Transversus Abdominis Plane Block as a Strategy for Effective Pain Management in Patients with Pain during Laparoscopic Cholecystectomy: A Systematic Review
Abstract
1. Introduction
2. Objectives
- Explore the optimal dose of TAP block anesthesia for laparoscopic cholecystectomy.
- Identify the types and concentrations of local anesthetics and other supportive agents commonly used for laparoscopic cholecystectomy.
- Compare the analgesic efficacy of different types of TAP block procedures and their long-term effects.
- Examine the clinical significance of TAP.
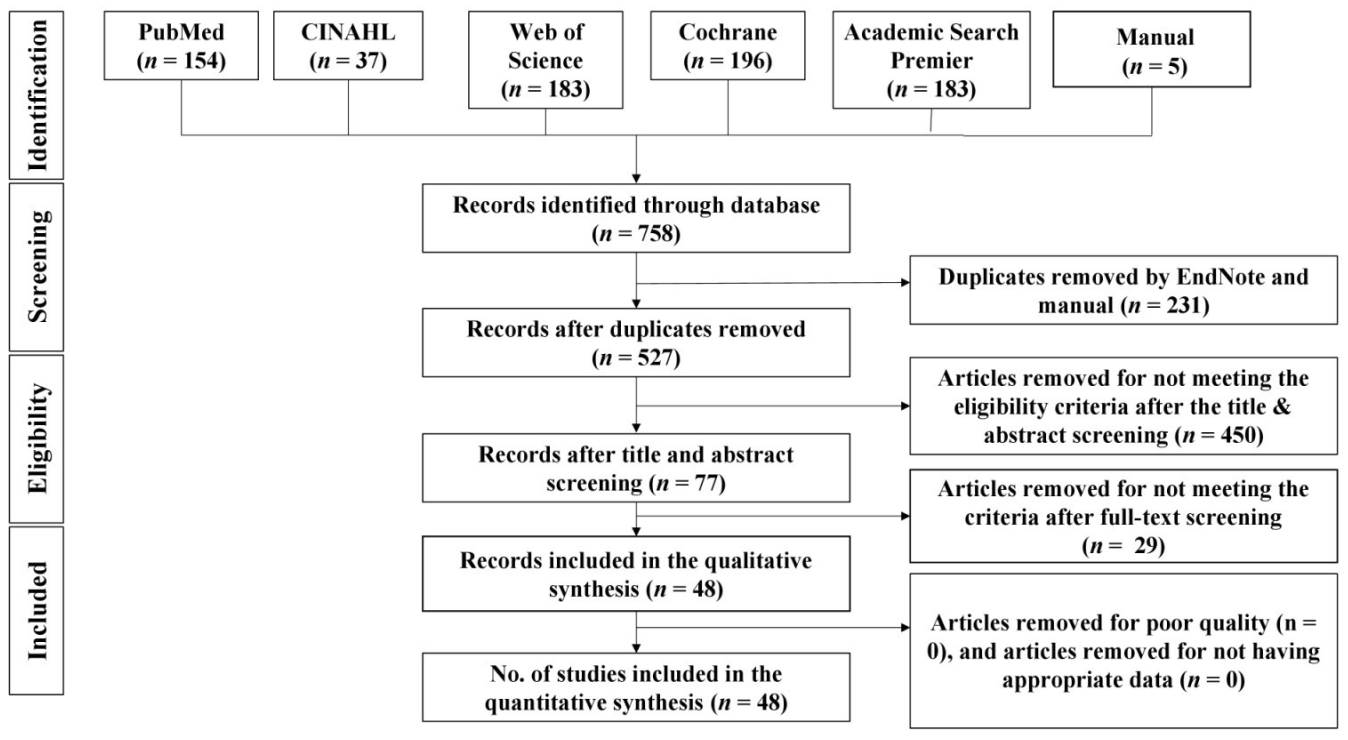
3. Methods
4. Eligibility Criteria
Inclusion Criteria
- 5.
- Population: Adult patients undergoing LC.
- 6.
- Intervention: Postoperative pain management using TAP block or in combination with adjutants.
- 7.
- Comparators: Active placebo or adjunct treatment.
- 8.
- Outcomes: Postoperative use of analgesia use if they reported a visual analogue scale (VAS) or numeric rating scale (NRS) outcome of postoperative pain after 24 h.
- 9.
- Design: Randomized trials published in peer-reviewed journals.
5. Exclusion Criteria
6. Information Sources
7. Search
8. Study Selection
9. Data Collection Process
10. Data Items
11. Risk of Bias in Individual Studies
12. Summary of Measure and Synthesis of Results
13. Results
14. Risk of Bias within Studies
15. Study Characteristics
15.1. Objective #1. The Optimal Dose of TAP Block Anesthesia for Laparoscopic Cholecystectomy
15.2. Objective #2. Types and Concentrations of Local Anesthetics and Other Supportive Agents Commonly Used for Laparoscopic Cholecystectomy
15.3. Objective #3. Effects of TAP Block Anesthesia
- a.
- Comparison of different approaches to ultrasound-guided blockade of the transversus abdominis plane
15.3.1. Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block Versus General Anesthesia Only
15.3.2. Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block versus Port SITES Infiltration
15.3.3. Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block before Induction of Anesthesia and after Surgery
15.3.4. Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block Using Different Concentrations of Local Anesthetics versus Normal Saline
15.3.5. Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Block Using Different Concentrations of Local Anesthetics
15.3.6. Comparison of Analgesic Efficacy of Ultrasound-Guided Oblique Subcostal Transversus Abdominis Block versus Transversus Abdominis Plane Block
15.3.7. Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Plane Blockade with Equal Anesthetic Concentration and Adjuvant of Dexamethasone, and Dexmedetomidine versus Normal Saline
15.3.8. Analgesic Efficacy of Ultrasound-Guided Subcostal Transversus Abdominis Plane versus Quadratus Lumborum Blocks
15.3.9. Analgesic Efficacy of Ultrasound-Guided Transversus Abdominis Versus Quadratus Lumborum Blocks
- b.
- Comparison of different approaches to laparoscopic-assisted transversus abdominal blockade
15.3.10. Comparison of Analgesic Efficacy Analgesic Efficacy of Laparoscopic-Assisted Transversus Abdominal Block with Bupivacaine versus Normal Saline
15.3.11. Analgesic Efficacy of Laparoscopic-Assisted Transversus Abdominal Block versus Port Sites Infiltration
15.3.12. Analgesic Efficacy of Laparoscopic-Assisted Infiltration Using Different Doses of Local Anesthetic versus Normal Saline
- c.
