Corneal Confocal Microscopy Identifies People with Type 1 Diabetes with More Rapid Corneal Nerve Fibre Loss and Progression of Neuropathy
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of Patients
2.2. Anthropometric and Biochemistry Measures
2.3. Neuropathy Assessments
2.4. Quantitative Sensory Testing (QST)
2.5. Nerve Conduction Studies (NCS)
2.6. Corneal Sensitivity
2.7. Corneal Confocal Microscopy (CCM)
2.8. Skin Biopsy and Immunohistochemistry
2.9. Rapid Corneal Nerve Fiber Loss (RCNFL)
2.10. Statistical Analysis
2.11. Sample Size
3. Results
3.1. Clinical and Metabolic Data
3.1.1. Baseline
3.1.2. Follow-Up
3.2. Diabetic Neuropathy Assessments
3.2.1. Baseline
3.2.2. Follow-Up
3.2.3. Rapid Corneal Nerve Fiber Loss (RCNFL)
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Iqbal, Z.; Azmi, S.; Yadav, R.; Ferdousi, M.; Kumar, M.; Cuthbertson, D.; Lim, J.; Malik, R.A.; Alam, U. Diabetic Peripheral Neuropathy: Epidemiology, Diagnosis, and Pharmacotherapy. Clin. Ther. 2018, 40, 828–849. [Google Scholar] [CrossRef] [PubMed]
- Adler, I.A.; Boyko, E.J.; Ahroni, J.H.; Smith, D.G. Lower-extremity amputation in diabetes. The independent effects of peripheral vascular disease, sensory neuropathy, and foot ulcers. Diabetes Care 1999, 22, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Calles-Escandon, J.; Lovato, L.C.; Simons-Morton, D.G.; Kendall, D.M.; Pop-Busui, R.; Cohen, R.M.; Bonds, D.E.; Fonseca, V.A.; Ismail-Beigi, F.; Banerji, M.A.; et al. Effect of intensive compared with standard glycemia treatment strategies on mortality by baseline subgroup characteristics: The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Diabetes Care 2010, 33, 721–727. [Google Scholar] [CrossRef]
- Elliott, J.; Tesfaye, S.; Chaturvedi, N.; Gandhi, R.A.; Stevens, L.K.; Emery, C.; Fuller, J.H.; EURODIAB Prospective Complications Study Group. Large-Fiber Dysfunction in Diabetic Peripheral Neuropathy Is Predicted by Cardiovascular Risk Factors. Diabetes Care 2009, 32, 1896–1900. [Google Scholar] [CrossRef] [PubMed]
- Tesfaye, S.; Chaturvedi, N.; Eaton, S.E.; Ward, J.D.; Manes, C.; Ionescu-Tirgoviste, C.; Witte, D.; Fuller, J.H. Vascular Risk Factors and Diabetic Neuropathy. N. Engl. J. Med. 2005, 352, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Boulton, A.J. Whither clinical research in diabetic sensorimotor peripheral neuropathy? Problems of end point selection for clinical trials. Diabetes Care 2007, 30, 2752–2753. [Google Scholar] [CrossRef][Green Version]
