Markers of Subclinical Atherosclerosis in Severe Obesity and One Year after Bariatric Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Echocardiographic Protocol
2.3. Laboratory Analyses
2.4. Statistical Analyses
2.5. Patient and Public Involvement
3. Results
3.1. Clinical Characteristics
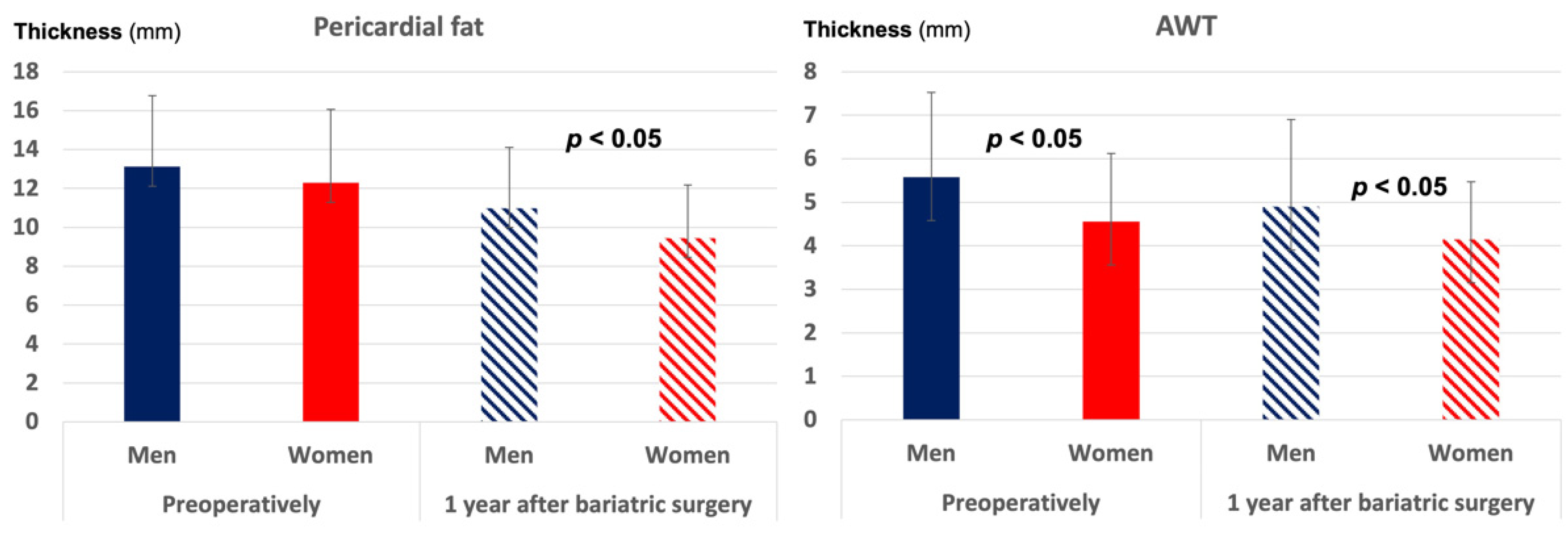
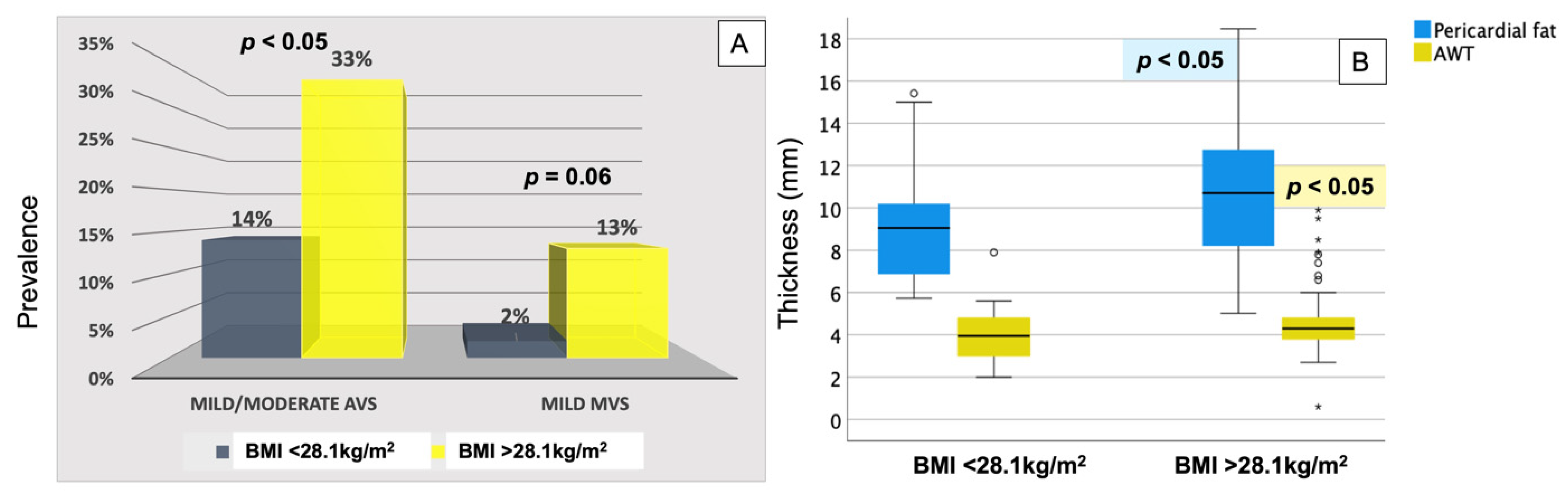
3.2. Preoperative Markers of Atherosclerosis
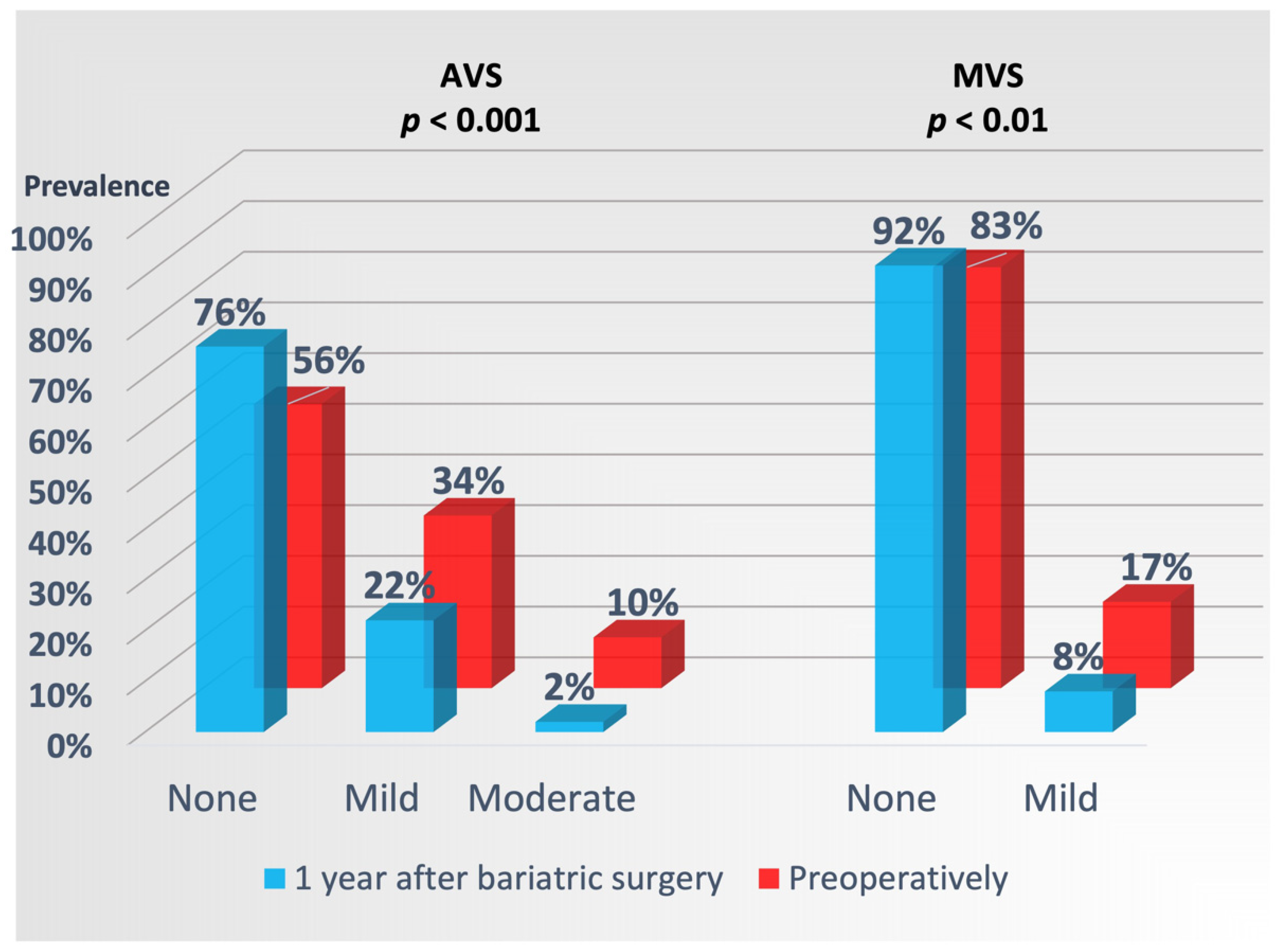
3.3. Markers of Atherosclerosis 1 Year after Bariatric Surgery
4. Discussion
4.1. Valve Sclerosis in Severe Obesity and after Bariatric Surgery
4.2. Pericardial Fat in Severe Obesity and after Bariatric Surgery
4.3. Aortic Wall Changes in Severe Obesity and after Bariatric Surgery
4.4. Clinical Implications
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- McGill, H.C., Jr.; Herderick, E.E.; McMahan, C.A.; Zieske, A.W.; Malcolm, G.T.; Tracy, R.E.; Strong, J.P. Atherosclerosis in youth. Minerva Pediatr. 2002, 54, 437–447. [Google Scholar] [PubMed]
- Rocha, V.Z.; Libby, P. Obesity, inflammation, and atherosclerosis. Nat. Rev. Cardiol. 2009, 6, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Abraham, T.M.; Pedley, A.; Massaro, J.M.; Hoffmann, U.; Fox, C.S. Association between visceral and subcutaneous adipose depots and incident cardiovascular disease risk factors. Circulation 2015, 132, 1639–1647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffmann, U.; Massaro, J.M.; D’Agostino, R.B., Sr.; Kathiresan, S.; Fox, C.S.; O’Donnell, C.J. Cardiovascular Event Prediction and Risk Reclassification by Coronary, Aortic, and Valvular Calcification in the Framingham Heart Study. J. Am. Heart Assoc. 2016, 5, e003144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polonsky, T.S.; McClelland, R.L.; Jorgensen, N.W.; Bild, D.E.; Burke, G.L.; Guerci, A.D.; Greenland, P. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010, 303, 1610–1616. [Google Scholar] [CrossRef]
- Kaltoft, M.; Langsted, A.; Nordestgaard, B.G. Obesity as a Causal Risk Factor for Aortic Valve Stenosis. J. Am. Coll. Cardiol. 2020, 75, 163–176. [Google Scholar] [CrossRef]
