Patients’ Perspectives on Artificial Intelligence in Dentistry: A Controlled Study
Abstract
:1. Introduction
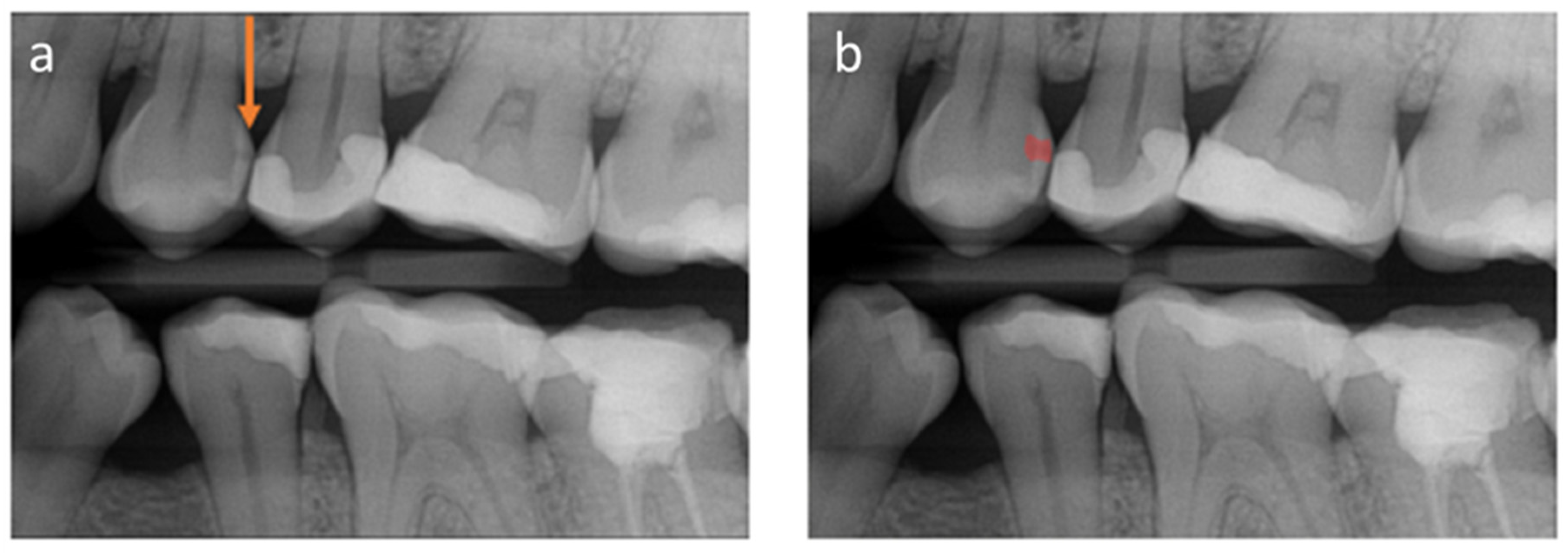
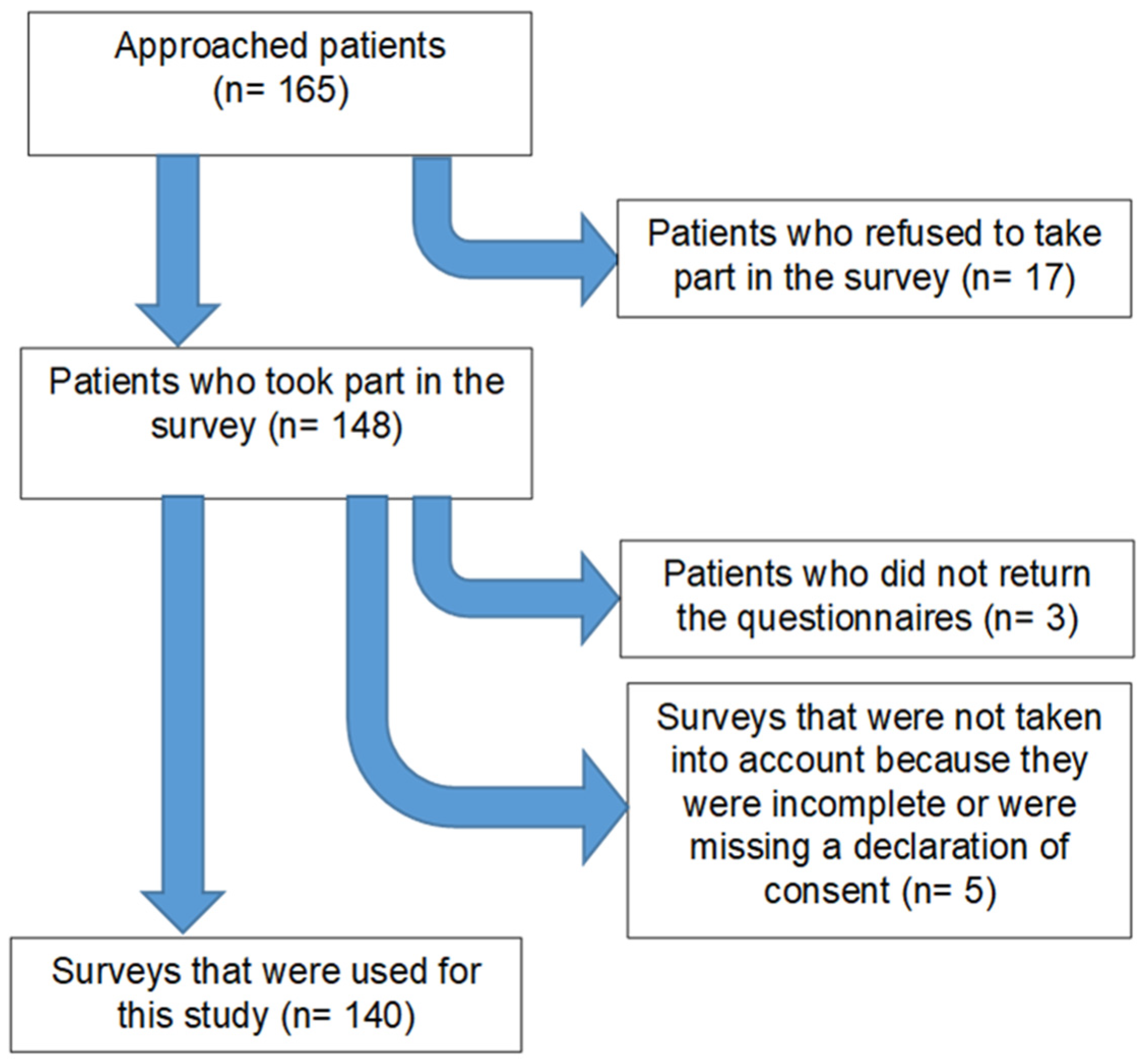
2. Materials and Methods
2.1. Study Design
2.2. Setting and Participants
2.3. Variables
2.4. Bias
2.5. Sample Size
2.6. Quantitative Variables
2.7. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef]
- Esteva, A.; Kuprel, B.; Novoa, R.A.; Ko, J.; Swetter, S.M.; Blau, H.M.; Thrun, S. Dermatologist-level classification of skin cancer with deep neural networks. Nature 2017, 542, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Gulshan, V.; Peng, L.; Coram, M.; Stumpe, M.C.; Wu, D.; Narayanaswamy, A.; Venugopalan, S.; Widner, K.; Madams, T.; Cuadros, J.; et al. Development and Validation of a Deep Learning Algorithm for Detection of Diabetic Retinopathy in Retinal Fundus Photographs. JAMA 2016, 316, 2402–2410. [Google Scholar] [CrossRef] [PubMed]
- Bejnordi, B.E.; Veta, M.; Van Diest, P.J.; Van Ginneken, B.; Karssemeijer, N.; Litjens, G.; Van Der Laak, J.A.; Hermsen, M.; Manson, Q.F.; Balkenhol, M.; et al. Diagnostic Assessment of Deep Learning Algorithms for Detection of Lymph Node Metastases in Women With Breast Cancer. JAMA 2017, 318, 2199–2210. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Golla, T.; Dreher, M.; Krois, J. Convolutional neural networks for dental image diagnostics: A scoping review. J. Dent. 2019, 91, 103226. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Stanley, K.; Att, W. Artificial intelligence in dentistry: Current applications and future perspectives. Quintessence Int. 2020, 51, 248–257. [Google Scholar] [PubMed]
- Kassebaum, N.J.; Smith, A.G.C.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.J.L.; Marcenes, W.; GBD 2015 Oral Health Collaborators. Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990–2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef]
- Bader, J.D.; Shugars, D.A.; Bonito, A.J. Systematic Reviews of Selected Dental Caries Diagnostic and Management Methods. J. Dent. Educ. 2001, 65, 960–968. [Google Scholar] [CrossRef]
- Rindal, D.B.; Gordan, V.V.; Litaker, M.S.; Bader, J.D.; Fellows, J.L.; Qvist, V.; Wallace-Dawson, M.C.; Anderson, M.L.; Gilbert, G.H.; Group, D.C. Methods dentists use to diagnose primary caries lesions prior to restorative treatment: Findings from The Dental PBRN. J. Dent. 2010, 38, 1027–1032. [Google Scholar] [CrossRef] [Green Version]