- Other known techniques
16. Long-Term Effects
Objective #4. Clinical Significance of TAP Block
17. Discussion
18. Limitations
19. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mitra, S.; Khandelwal, P.; Roberts, K.; Kumar, S.; Vadivelu, N. Pain relief in laparoscopic cholecystectomy—A review of the current options. Pain Pract. 2012, 12, 485–496. [Google Scholar]
- Bisgaard, T.; Warltier, D.C. Analgesic treatment after laparoscopic cholecystectomy: A critical assessment of the evidence. Anesthesiology 2006, 104, 835–846. [Google Scholar] [CrossRef]
- Johns, N.; O’Neill, S.; Ventham, N.; Barron, F.; Brady, R.; Daniel, T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: A systematic review and meta-analysis. Color. Dis. 2012, 14, e635–e642. [Google Scholar]
- Tekeli, A.E.; Eker, E.; Bartin, M.K.; Öner, M.Ö. The efficacy of transversus abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy cases: A retrospective evaluation of 515 patients. J. Int. Med. Res. 2020, 48, 1–9. [Google Scholar] [CrossRef]
- Abrahams, M.S.; Horn, J.-L.; Noles, L.M.; Aziz, M.F. Evidence-based medicine: Ultrasound guidance for truncal blocks. Reg. Anesthesia Pain Med. 2010, 35, S36–S42. [Google Scholar] [CrossRef]
- Bhatia, N.; Arora, S.; Jyotsna, W.; Kaur, G. Comparison of posterior and subcostal approaches to ultrasound-guided transverse abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy. J. Clin. Anesth. 2014, 26, 294–299. [Google Scholar] [CrossRef]
- Ra, Y.S.; Kim, C.H.; Lee, G.Y.; Han, J.I. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J. Anesthesiol. 2010, 58, 362–368. [Google Scholar] [CrossRef]
- Wassef, M.; Lee, D.Y.; Levine, J.; Ross, R.E.; Guend, H.; Vandepitte, C.; Hadzic, A.; Teixeira, J. Feasibility and analgesic efficacy of the transversus abdominis plane block after single-port laparoscopy in patients having bariatric surgery. J. Pain Res. 2013, 6, 837–841. [Google Scholar] [CrossRef]
- Statzer, N.; Cummings, K.C. Transversus abdominis plane blocks. Adv. Anesth. 2018, 36, 163–180. [Google Scholar]
- Rafi, A.N. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia 2001, 56, 1024–1026. [Google Scholar] [CrossRef]
- Rozen, W.; Tran, T.; Ashton, M.; Barrington, M.; Ivanusic, J.; Taylor, G. Refining the course of the thoracolumbar nerves: A new understanding of the innervation of the anterior abdominal wall. Clin. Anat. 2008, 21, 325–333. [Google Scholar] [CrossRef]
- Szental, J.; Webb, A.; Weeraratne, C.; Campbell, A.; Sivakumar, H.; Leong, S. Postoperative pain after laparoscopic cholecystectomy is not reduced by intraoperative analgesia guided by analgesia nociception index (ANI®) monitoring: A randomized clinical trial. Br. J. Anaesth. 2015, 114, 640–645. [Google Scholar]
- Brogi, E.; Kazan, R.; Cyr, S.; Giunta, F.; Hemmerling, T.M. Transversus abdominal plane block for postoperative analgesia: A systematic review and meta-analysis of randomized-controlled trials. Can. J. Anaesth. 2016, 63, 1184–1196. [Google Scholar] [CrossRef]
- Champaneria, R.; Shah, L.; Geoghegan, J.; Gupta, J.K.; Daniels, J.P. Analgesic effectiveness of transversus abdominis plane blocks after hysterectomy: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 166, 1–9. [Google Scholar] [CrossRef]
- Elkassabany, N.; Ahmed, M.; Malkowicz, S.B.; Heitjan, D.F.; Isserman, J.A.; Ochroch, E.A. Comparison between the analgesic efficacy of transversus abdominis plane (TAP) block and placebo in open retropubic radical prostatectomy: A prospective, randomized, double-blinded study. J. Clin. Anesth. 2013, 25, 459–465. [Google Scholar] [CrossRef]
- Abdallah, F.W.; Laffey, J.G.; Halpern, S.H.; Brull, R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: A meta-analysis. Br. J. Anaesth. 2013, 111, 721–735. [Google Scholar] [CrossRef]
- Maeda, A.; Shibata, S.C.; Kamibayashi, T.; Fujino, Y. Continuous subcostal oblique transversus abdominis plane block provides more effective analgesia than single-shot block after gynaecological laparotomy. Eur. J. Anaesthesiol. 2015, 32, 514–515. [Google Scholar] [CrossRef]
- Niraj, G.; Kelkar, A.; Hart, E.; Kaushik, V.; Fleet, D.; Jameson, J. Four quadrant transversus abdominis plane block and continuous transversus abdominis plane analgesia: A 3-year prospective audit in 124 patients. J. Clin. Anesth. 2015, 27, 579–584. [Google Scholar] [CrossRef]
- Hutchins, J.L.; Kesha, R.; Blanco, F.; Dunn, T.; Hochhalter, R. Ultrasound-guided subcostal transversus abdominis plane blocks with liposomal bupivacaine vs. non-liposomal bupivacaine for postoperative pain control after laparoscopic hand-assisted donor nephrectomy: A prospective randomised observer-blinded study. Anaesthesia 2016, 71, 930–937. [Google Scholar] [CrossRef]
- Ortiz, J.; Suliburk, J.; Wu, K.; Bailard, N.S.; Mason, C.; Minard, C.G.; Palvadi, R.R. Bilateral Transversus Abdominis Plane Block Does Not Decrease Postoperative Pain After Laparoscopic Cholecystectomy When Compared with Local Anesthetic Infiltration of Trocar Insertion Sites. Reg. Anesth. Pain Med. 2012, 37, 188–192. [Google Scholar] [CrossRef]
- Petersen, P.L.; Stjernholm, P.; Kristiansen, V.B.; Torup, H.; Hansen, E.G.; Mitchell, A.U.; Moeller, A.; Rosenberg, J.; Dahl, J.B.; Mathiesen, O. The Beneficial Effect of Transversus Abdominis Plane Block After Laparoscopic Cholecystectomy in Day-Case Surgery. Anesth. Analg. 2012, 115, 527–533. [Google Scholar] [CrossRef]
- Kaye, A.; Urman, R.; Rappaport, Y.; Siddaiah, H.; Cornett, E.; Belani, K.; Salinas, O.; Fox, C. Multimodal analgesia as an essential part of enhanced recovery protocols in the ambulatory settings. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, 40–45. [Google Scholar] [CrossRef]
- Koyyalamudi, V.; Sen, S.; Patil, S.; Creel, J.B.; Cornett, E.M.; Fox, C.J.; Kaye, A.D. Adjuvant Agents in Regional Anesthesia in the Ambulatory Setting. Curr. Pain Headache Rep. 2017, 21, 6. [Google Scholar] [CrossRef]
- Bisgaard, T.; Klarskov, B.; Rosenberg, J.; Kehlet, H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain 2001, 90, 261–269. [Google Scholar]
- Desai, N.; El-Boghdadly, K.; Albrecht, E. Epidural vs. transversus abdominis plane block for abdominal surgery–a systematic review, meta-analysis and trial sequential analysis. Anaesthesia 2021, 76, 101–117. [Google Scholar]
- Grape, S.; Kirkham, K.R.; Akiki, L.; Albrecht, E. Transversus abdominis plane block versus local anesthetic wound infiltration for optimal analgesia after laparoscopic cholecystectomy: A systematic review and meta-analysis with trial sequential analysis. J. Clin. Anesth. 2021, 75, 110450. [Google Scholar]
- Panda, A.; Saxena, S.; Pathak, M.; Rath, S. Laparoscopic assisted versus ultrasound guided transversus abdominis plane block in laparoscopic surgeries: A systematic review and meta-analysis. Trends Anaesth. Crit. Care 2022, 44, 20–26. [Google Scholar] [CrossRef]
