1. Introduction
Patients who have lost their teeth due to severe periodontitis or who have been wearing dentures for a long period often experience alveolar bone atrophy. Bone regeneration therapy is mandatory for the installation of dental implants in severely atrophic alveolar bones. Autologous bone transplantation is the gold standard for bone regeneration therapies. However, harvesting autologous bone is inevitably accompanied by swelling and pain at healthy donor sites. Recently, artificial bones such as hydroxyapatite, β-tricalcium phosphate (β-TCP), and carbonate apatite have been widely used [
1,
2]. Most artificial bones only possess osteoconduction capability and lack osteo-induction and bone regeneration capabilities; thus, the size and shape of the target bone defect are limited. Accordingly, there has been a strong demand for novel transplantation materials that are not invasive, are more functional, and can be applied to severe alveolar bone atrophy cases.
Langer and Vacanti first introduced the concept of tissue engineering in 1993 [
3]. This concept advocates three main elements for tissue regeneration: living cells, scaffolds, and growth factors. Bone marrow stromal cells (BMSCs) have been widely used in bone tissue engineering and have already been clinically applied [
4,
5]. Since 2004, our group has conducted a clinical study of alveolar bone regeneration using BMSCs. The transplants from all participants showed bone regeneration, and the integration of implants was achieved in 93% (27/29) [
6], showing the feasibility of bone tissue engineering using BMSCs. However, non-negligible individual variation was noted in the histology of the regenerated bone, which might be due to the individual variation in BMSCs, such as cell proliferation capability and alkaline phosphatase (ALP) activity [
7]. These results suggest the need for further optimization of cell-processing protocols and investigation of the effect of cultured cell quality on clinical efficacy.
Therefore, we optimized the cell culture and processing conditions of BMSCs for bone tissue engineering based on their ability to form bone in vivo [
7] and generated a novel modified protocol for a clinical study on alveolar bone tissue engineering [
8]. We report the results of a clinical study using this modified protocol and compared them with those of the previous clinical study [
6].
2. Materials and Methods
This study conformed to the tenets of the Declaration of Helsinki, and the protocol was approved by the institutional review board of the Institute of Medical Science, The University of Tokyo (IMSUT) (IRB for clinical study using human stem cells, No. 21-1) and with the permission of the Minister of Health, Labour, and Welfare of Japan. All participants provided written informed consent. This study was registered in the University Hospital Medical Information Network (UMIN) Clinical Trials Registry (UMIN000006255).
The study design and time points for each intervention are summarized in
Table 1.
2.1. Inclusion Criteria
The subjects should have continuous tooth defects (>2), where fixed prostheses are not applicable. The participants wished to undergo dental implant treatment rather than conventional removable prostheses. The subjects had severely atrophic maxillae or mandibles, which required bone transplantation. The width of the alveolar bone at the installation site was <5 mm. In the maxilla, the distance between the alveolar ridge and the sinus floor was <5 mm. Similarly, in the mandible, the distance between the ridge and the mandibular canal was <5 mm. Tooth-brushing and scaling were performed prior to protocol treatment, and good oral hygiene was maintained. The age of the participants was limited to 20–70 years.
2.2. Exclusion Criteria
Patients with diabetes and/or autoimmune diseases who presented hemorrhagic diathesis where partial thromboplastin time was <50% and activated partial thromboplastin time less than 23.5 s or longer than 42.5 s, who were taking anticoagulant or antiplatelet drugs of a type that were difficult to stop; who were positive for syphilis, anti-HBV antigen, anti-HCV antibody, anti-HTLV-1 antibody, or anti-HIV antibody; with osteoporosis, liver dysfunction with an aspartate aminotransferase value <10 or >40 IU/L or with an alanine aminotransferase <5 or >45 IU/L; who were pregnant or possibly pregnant; with an allergy for any of the medications used in this study and/or allergy that required continuous systemic medication, who smoked, or who had other special conditions that the responsible physician or dentist considered inappropriate, were excluded.
2.3. Number of Subjects and Duration of Study
The participants were referred from other hospitals/clinics and primarily fulfilled the eligibility criteria. No one was excluded after examination, and there was no drop out. Fifteen patients were enrolled in this study, and the follow-up period was 2 years after cell transplantation.
2.4. Donor Screening
Blood tests, urinalysis, chest X-ray, panoramic X-ray, computed tomography of the head, and electrocardiography were performed to screen the subjects before enrollment in this clinical study.
2.5. Autologous Serum Preparation
Peripheral blood and bone marrow were harvested, as previously described [
6]. Briefly, prior to bone marrow aspiration, 200–400 mL of peripheral blood was collected and autologous serum was prepared. Peripheral blood was stored at 4 °C for 1 h and centrifuged. The serum was transferred to fresh bags (approximately 50 g each) for aseptic cryopreservation (Nipro Corp., Osaka, Japan). The bags were stored in a freezer at −20 °C until use. Before use, the serum was thawed and added to the culture medium containing antibiotics to a final serum concentration of 10%.
2.6. Harvest and Expansion of Bone Marrow Stromal Cells
Bone marrow was harvested from the iliac crest under local anesthesia. The marrow (10 mL) was aspirated into a syringe containing 500 U of heparin, and two syringes were used (total of 20 mL). The aspirated bone marrow was diluted four-fold with α-MEM (Gibco BRL, Grand Island, NY, USA) containing 10% autoserum, 2.5 µg/mL amphotericin B, and 50 µg/mL gentamicin sulfate. The medium containing cells was plated in 150-cm
2 flasks (Corning, New York, NY, USA). On day 4, the culture medium was changed to medium containing basic fibroblast growth factor (bFGF; FIBLAST Spray 250, Kaken Pharmaceutical Co., Ltd., Tokyo, Japan), and non-adherent cells were discarded. Adherent cells were cultured as BMSCs [
9]. The BMSCs were maintained in the same medium at 37 °C in a 5% CO
2 atmosphere. The cells demonstrated a typical spindle shape that was maintained throughout the cell culture period. When the cells attained 80% confluence, they were subcultured into tubes containing 50 mg of β-TCP granules (OSferion, Olympus Terumo Biomaterials Corp., Tokyo, Japan). The next day, the medium was changed to osteogenic induction medium containing 10 nM dexamethasone (Dex, Sigma-Aldrich, St. Louis, MO, USA) and 100 μM ascorbic acid (Wako Pure Chemical Industries, Ltd., Osaka, Japan) in α-MEM with 10% autoserum, 2.5 µg/mL amphotericin B, and 50 µg/mL gentamicin sulfate and induced for 13–16 days before transplantation. The medium was changed twice a week.