- Moreira, A.G.; Nicolini, A.C.; Gaio, E.J.; Visioli, F.; Rosing, C.K.; Cavagni, J. Effect of Obesity and/or Ligature-induced Periodontitis on Aortic Wall Thickness in Wistar Rats. Acta Odontol. Latinoam. 2020, 33, 50–55. [Google Scholar] [CrossRef]
- Bos, D.; Shahzad, R.; van Walsum, T.; van Vliet, L.J.; Franco, O.H.; Hofman, A.; Niessen, W.J.; Vernooij, M.W.; van der Lugt, A. Epicardial fat volume is related to atherosclerotic calcification in multiple vessel beds. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 1264–1269. [Google Scholar] [CrossRef] [Green Version]
- Eroglu, S.; Sade, L.E.; Yildirir, A.; Bal, U.; Ozbicer, S.; Ozgul, A.S.; Bozbas, H.; Aydinalp, A.; Muderrisoglu, H. Epicardial adipose tissue thickness by echocardiography is a marker for the presence and severity of coronary artery disease. Nutr. Metab. Cardiovasc. Dis. 2009, 19, 211–217. [Google Scholar] [CrossRef]
- Sicari, R.; Sironi, A.M.; Petz, R.; Frassi, F.; Chubuchny, V.; De Marchi, D.; Positano, V.; Lombardi, M.; Picano, E.; Gastaldelli, A. Pericardial rather than epicardial fat is a cardiometabolic risk marker: An MRI vs echo study. J. Am. Soc. Echocardiogr. 2011, 24, 1156–1162. [Google Scholar] [CrossRef] [Green Version]
- Goeller, M.; Achenbach, S.; Cadet, S.; Kwan, A.C.; Commandeur, F.; Slomka, P.J.; Gransar, H.; Albrecht, M.H.; Tamarappoo, B.K.; Berman, D.S.; et al. Pericoronary Adipose Tissue Computed Tomography Attenuation and High-Risk Plaque Characteristics in Acute Coronary Syndrome Compared with Stable Coronary Artery Disease. JAMA Cardiol. 2018, 3, 858–863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kenchaiah, S.; Ding, J.; Carr, J.J.; Allison, M.A.; Budoff, M.J.; Tracy, R.P.; Burke, G.L.; McClelland, R.L.; Arai, A.E.; Bluemke, D.A. Pericardial Fat and the Risk of Heart Failure. J. Am. Coll. Cardiol. 2021, 77, 2638–2652. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Tomita, T.; Kim, M.J.; Sasai, H.; Maeda, S.; Tanaka, K. Aerobic exercise training reduces epicardial fat in obese men. J. Appl. Physiol. 2009, 106, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Willens, H.J.; Byers, P.; Chirinos, J.A.; Labrador, E.; Hare, J.M.; de Marchena, E. Effects of weight loss after bariatric surgery on epicardial fat measured using echocardiography. Am. J. Cardiol. 