- Malik, R.A. Chapter Fourteen—Wherefore Art Thou, O Treatment for Diabetic Neuropathy? In International Review of Neurobiology; Nigel, A.C., Paul, F., Eds.; Academic Press: Cambridge, MA, USA, 2016; pp. 287–317. [Google Scholar]
- Ziegler, D.; Nowak, H.; Kempler, P.; Vargha, P.; Low, P.A. Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: A meta-analysis. Diabet. Med. 2004, 21, 114–121. [Google Scholar] [CrossRef]
- Tesfaye, S.; Tandan, R.; Bastyr, E.J.; Kles, K.A.; Skljarevski, V.; Price, K.L.; for the Ruboxistaurin Study Group. Factors That Impact Symptomatic Diabetic Peripheral Neuropathy in Placebo-Administered Patients from Two 1-Year Clinical Trials. Diabetes Care 2007, 30, 2626–2632. [Google Scholar] [CrossRef]
- The Diabetes Control and Complications Trial Research Group. The effect of intensive diabetes therapy on the development and progression of neuropathy. Ann. Intern. Med. 1995, 122, 561–568. [Google Scholar] [CrossRef]
- Partanen, J.; Niskanen, L.; Lehtinen, J.; Mervaala, E.; Siitonen, O.; Uusitupa, M. Natural History of Peripheral Neuropathy in Patients with Non-Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1995, 333, 89–94. [Google Scholar] [CrossRef]
- Diabetes Control and Complications Trial Research Group. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Albers, J.W.; Herman, W.H.; Pop-Busui, R.; Feldman, E.L.; Martin, C.L.; Cleary, P.A.; Waberski, B.H.; Lachin, J.M.; DCCT/EDIC Research Group. Effect of Prior Intensive Insulin Treatment during the Diabetes Control and Complications Trial (DCCT) on Peripheral Neuropathy in Type 1 Diabetes during the Epidemiology of Diabetes Interventions and Complications (EDIC) Study. Diabetes Care 2010, 33, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.R.; Williamson, S.; Abbott, C.; Carrington, A.L.; Iqbal, J.; Schady, W.; Boulton, A.J. Effect of angiotensin-converting-enzyme (ACE) inhibitor trandolapril on human diabetic neuropathy: Randomised double-blind controlled trial. Lancet 1998, 352, 1978–1981. [Google Scholar] [CrossRef]
- Davis, T.; Yeap, B.B.; Davis, W.; Bruce, D. Lipid-lowering therapy and peripheral sensory neuropathy in type 2 diabetes: The Fremantle Diabetes Study. Diabetologia 2008, 51, 562–566. [Google Scholar] [CrossRef] [PubMed]