2.6.1. Test for Osteogenic Differentiation
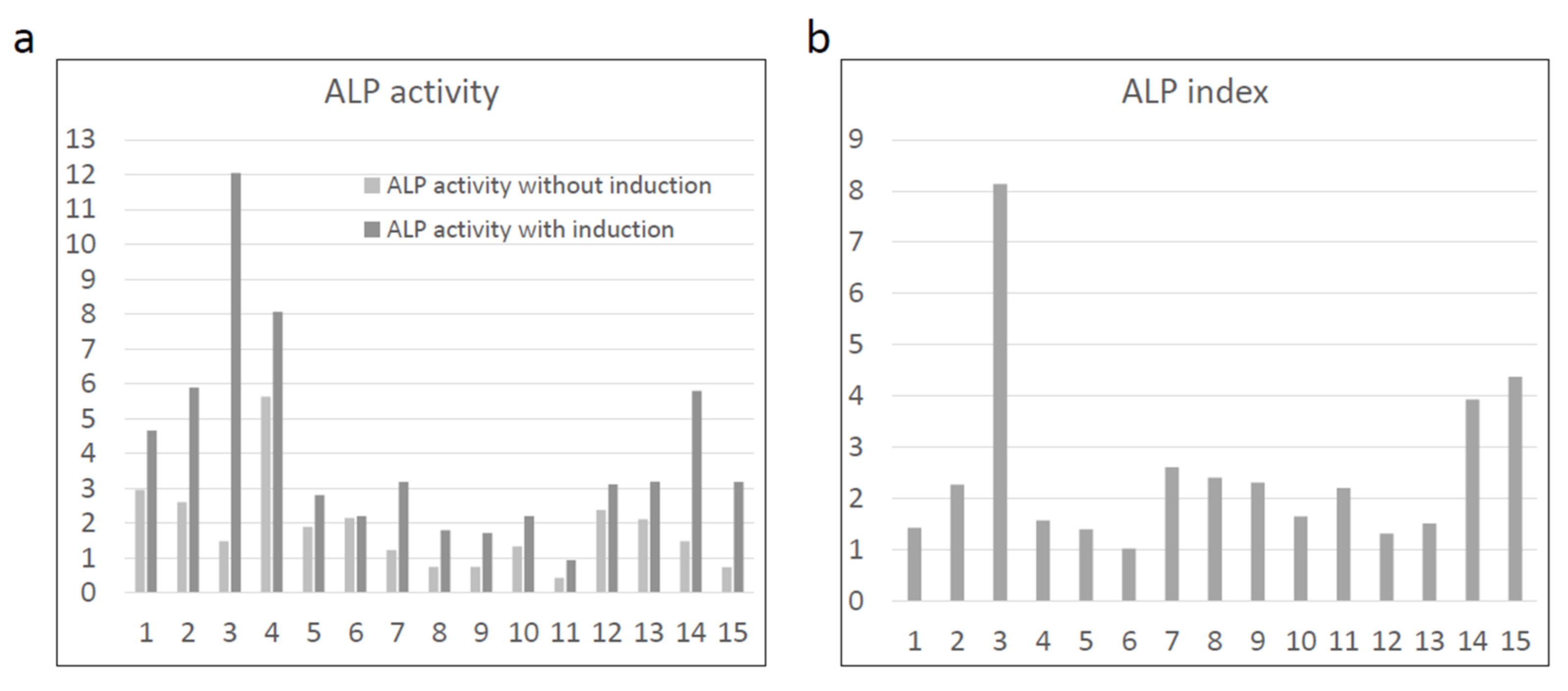
Osteogenic differentiation of BMSCs was confirmed by ALP activity as previously described [
10]. Briefly, 1 × 10
6 of harvested cells were incubated with 400 µL of 20 mM HEPES (Dojindo, Kumamoto, Japan) buffer (pH 7.5) containing 1% Triton X-100 (Wako Pure Chemical Industries, Ltd., Osaka, Japan) to extract proteins. After extraction, the supernatants were incubated with BCA protein assay reagent (Pierce Thermo Scientific, Waltham, MA, USA) or p-nitrophenyl phosphate solution (Sigma-Aldrich) in tubes (30 min for the protein assay and 5 min for p-nitrophenyl phosphate in a dark room at room temperature). The conversion of p-nitrophenyl phosphate to p-nitrophenol was stopped using 3 N NaOH after 5 min. Absorbance (405 nm for p-nitrophenol analysis; 570 nm for protein analysis) was measured using a spectrophotometer (Bio-Rad Laboratories, Inc., Hercules, CA, USA). The ratio of ALP activity (calculated as p-nitrophenol value/WST-8 value) was calculated and used as “ALP index”. Previous reports [
11] and our own data showed that the ALP index of bone-forming cells in the bone marrow was ≥1.0, and this value was used for quality assurance of cultured cells.
2.6.2. Safety Tests
The culture medium with 10% autologous serum (1 mL) was subjected to three safety checks. To test for bacterial and fungal contamination, the medium was subjected to aerobic and anaerobic cultures using a membrane filter technique, which was performed at the last medium change before cell transplantation and at the time of cell transplantation.
The medium was tested for mycoplasma contamination using PCR, the mycoplasma-specific enzyme detection method, and the culture method. DNA was extracted from the prepared medium using phenol:chloroform:isoamyl alcohol (PCI) (Sigma-Aldrich). Equal volumes of PCI were added to the medium (600 µL) and centrifuged at 15,000 rpm for 5 min at room temperature. The supernatant of the centrifuged tube was mixed with 400 µL ice-cold 100% isopropanol (Wako Pure Chemical Industries, Ltd.) (400 µL) and centrifuged at 15,000 rpm for 10 min. The pellet was then rinsed with 400 µL ice-cold 70% ethanol (Wako, Osaka, Japan) and centrifuged at 15,000 rpm for 5 min. The final pellet was dried for 3 min and dissolved in distilled water (20 µL) for PCR. Two-step PCR was performed (Hasegawa et al., 1993). The reaction mixture for PCR contained 1 μL of each primer (10 pmol/μL), 5 μL of 10× reaction buffer, 10 nmol of each deoxynucleotide, samples as templates, and water to a volume of 49 μL. The primers used for the first-step PCR were MCGpF11(5′-ACACCATGGGAG(C/T)TGGTAAT-3′) and R23-JR(5′-CTCCTAGTGCCAAG(C/G)CAT(C/T)C-3′). The second-step PCR was also performed in a 50 µL volume with inner primers R16-2 (5′-CTG(C/G)FF(A/C)TGGATCACCTCCT-3′) and MCGpR21 (5′-GCATCCACCA(A/T)A(A/T)AC(C/T)CTT-3′). The reaction mixture contained 1 µL of the first PCR product. Thirty-five cycles were performed under the following conditions: denaturation at 94 °C for 30 s, annealing at 55 °C for 2 min, and polymerization at 72 °C for 2 min. Amplified DNA was separated on a 1.5% agarose gel and soaked in TAE buffer containing 0.1 µg/mL ethidium bromide. The products were analyzed using a ChemiDoc XRS gel documentation system (Bio-Rad Laboratories, Inc., Hercules, CA, USA). Mycoplasma contamination was also assessed using the MycoAlertTM kit (LONZA KK., Tokyo, Japan). The ratio of luminescence before adding the substrate solution (measured value A) and luminescence 10 min after adding the substrate solution (measured value B) were measured and considered negative when the ratio was ≤1.0. In the mycoplasma culture method, the presence or absence of a mycoplasma colony was examined under a microscope at a magnification of 100 times or higher. If the results of the mycoplasma culture, PCR, and enzyme methods were all negative, it was considered mycoplasma-negative.
Endotoxin levels were measured at the time of the final medium exchange and at the time of cell transplantation. The Limulus ES-II Test Wako (299-51201, FUJIFILM Wako Pure Chemical Corporation, Osaka, Japan) was used, and the judgment was made with Toxinometer® ET-201(FUJIFILM Wako Pure Chemical Corporation). Samples containing 1 EU/mL or less were considered negative.