2007, 99, 1242–1245. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Hashim, M.J.; Mustafa, H.; Baniyas, M.Y.; Al Suwaidi, S.; AlKatheeri, R.; Alblooshi, F.M.K.; Almatrooshi, M.; Alzaabi, M.E.H.; Al Darmaki, R.S.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, e9349. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, H.J.; Nedrebo, B.G.; Fossa, A.; Andersen, J.R.; Assmus, J.; Dagsland, V.H.; Dankel, S.N.; Gudbrandsen, O.A.; Ferno, J.; Hjellestad, I.; et al. Seven-year trajectories of body weight, quality of life and comorbidities following Roux-en-Y gastric bypass and sleeve gastrectomy. Int. J. Obes. 2022, 46, 739–749. [Google Scholar] [CrossRef]
- Grymyr, L.M.D.; Nadirpour, S.; Gerdts, E.; Nedrebo, B.G.; Hjertaas, J.J.; Matre, K.; Cramariuc, D. Left ventricular myocardial oxygen demand and subclinical dysfunction in patients with severe obesity referred for bariatric surgery. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 666–674. [Google Scholar] [CrossRef]
- Grymyr, L.M.D.; Nadirpour, S.; Gerdts, E.; Nedrebø, B.G.; Hjertaas, J.J.; Matre, K.; Cramariuc, D. One-year impact of bariatric surgery on left ventricular mechanics: Results from the prospective FatWest study. Eur. Heart J. Open 2021, 1, oeab024. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–270. [Google Scholar] [CrossRef]
- Gerdts, E.; Rossebo, A.B.; Pedersen, T.R.; Cioffi, G.; Lonnebakken, M.T.; Cramariuc, D.; Rogge, B.P.; Devereux, R.B. Relation of Left Ventricular Mass to Prognosis in Initially Asymptomatic Mild to Moderate Aortic Valve Stenosis. Circ. Cardiovasc. Imaging 2015, 8, e003644. [Google Scholar] [CrossRef] [Green Version]
- Thomassen, H.K.; Cioffi, G.; Gerdts, E.; Einarsen, E.; Midtbo, H.B.; Mancusi, C.; Cramariuc, D. Echocardiographic aortic valve calcification and outcomes in women and men with aortic stenosis. Heart 2017, 103, 1619–1624. [Google Scholar] [CrossRef] [PubMed]
