increases short- and long-term mortality after transcatheter aortic valve implantation (TAVI). Dtsch. Med. Wochenschr. 2014, 139, 822–828. [Google Scholar] [CrossRef]
- Matsumoto, S.; Ohno, Y.; Miyamoto, J.; Ikari, Y.; Tada, N.; Naganuma, T.; Yamawaki, M.; Yamanaka, F.; Shirai, S.; Mizutani, K.; et al. Impact of diabetes mellitus on outcome after transcatheter aortic valve replacement: Identifying high-risk diabetic population from the OCEAN-TAVI registry. Catheter. Cardiovasc. Interv. 2021, 98, E1058–E1065. [Google Scholar] [CrossRef] [PubMed]
- Ueshima, D.; Barioli, A.; Fovino, L.N.; D’Amico, G.; Fabris, T.; Brener, S.J.; Tarantini, G. The impact of pre-existing peripheral artery disease on transcatheter aortic valve implantation outcomes: A systematic review and meta-analysis. Catheter. Cardiovasc. Interv. 2020, 95, 993–1000. [Google Scholar] [CrossRef] [PubMed]
- Takagi, H.; Hari, Y.; Nakashima, K.; Kuno, T.; Ando, T.; ALICE (All-Literature Investigation of Cardiovascular Evidence) Group. Meta-analysis of prognostic impact of peripheral arterial disease on mortality after transcatheter aortic valve implantation. J. Cardiovasc. Surg. 2019, 60, 723–732. [Google Scholar] [CrossRef]
- Sinning, J.-M.; Horack, M.; Grube, E.; Gerckens, U.; Erbel, R.; Eggebrecht, H.; Zahn, R.; Linke, A.; Sievert, H.; Figulla, H.-R.; et al. The impact of peripheral arterial disease on early outcome after transcatheter aortic valve implantation: Results from the German Transcatheter Aortic Valve Interventions Registry. Am. Heart J. 2012, 164, 102–110.e1. [Google Scholar] [CrossRef]
- Shah, K.; Chaker, Z.; Busu, T.; Shah, R.; Osman, M.; Alqahtani, F.; Alkhouli, M. Meta-Analysis Comparing Renal Outcomes after Transcatheter versus Surgical Aortic Valve Replacement. J. Interv. Cardiol. 2019, 2019, 3537256. [Google Scholar] [CrossRef]
- Haase-Fielitz, A.; Altendeitering, F.; Iwers, R.; Sliziuk, V.; Barabasch, S.; Bannehr, M.; Hähnel, V.; Neuss, M.; Haase, M.; Apfelbacher, C.; et al. Acute kidney injury may impede results after transcatheter aortic valve implantation. Clin. Kidney J. 2021, 14, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-García, A.J.; Muñoz-García, E.; Jiménez-Navarro, M.F.; Domínguez-Franco, A.J.; Alonso-Briales, J.H.; Hernández-García, J.M.; de Teresa-Galván, E. Clinical impact of acute kidney injury on short- and long-term outcomes after transcatheter aortic valve implantation with the CoreValve prosthesis. J. Cardiol. 2015, 66, 46–49. [Google Scholar] [CrossRef]