- Schwendicke, F.; Tzschoppe, M.; Paris, S. Radiographic caries detection: A systematic review and meta-analysis. J. Dent. 2015, 43, 924–933. [Google Scholar] [CrossRef]
- Cantu, A.G.; Gehrung, S.; Krois, J.; Chaurasia, A.; Rossi, J.G.; Gaudin, R.; Elhennawy, K.; Schwendicke, F. Detecting caries lesions of different radiographic extension on bitewings using deep learning. J. Dent. 2020, 100, 103425. [Google Scholar] [CrossRef] [PubMed]
- Mertens, S.; Krois, J.; Cantu, A.G.; Arsiwala, L.T.; Schwendicke, F. Artificial intelligence for caries detection: Randomized trial. J. Dent. 2021, 115, 103849. [Google Scholar] [CrossRef] [PubMed]
- Metzger, Z.; Colson, D.G.; Bown, P.; Weihard, T.; Baresel, I.; Nolting, T. Reflected near-infrared light versus bite-wing radiography for the detection of proximal caries: A multicenter prospective clinical study conducted in private practices. J. Dent. 2022, 116, 103861. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial Intelligence in Dentistry: Chances and Challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef]
- Haan, M.; Ongena, Y.P.; Hommes, S.; Kwee, T.C.; Yakar, D. A Qualitative Study to Understand Patient Perspective on the Use of Artificial Intelligence in Radiology. J. Am. Coll. Radiol. 2019, 16, 1416–1419. [Google Scholar] [CrossRef] [Green Version]
- Ongena, Y.P.; Haan, M.; Yakar, D.; Kwee, T.C. Patients’ views on the implementation of artificial intelligence in radiology: Development and validation of a standardized questionnaire. Eur. Radiol. 2020, 30, 1033–1040. [Google Scholar] [CrossRef] [Green Version]
- Knowles, E.M. Oxford Dictionary of Phrase and Fable; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Rammstedt, B.; Kemper, C.J.; Klein, M.C.; Beierlein, C.; Kovaleva, A. A short scale for assessing the big five dimensions of personality: 10 Item Big Five Inventory (BFI-10). Methoden Daten Anal. (MDA) 2013, 7, 1–23. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 2009, 50, 613–621. [Google Scholar]
- Gaalaas, L.; Tyndall, D.; Mol, A.; Everett, E.T.; Bangdiwala, A. Ex vivo evaluation of new 2D and 3D dental radiographic technology for detecting caries. Dentomaxillofac. Radiol. 2016, 45, 20150281. [Google Scholar] [CrossRef] [Green Version]
- Armfield, J.; Ketting, M.; Chrisopoulos, S.; Baker, S. Do people trust dentists? Development of the Dentist Trust Scale. Aus. Dent. J. 2017, 62, 355–362. [Google Scholar] [CrossRef] [Green Version]
