The Safety and Impact of Raising the Urine Culture Reporting Threshold in Hospitalized Patients
Abstract
1. Introduction
1.1. Background Rationale
1.2. Objectives
2. Methods
2.1. Design
2.2. Setting
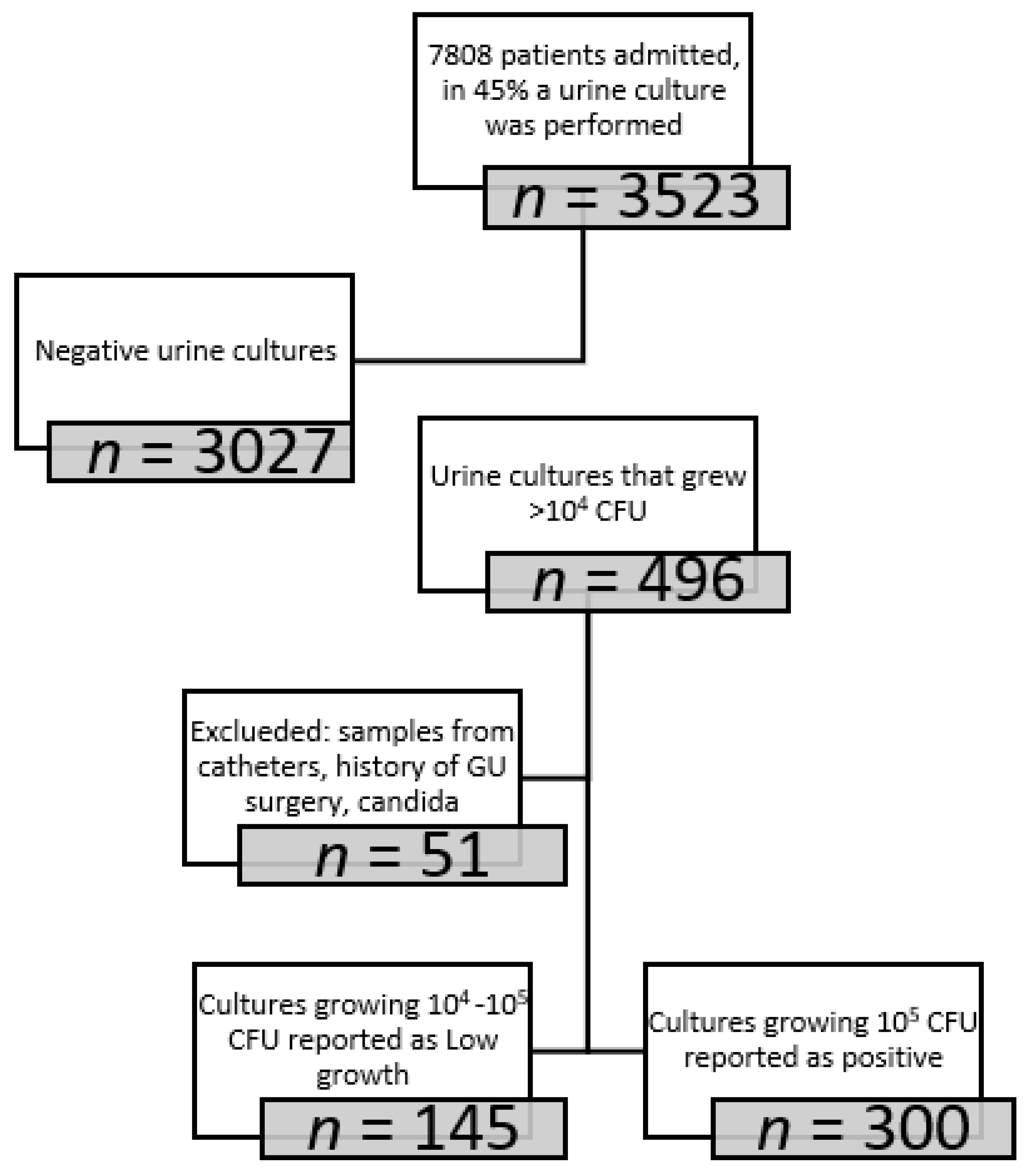
2.3. Participants
2.4. Intervention
2.5. Data
2.6. Outcomes
2.7. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mody, L.; Riddell, J.; Kaye, K.S.; Chopra, T. Common Infections. In Current Diagnosis & Treatment: Geriatrics, 2nd ed.; Williams, B.A., Chang, A., Ahalt, C., Chen, H., Conant, R., Landefeld, C.S., Ritchie, C., Yukawa, M., Eds.; McGraw-Hill Education: New York, NY, USA, 2014. [Google Scholar]
- Nicolle, L.E.; Gupta, K.; Bradley, S.F.; Colgan, R.; DeMuri, G.P.; Drekonja, D.; Eckert, L.O.; Geerlings, S.E.; Köves, B.; Hooton, T.M.; et al. Clinical Practice Guideline for the Management of Asymptomatic Bacteriuria: 2019 Update by the Infectious Diseases Society of Americaa. Clin. Infect. Dis. 2019, 68, e83–e110. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.R.; Little, P.J. Suprapubic Bladder Aspiration in Diagnosis of Urinary Tract Infection. BMJ 1969, 1, 293–294. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hooton, T.M.; Roberts, P.L.; Cox, M.E.; Stapleton, A.E. Voided Midstream Urine Culture and Acute Cystitis in Premenopausal Women. N. Engl. J. Med. 2013, 369, 1883–1891. [Google Scholar] [CrossRef] [PubMed]
- LaRocco, M.T.; Franek, J.; Leibach, E.K.; Weissfeld, A.S.; Kraft, C.S.; Sautter, R.L.; Baselski, V.; Rodahl, D.; Peterson, E.J.; Cornish, N.E. Effectiveness of Preanalytic Practices on Contamination and Diagnostic Accuracy of Urine Cultures: A Laboratory Medicine Best Practices Systematic Review and Meta-analysis. Clin. Microbiol. Rev. 2016, 29, 105–147. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.L.; Gaido, L. Laboratory Diagnosis of Urinary Tract Infections in Adult Patients. Clin. Infect. Dis. 2004, 38, 1150–1158. [Google Scholar] [CrossRef]
- Kass, E.H. Asymptomatic infections of the urinary tract. Trans. Assoc. Am. Physicians 1956, 69, 56–64. [Google Scholar] [PubMed]
- Platt, R. Quantitative definition of bacteriuria. Am. J. Med. 1983, 75, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Kunin, C.M.; White, L.V.; Hua, T.H. A Reassessment of the Importance of Low-Count Bacteriuria in Young Women with Acute Urinary Symptoms. Ann. Intern. Med. 1993, 119, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.H.; Fausone, M.K.; Du, H.; Robicsek, A.; Peterson, L.R. Impact of laboratory-reported urine culture colony counts on the diagnosis and treatment of urinary tract infection for hospitalized patients. Am. J. Clin. Pathol. 2012, 137, 778–784. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.-A.; Lamb, M.J.; Baillie, L.; Simor, A.; Leis, J.A. Clinical Significance of Low Colony-Count Urine Cultures Among Hospitalized Inpatients. Infect. Control Hosp. Epidemiol. 2018, 39, 488–489. [Google Scholar] [CrossRef] [PubMed]