- Meneguz-Moreno, R.A.; Ramos, A.I.; Siqueira, D.; de Castro-Filho, A.; Jatene, T.; Jeronimo, A.D.; Le Bihan, D.; Moreira, A.; Arrais, M.; Abizaid, A.; et al. Prognostic value of renal function in patients with aortic stenosis treated with transcatheter aortic valve replacement. Catheter. Cardiovasc. Interv. 2017, 89, 452–459. [Google Scholar] [CrossRef]
- Ma, M.; Gao, W.-D.; Gu, Y.-F.; Wang, Y.-S.; Zhu, Y.; He, Y. Clinical effects of acute kidney injury after transcatheter aortic valve implantation: A systematic review and meta-analysis. Intern. Emerg. Med. 2019, 14, 161–175. [Google Scholar] [CrossRef]


| STS Score < 4% | STS Score 4–8% | STS Score > 8% | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | TAVI (n = 20) | SAVR (n = 37) | p Value | TAVI (n = 37) | SAVR (n = 28) | p Value | TAVI (n = 45) | SAVR (n = 10) | p Value | ||||||
| Age | 79.6 | ±3.8 | 75.4 | ±3.9 | <0.001 ** | 83.1 | ±5.2 | 79.5 | ±4.6 | 0.015 * | 83.9 | ±6.2 | 74.3 | ±4.1 | <0.001 ** |
| Gender | 0.898 | 0.861 | 1.000 | ||||||||||||
| Female | 11 | (55.0%) | 21 | (56.8%) | 23 | (62.2%) | 18 | (64.3%) | 26 | (57.8%) | 6 | (60.0%) | |||
| Male | 9 | (45.0%) | 16 | (43.2%) | 14 | (37.8%) | 10 | (35.7%) | 19 | (42.2%) | 4 | (40.0%) | |||
| Body height (cm) | 155.4 | ±7.1 | 157.0 | ±8.7 | 0.525 | 155.1 | ±7.2 | 153.3 | ±8.0 | 0.323 | 153.3 | ±8.2 | 153.7 | ±5.4 | 0.662 |
| Body weight (kg) | 63.1 | ±9.1 | 66.3 | ±12.7 | 0.682 | 59.2 | ±10.5 | 57.0 | ±9.2 | 0.317 | 53.9 | ±8.9 | 53.6 | ±10.5 | 0.777 |
| Body mass index | 26.1 | ±2.8 | 26.9 | ±4.7 | 0.907 | 24.5 | ±3.5 | 24.3 | ±3.7 | 0.731 | 22.9 | ±3.6 | 22.7 | ±4.6 | 0.600 |
| Body mass index < 20 f | 1 | (5.0%) | 1 | (2.7%) | 1.000 | 4 | (10.8%) | 5 | (17.9%) | 0.483 | 10 | (22.2%) | 3 | (30.0%) | 0.685 |
| STS score (%) | 2.8 | ±0.7 | 2.5 | ±0.7 | 0.201 | 5.9 | ±1.3 | 5.4 | ±1.2 | 0.131 | 15.4 | ±6.5 | 14.2 | ±5.0 | 0.678 |
| Euroscore II (%) | 2.5 | ±1.1 | 3.3 | ±2.4 | 0.504 | 5.9 | ±4.4 | 6.9 | ±5.7 | 0.781 | 10.4 | ±8.9 | 13.4 | ±8.6 | 0.150 |
| Symptoms and Signs | |||||||||||||||
| Heart failure f | 10 | (50.0%) | 34 | (91.9%) | 0.001 ** | 25 | (67.6%) | 26 | (92.9%) | 0.014 * | 40 | (88.9%) | 10 | (100%) | 0.572 |
| Syncope f | 1 | (5.0%) | 3 | (8.1%) | 1.000 | 3 | (8.1%) | 3 | (10.7%) | 1.000 | 5 | (11.1%) | 3 | (30.0%) | 0.149 |
| Angina | 8 | (40.0%) | 16 | (43.2%) | 0.813 | 11 | (29.7%) | 15 | (53.6%) | 0.052 | 14 | (31.1%) | 6 | (60.0%) | 0.144 |
| Mild symptom f | 8 | (40.0%) | 3 | (8.1%) | 0.011 * | 8 | (21.6%) | 0 | (0%) | 0.008 ** | 5 | (11.1%) | 0 | (0%) | 0.572 |
| NYHA | <0.001 ** | 0.001 ** | 0.072 | ||||||||||||
| 1 | 3 | (15.0%) | 0 | (0%) | 5 | (13.5%) | 0 | (0%) | 1 | (2.2%) | 0 | (0%) | |||
| 2 | 10 | (50.0%) | 4 | (10.8%) | 15 | (40.5%) | 2 | (7.1%) | 18 | (40.0%) | 0 | (0%) | |||