- Perkins, B.A.; Dholasania, A.; Buchanan, R.A.; Bril, V. Short-term metabolic change is associated with improvement in measures of diabetic neuropathy: A 1-year placebo cohort analysis. Diabet. Med. 2010, 27, 1271–1279. [Google Scholar] [CrossRef] [PubMed]
- Pittenger, G.L.; Ray, M.; Burcus, N.I.; McNulty, P.; Basta, B.; Vinik, A.I. Intraepidermal Nerve Fibers Are Indicators of Small-Fiber Neuropathy in Both Diabetic and Nondiabetic Patients. Diabetes Care 2004, 27, 1974–1979. [Google Scholar] [CrossRef]
- Vas, P.R.J.; Rayman, G. The Rate of Decline in Small Fibre Function Assessed Using Axon Reflex-Mediated Neurogenic Vasodilatation and the Importance of Age Related Centile Values to Improve the Detection of Clinical Neuropathy. PLoS ONE 2013, 8, e69920. [Google Scholar] [CrossRef]
- Smith, A.G.; Russell, J.; Feldman, E.L.; Goldstein, J.; Peltier, A.; Smith, S.; Hamwi, J.; Pollari, D.; Bixby, B.; Howard, J.; et al. Lifestyle Intervention for Pre-Diabetic Neuropathy. Diabetes Care 2006, 29, 1294–1299. [Google Scholar] [CrossRef]
- Azmi, S.; Jeziorska, M.; Ferdousi, M.; Petropoulos, I.N.; Ponirakis, G.; Marshall, A.; Alam, U.; Asghar, O.; Atkinson, A.; Jones, W.; et al. Early nerve fibre regeneration in individuals with type 1 diabetes after simultaneous pancreas and kidney transplantation. Diabetologia 2019, 62, 1478–1487. [Google Scholar] [CrossRef]
- Tavakoli, M.; Mitu-Pretorian, M.; Petropoulos, I.N.; Fadavi, H.; Asghar, O.; Alam, U.; Ponirakis, G.; Jeziorska, M.; Marshall, A.; Efron, N.; et al. Corneal Confocal Microscopy Detects Early Nerve Regeneration in Diabetic Neuropathy After Simultaneous Pancreas and Kidney Transplantation. Diabetes 2013, 62, 254–260. [Google Scholar] [CrossRef]
- Dehghani, C.; Pritchard, N.; Edwards, K.; Russell, A.W.; Malik, R.A.; Efron, N. Risk Factors Associated with Corneal Nerve Alteration in Type 1 Diabetes in the Absence of Neuropathy: A Longitudinal In Vivo Corneal Confocal Microscopy Study. Cornea 2016, 35, 847–852. [Google Scholar] [CrossRef] [PubMed]
- Misra, S.L.; Slater, J.A.; McGhee, C.N.J.; Pradhan, M.; Braatvedt, G.D. Corneal Confocal Microscopy in Type 1 Diabetes Mellitus: A Six-Year Longitudinal Study. Transl. Vis. Sci. Technol. 2022, 11, 17. [Google Scholar] [CrossRef] [PubMed]
- Perkins, B.A.; Lovblom, L.E.; Lewis, E.J.; Bril, V.; Ferdousi, M.; Orszag, A.; Edwards, K.; Pritchard, N.; Russell, A.; Dehghani, C.; et al. Corneal Confocal Microscopy Predicts the Development of Diabetic Neuropathy: A Longitudinal Diagnostic Multinational Consortium Study. Diabetes Care 2021, 44, 2107–2114. [Google Scholar] [CrossRef] [PubMed]
