What Exactly Makes Age a Risk Factor for an Unfavorable Outcome after Mitral Valve Surgery?
Abstract
1. Background
2. Patients and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Baseline and Comorbidities
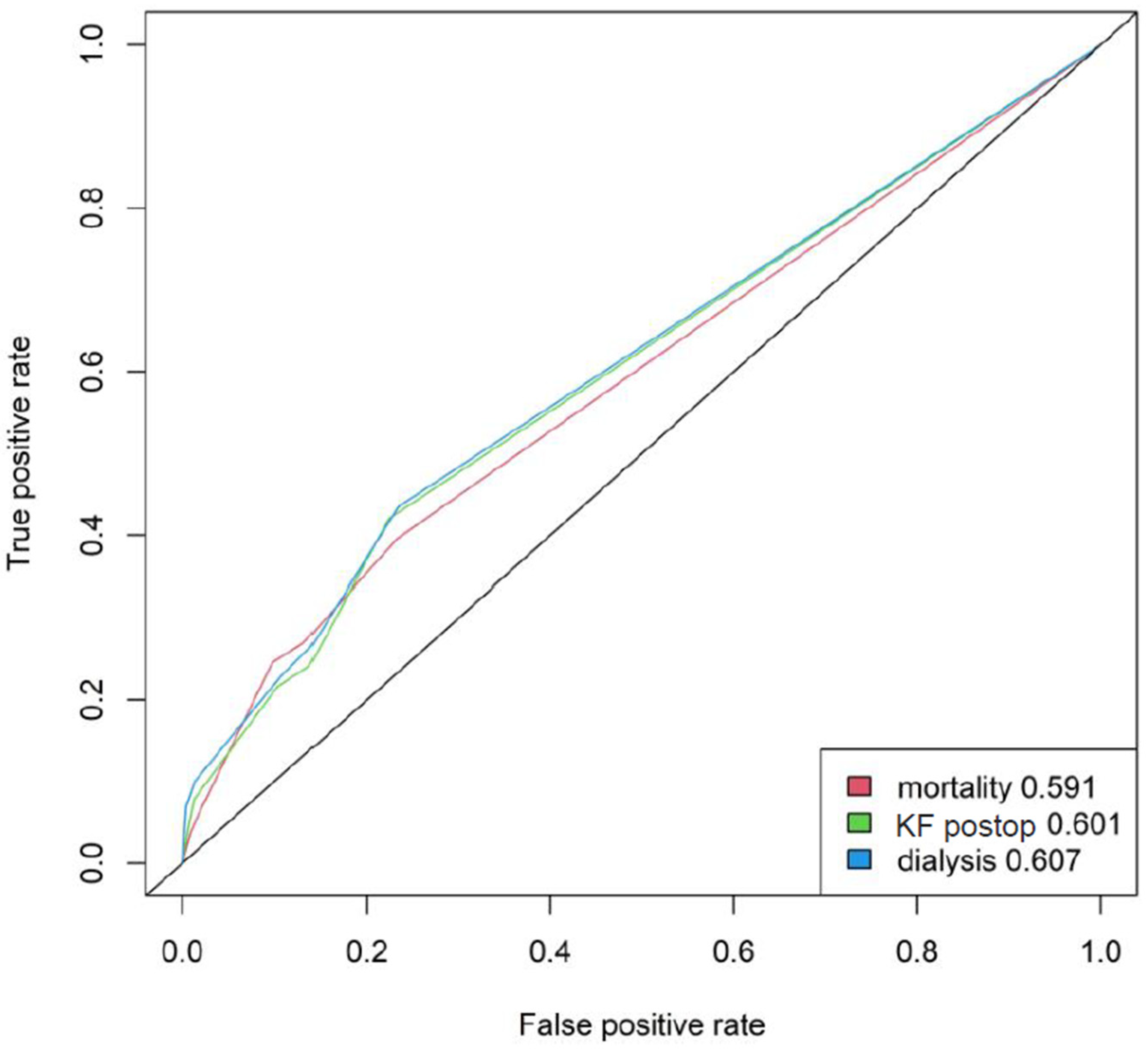
3.2. Outcome
3.3. Age-Related Complications
3.4. Subgroup Analysis in Advanced Age
4. Discussion
Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Podsiadlo, D.; Richardson, S. The timed “Up & Go“: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Bohannon, R.W. Sit-to-stand test for measuring performance of lower extremity muscles. Percept. Mot. Ski. 1995, 80, 163–166. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Wang, L.; Ren, J. Aging as a risk factor for cardiac surgery: Blunted ischemic-reperfusion stress response? J. Card. Surg. 2021, 36, 3641–3642. [Google Scholar] [CrossRef]
- Humphreys, B.D. Mechanisms of Renal Fibrosis. Annu. Rev. Physiol. 2018, 80, 309–326. [Google Scholar] [CrossRef]
- Walker, S.R.; Wagner, M.; Tangri, N. Chronic kidney disease, frailty, and unsuccessful aging: A review. J. Ren. Nutr. 2014, 24, 364–370. [Google Scholar] [CrossRef]
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging 2018, 13, 757–772. [Google Scholar] [CrossRef]
- Morcos, R.; Lazar, I.; Kucharik, M.; Lavin, A.; Fahmy, A.; Chandrasekhar, S.; Ibrahim, A.; Neupane, A.; Khalili, H.; Maini, B.; et al. The Healthy, Aging, and Diseased Kidney: Relationship with Cardiovascular Disease. J. Am. Geriatr. Soc. 2021, 69, 539–546. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 10 January 2022).
- Kamijo, Y.; Kanda, E.; Ishibashi, Y.; Yoshida, M. Sarcopenia and Frailty in PD: Impact on Mortality, Malnutrition, and Inflammation. Perit. Dial. Int. 2018, 38, 447–454. [Google Scholar] [CrossRef]
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; McLean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M.; et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final estimates. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2014, 69, 547–558. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Wu, L.C.; Kao, H.H.; Chen, H.J.; Huang, P.F. Preliminary screening for sarcopenia and related risk factors among the elderly. Medicine 2021, 100, e25946. [Google Scholar] [CrossRef]