| 3 | 6 | (30.0%) | 32 | (86.5%) | 15 | (40.5%) | 21 | (75.0%) | 16 | (35.6%) | 5 | (50.0%) | |||
| 4 | 1 | (5.0%) | 1 | (2.7%) | 2 | (5.4%) | 5 | (17.9%) | 10 | (22.2%) | 5 | (50.0%) | |||
| Cardiac ultrasonography | |||||||||||||||
| Left ventricular ejection fraction (%) | 59.3 | ±5.0 | 57.8 | ±7.1 | 0.357 | 53.6 | ±10.5 | 49.8 | ±11.7 | 0.227 | 48.1 | ±12.8 | 46.2 | ±14.4 | 0.654 |
| Aortic valve area (cm2) | 0.8 | ±0.1 | 0.8 | ±0.2 | 0.514 | 0.8 | ±0.2 | 0.8 | ±0.3 | 0.268 | 0.8 | ±0.2 | 0.9 | ±0.1 | 0.027 * |
| Mean pressure gradient (mmHg) | 54.4 | ±22.6 | 58.7 | ±21.2 | 0.349 | 44.4 | ±14.4 | 54.2 | ±24.9 | 0.081 | 44.7 | ±17.5 | 49.8 | ±17.2 | 0.341 |
| PA systolic pressure (mmHg) | 34.6 | ±11.6 | 38.6 | ±14.1 | 0.417 | 43.4 | ±14.8 | 39.2 | ±12.4 | 0.286 | 42.4 | ±15.0 | 46.2 | ±11.8 | 0.365 |
| Mitral regurgitation | 0.482 | 0.017 * | 0.124 | ||||||||||||
| 0 | 1 | (5.0%) | 2 | (5.4%) | 0 | (0%) | 1 | (3.6%) | 1 | (2.2%) | 0 | (0%) | |||
| 1 | 13 | (65.0%) | 18 | (48.6%) | 27 | (73.0%) | 10 | (35.7%) | 32 | (71.1%) | 5 | (50.0%) | |||
| 2 | 6 | (30.0%) | 17 | (45.9%) | 10 | (27.0%) | 16 | (57.1%) | 12 | (26.7%) | 4 | (40.0%) | |||
| 3 | 0 | (0%) | 0 | (0%) | 0 | (0%) | 1 | (3.6%) | 0 | (0%) | 1 | (10.0%) | |||
| Clinical history | |||||||||||||||
| Diabetes mellitus | 4 | (20.0%) | 15 | (40.5%) | 0.116 | 11 | (29.7%) | 11 | (39.3%) | 0.420 | 16 | (35.6%) | 5 | (50.0%) | 0.480 |
| Dyslipidemia f | 5 | (25.0%) | 8 | (21.6%) | 0.754 | 7 | (18.9%) | 9 | (32.1%) | 0.220 | 13 | (28.9%) | 2 | (20.0%) | 0.710 |
| Hypertension | 14 | (70.0%) | 25 | (67.6%) | 0.850 | 22 | (59.5%) | 21 | (75.0%) | 0.190 | 35 | (77.8%) | 7 | (70.0%) | 0.685 |
| Atrial fibrillation f | 4 | (20.0%) | 6 | (16.2%) | 0.728 | 10 | (27.0%) | 5 | (17.9%) | 0.385 | 17 | (37.8%) | 4 | (40.0%) | 1.000 |
| Pacemaker | 0 | (0%) | 0 | (0%) | --- | 2 | (5.4%) | 1 | (3.6%) | 1.000 | 1 | (2.2%) | 0 | (0%) | 1.000 |
| COPD f | 3 | (15.0%) | 5 | (13.5%) | 1.000 | 9 | (24.3%) | 6 | (21.4%) | 0.784 | 12 | (26.7%) | 4 | (40.0%) | 0.453 |
| Smoker f | 1 | (5.0%) | 3 | (8.1%) | 1.000 | 6 | (16.2%) | 6 | (21.4%) | 0.592 | 6 | (13.3%) | 2 | (20.0%) | 0.627 |
| Old Stroke f | 2 | (10.0%) | 2 | (5.4%) | 0.607 | 2 | (5.4%) | 1 | (3.6%) | 1.000 | 8 | (17.8%) | 0 | (0%) | 0.326 |
| Uremia f | 2 | (10.0%) | 0 | (0%) | 0.119 | 0 | (0%) | 1 | (3.6%) | 0.431 | 14 | (31.1%) | 6 | (60.0%) | 0.144 |
| Cancer f | 3 | (15.0%) | 0 | (0%) | 0.039 * | 6 | (16.2%) | 2 | (7.1%) | 0.449 | 8 | (17.8%) | 0 | (0%) | 0.326 |
| PAOD | 0 | (0%) | 0 | (0%) | --- | 3 | (8.1%) | 3 | (10.7%) | 1.000 | 4 | (8.9%) | 2 | (20.0%) | 0.298 |