- Lewis, E.J.; Lovblom, L.E.; Ferdousi, M.; Halpern, E.M.; Jeziorska, M.; Pacaud, D.; Pritchard, N.; Dehghani, C.; Edwards, K.; Srinivasan, S.; et al. Rapid Corneal Nerve Fiber Loss: A Marker of Diabetic Neuropathy Onset and Progression. Diabetes Care 2020, 43, 1829–1835. [Google Scholar] [CrossRef]
- Young, M.J.; Boulton, A.J.M.; MacLeod, A.F.; Williams, D.R.R.; Sonksen, P.H. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia 1993, 36, 150–154. [Google Scholar] [CrossRef]
- Tesfaye, S.; Boulton, A.J.M.; Dyck, P.J.; Freeman, R.; Horowitz, M.; Kempler, P.; Lauria, G.; Malik, R.A.; Spallone, V.; Vinik, A.; et al. Diabetic Neuropathies: Update on Definitions, Diagnostic Criteria, Estimation of Severity, and Treatments. Diabetes Care 2010, 33, 2285–2293. [Google Scholar] [CrossRef]
- Bravenboer, B.; van Dam, P.; Hop, J.; Steenhoven, J.V.; Erkelens, D. Thermal Threshold Testing for the Assessment of Small Fibre Dysfunction: Normal Values and Reproducibility. Diabet. Med. 1992, 9, 546–549. [Google Scholar] [CrossRef]
- Petropoulos, I.N.; Manzoor, T.; Morgan, P.; Fadavi, H.; Asghar, O.; Alam, U.; Ponirakis, G.; Dabbah, M.A.; Chen, X.; Graham, J.; et al. Repeatability of In Vivo Corneal Confocal Microscopy to Quantify Corneal Nerve Morphology. Cornea 2013, 32, e83–e89. [Google Scholar] [CrossRef]
- Dabbah, M.; Graham, J.; Petropoulos, I.; Tavakoli, M.; Malik, R. Automatic analysis of diabetic peripheral neuropathy using multi-scale quantitative morphology of nerve fibres in corneal confocal microscopy imaging. Med. Image Anal. 2011, 15, 738–747. [Google Scholar] [CrossRef]
- Dabbah, M.A.; Graham, J.; Petropoulos, I.; Tavakoli, M.; Malik, R.A. Dual-Model Automatic Detection of Nerve-Fibres in Corneal Confocal Microscopy Images. Med. Image Comput. Comput. Assist. Interv. 2010, 13 Pt 1, 300–307. [Google Scholar] [CrossRef]
- Alam, U.; Jeziorska, M.; Petropoulos, I.N.; Asghar, O.; Fadavi, H.; Ponirakis, G.; Marshall, A.; Tavakoli, M.; Boulton, A.J.M.; Efron, N.; et al. Diagnostic utility of corneal confocal microscopy and intra-epidermal nerve fibre density in diabetic neuropathy. PLoS ONE 2017, 12, e0180175. [Google Scholar] [CrossRef] [PubMed]