- Peng, K.; Ji, F.-H.; Liu, H.-Y.; Wu, S.-R. Ultrasound-Guided Transversus Abdominis Plane Block for Analgesia in Laparoscopic Cholecystectomy: A Systematic Review and Meta-Analysis. Med. Princ. Pract. 2016, 25, 237–246. [Google Scholar]
- Howle, R.; Ng, S.-C.; Wong, H.-Y.; Onwochei, D.; Desai, N. Comparison of analgesic modalities for patients undergoing midline laparotomy: A systematic review and network meta-analysis. Can. J. Anaesth. 2021, 69, 140–176. [Google Scholar]
- Liheng, L.; Siyuan, C.; Zhen, C.; Changxue, W. Erector Spinae Plane Block versus Transversus Abdominis Plane Block for Postoperative Analgesia in Abdominal Surgery: A Systematic Review and Meta-Analysis. J. Investig. Surg. 2022, 35, 1711–1722. [Google Scholar]
- Liu, X.; Song, T.; Chen, X.; Zhang, J.; Shan, C.; Chang, L.; Xu, H. Quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in patients undergoing abdominal surgeries: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020, 20, 1–10. [Google Scholar]
- Qin, C.; Liu, Y.; Xiong, J.; Wang, X.; Dong, Q.; Su, T.; Liu, J. The analgesic efficacy compared ultrasound-guided continuous transverse abdominis plane block with epidural analgesia following abdominal surgery: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020, 20, 1–9. [Google Scholar]
- Yu, N.; Long, X.; Lujan-Hernandez, J.R.; Succar, J.; Xin, X.; Wang, X. Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: A systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2014, 14, 121. [Google Scholar] [CrossRef]
- Zhang, D.; Zhou, C.; Wei, D.; Ge, L.; Li, Q. Dexamethasone added to local anesthetics in ultrasound-guided transversus abdominis plain (TAP) block for analgesia after abdominal surgery: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2019, 14, 1–15. [Google Scholar] [CrossRef]
- Hain, E.; Maggiori, L.; à la Denise, P.; Panis, Y. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: A meta-analysis. Colorectal. Dis. 2018, 20, 279–287. [Google Scholar]
- Peltrini, R.; Cantoni, V.; Green, R.; Greco, P.A.; Calabria, M.; Bucci, L.; Corcione, F. Efficacy of transversus abdominis plane (TAP) block in colorectal surgery: A systematic review and meta-analysis. Tech. Coloproctol. 2020, 24, 787–802. [Google Scholar]
- Guo, Q.; Li, R.; Wang, L.; Zhang, D.; Ma, Y. Transversus abdominis plane block versus local anaesthetic wound infiltration for postoperative analgesia: A systematic review and meta-analysis. Int. J. Clin. Exp. Med. 2015, 8, 17343. [Google Scholar]
- Abdallah, F.W.; Halpern, S.H.; Margarido, C.B. Transversus abdominis plane block for postoperative analgesia after Caesarean delivery performed under spinal anaesthesia? A systematic review and meta-analysis. Br. J. Anaesth. 2012, 109, 679–687. [Google Scholar]
- Aamir, M.A.; Sahebally, S.M.; Heneghan, H. Transversus Abdominis Plane Block in Laparoscopic Bariatric Surgery—A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Obes. Surg. 2021, 31, 133–142. [Google Scholar]
- Chaw, S.H.; Lo, Y.L.; Goh, S.-L.; Cheong, C.C.; Tan, W.K.; Loh, P.S.; Wong, L.F.; Shariffuddin, I.I. Transversus Abdominis Plane Block Versus Intraperitoneal Local Anesthetics in Bariatric Surgery: A Systematic Review and Network Meta-analysis. Obes. Surg. 2021, 31, 4305–4315. [Google Scholar]
- Abdou, S.A.; Daar, D.A.; Wilson, S.C.; Thanik, V. Transversus Abdominis Plane Blocks in Microsurgical Breast Reconstruction: A Systematic Review and Meta-analysis. J. Reconstr. Microsurg. 2020, 36, 353–361. [Google Scholar]
- Hamid, H.K.; Emile, S.H.; Saber, A.A.; Ruiz-Tovar, J.; Minas, V.; Cataldo, T.E. Laparoscopic-Guided Transversus Abdominis Plane Block for Postoperative Pain Management in Minimally Invasive Surgery: Systematic Review and Meta-Analysis. J. Am. Coll. Surg. 2020, 231, 376–386.e315. [Google Scholar]
- Koo, C.-H.; Hwang, J.-Y.; Shin, H.-J.; Ryu, J.-H. The Effects of Erector Spinae Plane Block in Terms of Postoperative Analgesia in Patients Undergoing Laparoscopic Cholecystectomy: A Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2020, 9, 2928. [Google Scholar]
- Ni, X.; Zhao, X.; Li, M.; Li, Q.; Liu, Z. The effect of transversus abdominis plane block for pain after laparoscopic cholecystectomy: A meta-analysis of randomized controlled trials. Int. J. Clin. Exp. Med. 2016, 9, 9974–9982. [Google Scholar]
- Zhao, X.; Tong, Y.; Ren, H.; Ding, X.-B.; Wang, X.; Zong, J.-Y.; Jin, S.-Q.; Li, Q. Transversus abdominis plane block for postoperative analgesia after laparoscopic surgery: A systematic review and meta-analysis. Int. J. Clin. Exp. Med. 2014, 7, 2966–2975. [Google Scholar]
- Ma, N.; Duncan, J.K.; Scarfe, A.J.; Schuhmann, S.; Cameron, A.L. Clinical safety and effectiveness of transversus abdominis plane (TAP) block in post-operative analgesia: A systematic review and meta-analysis. J. Anesth. 2017, 31, 432–452. [Google Scholar]
- Ripollés, J.; Mezquita, S.M.; Abad, A.; Calvo, J. Analgesic efficacy of the ultrasound-guided blockade of the transversus abdominis plane–A systematic review. Braz. J. Anesthesiol. Engl. Ed. 2015, 65, 255–280. [Google Scholar]
- Wang, W.; Wang, L.; Gao, Y. A Meta-Analysis of Randomized Controlled Trials Concerning the Efficacy of Transversus Abdominis Plane Block for Pain Control After Laparoscopic Cholecystectomy. Front. Surg. 2021, 8, 700318. [Google Scholar]
- Wang, Y.; Wang, X.; Zhang, K. Effects of transversus abdominis plane block versus quadratus lumborum block on postoperative analgesia: A meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020, 20, 1–9. [Google Scholar]
- Keir, A.; Rhodes, L.; Kayal, A.; Khan, O.A. Does a transversus abdominis plane (TAP) local anaesthetic block improve pain control in patients undergoing laparoscopic cholecystectomy? A best evidence topic. Int. J. Surg. 2013, 11, 792–794. [Google Scholar]
- Parums, D.V. Editorial: Review Articles, Systematic Reviews, Meta-Analysis, and the Updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 Guidelines. Med. Sci. Monit. 2021, 27, e934475. [Google Scholar] [CrossRef]
- de Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar]
- Batchelor, F.; Hill, K.; Mackintosh, S.; Said, C. What works in falls prevention after stroke? A systematic review and meta-analysis. Stroke 2010, 41, 1715–1722. [Google Scholar]
- Macedo, L.G.; Elkins, M.R.; Maher, C.G.; Moseley, A.M.; Herbert, R.D.; Sherrington, C. There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J. Clin. Epidemiol. 2010, 63, 920–925. [Google Scholar]
- Silverman, S.R.; Schertz, L.A.; Yuen, H.K.; Lowman, J.D.; Bickel, C.S. Systematic review of the methodological quality and outcome measures utilized in exercise interventions for adults with spinal cord injury. Spinal Cord 2012, 50, 718–727. [Google Scholar]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Watt, J.A.; Veroniki, A.A.; Tricco, A.C.; Straus, S.E. Using a distribution-based approach and systematic review methods to derive minimum clinically important differences. BMC Med. Res. Methodol. 2021, 21, 1–7. [Google Scholar]