- Bolton, C.F.; Laverty, D.A.; Brown, J.D.; Witt, N.J.; Hahn, A.F.; Sibbald, W.J. Critically ill polyneuropathy: Electrophysiological studies and differentiation from Guillain-Barre syndrome. J. Neurol. Neurosurg. Psychiatry 1986, 49, 563–573. [Google Scholar] [CrossRef]
- Witt, N.J.; Zochodne, D.W.; Bolton, C.F.; Grand’Maison, F.; Wells, G.; Young, G.B.; Sibbald, W.J. Peripheral nerve function in sepsis and multiple organ failure. Chest 1991, 99, 176–184. [Google Scholar] [CrossRef]
- Bolton, C.F.; Young, G.B.; Zochodne, D.W. The neurological complications of sepsis. Ann. Neurol. 1993, 33, 94–100. [Google Scholar] [CrossRef]
- De Jonghe, B.; Sharshar, T.; Lefaucheur, J.P.; Authier, F.J.; Durand-Zaleski, I.; Boussarsar, M.; Cerf, C.; Renaud, E.; Mesrati, F.; Carlet, J.; et al. Paresis acquired in the intensive care unit: A prospective multicenter study. JAMA 2002, 288, 2859–2867. [Google Scholar] [CrossRef]
- Divo, M.J.; Martinez, C.H.; Mannino, D.M. Ageing and the epidemiology of multimorbidity. Eur. Respir. J. 2014, 44, 1055–1068. [Google Scholar] [CrossRef]
- Mallappallil, M.; Friedman, E.A.; Delano, B.G.; McFarlane, S.I.; Salifu, M.O. Chronic kidney disease in the elderly: Evaluation and management. Clin. Pract. 2014, 11, 525–535. [Google Scholar] [CrossRef]
- Ray, S.; Mukherjee, S.; Ganguly, J.; Abhishek, K.; Mitras, S.; Kundu, S. A cross-sectional prospective study of pleural effusion among cases of chronic kidney disease. Indian J. Chest Dis. Allied Sci. 2013, 55, 209–213. [Google Scholar]
- Maher, J.F. Uremic pleuritis. Am. J. Kidney Dis. 1987, 10, 19–22. [Google Scholar] [CrossRef]
- Jabbar, A.; Qureshi, R.; Nasir, K.; Dhrolia, M.; Ahmad, A. Transudative and Exudative Pleural Effusion in Chronic Kidney Disease Patients: A Prospective Single-Center Study. Cureus 2021, 13, e18649. [Google Scholar] [CrossRef]
- Zeng, Q.X.; Jiang, K.L.; Wu, Z.H.; Huang, D.L.; Huang, Y.S.; Zhuang, H.W.; Zhong, H.J. Pleural Effusion Is Associated with Severe Renal Dysfunction in Patients with Acute Pancreatitis. Med. Sci. Monit. 2021, 27, e928118. [Google Scholar] [CrossRef]
- Hartrumpf, M.; Kuehnel, R.U.; Albes, J.M. The obesity paradox is still there—A risk analysis of over 15,000 cardiosurgical patients based on body mass index. Interact. Cardiovasc. Thorac. Surg. 2017, 25, 18–24. [Google Scholar] [CrossRef]

| Age-Distribution (Years) | 40–59 | 60–74 | ≥75 | p-Value |
|---|---|---|---|---|
| Gender (male) | 78.7% | 60% | 46.8% | <0.001 |
| Mean logistic EuroSCORE (%) | 10.4 ± 15.1 | 15.3 ± 17.3 | 22.7 ± 20.6 | <0.001 |