- Lauria, G.; Bakkers, M.; Schmitz, C.; Lombardi, R.; Penza, P.; Devigili, G.; Smith, A.G.; Hsieh, S.-T.; Mellgren, S.I.; Umapathi, T.; et al. Intraepidermal nerve fiber density at the distal leg: A worldwide normative reference study. J. Peripher. Nerv. Syst. 2010, 15, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Pfau, D.B.; Krumova, E.K.; Treede, R.-D.; Baron, R.; Toelle, T.; Birklein, F.; Eich, W.; Geber, C.; Gerhardt, A.; Weiss, T.; et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): Reference data for the trunk and application in patients with chronic postherpetic neuralgia. Pain 2014, 155, 1002–1015. [Google Scholar] [CrossRef] [PubMed]
- Weisman, A.; Bril, V.; Ngo, M.; Lovblom, L.E.; Halpern, E.M.; Orszag, A.; Perkins, B.A. Identification and Prediction of Diabetic Sensorimotor Polyneuropathy Using Individual and Simple Combinations of Nerve Conduction Study Parameters. PLoS ONE 2013, 8, e58783. [Google Scholar] [CrossRef]
- Vinik, A.I.; Bril, V.; Litchy, W.J.; Price, K.L.; Bastyr, E.J.; MBBQ Study Group. Sural sensory action potential identifies diabetic peripheral neuropathy responders to therapy. Muscle Nerve 2005, 32, 619–625. [Google Scholar] [CrossRef]
- Carrington, A.L.; Shaw, J.E.; Van Schie, C.H.; Abbott, C.A.; Vileikyte, L.; Boulton, A.J. Can Motor Nerve Conduction Velocity Predict Foot Problems in Diabetic Subjects over a 6-Year Outcome Period? Diabetes Care 2002, 25, 2010–2015. [Google Scholar] [CrossRef]
- Lovblom, L.E.; Halpern, E.M.; Wu, T.; Kelly, D.; Ahmed, A.; Boulet, G.; Orszag, A.; Ng, E.; Ngo, M.; Bril, V.; et al. In Vivo Corneal Confocal Microscopy and Prediction of Future-Incident Neuropathy in Type 1 Diabetes: A Preliminary Longitudinal Analysis. Can. J. Diabetes 2015, 39, 390–397. [Google Scholar] [CrossRef]
- Jiang, M.-S.; Yuan, Y.; Gu, Z.-X.; Zhuang, S.-L. Corneal confocal microscopy for assessment of diabetic peripheral neuropathy: A meta-analysis. Br. J. Ophthalmol. 2015, 100, 9–14. [Google Scholar] [CrossRef]
- Breiner, A.; Lovblom, L.E.; Perkins, B.A.; Bril, V. Response to Comment on Breiner et al. Does the Prevailing Hypothesis That Small-Fiber Dysfunction Precedes Large-Fiber Dysfunction Apply to Type 1 Diabetic Patients? Diabetes Care 2014, 37, 1418–1424. [Google Scholar] [CrossRef]
- Gibbons, C.H.; Freeman, R.; Tecilazich, F.; Dinh, T.; Lyons, T.E.; Gnardellis, C.; Veves, A. The evolving natural history of neurophysiologic function in patients with well-controlled diabetes. J. Peripher. Nerv. Syst. 2013, 18, 153–161. [Google Scholar] [CrossRef]