2.6.3. Flow Cytometric Analysis
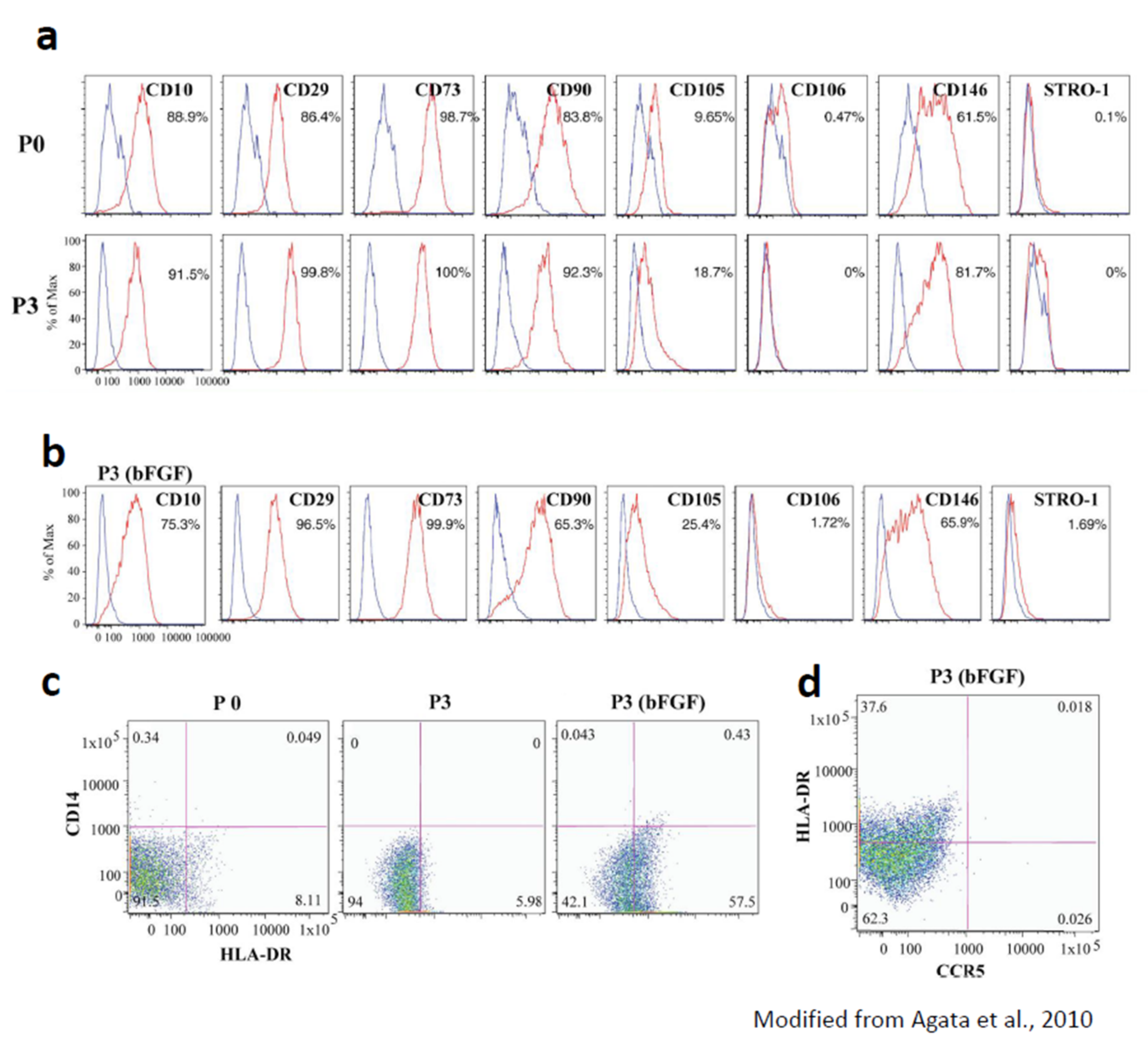
The characteristics of the BMSCs were evaluated using flow cytometry in a previous study [
7]. Aria flow cytometer (Becton Dickinson, San Jose, CA, USA) and the following antibodies were used: fluorescence isothiocyanate (FITC)-conjugated, phycoerythrin-conjugated, peridinin-chlorophyll-protein-conjugated (PerCP-Cy5.5), allophycocyanin-conjugated, Alexa Fluor 405-conjugated, or biotinylated antibodies against HLA-ABC, HLA-DR, CD3, CD14, CD19, CD34, CD73, CD90, CD106, CD146, CC chemokine receptor-5 (all from BD Pharmingen, Franklin Lakes, NJ, USA), CD10, CD29 (both from Dako, Glostrup, Denmark), and CD45 (Caltag; Invitrogen). Unconjugated CD105 antibody (Immunotech, Marseille Cedex 9, France) was covalently conjugated to FITC. The STRO-1 antibody (R&D Systems, Minneapolis, MN, USA) was detected using phycoerythrin-conjugated anti-mouse IgM. Biotinylated antibodies were detected using streptavidin Pacific Blue (Molecular Probes, Invitrogen, Carlsbad, CA, USA) or streptavidin PerCPCy5.5 (BD Pharmingen) conjugates. Propidium iodide (Dojindo) was used to detect dead cells. Color-conjugated mouse-IgG1k (BD Pharmingen) was used as a negative control. Data analysis was performed using the FlowJo software (TreeStar, San Carlos, CA, USA).
2.7. Preparation of Transplants
The cells in the scaffold were washed with saline three times and transferred to the operating room. The β-TCP granules were loosely connected to the cells and matrices and could be transferred as a mass in most cases.
2.8. Major Differences in Cell Culture and Processing Protocol between the Previous and Present Clinical Studies
In terms of the cell culture protocol, the results from an optimization study showed that the ability to form ectopic bone was immediately lost after passage [