- Sullivan, G.M.; Feinn, R. Using effect size—Or why the P value is not enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar]
- El-Dawlatly, A.A.; Turkistani, A.; Kettner, S.C.; Machata, A.-M.; Delvi, M.B.; Thallaj, A.; Kapral, S.; Marhofer, P. Ultrasound-guided transversus abdominis plane block: Description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br. J. Anaesth. 2009, 102, 763–767. [Google Scholar]
- Tolchard, S.; Davies, R.; Martindale, S. Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: Comparison with conventional port-site infiltration. J. Anaesthesiol. Clin. Pharmacol. 2012, 28, 339. [Google Scholar]
- Shin, H.-J.; Oh, A.-Y.; Baik, J.-S.; Kim, J.-H.; Han, S.-H.; Hwang, J.-W. Ultrasound-guided oblique subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy: A randomized, controlled, observer-blinded study. Minerva Anestesiol. 2014, 80, 185–193. [Google Scholar]
- Basaran, B.; Basaran, A.; Kozanhan, B.; Kasdogan, E.; Eryilmaz, M.A.; Ozmen, S. Analgesia and respiratory function after laparoscopic cholecystectomy in patients receiving ultrasound-guided bilateral oblique subcostal transversus abdominis plane block: A randomized double-blind study. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2015, 21, 1304–1312. [Google Scholar]
- Elamin, G.; Waters, P.S.; Hamid, H.; O’Keeffe, H.M.; Waldron, R.M.; Duggan, M.; Khan, W.; Barry, M.K.; Khan, I.Z. Efficacy of a Laparoscopically Delivered Transversus Abdominis Plane Block Technique during Elective Laparoscopic Cholecystectomy: A Prospective, Double-Blind Randomized Trial. J. Am. Coll. Surg. 2015, 221, 335–344. [Google Scholar]
- Saliminia, A.; Azimaraghi, O.; Babayipour, S.; Ardavan, K.; Movafegh, A. Efficacy of transverse abdominis plane block in reduction of postoperation pain in laparoscopic cholecystectomy. Acta Anaesthesiol. Taiwanica 2015, 53, 119–122. [Google Scholar]
- Al-Refaey, K.; Usama, E.; Al-Hefnawey, E. Adding magnesium sulfate to bupivacaine in transversus abdominis plane block for laparoscopic cholecystectomy: A single blinded randomized controlled trial. Saudi J. Anaesth. 2016, 10, 187. [Google Scholar]
- Bava, E.P.; Ramachandran, R.; Rewari, V.; Chandralekha; Bansal, V.K.; Trikha, A. Analgesic efficacy of ultrasound guided transversus abdominis plane block versus local anesthetic infiltration in adult patients undergoing single incision laparoscopic cholecystectomy: A randomized controlled trial. Anesth. Essays Res. 2016, 10, 561. [Google Scholar]
- Huang, S.-H.; Lu, J.; Gan, H.-Y.; Li, Y.; Peng, Y.-G.; Wang, S.-K. Perineural dexamethasone does not enhance the analgesic efficacy of ultrasound-guided subcostal transversus abdominis plane block during laparoscopic cholecystectomy. Hepatobiliary Pancreat. Dis. Int. 2016, 15, 540–545. [Google Scholar]
- Oksar, M.; Koyuncu, O.; Turhanoglu, S.; Temiz, M.; Oran, M.C. Transversus abdominis plane block as a component of multimodal analgesia for laparoscopic cholecystectomy. J. Clin. Anesth. 2016, 34, 72–78. [Google Scholar]
- Sinha, S.; Palta, S.; Saroa, R.; Prasad, A. Comparison of ultrasound-guided transversus abdominis plane block with bupivacaine and ropivacaine as adjuncts for postoperative analgesia in laparoscopic cholecystectomies. Indian J. Anaesth. 2016, 60, 264. [Google Scholar]
- Breazu, C.M.; Ciobanu, L.; Bartos, A.; Bodea, R.; Mircea, P.A.; Ionescu, D. Pethidine efficacy in achieving the ultrasound-guided oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: A prospective study. Bosn. J. Basic Med. Sci. 2017, 17, 67. [Google Scholar]
- Choi, Y.-M.; Byeon, G.-J.; Park, S.-J.; Ok, Y.-M.; Shin, S.-W.; Yang, K. Postoperative analgesic efficacy of single-shot and continuous transversus abdominis plane block after laparoscopic cholecystectomy: A randomized controlled clinical trial. J. Clin. Anesthesia 2017, 39, 146–151. [Google Scholar]
- Şahin, A.S.; Ay, N.; Şahbaz, N.A.; Akay, M.K.; Demiraran, Y.; Derbent, A. Analgesic effects of ultrasound-guided transverse abdominis plane block using different volumes and concentrations of local analgesics after laparoscopic cholecystectomy. J. Int. Med. Res. 2017, 45, 211–219. [Google Scholar]
- Baral, B.; Poudel, P.R. Comparison of Analgesic Efficacy of Ultrasound Guided Subcostal Transversus Abdominis Plane Block with Port Site Infiltration Following Laparoscopic Cholecystectomy. J. Nepal Health Res. Counc. 2018, 16, 457–461. [Google Scholar]
- Bhalekar, P.; Gosavi, R.; Mutha, S.; Mahajan, V.; Phalgune, D. Efficacy of ultrasound-guided subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy. Indian Anaesth. Forum. 2018, 19, 73. [Google Scholar]
- Sarvesh, B.; Shivaramu, B.T.; Sharma, K.; Agarwal, A. Addition of dexmedetomidine to ropivacaine in subcostal transversus abdominis plane block potentiates postoperative analgesia among laparoscopic cholecystectomy patients: A prospective randomized controlled trial. Anesth. Essays Res. 2018, 12, 809–813. [Google Scholar]
- Suseela, I.; Anandan, K.; Aravind, A.; Kaniyil, S. Comparison of ultrasound-guided bilateral subcostal transversus abdominis plane block and port-site infiltration with bupivacaine in laparoscopic cholecystectomy. Indian J. Anaesth. 2018, 62, 497. [Google Scholar]
- Altıparmak, B.; Toker, M.K.; Uysal, A.I.; Kuşçu, Y.; Demirbilek, S.G. Ultrasound-guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: Randomized, controlled trial. J. Clin. Anesthesia 2019, 57, 31–36. [Google Scholar]
- Baytar, Ç.; Yılmaz, C.; Karasu, D.; Topal, S. Comparison of Ultrasound-Guided Subcostal Transversus Abdominis Plane Block and Quadratus Lumborum Block in Laparoscopic Cholecystectomy: A Prospective, Randomized, Controlled Clinical Study. Pain Res. Manag. 2019, 2019, 1–6. [Google Scholar]
- Houben, A.M.; Moreau, A.-S.J.; Detry, O.M.; Kaba, A.; Joris, J.L. Bilateral subcostal transversus abdominis plane block does not improve the postoperative analgesia provided by multimodal analgesia after laparoscopic cholecystectomy: A randomised placebo-controlled trial. Eur. J. Anaesthesiol. 2019, 36, 772–777. [Google Scholar]
- Janjua, S.; Aslam, K.Z.; Sarfraz, S.; Qarni, A.; Niazi, W.; Sarfraz, M.B. Comparison of modified unilateral ultrasound guided subcostal transversus abdominis plane block with conventional port-site and intraperitoneal infiltration of bupivacaine for postoperative pain relief in laparoscopic cholecystectomy. PAFMJ 2019, 69, 800–807. [Google Scholar]
- Karnik, P.P.; Dave, N.M.; Shah, H.B.; Kulkarni, K. Comparison of ultrasound-guided transversus abdominis plane (TAP) block versus local infiltration during paediatric laparoscopic surgeries. Indian J. Anaesth. 2019, 63, 356–360. [Google Scholar]
- Khandelwal, H.; Parag, K.; Singh, A.; Anand, N.; Govil, N. Comparison of subcostal transversus abdominis block with intraperitoneal instillation of levobupivacaine for pain relief after laparoscopic cholecystectomy: A prospective study. Anesth. Essays Res. 2019, 13, 144. [Google Scholar]