- Dehghani, C.; Russell, A.W.; Perkins, B.A.; Malik, R.A.; Pritchard, N.; Edwards, K.; Shahidi, A.M.; Srinivasan, S.; Efron, N. A rapid decline in corneal small fibers and occurrence of foot ulceration and Charcot foot. J. Diabetes Its Complicat. 2016, 30, 1437–1439. [Google Scholar] [CrossRef] [PubMed]
- Mehra, S.; Tavakoli, M.; Kallinikos, P.A.; Efron, N.; Boulton, A.J.; Augustine, T.; Malik, R.A. Corneal Confocal Microscopy Detects Early Nerve Regeneration after Pancreas Transplantation in Patients with Type 1 Diabetes. Diabetes Care 2007, 30, 2608–2612. [Google Scholar] [CrossRef] [PubMed]
- Azmi, S.; Ferdousi, M.; Petropoulos, I.N.; Ponirakis, G.; Fadavi, H.; Tavakoli, M.; Alam, U.; Jones, W.; Marshall, A.; Jeziorska, M.; et al. Corneal Confocal Microscopy Shows an Improvement in Small-Fiber Neuropathy in Subjects with Type 1 Diabetes on Continuous Subcutaneous Insulin Infusion Compared with Multiple Daily Injection. Diabetes Care 2015, 38, e3–e4. [Google Scholar] [CrossRef] [PubMed]
- Brines, M.; Dunne, A.N.; Van Velzen, M.; Proto, P.L.; Ostenson, C.-G.; Kirk, R.I.; Petropoulos, I.N.; Javed, S.; Malik, R.A.; Cerami, A.; et al. ARA 290, a Nonerythropoietic Peptide Engineered from Erythropoietin, Improves Metabolic Control and Neuropathic Symptoms in Patients with Type 2 Diabetes. Mol. Med. 2014, 20, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Culver, D.A.; Dahan, A.; Bajorunas, D.; Jeziorska, M.; Van Velzen, M.; Aarts, L.P.H.J.; Tavee, J.; Tannemaat, M.R.; Dunne, A.N.; Kirk, R.I.; et al. Cibinetide Improves Corneal Nerve Fiber Abundance in Patients with Sarcoidosis-Associated Small Nerve Fiber Loss and Neuropathic Pain. Investig. Opthalmol. Vis. Sci. 2017, 58, BIO52–BIO60. [Google Scholar] [CrossRef]
- Lewis, E.J.H.; Perkins, B.A.; Lovblom, L.E.; Bazinet, R.P.; Wolever, T.M.; Bril, V. Effect of omega-3 supplementation on neuropathy in type 1 diabetes: A 12-month pilot trial. Neurology 2017, 88, 2294–2301. [Google Scholar] [CrossRef]
- Britten-Jones, A.C.; Kamel, J.T.; Roberts, L.J.; Braat, S.; Craig, J.P.; MacIsaac, R.J.; Downie, L.E. Investigating the Neuroprotective Effect of Oral Omega-3 Fatty Acid Supplementation in Type 1 Diabetes (nPROOFS1): A Randomized Placebo-Controlled Trial. Diabetes 2021, 70, 1794–1806. [Google Scholar] [CrossRef]