- Leis, J.A.; Rebick, G.; Daneman, N.; Gold, W.L.; Poutanen, S.; Lo, P.; Larocque, M.; Shojania, K.G.; McGeer, A. Reducing Antimicrobial Therapy for Asymptomatic Bacteriuria Among Noncatheterized Inpatients: A Proof-of-Concept Study. Clin. Infect. Dis. 2014, 58, 980–983. [Google Scholar] [CrossRef] [PubMed]
- Tacconelli, E.; Cataldo, A.M.; Paul, M.; Leibovici, L.; Kluytmans, J.; Schröder, W.; Foschi, F.; De Angelis, G.; De Waure, C.; Cadeddu, C.; et al. STROBE-AMS: Recommendations to optimise reporting of epidemiological studies on antimicrobial resistance and informing improvement in antimicrobial stewardship. BMJ Open 2016, 6, e010134. [Google Scholar] [CrossRef]
- CLSI. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing an Informational Supplement for Global Application Developed through the Clinical and Laboratory Standards Institute Consensus Process, 26th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2016. [Google Scholar]
- Stamm, W.E.; Wagner, K.F.; Amsel, R.; Alexander, E.R.; Turck, M.; Counts, G.W.; Holmes, K.K. Causes of the Acute Urethral Syndrome in Women. N. Engl. J. Med. 1980, 303, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.; Hooton, T.M.; Naber, K.G.; Wullt, B.; Colgan, R.; Miller, L.G.; Moran, G.J.; Nicolle, L.E.; Raz, R.; Schaeffer, A.J.; et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin. Infect. Dis. 2011, 52, e103–e120. [Google Scholar] [CrossRef]
| Admission Duration | Length of Hospitalization in Which the Positive Urine Culture Was Identified |
|---|---|
| No antibiotics therapy | Patients in whom no antibiotic therapy was provided during the hospitalization or recommended on discharge |
| Antibiotic therapy duration | Length of antibiotic therapy during hospitalization |
| Recurrent admission 30 day | Patients who were readmitted for any cause within 30 days |
| positive urine culture 90-day same pathogen | A positive urine culture obtained within 90 days of the original culture and grew the same pathogen as the original culture |
| positive urine culture 90-day different pathogen | A positive urine culture obtained within 90 days of the original culture and grew a different from the original culture |
| Bacteremia within 30 day | Bacteremia within 30 days of the same pathogen that grew in the original urine culture |
| Mortality all cause 90 day | All-cause mortality within 90 days |
| C. difficile | Patients who developed C. difficle infection within 3 months of the positive culture |
| Reported Low Growth n = 145 n (%) | Reported Positive n = 300 n (%) | p Value | |
|---|---|---|---|
| Gender female | 97 (68.3) | 217 (72.3) | 0.384 |
| Age (standard deviation) | 58 ± 23 | 59 ± 24 | 0.578 |
| Diabetes mellitus | 45 (31.7) | 91 (30.3) | 0.773 |
| Chronic renal failure | 25 (17.6) | 52 (17.3) | 0.944 |
| Congestive heart failure | 8 (5.6) | 25 (8.3) | 0.313 |
| Chronic heart disease | 18 (12.7) | 49 (16.3) | 0.317 |
| Chronic lung disease | 11 (7.7) | 12 (4) | 0.098 |
| History of Stroke | 11 (7.7) | 27 (9) | 0.661 |