- Ribeiro, K.N.S.; Misquith, J.C.; Eapen, A.; A Naik, S. Ultrasound Guided Oblique Subcostal Transverse Abdominis Plane Block using Local Anaesthetic Versus Saline for Laparoscopic Cholecystectomies: A Randomised Controlled Trial. J. Clin. Diagn. Res. 2019, 13, 7–10. [Google Scholar]
- Siriwardana, R.C.; Kumarage, S.K.; Gunathilake, B.M.; Thilakarathne, S.B.; Wijesinghe, J.S. Local infiltration versus laparoscopic-guided transverse abdominis plane block in laparoscopic cholecystectomy: Double-blinded randomized control trial. Surg. Endosc. 2019, 33, 179–183. [Google Scholar]
- Wu, L.; Wu, L.; Sun, H.; Dong, C.; Yu, J. Effect of Ultrasound-Guided Peripheral Nerve Blocks of the Abdominal Wall on Pain Relief After Laparoscopic Cholecystectomy [Corrigendum]. J. Pain Res. 2019, 13, 2169–2170. [Google Scholar]
- Arık, E.; Akkaya, T.; Ozciftci, S.; Alptekin, A.; Balas, Ş. Unilateral transversus abdominis plane block and port-site infiltration. Der Anaesthesist 2020, 69, 270–276. [Google Scholar]
- Kharbuja, K.; Singh, J.; Ranjit, S.; Pradhan, B.B.; Shrestha, A.; Tandukar, A.; Shalike, N. Efficacy of The Subcostal Transversus Abdominis Plane Block in Laparoscopic Cholecystectomy: A Comparison with Conventional Port- Site Infiltration. J. KIST Med. Coll. 2020, 2, 42–47. [Google Scholar]
- Liang, M.; Chen, Y.; Zhu, W.; Zhou, D. Efficacy and safety of different doses of ropivacaine for laparoscopy-assisted infiltration analgesia in patients undergoing laparoscopic cholecystectomy: A prospective randomized control trial. Medicine 2020, 99, e22540. [Google Scholar]
- Abdelfatah, F.A.; Amin, S.R. Does esmolol infusion have an adjuvant effect on transversus abdominis plane block for pain control in laparoscopic cholecystectomy? A randomized controlled double-blind trial. Egypt. J. Anaesth. 2021, 37, 418–424. [Google Scholar]
- Ergin, A.; Aydin, M.T.; Çiyiltepe, H.; Karip, A.B.; Fersahoğlu, M.M.; Özcabi, Y.; Ar, A.Y. Effectiveness of local anesthetic application methods in postoperative pain control in laparoscopic cholecystectomies: A randomised controlled trial. Int. J. Surg. 2021, 95, 106134. [Google Scholar]
- Jung, J.; Jung, W.; Ko, E.Y.; Chung, Y.-H.; Koo, B.-S.; Chung, J.C.; Kim, S.-H. Impact of Bilateral Subcostal Plus Lateral Transversus Abdominis Plane Block on Quality of Recovery After Laparoscopic Cholecystectomy: A Randomized Placebo-Controlled Trial. Anesthesia Analg. 2021, 133, 1624–1632. [Google Scholar]
- Sahu, L.; Behera, S.K.; Satapathy, G.C.; Saxena, S.; Priyadarshini, S.; Sahoo, R.K. Comparison of Analgesic Efficacy of Erector Spinae and Oblique Subcostal Transverse Abdominis Plane Block in Laparoscopic Cholecystectomy. J. Clin. Diagn. Res. 2021, 15, UC09–UC13. [Google Scholar]
- Saravanan, R.; Venkatraman, R.; Karthika, U. Comparison of Ultrasound-Guided Modified BRILMA Block with Subcostal Transversus Abdominis Plane Block for Postoperative Analgesia in Laparoscopic Cholecystectomy—A Randomized Controlled Trial. Local Reg. Anesth. 2021, 14, 109. [Google Scholar]
- Vindal, A.; Sarda, H.; Lal, P. Laparoscopically guided transversus abdominis plane block offers better pain relief after laparoscopic cholecystectomy: Results of a triple blind randomized controlled trial. Surg. Endosc. 2021, 35, 1713–1721. [Google Scholar]
- Priyanka, B.G.; Krishnamurthy, P.K.D.; Rohit, S. Comparative Study of Pre-Operative Ultrasound Guided Transversus Abdominis Plane Block Versus Post-Operative Ultrasound Guided Transversus Abdominis Plane Block on Perioperative Hemodynamic Status and Post Operative Analgesic Requirement in Patients Undergoing Laparoscopic Abdominal Surgeries. Eur. J. Mol. Clin. Med. 2022, 9, 2781–2789. Available online: https://ejmcm.com/article_17726.html (accessed on 17 August 2022).
- Emile, S.H.; Elfeki, H.; Elbahrawy, K.; Sakr, A.; Shalaby, M. Ultrasound-guided versus laparoscopic-guided subcostal transversus abdominis plane (TAP) block versus No TAP block in laparoscopic cholecystectomy: A randomized double-blind controlled trial. Int. J. Surg. 2022, 101, 106639. [Google Scholar]
- Fargaly, O.S.; Boules, M.L.; Hamed, M.A.; Abbas, M.A.A.; Shawky, M.A. Lateral Quadratus Lumborum Block versus Transversus Abdominis Plane Block in Laparoscopic Surgery: A Randomized Controlled Study. Anesthesiol. Res. Pract. 2022, 2022, 1–6. [Google Scholar]
- Han, K.; Zhang, Y.; Bai, R.; An, R.; Zhang, S.; Xue, M.; Shen, X. Application of Ultrasound-Guided Transversus Abdominis Plane Block Combined with Nalbuphine Patient-Controlled Intravenous Analgesia in Postoperative Analgesia After Laparotomy: A Randomized Controlled Trial. Pain Ther. 2022, 11, 627–641. [Google Scholar]
- Lee, S.Y.; Ryu, C.G.; Koo, Y.H.; Cho, H.; Jung, H.; Park, Y.H.; Kang, H.; Lee, S.E.; Shin, H.Y. The effect of ultrasound-guided transversus abdominis plane block on pulmonary function in patients undergoing laparoscopic cholecystectomy: A prospective randomized study. Surg. Endosc. 2022, 18, 1–9. [Google Scholar]
- Ozciftci, S.; Sahiner, Y.; Sahiner, I.T.; Akkaya, T. Is Right Unilateral Transversus Abdominis Plane (TAP) Block Successful in Postoperative Analgesia in Laparoscopic Cholecystectomy? Int. J. Clin. Pract. 2022, 2022, 2668215. [Google Scholar]
- Paudel, B.; Paudel, S.; Rai, P.; Dahal, S.; Pokhrel, A. Comparison of Ultrasound Guided Bilateral Subcostal Transversus Abdominis Plane Block versus Local Infiltration of Port Site with Bupivacaine in Patients Undergoing Laparoscopic Cholecystectomy under General Anesthesia. Birat J. Health Sci. 2021, 6, 1642–1646. [Google Scholar]
- Rahimzadeh, P.; Faiz, S.H.R.; Latifi-Naibin, K.; Alimian, M. A Comparison of effect of preemptive versus postoperative use of ultrasound-guided bilateral transversus abdominis plane (TAP) block on pain relief after laparoscopic cholecystectomy. Sci. Rep. 2022, 12, 1–7. [Google Scholar]
- Mukherjee, A.; Pal, A.; Agrawal, J.; Mehrotra, A.; Dawar, N. Intrathecal nalbuphine as an adjuvant to subarachnoid block: What is the most effective dose? Anesth. Essays Res. 2011, 5, 171. [Google Scholar]
- Kalu, R.; Boateng, P.; Carrier, L.; Garzon, J.; Tang, A.; Reickert, C.; Stefanou, A. Effect of preoperative versus postoperative use of transversus abdominis plane block with plain 0.25% bupivacaine on postoperative opioid use: A retrospective study. BMC Anesthesiol. 2021, 21, 1–6. [Google Scholar]
- Marret, E.; Gentili, M.; Bonnet, M.P.; Bonnet, F. Intra-articular ropivacaine 0.75% and bupivacaine 0.50% for analgesia after arthroscopic knee surgery: A randomized prospective study. Arthrosc. J. Arthrosc. Relat. Surg. 2005, 21, 313–316. [Google Scholar]
- Sinardi, D.; Marino, A.; Chillemi, S.; Siliotti, R.; Mondello, E. Sciatic nerve block with lateral popliteal approach for hallux vagus correction. Comparison between 0.5% bupivacaine and 0.75% ropivacaine. Minerva Anestesiol. 2004, 70, 625–629. [Google Scholar]