| Coronary artery disease | 7 | (35.0%) | 9 | (24.3%) | 0.392 | 22 | (59.5%) | 13 | (46.4%) | 0.297 | 31 | (68.9%) | 1 | (10.0%) | 0.001 ** |
| Previous MI f | 2 | (10.0%) | 1 | (2.7%) | 0.279 | 6 | (16.2%) | 6 | (21.4%) | 0.592 | 12 | (26.7%) | 1 | (10.0%) | 0.421 |
| s/p CABG | 0 | (0%) | 0 | (0%) | --- | 1 | (2.7%) | 0 | (0%) | 1.000 | 1 | (2.2%) | 0 | (0%) | 1.000 |
| Previous PCI f | 5 | (25.0%) | 2 | (5.4%) | 0.084 | 19 | (51.4%) | 7 | (25.0%) | 0.032 * | 26 | (57.8%) | 1 | (10.0%) | 0.012 * |
| PCI in last 12 months f | 5 | (25.0%) | 0 | (0%) | 0.004 ** | 13 | (35.1%) | 4 | (14.3%) | 0.058 | 24 | (53.3%) | 1 | (10.0%) | 0.015 * |
| Previous cardiac surgery f | 0 | (0%) | 1 | (2.7%) | 1.000 | 0 | (0%) | 0 | (0%) | --- | 1 | (2.2%) | 1 | (10.0%) | 0.333 |
| STS Score < 4% | STS Score 4–8% | STS Score > 8% | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcomes | TAVI (n = 20) | SAVR (n = 37) | p Value | TAVI (n = 37) | SAVR (n = 28) | p Value | TAVI (n = 45) | SAVR (n = 10) | p Value | ||||||
| Combined CABG | 0 | (0%) | 7 | (18.9%) | 0.045 * | 0 | (0%) | 6 | (21.4%) | 0.005 ** | 0 | (0%) | 0 | (0%) | --- |
| Intraoperative Complications f | |||||||||||||||
| Paravalvular leak | 8 | (40.0%) | 0 | (0%) | <0.001 ** | 10 | (27.0%) | 0 | (0%) | 0.007 ** | 19 | (42.2%) | 0 | (0%) | 0.010 * |
| Coronary occlusion | 0 | (0%) | 0 | (0%) | --- | 1 | (2.7%) | 0 | (0%) | 0 | (0%) | 0 | (0%) | --- | |
| Major bleeding | 0 | (0%) | 0 | (0%) | --- | 2 | (5.4%) | 3 | (10.7%) | 0.644 | 8 | (17.8%) | 0 | (0%) | 0.326 |
| Stoke | 0 | (0%) | 0 | (0%) | --- | 0 | (0%) | 0 | (0%) | --- | 1 | (2.2%) | 1 | (10.0%) | 0.333 |
| Major vascular complication f | 1 | (5.0%) | 0 | (0%) | 0.351 | 3 | (8.1%) | 1 | (3.6%) | 0.628 | 3 | (6.7%) | 0 | (0%) | 1.000 |
| Postoperative Complications | |||||||||||||||
| New pacemaker f | 3 | (15.0%) | 2 | (5.4%) | 0.332 | 6 | (16.2%) | 2 | (7.1%) | 0.449 | 8 | (18.2%) | 4 | (40.0%) | 0.203 |
| Re-on Endo f | 1 | (5.0%) | 0 | (0%) | 0.351 | 1 | (2.7%) | 3 | (10.7%) | 0.307 | 4 | (8.9%) | 2 | (20.0%) | 0.298 |
| Acute kidney injury f | 0 | (0%) | 4 | (10.8%) | 0.286 | 7 | (18.9%) | 7 | (25.0%) | 0.555 | 8 | (17.8%) | 3 | (30.0%) | 0.400 |
| Extubation in operation room | 16 | (80.0%) | 0 | (0%) | <0.001 ** | 16 | (43.2%) | 0 | (0%) | <0.001 ** | 12 | (26.7%) | 0 | (0%) | 0.096 |
| Ventilator (hour) | 4.3 | ±0.6 | 31.7 | ±62.3 | 0.001 ** | 36.8 | ±126.6 | 474.4 | ±1678.3 | <0.001 ** | 145.5 | ±397.8 | 183.6 | ±265.1 | 0.237 |
| ICU stay (h) | 107.0 | ±73.6 | 76.3 | ±65.4 | 0.012 * | 356.5 | ±1432.1 | 506.6 | ±1673.9 | 0.491 | 265.5 | ±467.6 | 268.2 | ±333.8 | 0.785 |