- Mayer, R.C.; Davis, J.H.; Schoorman, F.D. An Integrative Model of Organizational Trust. AMR 1995, 20, 709–734. [Google Scholar] [CrossRef]
- Lee, J.D.; See, K.A. Trust in Automation: Designing for Appropriate Reliance. Hum. Factors 2004, 46, 50–80. [Google Scholar] [CrossRef] [PubMed]
- McKnight, D.H.; Lankton, N.; Tripp, J. Social Networking Information Disclosure and Continuance Intention: A Disconnect. In Proceedings of the 2011 44th Hawaii International Conference on System Sciences, Kauai, HI, USA, 4–7 January 2011; pp. 1–10. [Google Scholar]
- Thom, D.H.; Wong, S.T.; Guzman, D.; Wu, A.; Penko, J.; Miaskowski, C.; Kushel, M. Physician trust in the patient: Development and validation of a new measure. Ann. Fam. Med. 2011, 9, 148–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Önkal, D.; Goodwin, P.; Thomson, M.; Gönül, S.; Pollock, A. The relative influence of advice from human experts and statistical methods on forecast adjustments. J. Behav. Decis. Mak. 2009, 22, 390–409. [Google Scholar] [CrossRef]
- Promberger, M.; Baron, J. Do patients trust computers? J. Behav. Decis. Mak. 2006, 19, 455–468. [Google Scholar] [CrossRef]
- Juravle, G.; Boudouraki, A.; Terziyska, M.; Rezlescu, C. Chapter 14—Trust in artificial intelligence for medical diagnoses. Prog. Brain Res. 2020, 253, 263–282. [Google Scholar]
- York, T.; Jenney, H.; Jones, G. Clinician and computer: A study on patient perceptions of artificial intelligence in skeletal radiography. BMJ Health Care Inform. 2020, 27, e100233. [Google Scholar] [CrossRef]
- Wälivaara, B.-M.; Andersson, S.; Axelsson, K. Views on technology among people in need of health care at home. Int. J. Circumpolar. Health 2009, 68, 158–169. [Google Scholar] [CrossRef]
- Harrefors, C.; Axelsson, K.; Sävenstedt, S. Using assistive technology services at differing levels of care: Healthy older couples’ perceptions. J. Adv. Nurs. 2010, 66, 1523–1532. [Google Scholar] [CrossRef]
- Bildungstand-Bevölkerung im Alter von 15 Jahren und Mehr nach Allgemeinen und Beruflichen Bildungsabschlüssen nach Jahren. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bildung-Forschung-Kultur/Bildungsstand/Tabellen/bildungsabschluss.html;jsessionid=5C59C4965CD7014044F1EFAB5A449832.live712 (accessed on 7 December 2021).