- Martín, M.F.; Álvarez, S.L.; Herrero, M.P. Bloqueo interfascial serrato-intercostal como estrategia ahorradora de opioides en cirugía supraumbilical abierta. Revista Española de Anestesiología y Reanimación 2018, 65, 456–460. [Google Scholar]
- Esmaoglu, A.; Yegenoglu, F.; Akin, A.; Turk, C.Y. Dexmedetomidine Added to Levobupivacaine Prolongs Axillary Brachial Plexus Block. Anesth. Analg. 2010, 111, 1548–1551. [Google Scholar]
- Lahiri, S.; Das, S.; Basu, S.R. Effect of intraoperative esmolol infusion on postoperative analgesia in laparoscopic cholecystectomy patients: A randomised controlled trial. J. Evol. Med. Dent. Sci. 2015, 4, 14143–14152. [Google Scholar]
- Akkaya, A.; Yıldız, İ.; Tekelioğlu, Ü.Y.; Demirhan, A.; Bayır, H.; Özlü, T.; Bilgi, M. Dexamethasone added to levobupivacaine in ultrasound-guided tranversus abdominis plain block increased the duration of postoperative analgesia after caesarean section: A randomized, double blind, controlled trial. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 717–722. [Google Scholar]
- Kitayama, M.; Wada, M.; Hashimoto, H.; Kudo, T.; Takada, N.; Hirota, K. Effects of adding epinephrine on the early systemic absorption kinetics of local anesthetics in abdominal truncal blocks. J. Anesth. 2014, 28, 631–634. [Google Scholar]
- Bacal, V.; Rana, U.; McIsaac, D.I.; Chen, I. Transversus Abdominis Plane Block for Post Hysterectomy Pain: A Systematic Review and Meta-Analysis. J. Minim. Invasive Gynecol. 2019, 26, 40–52. [Google Scholar]
- Abd-Elsalam, K.A.; Fares, K.M.; Mohamed, M.A.; Mohamed, M.F.; El-Rahman, A.M.A.; Tohamy, M.M. Efficacy of Magnesium Sulfate Added to Local Anesthetic in a Transversus Abdominis Plane Block for Analgesia Following Total Abdominal Hysterectomy: A Randomized Trial. Pain Physician. 2017, 20, 641. [Google Scholar]
- McDonnell, J.G.; Curley, G.; Carney, J.; Benton, A.; Costello, J.; Maharaj, C.H.; Laffey, J.G. The Analgesic Efficacy of Transversus Abdominis Plane Block After Cesarean Delivery: A Randomized Controlled Trial. Anesth. Analg. 2008, 106, 186–191. [Google Scholar] [CrossRef]
- O’Donnell, B.D. The transversus abdominis plane (TAP) block in open retropubic prostatectomy. Reg. Anesth. Pain Med. 2006, 31, 91. [Google Scholar]
- Hebbard, P.; Fujiwara, Y.; Shibata, Y.; Royse, C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth. Intensiv. Care 2007, 35, 616–618. [Google Scholar]
- Niraj, G.; Searle, A.; Mathews, M.; Misra, V.; Baban, M.; Kiani, S.; Wong, M. Analgesic efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing open appendicectomy. Br. J. Anaesth. 2009, 103, 601–605. [Google Scholar]
- Dean, C.; Douglas, J. Magnesium and the obstetric anaesthetist. Int. J. Obstet. Anesth. 2013, 22, 52–63. [Google Scholar]
- Gutiérrez-Román, C.I.; Carrillo-Torres, O.; Pérez-Meléndez, E.S. Uses of magnesium sulfate in anesthesiology. Revista Médicadel Hospital General de México 2022, 85, 25–33. [Google Scholar]
- Herroeder, S.; Schoenherr, M.E.; De Hert, S.G.; Hollmann, M.W.; Warner, D.S. Magnesium—Essentials for anesthesiologists. J. Am. Soc. Anesthesiol. 2011, 114, 971–993. [Google Scholar]
- Goyal, P.; Jaiswal, R.; Hooda, S.; Goyal, R.; Lal, J. Role of magnesium sulphate for brachial plexus analgesia. Int. J. Anesth. 2008, 21, 1. [Google Scholar]
- Barbosa, F.T.; Barbosa, L.T.; Jucá, M.J.; da Cunha, R.M. Applications of Magnesium Sulfate in Obstetrics and Anesthesia. Braz. J. Anesthesiol. 2010, 60, 104–110. [Google Scholar]
- Bottiger, B.A.; Esper, S.A.; Stafford-Smith, M. Pain Management Strategies for Thoracotomy and Thoracic Pain Syndromes. In Seminars in Cardiothoracic and Vascular Anesthesia; SAGE Publications: Los Angeles, CA, USA, 2014; Volume 18, pp. 45–56. [Google Scholar]
- Buvanendran, A.; Kroin, J.S. Useful adjuvants for postoperative pain management. Best Pract. Res. Clin. Anaesthesiol. 2007, 21, 31–49. [Google Scholar]
- Dabbagh, A.; Elyasi, H.; Razavi, S.S.; Fathi, M.; Rajaei, S. Intravenous magnesium sulfate for post-operative pain in patients undergoing lower limb orthopedic surgery. Acta Anaesthesiol. Scand. 2009, 53, 1088–1091. [Google Scholar]
- Murphy, G.S.; Szokol, J.W.; Greenberg, S.B.; Avram, M.J.; Vender, J.S.; Nisman, M.; Vaughn, J. Preoperative dexamethasone enhances quality of recovery after laparoscopic cholecystectomy: Effect on in-hospital and postdischarge recovery outcomes. J. Am. Soc. Anesthesiol. 2011, 114, 882–890. [Google Scholar]
- Milan, Z.; Tabor, D.; McConnell, P.; Pickering, J.; Kocarev, M.; du Feu, F.; Barton, S. Three different approaches to transversus abdominis plane block: A cadaveric study. Med. Glas. 2011, 8, 181–184. [Google Scholar]
- Drager, C.; Benziger, D.; Gao, F.; Berde, C.B. Prolonged Intercostal Nerve Blockade in Sheep Using Controlled-release of Bupivacaine and Dexamethasone from Polymer Microspheres. Anesthesiology 1998, 89, 969–974. [Google Scholar]
- Castillo, J.; Curley, J.; Hotz, J.; Uezono, M.; Tigner, J.; Chasin, M.; Wilder, R.; Langer, R.; Berde, C. Glucocorticoids Prolong Rat Sciatic Nerve Blockade In Vivo from Bupivacaine Microspheres. Anesthesiology 1996, 85, 1157–1166. [Google Scholar]
- Sinnott, C.J.; Cogswell, L.P.; Johnson, A.; Strichartz, G.R. On the mechanism by which epinephrine potentiates lidocaine’s peripheral nerve block. J. Am. Soc. Anesthesiol. 2003, 98, 181–188. [Google Scholar]
- Eisenach, J.C.; Grice, S.C.; Dewan, D.M. Epinephrine Enhances Analgesia Produced by Epidural Bupivacaine during Labor. Anesth. Analg. 1987, 66, 447–451. [Google Scholar]
- Chatrath, V.; Khetarpal, R.; Kumari, H.; Kaur, H.; Sharma, A. Intermittent transcutaneous electrical nerve stimulation versus transversus abdominis plane block for postoperative analgesia after infraumbilical surgeries. Anesth. Essays Res. 2018, 12, 349. [Google Scholar]
- Chou, R.; Gordon, D.B.; de Leon-Casasola, O.A.; Rosenberg, J.M.; Bickler, S.; Brennan, T.; Carter, T.; Cassidy, C.L.; Chittenden, E.H.; Degenhardt, E.; et al. Management of Postoperative Pain: A Clinical Practice Guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J. Pain 2016, 17, 131–157. [Google Scholar]
- Hebbard, P.D.; Barrington, M.J.; Vasey, C. Ultrasound-guided continuous oblique subcostal transversus abdominis plane blockade: Description of anatomy and clinical technique. Reg. Anesth. Pain Med. 2010, 35, 436–441. [Google Scholar]
| Author | Year | Eligibility | Randomized Allocation | Concealed Allocation | Similarity at Baseline | Blinding of Participants | Blinding of Therapist | Blinding of Assessor | Dropout | Intention to Treat | Group Comparison | PMVD | Total Score (10) | Internal Validity (8) | Sub Scale (2) | Interpretation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| El-Dawlatly [59] | 2009 | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Ra [7] | 2010 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Ortiz [20] | 2012 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Petersen [21] | 2012 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | 9 | 7 | 2 | Good |
| Tolchard [60] | 2012 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 9 | 7 | 2 | Good |