7]. Accordingly, BMSCs were cultured in flasks for just one passage in this study, then seeded onto the scaffold and induced into osteogenic cells (passage 2 cells), instead of the passage 3 cells used for osteogenic differentiation in a previous clinical study [
6]. Because bFGF can enhance cell growth and help maintain the in vivo osteogenic ability, bFGF was added to the culture medium during the cell expansion phase [
7]. Optimization of the mixing conditions for BMSCs and the scaffold was also considered. The results of our study showed that cell seeding onto scaffolds prior to osteogenic induction resulted in more new in vivo bone formation than cell seeding after osteogenic induction [
12]. BMSCs were seeded onto the scaffolds before osteogenic induction.
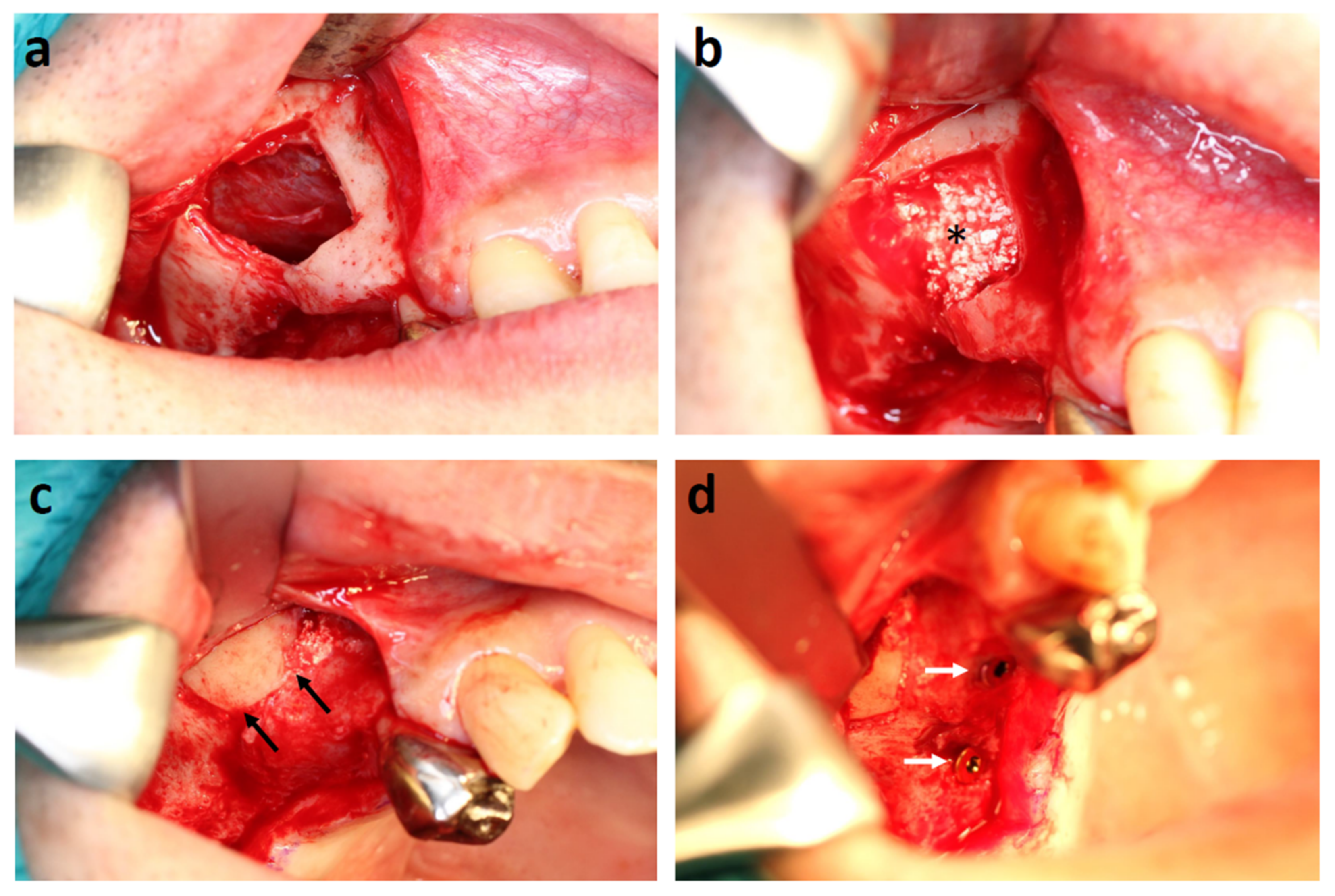
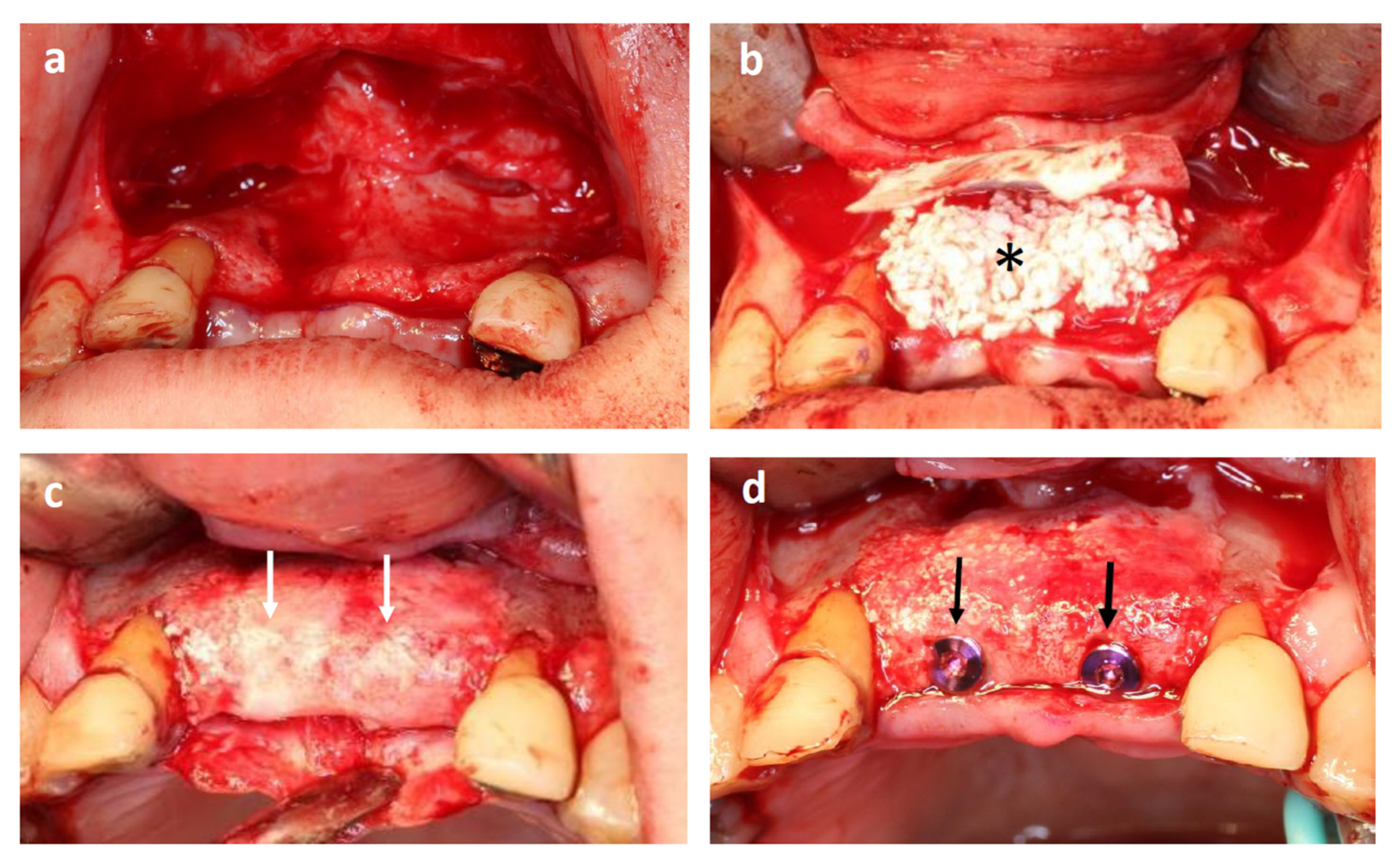
2.9. Surgical Procedure
Transplantation was performed under local anesthesia and intravenous sedation with propofol. The lateral sinus wall was removed and the sinus floor mucous membrane (Schneiderian membrane) was carefully elevated. The transplant was filled in the space between the sinus floor and the elevated membrane. The sinus wall was repositioned and the mucoperiosteal flap was sutured. In cases of alveolar ridge augmentation, the mucoperitoneal flap was elevated, and the transplant was placed on the atrophic alveolar ridge where the dental implant installation was planned and covered with a GTR membrane or titanium mesh. After flap extension, the incision was sutured.
In both sinus floor elevation and alveolar ridge augmentation cases, dental implants were installed four months after the transplantation. Novel active implants (Nobel Biocare, Zürich-Flughafen Switzerland) were used for all cases.
Abutment connection was performed after 3 months for lower jaw implants and 6 months for upper jaw implants.