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Monahan, P.O.; Löwe, B. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Howlett, J.R.; Paulus, M.P. Where perception meets belief updating: Computational evidence for slower updating of visual expectations in anxious individuals. J. Affect. Disord. 2020, 266, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Friedman, H.S.; Tucker, J.S.; Tomlinson-Keasey, C.; Schwartz, J.E.; Wingard, D.L.; Criqui, M.H. Does childhood personality predict longevity? J. Pers. Soc. Psychol. 1993, 65, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Amelang, M.; Bartussej, D. Differentielle Psychologie und Persönlichkeitsforschung; Kohlhammer: Stuttgart, Germany, 2006. [Google Scholar]
- Gassner, O. Künstliche Intelligenz in Deutschland- Meinungen und Zukünftige Einschätzung; FOM Hochschule für Oekonomie & Management; ifes Institut für Empirie & Statistik Standort München: Munich, Germany, 2019; pp. 1–26. [Google Scholar]
| Statement | Variable | Group | Mean (SD) |
|---|---|---|---|
| “I can see the disease (caries) on the radiograph”. | See | Control: (no AI) | 2.8 (1.3) |
| AI-based communication | 3.5 (1.3) | ||
| “I believe that my dentist can make a correct diagnosis (caries) based on radiograph and suggest an appropriate therapy (filling)”. | Believe | Control: (no AI) | 4.3 (0.8) |
| AI-based communication | 4.4 (0.7) | ||
| “I understand that the disease (caries) seen on the radiograph needs treatment”. | Understand | Control: (no AI) | 4.3 (0.9) |
| AI-based communication | 4.4 (0.8) | ||
| “I trust the decision my dentist has made based on the radiograph”. | Trust | Control: (no AI) | 4.4 (0.8) |
| AI-based communication | 4.5 (0.6) | ||
| “I feel adequately informed about the condition (caries) and the need for a therapy (filling)”. | Feel informed | Control: (no AI) | 3.9 (1.1) |
| AI-based communication | 4.2 (0.9) | ||
| “I have the feeling that I cannot make a decision on my own, and I feel at the mercy of my dentist”. | Feel unable | Control: (no AI) | 2.7 (1.3) |
| AI-based communication | 2.7 (1.3) |
| Statements | Mean (SD) |
|---|---|
| “AI is useful” | 4.2 (0.8) |
| “In principle, I would prefer to rely on humans rather than robots or AI.” | 3.4 (1.0) |
| “I have security concerns about using AI.” | 2.7 (1.0) |
| “AI makes life easier.” | 3.8 (0.8) |
| “I believe AI improves people’s quality of life.” | 3.6 (0.9) |
| “I am scared of the topic and its consequences” | 2.2 (1.0) |