- Davidovich, D.; Gastaldelli, A.; Sicari, R. Imaging cardiac fat. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 625–630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ding, J.; Hsu, F.C.; Harris, T.B.; Liu, Y.; Kritchevsky, S.B.; Szklo, M.; Ouyang, P.; Espeland, M.A.; Lohman, K.K.; Criqui, M.H.; et al. The association of pericardial fat with incident coronary heart disease: The Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Clin. Nutr. 2009, 90, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Faggiano, P.; Dasseni, N.; Gaibazzi, N.; Rossi, A.; Henein, M.; Pressman, G. Cardiac calcification as a marker of subclinical atherosclerosis and predictor of cardiovascular events: A review of the evidence. Eur. J. Prev. Cardiol. 2019, 26, 1191–1204. [Google Scholar] [CrossRef] [PubMed]
- Michaels, A.D.; Mehaffey, J.H.; Hawkins, R.B.; Kern, J.A.; Schirmer, B.D.; Hallowell, P.T. Bariatric surgery reduces long-term rates of cardiac events and need for coronary revascularization: A propensity-matched analysis. Surg. Endosc. 2020, 34, 2638–2643. [Google Scholar] [CrossRef]
- Moussa, O.; Ardissino, M.; Heaton, T.; Tang, A.; Khan, O.; Ziprin, P.; Darzi, A.; Collins, P.; Purkayastha, S. Effect of bariatric surgery on long-term cardiovascular outcomes: A nationwide nested cohort study. Eur. Heart J. 2020, 41, 2660–2667. [Google Scholar] [CrossRef]
- Coffey, S.; Cox, B.; Williams, M.J. The prevalence, incidence, progression, and risks of aortic valve sclerosis: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2014, 63 Pt A, 2852–2861. [Google Scholar] [CrossRef] [Green Version]
- Nsaibia, M.J.; Boulanger, M.C.; Bouchareb, R.; Mkannez, G.; Le Quang, K.; Hadji, F.; Argaud, D.; Dahou, A.; Bosse, Y.; Koschinsky, M.L.; et al. OxLDL-derived lysophosphatidic acid promotes the progression of aortic valve stenosis through a LPAR1-RhoA-NF-kappaB pathway. Cardiovasc. Res. 2017, 113, 1351–1363. [Google Scholar] [CrossRef] [Green Version]
- Wallby, L.; Janerot-Sjoberg, B.; Steffensen, T.; Broqvist, M. T lymphocyte infiltration in non-rheumatic aortic stenosis: A comparative descriptive study between tricuspid and bicuspid aortic valves. Heart 2002, 88, 348–351. [Google Scholar] [CrossRef] [Green Version]