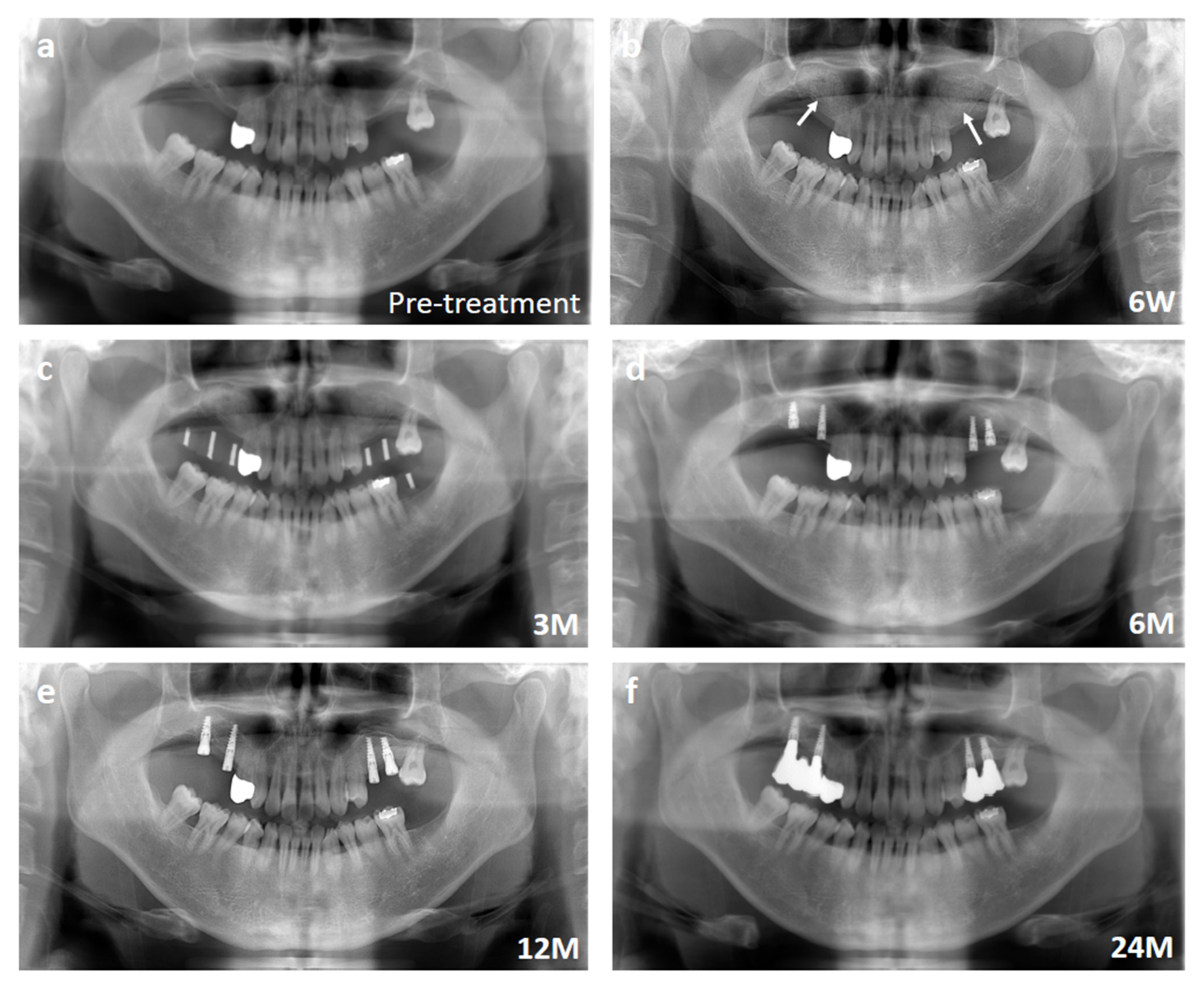
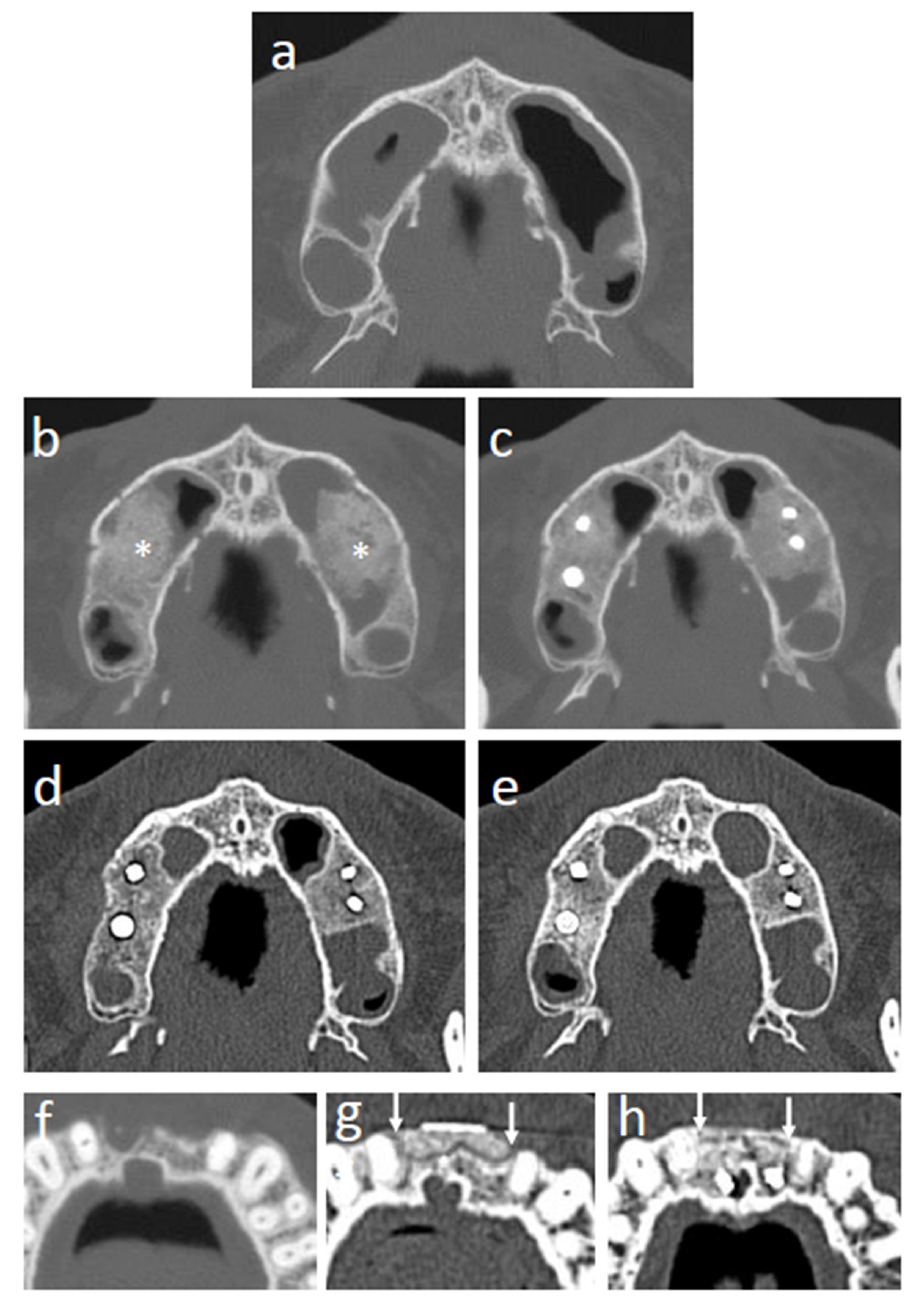
2.10. Evaluation
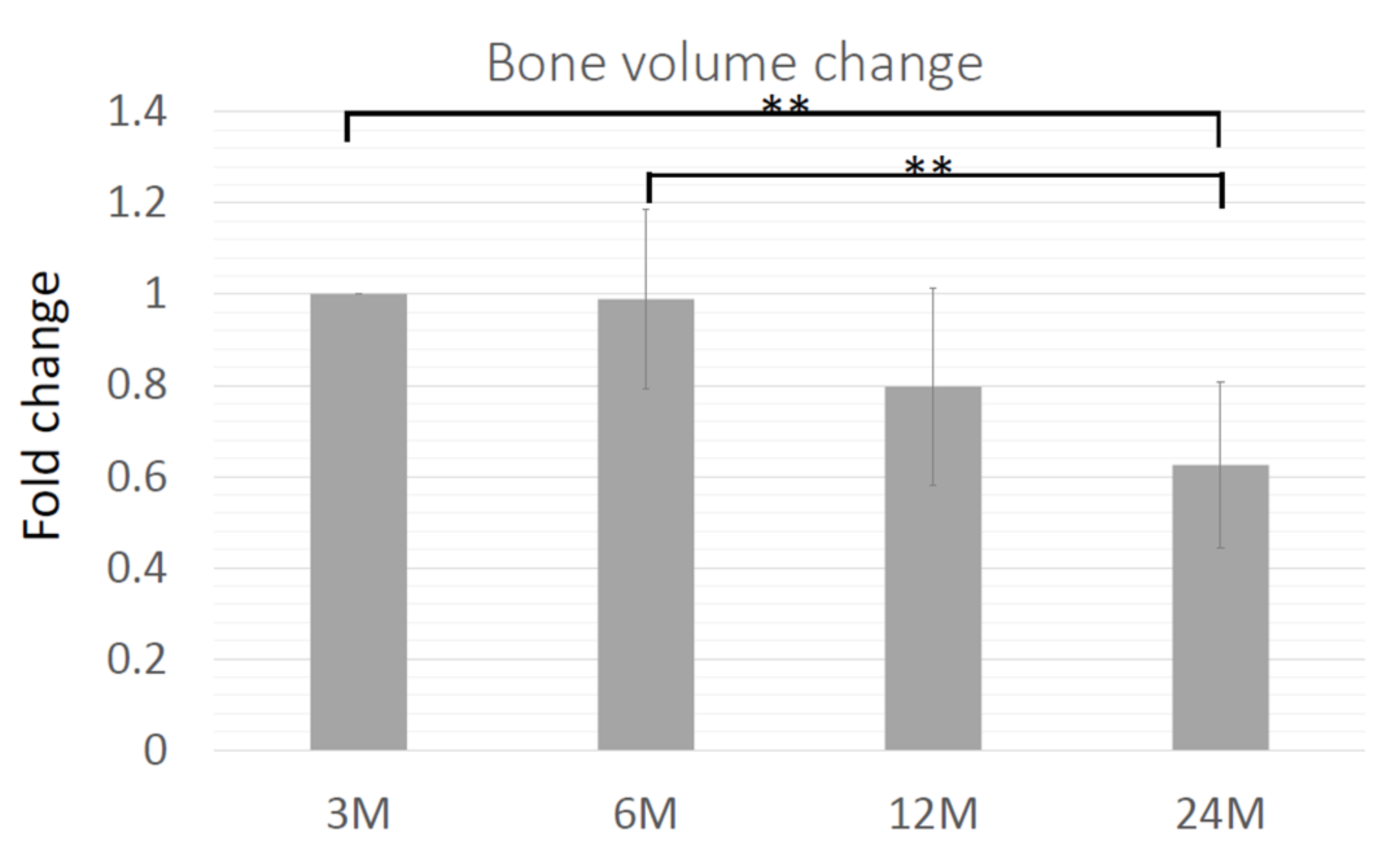
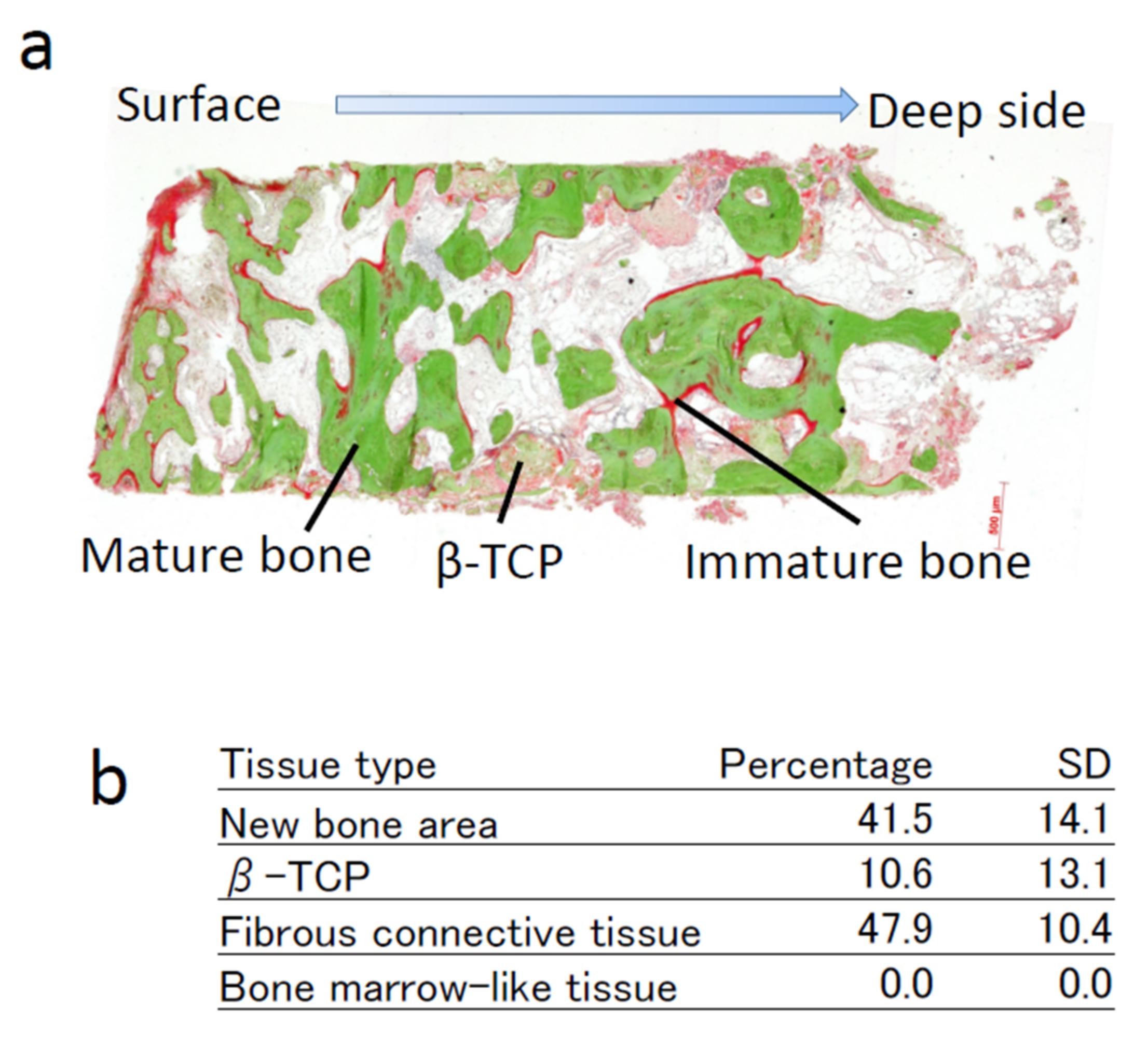
Panoramic X-rays were evaluated before the operation and at 6, 12, and 24 weeks and 1 and 2 years after the operation. Computed tomography (CT) was performed before the operation, at 12 and 24 weeks, and 1 and 2 years after the operation. The amount of regenerated bone was calculated using the SimPlant software (Materialize, Leven, Belgium). A bone biopsy was performed 16 weeks after cell transplantation at the time of dental implant installation using a trephine bur (2 mm inner diameter and 3 mm outer diameter; Stoma am Mark GmbH, Emmingen-Liptingen, Germany). After embedding in resin, non-decalcified ground sections were prepared, and the sections were evaluated using Villanueva Goldner staining and hematoxylin and eosin staining (H–E).
Histomorphometric Analysis
Light microscope images were captured using a digital camera (Carl Zeiss AG, Oberkochen, Germany) and transferred to a computer. The extent of new bone area, area of remaining scaffold, area of fibrous tissue, and area of bone marrow-like tissue were manually assessed using Image J [
13] by an examiner who was well-trained in bone histology, was not a co-investigator, but was a member of this clinical study. The data were confirmed by a bone histology specialist. The size of these specific areas is expressed as a percentage of the total area of the section.