| “I would base the choice of my dentist on whether he/she uses AI-based assistance systems or not.” | 2.5 (1.2) |
| “If my dentist doesn’t use AI-based assistance systems, I would switch to another dentist.” | 2.0 (1.0) |
| “The use of AI in dentistry scares me.” | 1.7 (0.8) |
| “I think that AI will support dentists’ diagnostics in the future.” | 4.2 (0.8) |
| “AI can prevent incorrect treatment.” | 3.7 (0.8) |
| “I can have more confidence in a dentist’s diagnosis when it’s assisted by AI.” | 3.4 (1.1) |
| “I believe AI can serve as a quality control for the dentist’s diagnosis.” | 4.1 (0.8) |
| “I would feel safer with a dentist if AI were used.” | 3.1 (1.0) |
| “I fear that AI can make mistakes and lead to wrong decisions by the dentist.” | 2.7 (0.8) |
| “I fear that a dentist would rely solely on AI to diagnose.” | 3.0 (1.0) |
| “I think that some problems with my teeth could have been prevented if the dentist had worked with AI to assist.” | 2.7 (1.2) |
| “I find it important to have a good understanding of the results of a radiograph.” | 4.6 (0.7) |
| “I would pay something for an AI-assisted radiograph analysis.” | 3.0 (1.2) |
| “I think it’s important to know how AI works when it is used on my radiograph.” | 4.2 (0.9) |
| “I think it’s important that I, as a patient, am shown what is conspicuous in a radiograph.” | 4.8 (0.6) |
| “Humans and AI can complement each other.” | 4.5 (0.8) |
| “AI can help dentists evaluate radiographs.” | 4.4 (0.7) |
| “In my opinion, people make more mistakes than computers.” | 3.2 (0.9) |
| See | Believe | Understand | Trust | Feel Informed | Feel Unable | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Covariates and Psychological Parameters | LD | 95% CI | LD | 95% CI | LD | 95% CI | LD | 95% CI | LD | 95% CI | LD | 95% CI | |
| Age group | <52 years (ref.: ≥52 years) | 1.12 | 0.38, 1.86 | 0.67 | −0.02, 1.37 | 0.61 | −0.33, 1.55 | −0.32 | −1.93, 0.66 | 0.79 | 0.13, 1.71 | −0.20 | −1.05, 0.64 |
| Sex | Female (ref.: male) | 0.36 | −0.34, 1.05 | −0.18 | −0.84, 0.48 | −0.46 | −1.36, 0.44 | 0.89 | −0.09, 1.86 | 0.37 | −0.53, 1.27 | −0.26 | −1.07, 0.56 |
| Education | university degree (ref.: no university degree) | 0.90 | 0.21, 1.59 | 0.55 | −0.09, 1.19 | 0.23 | −0.64, 1.10 | 0.15 | −0.76, 1.06 | 0.90 | −0.01, 1.80 | 0.50 | −0.30, 1.29 |
| Occupation | with | −0.39 | −1.59, 0.81 | 0.16 | −0.96, 1.28 | −0.85 | −2.40, 0.70 | −0.23 | −1.87, 1.40 | 0.61 | −1.28, 2.50 | 0.06 | −1.33, 1.44 |