| Charleston comorbidity score Median (IQR 25.75) | 1 (0.3) | 1 (0.3) | 0.931 |
| Fever > 38.2 | 67 (47.2) | 155 (51.7) | 0.379 |
| Presented with Hypotension MAP < 70 | 11 (7.7) | 17 (5.7) | 0.402 |
| Presented with WBC > 10,000 | 65 (45.8) | 131 (43.7) | 0.677 |
| Bacteremia on presentation same pathogen as urine | 6 (4.1) | 16 (5.3) | 0.649 |
| Bacteremia on presentation different pathogen | 1(0.6) | 3 (1%) | 0.998 |
| Reported Low Growth n = 145 n (%) | Reported Positive n = 300 n (%) | p Value | |
|---|---|---|---|
| Escherichia coli | 84 (58) | 192 (64) | 0.128 |
| Klebsiella spp. | 17 (12) | 57 (19) | 0.057 |
| Enterococcus spp. | 19 (13) | 12 (4) | <0.001 |
| Pseudomonas aeruginosa | 13 (9) | 12 (4) | 0.028 |
| Proteus mirabilis | 8 (6) | 16 (5) | 0.999 |
| Morganella morganii | 4 (2) | 11 (4) | 0.999 |
| LOW Growth (%) | Positive Growth (%) | ||
|---|---|---|---|
| Antibiotic treatment | 100(69%) | 244(81.3%) | p = 0.015 |
| Not treated | 45(31%) | 56(18.7%) | p = 0.015 |
| Not treated recurrent hospitalization | 1(2.2%) | 7(12.5%) | p = 0.057 |
| Not treated Bacteremia within 30 d | 4(8.8%) | 6(10.7%) | p = 0.756 |
| Not treated mortality | 3(6.6%) | 5(8.9%) | p = 0.418 |
| Reported Low Growth n = 145 n (%) | Reported Positive n = 300 n (%) | p Value | |
|---|---|---|---|
| Admission duration median (IQR 25.75) | 3 (0.7) | 3 (0.6) | 0.879 |
| No antibiotics therapy | 45 (31) | 56 (18.7) | 0.015 |
| Antibiotic therapy duration median (IQR 25.75) | 5 (0.9) | 6 (0.9) | 0.015 |
| Recurrent admission 30 day | 18 (12.7) | 39 (13) | 0.924 |
| Pyelonephritis within 30 day | 0 (0) | 3 (1) | 0.764 |
| Positive urine culture 90-day same pathogen | 6 (4.2) | 12 (4) | 1 |
| Positive urine culture 90-day different pathogen | 4 (2.7) | 10 (3.3) | 0.785 |
| Bacteremia within 30 day | 1 (0.6) | 2 (0.7) | 0.507 |
| Mortality all cause 90 day | 8 (5.6) | 22 (7.3) | 0.507 |
| C. difficle | 0 (0) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gabay, O.; Cherki, T.; Tsaban, G.; Bichovsky, Y.; Nesher, L. The Safety and Impact of Raising the Urine Culture Reporting Threshold in Hospitalized Patients. J. Clin. Med. 2022, 11, 7014. https://doi.org/10.3390/jcm11237014
Gabay O, Cherki T, Tsaban G, Bichovsky Y, Nesher L. The Safety and Impact of Raising the Urine Culture Reporting Threshold in Hospitalized Patients. Journal of Clinical Medicine. 2022; 11(23):7014. https://doi.org/10.3390/jcm11237014
Chicago/Turabian StyleGabay, Ohad, Tal Cherki, Gal Tsaban, Yoav Bichovsky, and Lior Nesher. 2022. "The Safety and Impact of Raising the Urine Culture Reporting Threshold in Hospitalized Patients" Journal of Clinical Medicine 11, no. 23: 7014. https://doi.org/10.3390/jcm11237014
APA StyleGabay, O., Cherki, T., Tsaban, G., Bichovsky, Y., & Nesher, L. (2022). The Safety and Impact of Raising the Urine Culture Reporting Threshold in Hospitalized Patients. Journal of Clinical Medicine, 11(23), 7014. https://doi.org/10.3390/jcm11237014