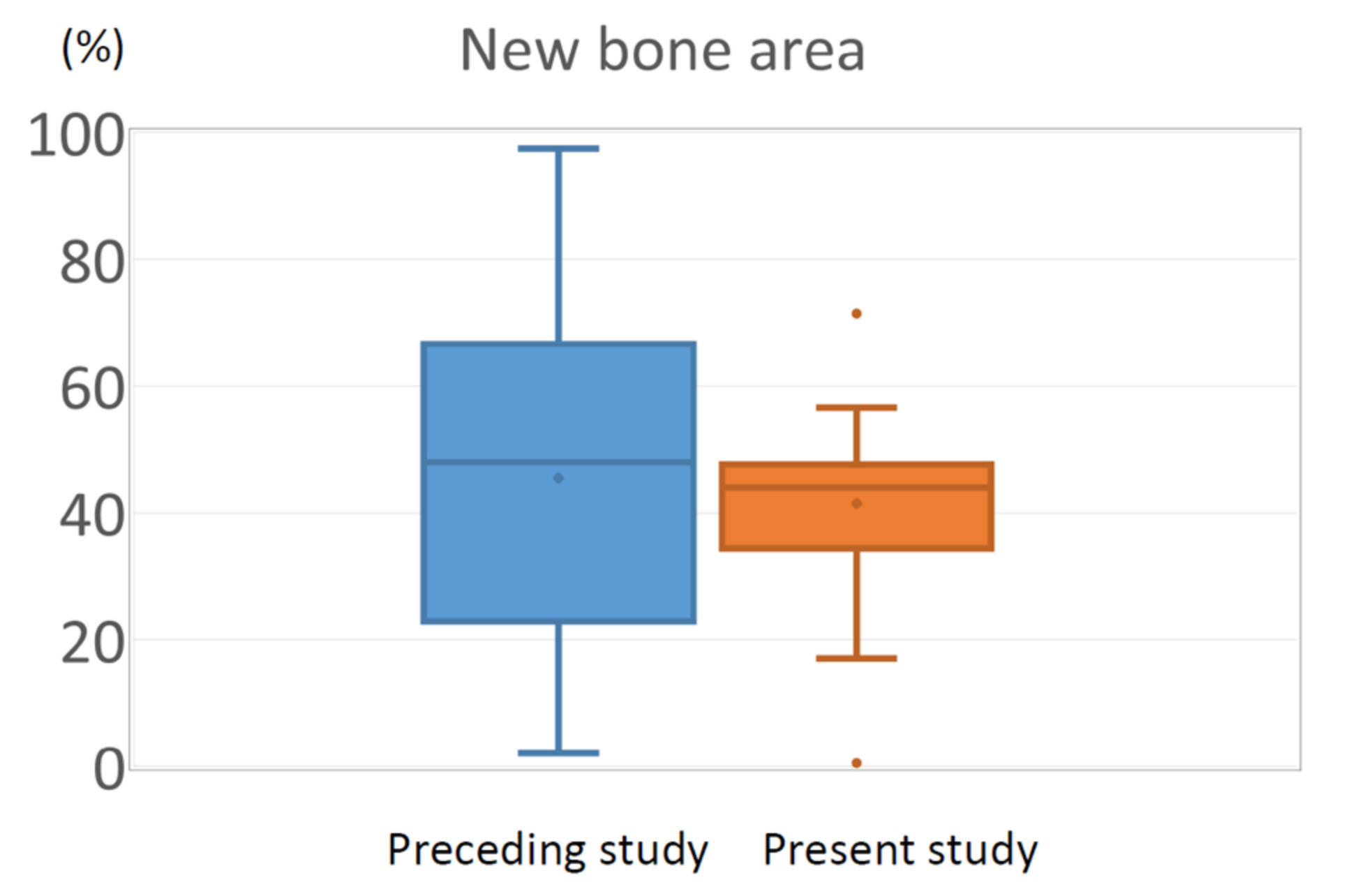
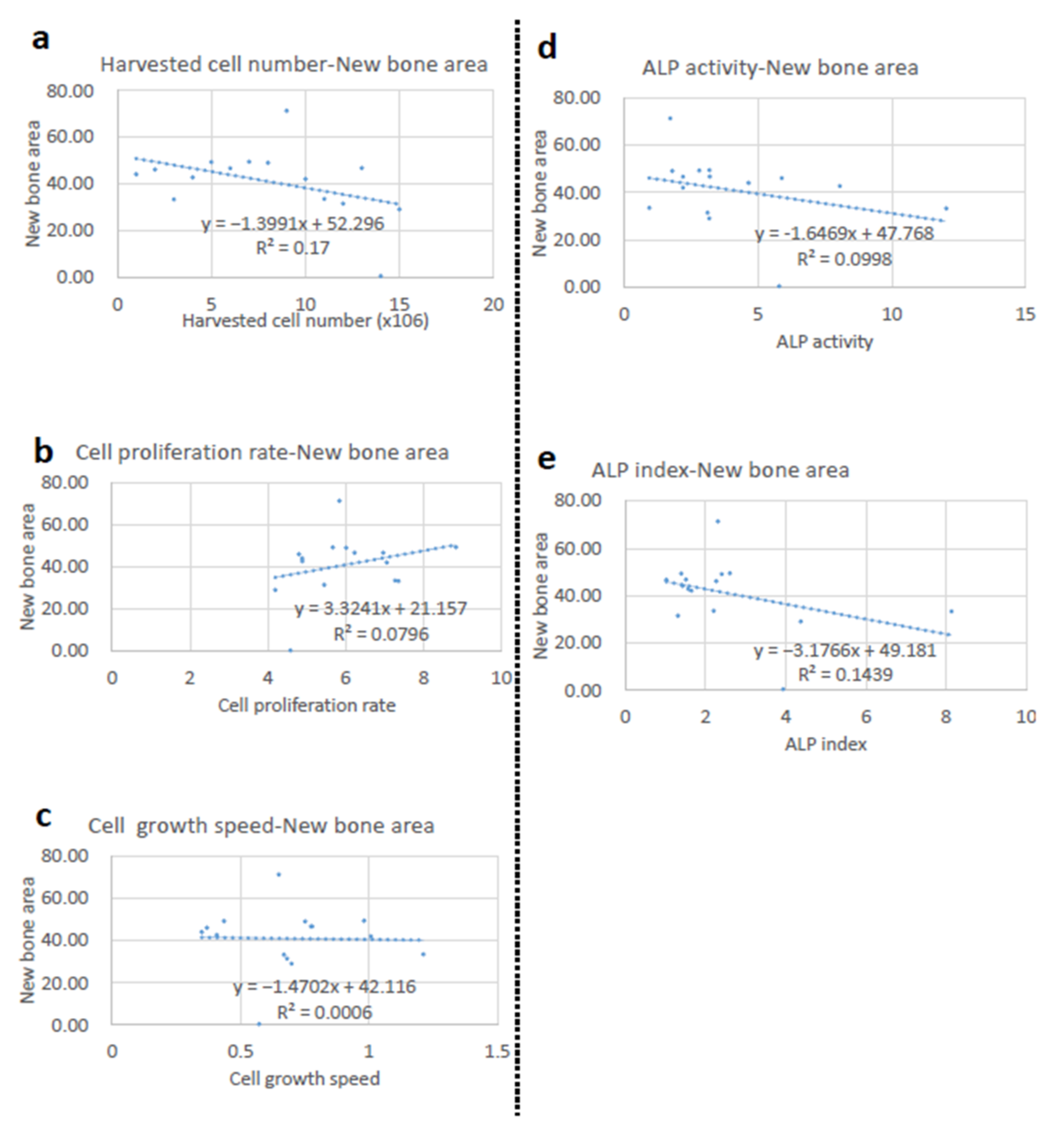
2.11. Statistical Analyses
For bone volume analysis, one-way ANOVA with Bonferroni correction was used for multiple comparisons as a post-test. A value of
p < 0.05 was considered statistically significant. For the histomorphometric analysis of regenerated bone, we conducted a pre-specified Bayesian inferiority test using the method of Thall and Sung [
14]. Specifically, if the posterior probability of the average bone area of current trial μ
C is larger than that of previous study μ
P minus non-inferiority margin δ (=13.92%), Pr[μ
C > μ
P – δ |y], is larger than 0.8, we consider our modified protocol was not inferior to the original protocol. Correlation coefficient was calculated using Excel (Microsoft Corporation, Redmond, Washington, DC, USA), and a correlation coefficient of less than 0.2 was considered as very weak or no association.