| Control BL (n = 16) | Control FU (n = 16) | p | T1DM BL (n = 50) | T1DM FU (n = 50) | p | |
|---|---|---|---|---|---|---|
| Age (years) | 41.4 ± 11.4 | 48.2 ± 15.5 | ||||
| Gender (Male) (%) | 63 | 54 | ||||
| Duration of Diabetes (years) Median(IQR) | N/a | 33.1 ± 16.7 | ||||
| HbA1c (%) | 5.6 ± 0.3 | 5.3 ± 0.3 | 0.003 | 8.2 ± 1.3 * | 8.1 ± 1.6 | NS |
| HbA1c (mmol/mol) | 38.0 ± 3.3 | 34.8 ± 3.4 | 66.2 ± 14.3 * | 65.2 ± 17.1 | ||
| BMI (kg/m2) | 25.7 ± 4.2 | 24.7 ± 3.8 | NS | 26.9 ± 4.4 | 27.1 ± 4.7 | NS |
| T-CHL (mmol/L) | 5.1 ± 0.9 | 4.8 ± 0.7 | NS | 4.3 ± 0.9 ** | 4.3 ± 0.9 | NS |
| HDL-C (mmol/L) | 1.5 ± 0.3 | 1.5 ± 0.3 | NS | 1.7 ± 0.5 | 1.7 ± 0.5 | NS |
| Triglycerides | 1.4 ± 0.7 | 1.2 ± 0.5 | NS | 1.1 ± 0.7 | 1.1 ± 0.5 | NS |
| Systolic BP (mmHg) | 125 ± 21 | 120 ± 19 | 0.02 | 132 ± 18 | 131 ± 26 | NS |
| Diastolic BP (mmHg) | 75 ± 12 | 74 ± 11 | NS | 73 ± 8 | 66 ± 9 | 0.004 |
| eGFR (mL/min/1.73) | 86 ± 7 | 83 ± 7 | NS | 81 ± 19 | 75 ± 17 | 0.02 |
| Control BL (n = 16) | Control FU (n = 16) | p | T1DM BL (n = 50) | T1DM FU (n = 50) | p | |
|---|---|---|---|---|---|---|
| NDS (-/10) | 0.5 ± 1.1 * | 0.4 ± 1.1 | NS | 3.4 ± 3.5 ¥ | 3.3 ± 3.6 | NS |
| Median (IQR) | 0 (0–0) | 0 (0–0) | 2 (0–6) | 2 (0–6) | ||
| NSP (-/38) | 0.1 ± 0.25 ** | 0 | NS | 3.8 ± 5.3 ¥¥ | 4.1 ± 6.7 | NS |
| Median (IQR) | 0 (0–0) | 0 (0–0) | 1 (0–5) | 1 (0–5.5) | ||
| McGill VAS (-/10 cm) | 0.3 ± 1.25 † | 0 | NS | 2.3 ± 3.3 † | 1.5 ± 3.0 | NS |
| Median (IQR) | 0 (0–0) | 0 (0–0) | 0 (0–4) | 0 (0–0) | ||
| NCCA (mBar) | 0.6 ± 0.3 | 0.6 ± 0.4 | NS | 1.4 ± 2.3 †† | 1.5 ± 2.3 | NS |
| CNFD (no./mm2) | 30.1 ± 4.9 | 28.3 ± 5.5 | NS | 19.5 ± 9.1 * | 18.7 ± 9.9 | NS |
| CNBD (no/mm2) | 36.6 ± 15.5 | 39.3 ± 18.0 | NS | 23.9 ± 15.0 ** | 22.6 ± 15.8 | NS |
| CNFL (mm/mm2) | 16.9 ± 2.8 | 16.6 ± 3.0 | NS | 12.0 ± 4.6 *** | 12.1 ± 5.0 | NS |
| CST (°C) | 28.6 ± 2.1 | 26.8 ± 4.8 | NS | 24.8 ± 6.9 ˚ | 22.5 ± 8.4 | 0.02 |
| WST (°C) | 37.6 ± 3.5 | 38.9 ± 3.8 | NS | 39.6 ± 4.6 | 40.2 ± 5.7 | NS |
| IENFD (no/mm) | 7.4 ± 4.8 | 7.4 ± 5.0 | NS | 5.8 ± 4.0 | 5.3 ± 3.5 | NS |
| (n = 4) | (n = 4) | (n = 28) | (n = 28) | |||
| VPT (volts) | 5.3 ± 4.8 | 6.0 ± 5.2 | NS | 15.5 ± 13.6 ª | 15.9 ± 12.6 | NS |
| SSNCV (m/s) | 49.4 ± 3.9 | 48.1 ± 4.7 | NS | 43.6 ± 6.3 f | 41.3 ± 6.4 | NS |
| SSNAmp (µV) | 21.0 ± 10.8 | 18.6 ± 8.7 | NS | 10.1 ± 6.7 ff | 8.7 ± 6.8 | NS |
| PMNCV (m/s) | 47.8 ± 3.6 | 47.3 ± 4.2 | NS | 40.6 ± 7.0 ^ | 40.0 ± 6.6 | NS |