| Body mass index (kg/m2) | 27.7 ± 5.1 | 28.2 ± 5.5 | 27.3 ± 4.8 | 0.007 |
| LVEF (%) | 50.9 ± 13.6 | 51.3± 13.3 | 51.9 ± 12.5 | n.s. |
| TAPSE (mm) | 21.88 ± 5.88 | 20.95 ± 5.94 | 19.87 ± 5.22 | 0.006 |
| PAP (mmHg) | 34.1 ± 13.9 | 39.45 ± 16.63 | 41.01 ± 15.16 | <0.001 |
| NT-proBNP (pg/mL) | 6445.5 ± 33,442.5 | 3904.2± 6918.5 | 4948.7 ± 19,704.3 | n.s. |
| Chronic kidney disease | 16.05% | 24.79% | 36.06% | <0.001 |
| Stage 1 | 6.02% | 9.94% | 14.82% | |
| Stage 2 | 3.01% | 3.50% | 2.65% | |
| Stage 3 | 2.68% | 9.24% | 16.37% | |
| Stage 4 | 1.34% | 0.84% | 1.77% | |
| Stage 5 | 3.34% | 1.26% | 0.44% | |
| Coronary heart disease (CHD) | 35.79% | 54.41% | 59.07% | <0.001 |
| One vessel CHD | 7.36% | 14.13% | 13.94% | |
| Two vessel CHD | 5.69% | 11.05% | 13.27% | |
| Three vessel CHD | 22.74% | 28.95% | 32.08% | |
| History of cancer | 8.75% | 11.66% | 15.96% | 0.003 |
| Atrial fibrillation | 25.59% | 48.38% | 55.28% | <0.001 |
| Arterial hypertension | 63.64% | 83.64% | 90.04% | <0.001 |
| COPD | 6.85% | 11.37% | 10.84% | n.s. |
| Peripheral arterial disease | 4.38% | 7.12% | 6.84% | n.s. |
| Pulmonary arterial hypertension | 13.7% | 16.4% | 14.9% | n.s. |
| Age Distribution | 40–59 | 60–74 | ≥75 | p-Value |
|---|---|---|---|---|
| renal failure | 14.09% [42] | 21.59% [152] | 28.09% [125] | <0.001 |
| dialysis requirement | 10.74% [32] | 16.45% [116] | 18.43% [82] | 0.007 |
| pleural effusions | 11.78% [35] | 16.64% [118] | 24.33% [109] | <0.001 |
| pericardial effusions | 4.7% [14] | 7.19% [51] | 9.4% [42] | 0.016 |
| respiratory insufficiency | 12.79% [38] | 17.63% [125] | 23.66% [106] | <0.001 |
| CIP/CIM | 1.34% [4] | 3.95% [28] | 4.25% [19] | 0.049 |
| Stroke | 1.69% [5] | 3.16% [22] | 3.41% [15] | 0.204 |
| Wound healing disorder | 3.36% [10] | 4.1% [29] | 4.26% [19] | 0.695 |
| Low output syndrome | 7.38% [22] | 5.36% [38] | 8.48% [38] | 0.384 |
| Pneumonia | 6.04% [18] | 7.62% [54] | 9.17% [41] | 0.114 |
| urinary tract infection | 1.01% [3] | 1.27% [9] | 2.47% [11] | 0.093 |
| SIRS | 18.79% [56] | 18.79% [133] | 22.99% [103] | 0.119 |
| Pneumothorax | 2.68% [8] | 2.4% [17] | 2.46% [11] | 0.865 |
| Atrial fibrillation | 5.39% [16] | 6.95% [49] | 6.09% [27] | 0.902 |
| AV-Block II° or III° | 2.36% [7] | 2.27% [16] | 2.26% [10] | 0.998 |
| Age-Distribution (Years) | 70–75 | 75–80 | >80 | p-Value |