| Bhatia [6] | 2014 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Shin [61] | 2014 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes | 7 | 5 | 2 | Good |
| Basaran [62] | 2015 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Elamin [63] | 2015 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Saliminia [64] | 2015 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 9 | 7 | 2 | Good |
| Al-refaey [65] | 2016 | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | 7 | 5 | 2 | Good |
| Bava [66] | 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | 9 | 7 | 2 | Good |
| Huang [67] | 2016 | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Oksar [68] | 2016 | Yes | Yes | No | Yes | No | Yes | No | Yes | No | Yes | Yes | 6 | 4 | 2 | Good |
| Sinha [69] | 2016 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Breazu [70] | 2017 | Yes | Yes | No | Yes | No | No | Yes | Yes | No | Yes | Yes | 6 | 4 | 2 | Good |
| Choi [71] | 2017 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Sahin [72] | 2017 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Baral [73] | 2018 | Yes | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | 6 | 4 | 2 | Good |
| Bhalekar [74] | 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 9 | 7 | 2 | Good |
| Sarvesh [75] | 2018 | Yes | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 | 3 | 2 | Moderate |
| Suseela [76] | 2018 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Altiparmak [77] | 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Baytar [78] | 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Houben [79] | 2019 | Yes | Yes | No | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 7 | 5 | 2 | Good |
| Janjua [80] | 2019 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Karnik [81] | 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 9 | 7 | 2 | Good |
| Khandelwal [82] | 2019 | Yes | Yes | No | Yes | No | No | Yes | Yes | No | Yes | Yes | 6 | 4 | 2 | Good |
| Ribeiro [83] | 2019 | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Siriwardana [84] | 2019 | Yes | Yes | No | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 7 | 5 | 2 | Good |
| Wu [85] | 2019 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Arik [86] | 2020 | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 7 | 5 | 2 | Good |
| Kharbuja [87] | 2020 | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Liang [88] | 2020 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Abdelfatah [89] | 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 9 | 7 | 2 | Good |
| Ergin [90] | 2021 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | 9 | 7 | 2 | Good |
| Jung [91] | 2021 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 10 | 8 | 2 | Excellent |
| Sahu [92] | 2021 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Saravanan [93] | 2021 | Yes | Yes | Yes | Yes | No | Yes | No | Yes | No | Yes | Yes | 7 | 5 | 2 | Good |
| Vindal [94] | 2021 | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | 8 | 6 | 2 | Good |
| Priyanka [95] | 2022 | Yes | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 4 | 2 | 2 | Moderate |
| Emile [96] | 2022 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | 8 | 6 | 2 | Good |
| Fargaly [97] | 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | 9 | 7 | 2 | Good |
| Han [98] | 2022 | Yes | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | 6 | 4 | 2 | Good |
| Lee [99] | 2022 | Yes | Yes | No | Yes | No | No | No | Yes | No | Yes | Yes | 5 | 3 | 2 | Moderate |
| Ozciftci [100] | 2022 | Yes | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | 6 | 4 | 2 | Good |
| Paudel [101] | 2022 | Yes | Yes | No | Yes | No | No | Yes | Yes | No | Yes | Yes | 6 | 4 | 2 | Good |
| Rahimzadeh [102] | 2022 | Yes | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | 7 | 5 | 2 | Good |
| No | Author (Year) | Sample Size | Gender, Age (Mean Age and/or Range, Ratio) | Pre-Medication | TAP Block Technique | Anesthetics Used for Surgical Infiltrations | Analgesia Used (Intra-Operative and Postoperative) | Use of PCA or PCIA | Outcomes | Outcome Measures |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | El-Dawlatly (2009) [59] | 42 | Gender (male n = 7, 16.7%; female = 35, 83.3%); Age TAP = 22–77 years; Control 34–65 years. | Lorazepam 2 mg, Ringers lactate 500 mL |
|
| Intra-operative: Sufentanil 0.1 mcg/kg Postoperative: Morphine 1.5 mg bolus, and total Morphine consumed in 24 h via PCIA were recorded. | Yes | Pain | NA |
| 2 | Ra (2010) [7] | 54 | Gender (male n = 28, 51.9%; female n = 26, 48.1%); Age: Control = 43.4 ± 12.4; US-TAP Block 0.25 = 48.2 ± 10.7; and US-TAP Block 0.5 = 45.0 ± 11.1. | None |
|
| Intra-operative: Remifentanil Postoperative: Ketorolac 30 mg tds by 24 h, and Fentanyl 20 mcg for those with un-relived pain. | Yes | Pain | VNRS |
| 3 | Ortiz (2012) [20] | 74 | Gender (male n = 14, 18.9%; female n = 60, 81.0%); Age: US-STA Block = 37 (11); Control = 36 (11). | Midazolam 1–2 mg |
|
| Intra-operative: Fentanyl 2 mcg/kg, additional 50 mcg bolus were added, and Morphine was given as needed at the end of the procedure. Postoperative: Ketorolac 30 mg. | No | Pain | NAS |
| 4 | Petersen (2012) [21] | 74 | Gender (male n = 53, 71.6%; female n = 21, 28.4%); Age: US-Posterior TAP (Ropivacaine) = 42 (13.5); US-Posterior TAP (saline) = 43 (17.0). | None |
|
| Preoperative: Remifentanil 0.4 mL/kg/h Postoperative: Acetaminophen 1000 mg by 4, Ibuprofen 400 mg by 3, Ketobemidone 2–24 h, and IV Morphine 0–2 h. | No | Pain | VAS |
| 5 | Tolchard (2012) [60] | 43 | Gender (male/female 2:0/5:16) Age: Intervention = 52 ± 3; Control = 48 ± 3. | Paracetamol 15–20 mg/kg; Diclofenac 0.5 mg/kg, Fentanyl 20 mcg |
| Standardized dose of 1 mg/kg Bupivacaine | Intra-operative: Fentanyl 3 mcg/kg, Diclofenac 0.5 mg/kg, and Paracetamol 15–20 mg/kg. Postoperative: Fentanyl 20 mcg bolus. | No | Pain | VPAS |
| 6 | Bhatia (2014) [6] | 64 | Gender = NA; Age: Control = 35.4 ± 7.16; TAP Posterior = 36.4 ± 10.4; TAP Subcostal = 36.4 ± 10.4. | Alprazolam 0.25 mg, Ranitidine 150 mg |
|
| Intra-operative: Morphine 0.1 mg/kg Postoperative: Paracetamol 1000 mg every 6 h; IV Tramadol 2 mg/kg were given as an initial dose for those with VAS scores >4, with a subsequent dose of 1 mg/kg. | NA | Pain | VAS |
| 7 | Shin (2014) [61] | 45 | Gender (male n = 25, 53.2%; female n = 22, 46.8%); Age: Control = 44.7 ± 11.1; US-TAP group = 43.9 ± 9.5; and OSTAP group = 43.0 ± 9.6. | NA |
|
| Intra-operative: Fentanyl 1 mcg/kg, Ketorolac 30 mg/kg (pre-emptive analgesia). Postoperative: Fentanyl 25 mcg for pain score >6, Ketorolac 30 mg for pain score 4–6, and Nalbuphine 10 mg for those needing analgesia at ward. | NA | Pain | VNRS |
| 8 | Basaran (2015) [62] | 76 | Gender (male n = 11, 14.5%; female n = 65, 85.5%); age: Control = 44.89 ± 14.2; Intervention = 43.2 ± 12.2. | Diazepam 10 mg |
|