| without | −0.56 | −2.24, 1.13 | 0.22 | −1.36, 1.82 | 0.14 | −1.96, 0.70 | −0.66 | −2.94, 1.62 | 0.17 | −2.28, 2.61 | −0.00 | −1.96, 1.96 | |
| Student (ref.: retired) | 1.19 | −0.47, 2.85 | 1.98 | 0.34, 3.62 | −1.48 | −3.70, 0.72 | 0.18 | −2.18, 2.53 | 1.60 | −0.73, 3.94 | 1.68 | −0.32, 3.67 | |
| Anxiety | 0.99 | 0.13, 1.86 | 0.70 | −0.13, 1.54 | −0.91 | −2.08, 0.25 | −0.21 | −1.43, 1.01 | 0.63 | −0.50, 1.76 | 0.97 | −0.08, 2.02 | |
| Depression | −0.68 | −1.72, 0.37 | 0.01 | −0.97, 0.98 | −0.72 | −2.10, 0.66 | 0.61 | −2.08, 0.86 | −1.19 | −2.69, 0.34 | 0.23 | −0.97, 1.42 | |
| Extraversion | 0.083 | −0.23, 0.45 | −0.38 | −0.69, −0.08 | 0.07 | −0.34, 0.48 | 0.02 | −0.40, 0.45 | 0.36 | −0.07, 0.79 | −0.26 | −0.63, 0.11 | |
| Neuroticism | 0.102 | −0.24, 0.45 | 0.18 | −0.15, 0.50 | 0.21 | −0.24, 0.66 | 0.48 | 0.01, 0.96 | 0.25 | −0.20, 0.69 | −0.8 | −0.48, 0.32 | |
| Openness | 0.04 | −0.36, 0.44 | −0.28 | −0.65, 0.11 | 0.31 | −0.22, 0.84 | 0.06 | −0.48, 0.60 | 0.64 | 0.05, 1.24 | 0.32 | −0.15, 0.78 | |
| Conscientiousness | −0.87 | −0.75, 0.18 | −0.05 | −0.49, 0.39 | −0.20 | −0.78, 0.38 | −0.14 | −0.77, 0.49 | −0.18 | −0.76, 0.41 | 0.33 | −0.22, 0.88 | |
| Tolerance | 0.01 | −0.42, 0.45 | −0.22 | −0.63, 1.36 | −0.13 | −0.42, 0.68 | −0.54 | −1.12, 0.05 | −0.55 | −0.13, 1.71 | −0.09 | −0.59, 0.41 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosan, E.; Krois, J.; Wingenfeld, K.; Deuter, C.E.; Gaudin, R.; Schwendicke, F. Patients’ Perspectives on Artificial Intelligence in Dentistry: A Controlled Study. J. Clin. Med. 2022, 11, 2143. https://doi.org/10.3390/jcm11082143
Kosan E, Krois J, Wingenfeld K, Deuter CE, Gaudin R, Schwendicke F. Patients’ Perspectives on Artificial Intelligence in Dentistry: A Controlled Study. Journal of Clinical Medicine. 2022; 11(8):2143. https://doi.org/10.3390/jcm11082143
Chicago/Turabian StyleKosan, Esra, Joachim Krois, Katja Wingenfeld, Christian Eric Deuter, Robert Gaudin, and Falk Schwendicke. 2022. "Patients’ Perspectives on Artificial Intelligence in Dentistry: A Controlled Study" Journal of Clinical Medicine 11, no. 8: 2143. https://doi.org/10.3390/jcm11082143
APA StyleKosan, E., Krois, J., Wingenfeld, K., Deuter, C. E., Gaudin, R., & Schwendicke, F. (2022). Patients’ Perspectives on Artificial Intelligence in Dentistry: A Controlled Study. Journal of Clinical Medicine, 11(8), 2143. https://doi.org/10.3390/jcm11082143