| Hospital stay (d) | 7.9 | ±5.9 | 10.4 | ±3.8 | 0.005 ** | 7.2 | ±7.7 | 17.2 | ±17.2 | <0.001 ** | 15.0 | ±24.1 | 22.5 | ±20.7 | 0.029* |
| In-Hospital Mortality f | 0 | (0%) | 1 | (2.7%) | 1.000 | 2 | (5.4%) | 2 | (7.1%) | 1.000 | 5 | (11.1%) | 3 | (30.0%) | 0.149 |
| Cardiac ultrasonography | |||||||||||||||
| Left ventricular ejection fraction (%) | 57.8 | ±5.5 | 56.4 | ±5.1 | 0.240 | 53.8 | ±8.7 | 55.9 | ±5.6 | 0.845 | 51.9 | ±9.1 | 63.0 | ±2.7 | 0.002 ** |
| Aortic valve area (cm2) | 1.8 | ±0.1 | 1.7 | ±0.3 | 0.265 | 1.8 | ±0.3 | 1.6 | ±0.3 | 0.052 | 1.8 | ±0.4 | 1.4 | ±0.2 | 0.012 * |
| Mean pressure gradient (mmHg) | 11.6 | ±4.5 | 14.8 | ±7.2 | 0.191 | 12.6 | ±8.6 | 14.6 | ±7.5 | 0.123 | 12.6 | ±7.0 | 15.0 | ±4.7 | 0.237 |
| PA systolic pressure (mmHg) | 35.1 | ±9.9 | 32.6 | ±7.9 | 0.478 | 40.8 | ±14.8 | 39.0 | ±14.4 | 0.475 | 44.6 | ±14.3 | 42.2 | ±15.2 | 0.889 |
| Follow-up time (year) | 3.4 | ±2.3 | 4.7 | ±3.2 | 0.155 | 2.6 | ±2.5 | 4.2 | ±2.6 | 0.012 * | 1.7 | ±1.8 | 2.2 | ±1.9 | 0.458 |
| Overall mortality f | 2 | (10.0%) | 8 | (21.6%) | 0.467 | 10 | (27.0%) | 12 | (42.9%) | 0.182 | 21 | (46.7%) | 9 | (90.0%) | 0.015 * |
| 1-year mortality f | 0 | (0%) | 2 | (5.4%) | 0.536 | 4 | (10.8%) | 2 | (7.1%) | 0.692 | 17 | (37.8%) | 3 | (30.0%) | 0.731 |
| 5-year mortality f | 2 | (10.0%) | 4 | (10.8%) | 1.000 | 10 | (27.0%) | 7 | (25.0%) | 0.854 | 21 | (46.7%) | 7 | (70.0%) | 0.295 |
| Re-Hospitalization f | 2 | (10.0%) | 8 | (21.6%) | 0.467 | 6 | (16.2%) | 6 | (21.4%) | 0.592 | 8 | (17.8%) | 3 | (30.0%) | 0.400 |
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95%CI | p Value | HR | 95%CI | p Value | |
| In-Hospital Mortality | ||||||
| Group | ||||||
| TAVI | 1.00 | |||||
| AVR | 0.88 | (0.29–2.66) | 0.814 | |||
| Gender | ||||||
| Female | 1.00 | 1.00 | ||||
| Male | 1.55 | (0.52–4.61) | 0.435 | 1.40 | (0.39–5.04) | 0.607 |
| STS score (%) | ||||||
| <4% | 1.00 | 1.00 | ||||
| 4–8% | 2.46 | (0.27–22.88) | 0.428 | 1.83 | (0.18–18.41) | 0.610 |
| >8% | 3.44 | (0.38–30.75) | 0.270 | 2.40 | (0.23–25.23) | 0.465 |
| LVEF | 0.96 | (0.93–1.00) | 0.062 | 0.97 | (0.93–1.02) | 0.283 |
| Diabetes mellitus | 3.24 | (1.05–9.98) | 0.040 * | 3.71 | (1.12–12.32) | 0.032 * |
| PAOD | 2.05 | (0.44–9.57) | 0.362 | 2.28 | (0.44–11.93) | 0.330 |
| 1-year Mortality | ||||||
| Group | ||||||
| TAVI | 1.00 | |||||
| AVR | 0.74 | (0.44–1.24) | 0.253 | |||
| Age | 1.07 | (1.01–1.13) | 0.028 * | 1.00 | (0.94–1.07) | 0.893 |
| Gender | ||||||
| Female | 1.00 | 1.00 | ||||
| Male | 2.42 | (1.14–5.18) | 0.022 * | 1.88 | (0.79–4.49) | 0.156 |
| BMI < 20 | 2.80 | (1.23–6.36) | 0.014 * | 1.03 | (0.40–2.67) | 0.954 |
| STS score (%) | ||||||
| <4% | 1.00 | 1.00 | ||||