| PMNAmp (mV) | 6.0 ± 1.6 | 5.8 ± 1.2 | NS | 3.4 ± 2.4 ^^ | 3.2 ± 2.0 | NS |
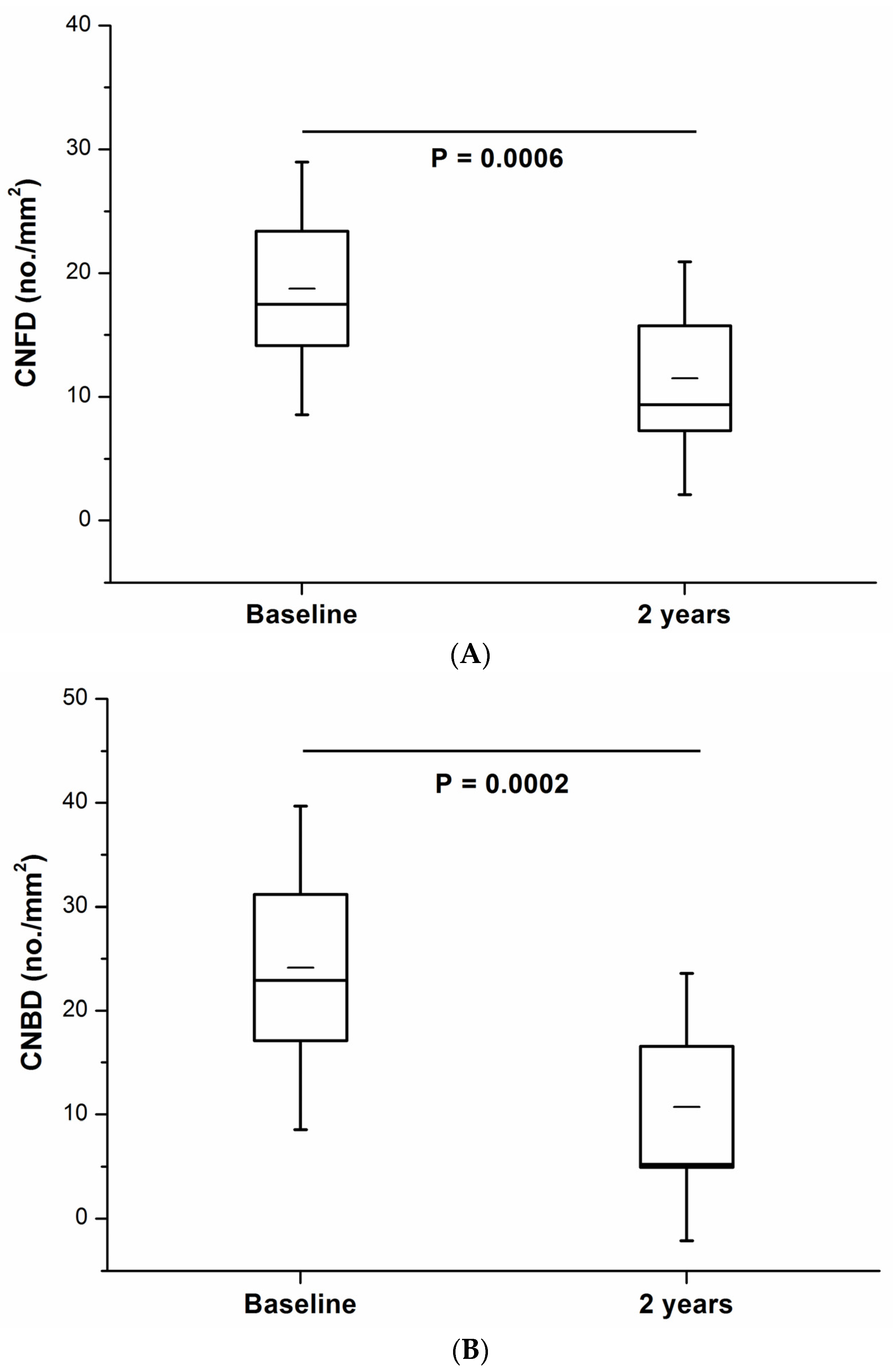
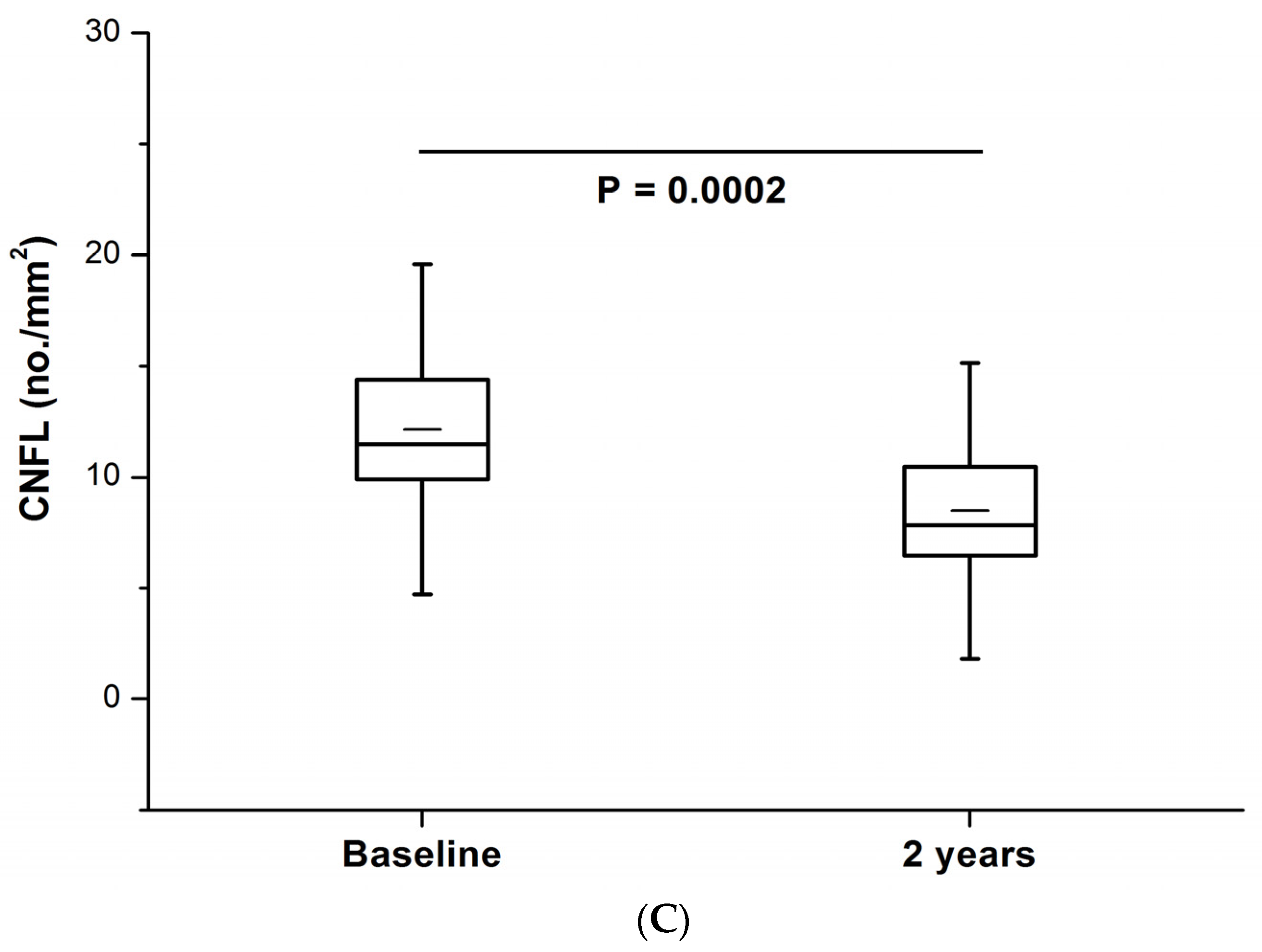
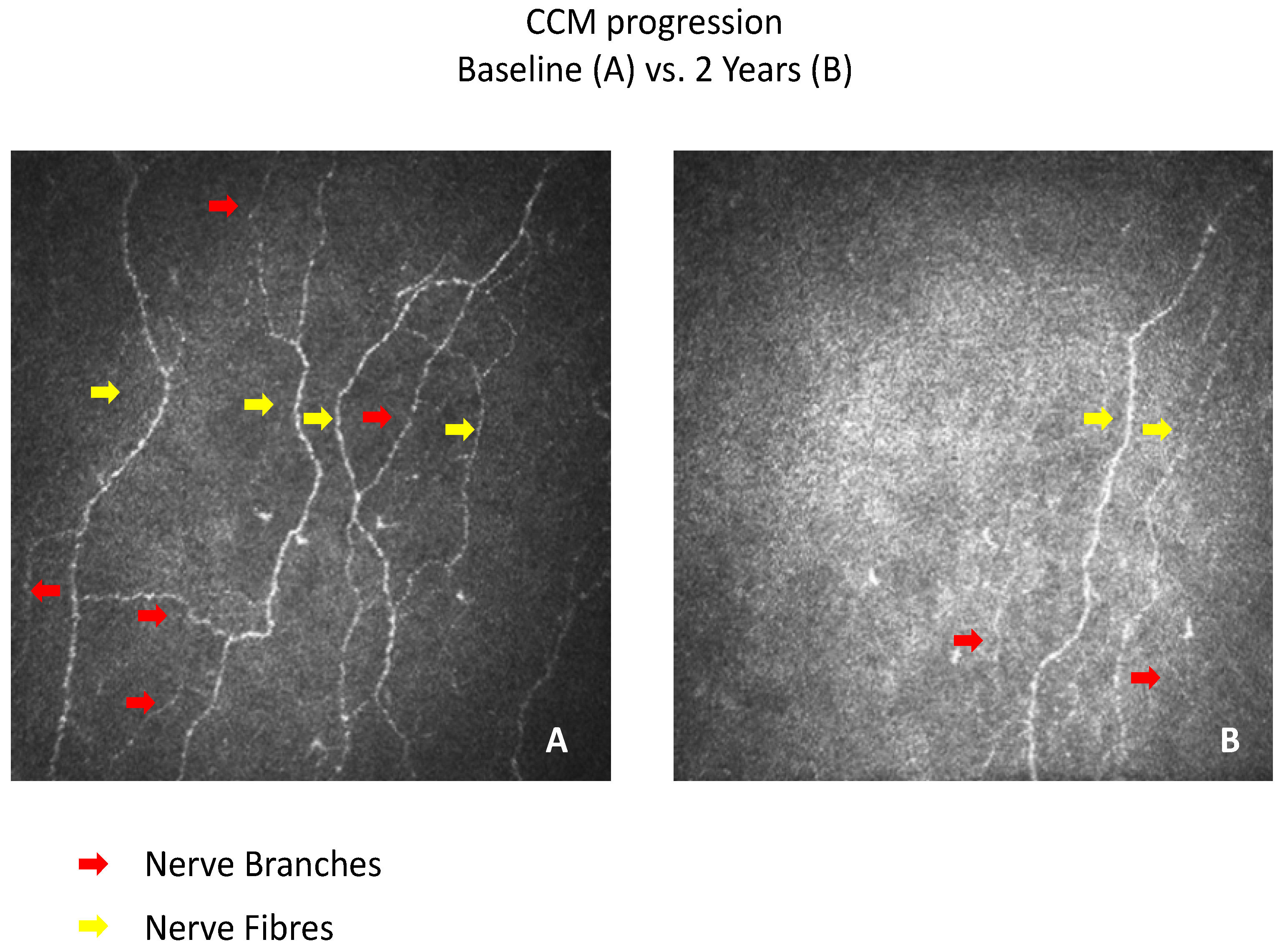
| T1DM BL (n = 11) | T1DM FU (n = 11) | p | |
|---|---|---|---|
| Age (years) | 54.8 ± 9.2 | N/a | - |
| HbA1c (%) | 7.9 ± 0.6 | 7.7 ± 1.0 | NS |
| HbA1c (mmol/mol) | 63 ± 6 | 61 ± 11 | NS |
| BMI (kg/m2) | 27.9 ± 3.3 | 28.8 ± 4.3 | NS |
| T-CHL (mmol/L) | 4.6 ± 1.2 | 4.6 ± 1.3 | NS |
| Systolic BP (mmHg) | 141 ± 20 | 132 ± 24 | NS |
| CNFD (no/mm2) | 18.8 ± 10.2 | 11.5 ± 9.4 | 0.0006 |
| CNBD (no/mm2) | 24.1 ± 15.6 | 10.7 ± 12.8 | 0.0002 |
| CNFL (mm/mm2) | 12.1 ± 5.0 | 8.5 ± 4.5 | 0.0002 |
| SSNCV (m/s) | 42.7 ± 6.1 | 38.1 ± 7.0 | 0.04 |
| SSNAmp (µV) | 9.3 ± 8.7 | 6.3 ± 5.8 | NS |
| PMNCV (m/s) | 42.4 ± 3.3 | 41.1 ± 4.2 | 0.05 |
| PMNAmp (mV) | 2.8 ± 2.1 | 3.0 ± 1.5 | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, U.; Ponirakis, G.; Asghar, O.; Petropoulos, I.N.; Azmi, S.; Jeziorska, M.; Marshall, A.; Boulton, A.J.M.; Efron, N.; Malik, R.A. Corneal Confocal Microscopy Identifies People with Type 1 Diabetes with More Rapid Corneal Nerve Fibre Loss and Progression of Neuropathy. J. Clin. Med. 2022, 11, 2249. https://doi.org/10.3390/jcm11082249
Alam U, Ponirakis G, Asghar O, Petropoulos IN, Azmi S, Jeziorska M, Marshall A, Boulton AJM, Efron N, Malik RA. Corneal Confocal Microscopy Identifies People with Type 1 Diabetes with More Rapid Corneal Nerve Fibre Loss and Progression of Neuropathy. Journal of Clinical Medicine. 2022; 11(8):2249. https://doi.org/10.3390/jcm11082249
Chicago/Turabian StyleAlam, Uazman, Georgios Ponirakis, Omar Asghar, Ioannis N. Petropoulos, Shazli Azmi, Maria Jeziorska, Andrew Marshall, Andrew J. M. Boulton, Nathan Efron, and Rayaz A. Malik. 2022. "Corneal Confocal Microscopy Identifies People with Type 1 Diabetes with More Rapid Corneal Nerve Fibre Loss and Progression of Neuropathy" Journal of Clinical Medicine 11, no. 8: 2249. https://doi.org/10.3390/jcm11082249
APA StyleAlam, U., Ponirakis, G., Asghar, O., Petropoulos, I. N., Azmi, S., Jeziorska, M., Marshall, A., Boulton, A. J. M., Efron, N., & Malik, R. A. (2022). Corneal Confocal Microscopy Identifies People with Type 1 Diabetes with More Rapid Corneal Nerve Fibre Loss and Progression of Neuropathy. Journal of Clinical Medicine, 11(8), 2249. https://doi.org/10.3390/jcm11082249