- Allison, M.A.; Cheung, P.; Criqui, M.H.; Langer, R.D.; Wright, C.M. Mitral and aortic annular calcification are highly associated with systemic calcified atherosclerosis. Circulation 2006, 113, 861–866. [Google Scholar] [CrossRef] [Green Version]
- Sutton-Tyrrell, K.; Kuller, L.H.; Matthews, K.A.; Holubkov, R.; Patel, A.; Edmundowicz, D.; Newman, A. Subclinical atherosclerosis in multiple vascular beds: An index of atherosclerotic burden evaluated in postmenopausal women. Atherosclerosis 2002, 160, 407–416. [Google Scholar] [CrossRef]
| Preoperatively | 1-Year Postoperatively | p-Value | |
|---|---|---|---|
| Clinical data | |||
| Weight (kg) | 121 ± 20 | 84 ± 16 | <0.001 |
| BMI (kg/m2) | 41.8 ± 4.9 | 28.9 ± 4.7 | <0.001 |
| Heart rate (bpm) | 74 ±13 | 65 ± 9 | <0.001 |
| Systolic BP (mmHg) | 134 ± 10 | 126 ± 9 | <0.001 |
| Diastolic BP (mmHg) | 87 ± 7 | 83 ± 5 | <0.001 |
| Preoperative hypertension | 55% | na | |
| Preoperative diabetes | 16% | na | |
| % on medication | |||
| -Aspirin | 3% | 2% | 0.03 |
| -Lipid lowering treatment | 14% | 5% | <0.001 |
| -Antihypertensive treatment | 26% | 15% | <0.001 |
| -Antidiabetic treatment | 15% | 7% | <0.001 |
| Biochemical data | |||
| Serum creatinine (µmol/L) | 71 ± 13 | 64 ± 11 | <0.001 |
| Serum total cholesterol (mmol/L) | 4.7 ± 1.0 | 4.4 ± 0.9 | 0.06 |
| Serum LDL cholesterol (mmol/L) | 3.1 ± 0.9 | 2.8 ± 0.8 | 0.003 |
| Serum triglycerides (mmol/L) | 1.6 ± 0.7 | 1.0 ± 0.4 | <0.001 |
| Serum 25-hydroxyvitamin D | 57.7 ± 24.0 | 68.9 ± 25.2 | 0.002 |
| HbA1c (%) | 5.8 ± 1.2 | 5.4 ± 0.7 | <0.001 |
| Echocardiographic data | |||
| LV end-diastolic diameter (cm) | 5.06 ± 0.42 | 4.93 ± 0.42 | <0.002 |
| LV end-systolic diameter (cm) | 3.41 ± 0.38 | 3.32 ± 0.35 | 0.06 |
| LV mass index (g/m2.7) | 44 ± 12 | 39 ± 11 | <0.001 |
| LV hypertrophy | 35% | 20% | <0.001 |
| LV EF (%) | 61 ± 5 | 59 ± 6 | 0.07 |
| LV GLS (%) | −15.7 ± 4.7 | −20.3 ± 2.7 | <0.001 |
| Pericardial fat (mm) | 12.5 ± 3.7 | 9.9 ± 2.9 | <0.001 |
| Aortic root diameter (cm) | 2.73 | 2.72 | 0.87 |
| AWT (mm) | 4.86 ± 1.74 | 4.37 ± 1.59 | 0.02 |
| 1-Year Reduction in Pericardial Fat | R2 = 0.52, p < 0.001 | ||
|---|---|---|---|
| Beta | t | p-Value | |
| Preoperative pericardial fat | 0.71 | 8.88 | <0.001 |
| Female sex | 0.16 | 2.04 | 0.04 |