| 4–8% | 2.74 | (0.55–13.59) | 0.217 | 1.79 | (0.33–9.78) | 0.499 |
| >8% | 12.57 | (2.94–53.83) | 0.001 ** | 6.03 | (1.20–30.46) | 0.030 * |
| LVEF | 0.97 | (0.94–0.995) | 0.021 * | 0.98 | (0.94–1.01) | 0.202 |
| Diabetes mellitus | 1.25 | (0.58–2.66) | 0.570 | |||
| PAOD | 1.94 | (0.59–6.44) | 0.277 | |||
| Re-on Endo | 11.20 | (4.89–25.66) | <0.001 ** | 4.19 | (1.48–11.89) | 0.007 ** |
| Acute kidney injury | 5.50 | (2.61–11.57) | <0.001 ** | 4.12 | (1.74–9.73) | 0.001 ** |
| 5-year Mortality | ||||||
| Group | ||||||
| TAVI | 1.00 | 1.00 | ||||
| AVR | 0.54 | (0.30–0.97) | 0.040 * | 0.81 | (0.38–1.71) | 0.576 |
| Age | 1.06 | (1.01–1.11) | 0.015 * | 1.01 | (0.95–1.08) | 0.689 |
| BMI < 20 | 2.25 | (1.18–4.31) | 0.014 * | 1.52 | (0.75–3.09) | 0.246 |
| STS score (%) | ||||||
| <4% | 1.00 | 1.00 | ||||
| 4–8% | 2.84 | (1.12–7.20) | 0.028 * | 1.69 | (0.61–4.66) | 0.311 |
| >8% | 8.13 | (3.34–19.77) | <0.001 ** | 3.13 | (1.01–9.74) | 0.048 * |
| LVEF | 0.97 | (0.95–0.99) | 0.015 * | 0.99 | (0.96–1.01) | 0.360 |
| Diabetes mellitus | 1.54 | (0.89–2.68) | 0.124 | |||
| PAOD | 2.91 | (1.23–6.88) | 0.015 * | 2.96 | (1.13–7.77) | 0.028 * |
| Re-on Endo | 8.30 | (3.98–17.29) | <0.001 ** | 3.87 | (1.53–9.82) | 0.004 ** |
| Acute kidney injury | 3.50 | (1.95–6.28) | <0.001 ** | 3.98 | (1.95–8.15) | 0.001 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, P.-H.; Wei, H.-J.; Hsieh, S.-R.; Tsai, H.-W.; Yu, C.-L.; Lee, W.-L.; Wu, Y.-S. One-Year and Five-Year Outcomes of Transcatheter Aortic Valve Replacement or Surgical Aortic Valve Replacement in a Taiwanese Elderly Population. J. Clin. Med. 2023, 12, 3429. https://doi.org/10.3390/jcm12103429
Lin P-H, Wei H-J, Hsieh S-R, Tsai H-W, Yu C-L, Lee W-L, Wu Y-S. One-Year and Five-Year Outcomes of Transcatheter Aortic Valve Replacement or Surgical Aortic Valve Replacement in a Taiwanese Elderly Population. Journal of Clinical Medicine. 2023; 12(10):3429. https://doi.org/10.3390/jcm12103429
Chicago/Turabian StyleLin, Po-Han, Hao-Ji Wei, Shih-Rong Hsieh, Hung-Wen Tsai, Chu-Leng Yu, Wen-Lieng Lee, and Yung-Szu Wu. 2023. "One-Year and Five-Year Outcomes of Transcatheter Aortic Valve Replacement or Surgical Aortic Valve Replacement in a Taiwanese Elderly Population" Journal of Clinical Medicine 12, no. 10: 3429. https://doi.org/10.3390/jcm12103429
APA StyleLin, P.-H., Wei, H.-J., Hsieh, S.-R., Tsai, H.-W., Yu, C.-L., Lee, W.-L., & Wu, Y.-S. (2023). One-Year and Five-Year Outcomes of Transcatheter Aortic Valve Replacement or Surgical Aortic Valve Replacement in a Taiwanese Elderly Population. Journal of Clinical Medicine, 12(10), 3429. https://doi.org/10.3390/jcm12103429