4. Discussion
In this study, an optimized protocol for cell processing was used [
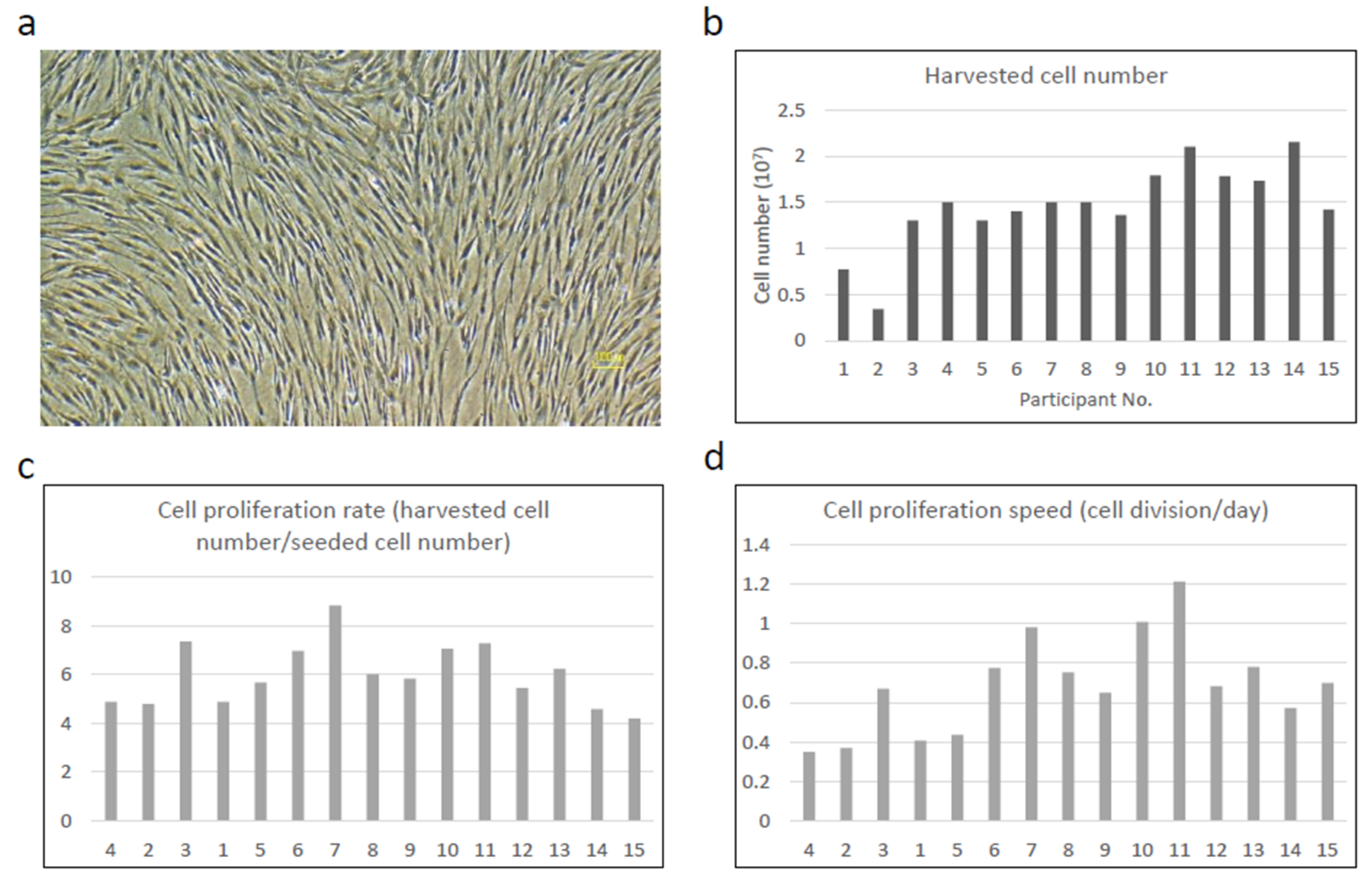
7,
12]. The optimized protocol limited the passage number, and bFGF was added to the culture medium, which may have affected the quality of the cells. A sufficient number of cells were harvested at passage 1 in all cases, and the cell number was identical to that of the previous study at passage 2 (1.5 × 10
7 cell versus 1.6 × 10
7 cells, respectively). In the preceding study, there was a case for which the protocol was discontinued due to the lack of cell proliferation. In this study, a sufficient number of cells was obtained in all cases (15 out of 15 cases). Although the results from only one case cannot be generalized, it is conceivable that the increased volume of bone marrow aspirate (20 mL vs. 10 mL) and the addition of bFGF in the culture medium contributed to the stable cell growth to sufficient number [
7]. In patients Nos. 1 and 2, the total cell number was relatively smaller than that in the other patients, although the cell proliferation rate (population doubling) was almost identical. This suggests that the difference might be due to the initial number of BMSCs in the bone marrow aspirate, but not due to the proliferation capability of BMSCs. Despite stable cell proliferation, ALP assay results showed significant individual variation. Although ALP is a conventional marker for osteogenic differentiation and has been widely used in both basic and clinical studies [
6], our previous study showed that the level of ALP activity did not parallel the in vivo osteogenic capability. The results of this study confirmed this finding, suggesting the limited usefulness of ALP activity for the quality assurance of BMSCs.
Safety was the primary endpoint of this clinical study. There were no side effects related to cell transplantation during the observation period (24 months) and up to now (8–10 years), which was comparable to the previous clinical study with the original protocol (no side effects or health concerns were noted) [
6]. The major safety concerns for tissue engineering using BMSCs include possible infection from transplanted cells and tumorigenic transformation. In this study, autologous cells were used to avoid potential donor infection. For the culture of individual cells, safety tests were performed, including the endotoxin test, mycoplasma test, and bacteriological examination. These commonly used tests appear to be effective in supporting the safety of cell transplantation. Tumorigenic transformation is considered a potential risk factor for BMSCs [
9]. In particular, genetic instability in BMSCs has been reported, which could cause malignant transformation [
15]. However, this is unlikely, and no such complications have been reported so far [
4,
5,
6,
16,
17]. The results from the present study further support the safety of BMSCs.
Fifteen participants were enrolled in this study, all of whom showed successful bone regeneration, which was sufficient to support implant instillation. Histomorphometric analysis of the bone biopsy sample was performed as the secondary endpoint. We conducted pre-specified Bayesian inferiority test using the method of Thall and Sung [
14]. The results showed that the average bone area was 41.51% in this trial, which was comparable to that in our previous study (41.9%) and Pr[μ
C > μ
P − δ |y] was 0.884; thus, the non-inferiority of this protocol was proven (
p < 0.05). Importantly, bone biopsy was performed 2 months earlier in the present study (4 months vs. 6 months after transplantation). Osteointegration of the implants installed in the tissue-engineered bone was 100%, and no implants were lost during the observation period, confirming the successful regeneration of functional bone.
It is well-known that regenerated bone shows resorption, which was also observed in tissue-engineered bone in our previous study [
6]. In this study, the volume of the regenerated bone was reduced to 63% over 24 months. This is one of the drawbacks of this protocol and should be considered when planning an operation. The histology of regenerated bone showed significant degradation and absorption of the β-TCP scaffold, which should be the reason for the initial volume reduction. However, radiographic images showed that the scaffold degraded after 12 months, and the morphology of the regenerated bone appeared to be like-normal by this stage, suggesting that the absorption after 12 months might be due to bone remodeling.
One of the major limitations of this study was the usage of a non-inferiority trial. A randomized controlled trial that compares this method with a clinical gold standard such as the autologous bone graft would be a preferable approach for future studies. In this study, autologous cells were used, which can avoid the triggering of immunological reactions and are safe in nature. However, their cell processing for clinical usage requires a GMP-compliant facility, and the process is highly labor-intensive. For the widespread usage of bone tissue engineering, allogenic cells should be considered; the development of a cell product such as an advanced therapy medicinal products (ATMP) is mandatory.
The optimization of the cell-processing protocol in this study was performed based on the in vivo bone-forming capability of cells, as the known osteogenic marker expression was not necessarily parallel to the level of bone formation in vivo [
7]. The results of this study clearly showed that BMSCs processed with the optimized protocol demonstrated bone regeneration with less individual variation compared to BMSCs processed with the conventional protocol. This suggests that an ectopic transplantation animal model using human cells can be used as a reliable model to predict clinical efficacy, which is important for future clinical studies. In contrast, as shown in an in vivo animal study [
7], all cell characteristic markers used in this study, such as cell proliferation and cell differentiation markers, did not correlate with clinical efficacy. The expression of higher levels of osteogenic markers may confirm the presence of osteogenic cells but does not support osteogenic function in vivo. This is a major drawback for quality assurance of cultured cells for bone tissue engineering, and further studies are needed.