| 1-year diastolic BP | −0.20 | −2.34 | 0.02 |
| 1-year BMI | −0.16 | −1.97 | 0.05 |
| 1-year reduction in LV mass | −0.14 | −1.78 | 0.08 |
| 1-Year Reduction in AWT | R2 = 0.50, p < 0.001 | ||
| Age | −0.22 | −2.82 | <0.01 |
| Preoperative AWT | 0.71 | 8.87 | <0.001 |
| 1-year BMI | −0.21 | −2.58 | 0.01 |
| 1-Year AVS | Nagelkerke R2 = 0.30, Wald 21, p < 0.001 | ||
|---|---|---|---|
| Wald | p-Value | OR [95% CI] | |
| Age | 6.56 | 0.01 | 1.08 [1.02–1.15] |
| 1-year BMI | 4.56 | 0.03 | 1.15 [1.01–1.30] |
| Preoperative AVS | |||
| -mild | 0.56 | 0.45 | 1.62 [0.46–5.69] |
| -moderate | 4.44 | 0.04 | 6.31 [1.14–35.03] |
| 1-Year MVS | Nagelkerke R2 = 0.43, Wald 38, p < 0.001 | ||
| 1-year BMI | 5.18 | 0.02 | 1.40 [1.05–1.87] |
| Preoperative systolic BP | 3.26 | 0.07 | 0.89 [0.78–1.01] |
| Preoperative MVS | 7.17 | <0.01 | 35.57 [2.61–485.54] |
| Preoperative AVS | 4.81 | 0.03 | 9.46 [1.27–70.53] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kovac, N.; Grymyr, L.M.D.; Gerdts, E.; Nadirpour, S.; Nedrebø, B.G.; Hjertaas, J.J.; Matre, K.; Cramariuc, D. Markers of Subclinical Atherosclerosis in Severe Obesity and One Year after Bariatric Surgery. J. Clin. Med. 2022, 11, 2237. https://doi.org/10.3390/jcm11082237
Kovac N, Grymyr LMD, Gerdts E, Nadirpour S, Nedrebø BG, Hjertaas JJ, Matre K, Cramariuc D. Markers of Subclinical Atherosclerosis in Severe Obesity and One Year after Bariatric Surgery. Journal of Clinical Medicine. 2022; 11(8):2237. https://doi.org/10.3390/jcm11082237
Chicago/Turabian StyleKovac, Nina, Lisa M. D. Grymyr, Eva Gerdts, Saied Nadirpour, Bjørn G. Nedrebø, Johannes J. Hjertaas, Knut Matre, and Dana Cramariuc. 2022. "Markers of Subclinical Atherosclerosis in Severe Obesity and One Year after Bariatric Surgery" Journal of Clinical Medicine 11, no. 8: 2237. https://doi.org/10.3390/jcm11082237
APA StyleKovac, N., Grymyr, L. M. D., Gerdts, E., Nadirpour, S., Nedrebø, B. G., Hjertaas, J. J., Matre, K., & Cramariuc, D. (2022). Markers of Subclinical Atherosclerosis in Severe Obesity and One Year after Bariatric Surgery. Journal of Clinical Medicine, 11(8), 2237. https://doi.org/10.3390/jcm11082237