|---|---|---|---|---|
| Gender (female) | 45.5% | 52% | 56.8% | 0.017 |
| Mean logistic EuroSCORE (%) | 17.7 ± 18.8 | 21.4 ± 20.2 | 26.5 ± 21.4 | <0.001 |
| Body mass index (kg/m2) | 27.6 ± 4.9 | 27.5 ± 4.9 | 26.5 ± 4.2 | 0.05 |
| Chronic kidney disease | 28.71% | 35.71% | 37.07% | 0.034 |
| Coronary heart disease | 39.8% | 40.48% | 41.38% | n.s. |
| History of cancer | 13.82% | 14.33% | 20.69% | n.s. |
| Atrial fibrillation | 52% | 51.2% | 54.87% | n.s. |
| Arterial hypertension | 85.2% | 91.37% | 86.21% | n.s. |
| COPD | 13.13% | 10.37% | 12.17% | n.s. |
| Peripheral arterial disease | 5.9% | 6.82% | 6.9% | n.s. |
| Pulmonary arterial hypertension | 17.51% | 14.63% | 15.65% | n.s. |
| Postoperative Complications | ||||
| Acute kidney failure | 24.5% | 23.87% | 40.35% | 0.009 |
| Dialysis requirement | 19.4% | 15.71% | 26.32% | n.s. |
| Pleural effusions | 17.88% | 22.22% | 30.43% | 0.006 |
| Pericardial effusions | 5.96% | 9.91% | 7.89% | n.s. |
| Respiratory insufficiency | 17.55% | 21.62% | 29.57% | 0.009 |
| CIP/CIM | 3.64% | 3.31% | 6.96% | n.s. |
| Stroke | 4.75% | 2.44% | 6.25% | n.s. |
| Low output syndrome | 5.96% | 7.51% | 11.3% | n.s. |
| Pneumonia | 7.28% | 7.53% | 13.91% | n.s. |
| SIRS | 20.27% | 21.02% | 28.7% | n.s. |
| In-hospital Mortality | 19.7% | 22.57% | 40.91% | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ostovar, R.; Schröter, F.; Kühnel, R.-U.; Hartrumpf, M.; Albes, J.M. What Exactly Makes Age a Risk Factor for an Unfavorable Outcome after Mitral Valve Surgery? J. Clin. Med. 2022, 11, 6907. https://doi.org/10.3390/jcm11236907
Ostovar R, Schröter F, Kühnel R-U, Hartrumpf M, Albes JM. What Exactly Makes Age a Risk Factor for an Unfavorable Outcome after Mitral Valve Surgery? Journal of Clinical Medicine. 2022; 11(23):6907. https://doi.org/10.3390/jcm11236907
Chicago/Turabian StyleOstovar, Roya, Filip Schröter, Ralf-Uwe Kühnel, Martin Hartrumpf, and Johannes Maximilian Albes. 2022. "What Exactly Makes Age a Risk Factor for an Unfavorable Outcome after Mitral Valve Surgery?" Journal of Clinical Medicine 11, no. 23: 6907. https://doi.org/10.3390/jcm11236907
APA StyleOstovar, R., Schröter, F., Kühnel, R.-U., Hartrumpf, M., & Albes, J. M. (2022). What Exactly Makes Age a Risk Factor for an Unfavorable Outcome after Mitral Valve Surgery? Journal of Clinical Medicine, 11(23), 6907. https://doi.org/10.3390/jcm11236907