| Intra-operative: Fentanyl 2 mcg/kg, 1 mcg/kg given (bolus) if heart rate or mean arterial pressure increased by 20% of initial values, Remifentanil 0.1 mcg/kg (maintenance), and 0.5 mg/kg Meperidine prior to the cessation of Remifentanil. Ephedrine 5 mg was given to reduce mean arterial pressure with an additional dose permitted after 2 min. IV Tenoxicam 20 mg after induction. Postoperative: Tramadol 50 mg IV on request with minimum of 20 min between doses, and a maximum dose was capped at 500 mg at 24 h. | NA | Pain | VAS |
| 9 | Elamin (2015) [63] | 80 | Gender (male n = 10, 12.5%, female 70, 87.5%); Age = 49.5 years versus 52.1 years. | None |
|
| Intra-operative: NA Postoperative: Paracetamol 1 g q6h, Diclofenac sodium 75 mg. | Yes | Pain | NRS |
| 10 | Saliminia (2015) [64] | 54 | Gender (male n = 24, 24.4%; female n = 30, 54.6%); Age = 28–61 years. | None |
|
| Intra-operative: Fentanyl 3 mcg/kg, with 1 mcg/kg as maintenance dose. Postoperative: 50 mL of Fentanyl bolus with a lockout time of 8 min. | Yes | Pain | VAS |
| 11 | Al-refaey (2016) [65] | 90 | Gender (NA); Years = Control = 32 ± 6; US-TAP Block B= 37 ± 8; US-TAP Block M = 34 ± 8. | None |
|
| Intra-operative: Fentanyl 1 mcg/kg Postoperative: Morphine 0.02 mg/kg bolus | No | Pain | VAS |
| 12 | Bava (2016) [66] | 42 | Gender (male n = 3, 7.1%; female n = 39, 92.3%); Age: TAP group = 33.7 ± 10.5, Control = 33.5 ± 6.5. | None |
|
| Intra-operative: Fentanyl 2 mcg/kg and 0.5 mcg was used as supplemental. Postoperative: Morphine 0.5 mg/kg with a maximum dose of 20 mg in 4 h. | Yes | Pain | VAS |
| 13 | Huang (2016) [67] | 60 | Gender: NA Age: Control 1: 38.5 ± 7.7; Group II: 39.7 ± 5.5; Group III: 38.6 ± 8.9. | None |
|
| Intra-operative: Remifentanil until its plasma concentration reaches 2.5 mcg/mL. Postoperative: Sufentanil 5–10 mcg. | No | Pain | NRS |
| 14 | Oksar (2016) [68] | 60 | Gender (male = 17, 28.3%; female 43, 71.7%); Age: 18–74. | Midazolam 2 mg IV, Ringers’ lactate solution 500 mL |
|
| Intra-operative: Remifentanil Postoperative: Paracetamol 1 g, and Diclofenac 75 mg. Pain relief using PCA was by 200 mg Tramadol (7 mL, 2 mg/kg bolus) with a 15 min lockout time. | Yes | Pain | VAS |
| 15 | Sinha (2016) [69] | 60 | Gender: (NA); Age: >40 years. | Oral Ranitidine 150 mg and alprazolam 0.25 mg |
|
| Intra-operative: Fentanyl 2 mcg/kg. Postoperative: Diclofenac sodium 75 mg. | No | Pain | VAS |
| 16 | Breazu (2017) [70] | 74 | Gender (male 29, 39.2%; female 45, 60.8%); Age: 42–65 years OSTAP-placebo; 38–67 years OSTAP-Bupivacaine; 40–65 OSTAP-Pethidine. | 7.5 mg Midazolam |
|
| Intra-operative: Fentanyl 2 mcg/kg Postoperative: Pethidine 25–50 mg. at the ward level, Acetaminophen 1 g 8-hourly; however, those with moderate to severe pain continue to receive 25–50 mg of Pethidine until the VAS score is lower than 3. | Yes | Pain | VAS |
| 17 | Choi (2017) [71] | 103 | Gender: (male n = 48, 46.6%; female n = 55, 53.4%); Age: IV-PCA + GA (Control): 50.4 ± 15.9; US-TAP block: 49.1 ± 14.2; TAP block: 52.2 ± 11.8. | Midazolam 0.05 mg/kg, Glycopyrrolate 0.003 mg/kg |
|
| Intra-operative: Remifentanil 1 mcg/kg and 0.5–1 mcg was used for maintenance. Postoperative: Morphine 3–5 mg was given for unrelieved pain. | Yes | Pain | NRS |
| 18 | Sahin (2017) [72] | 60 | Gender: (male n = 33, 55%; female n = 27, 45%); Age: Group 1: 47.2 ± 13.0; Group 2: 64.5 ± 11.5. | No |
|
| Intra-operative: Fentanyl 2 mcg/kg. Postoperative: Diclofenac 25 mg when the VAS is < 7. | No | Pain | VAS |
| 19 | Baral (2018) [73] | 60 | Gender: (male n = 19, 31.7%; female n = 41, 68.3%); Age Subcostal TAP block 42.47 ± 14.41; Control: 45.93 ± 14.34. | No |
|
| Intra-operative: Fentanyl 2 mcg/kg. Postoperative: Pethidine 0.5 mg/kg if the VAS score is less than equal to 4. | No | Yes | VAS |
| 20 | Bhalekar (2018) [74] | 50 | Gender: US-TAP (saline): (male = 11(44); female = 14(56.00); US-TAP block: male 14(56.00); female 11(44.00). Age: Subcostal TAP block = 44.1 ± 13.1; Control: 44.1 ± 13.3. | 0.2 mg glycopyrrolate, Ranitidine 50 mg and Ondansetron 4 mg. |
|
| Intra-operative: Fentanyl 2 mcg/kg; Diclofenac 75 mg administered after induction. Postoperative: Nalbuphine 10 mg/70 kg with a further dose of 5 mg/kg when required. | No | Pain | VAS |
| 21 | Sarvesh (2018) [75] | 60 | Gender: (NA); Age > 50 years. | Midazolam 0.03 mg/kg, |
|
| Intra-operative: Fentanyl 2 mcg/kg Postoperative: Morphine 1 mg loading dose with a lockout time of 10 min, and 0.25 mg/kg 4 h limit. | Yes | Pain | NRS |
| 22 | Suseela (2018) [76] | 80 | Gender: (NA); Age: US-TAP Block = 42.25 ± 11.91; Control (Port site infiltration) = 41.00 ± 11.34. | Metoclopramide 10 mg and Ranitidine 150 mg and midazolam 0.5 mg. |
|
| Intra-operative: Fentanyl 2 mcg/kg and Paracetamol 1 g. Postoperative: Paracetamol 1 g 8-hourly, Tramadol 1 mg/kg bolus, Diclofenac 1 mg/kg. | No | Pain | NRS |
| 23 | Altiparmak (2019) [77] | 68 | Gender: (male 25, 36.8%; female n = 43, 63.2%); Age: US-OSTAP Block = 53.1 ± 14.7; US-ESP Block = 51.1 ± 12.3. | No |
|
| Intra-operative: Fentanyl 1 mcg/kg Postoperative: Trometamol 50 mg, Tramadol 10 mg bolus with 20 min lockout time. | Yes | Pain | NRS |
| 24 | Baytar (2019) [78] | 107 | Gender: (male n = 26, 24.3%; female n = 81, 75.7%); Age QL Block: 46.42 ±16.57; US-TAP Block: 48.12 ± 12.42. | Midazolam 0.01–0.02 mg/kg |
|
| Intra-operative: Fentanyl 1–2 mcg Postoperative: Tenoxicam 20 mg, 54 mL normal saline + Tramadol 300 mg (6 mL). | Yes | Pain | VAS |
| 25 | Houben (2019) [79] | 52 | Gender: male n = 17, 32.7%; female n = 35, 67.3%; Age: US-TAP Block = 50.6 ± 12.9; Control (saline) = 47.5 ± 16.0. | Oral Etoricoxib 120 mg |
|
| Intra-operative: Sufentanil 0.1 mcg/kg Postoperative: Ketamine, Paracetamol 2 g (1 g for those with weight < 60 kg, and Morphine 2 mg bolus. | No | Pain | VAS |
| 26 | Janjua (2019) [80] | 100 | Gender: (male-female ratio = US-TAP Block 1.8: 2.6; Control (Port Site Infiltration): 1.7:2.8); Age: US-TAP Block = 48.70 ± 12.25; Port Site Infiltration = 48.35 ± 13.89. | No |
|
| Intra-operative: Nalbuphine 0.15 mg/kg, and Ketorolac 0.45 mg/kg Postoperative: Ketorolac 0.45 mg/kg by 2 8-hourly. | No | Pain | VAS |
| 27 | Karnik (2019) [81] | 80 | Gender: (male = 63, 78.8%; female 17, 21.2%); Age: US-TAP Block = 6.3 ± 3.8; Local infiltration = 5.5 ± 2.9. | Midazolam 0.05 mg/kg |
|
| Intra-operative: Fentanyl 2 mcg/kg, 1 mcg/kg as maintenance, and Paracetamol 15 mg/kg Postoperative: Diclofenac 1 mg/kg. | No | Pain | VAS |
| 28 | Khandelwal (2019) [82] | 80 | Gender (male = 25, 31.25%; female = 55, 68.75%); Age: US-STA Block = 42 ± 9.4; Control (intraperitoneal infiltration) = 44 ± 8.6. | No |
|
| Intra-operative: Fentanyl 2 mcg/kg. Postoperative: Tramadol 1 mg/kg. | No | Pain | NRS |
| 29 | Ribeiro (2019) [83] | 42 | Gender: (male = 27, 64.3%; female = 15, 35.7%); Age: US-OSTAP Block (Ropivacaine) = 45.45 ± 14.12; US-OSTAP Block (Normal saline) = 40.05 ± 11.91. | No |
|
| Intra-operative: Paracetamol 1 g Postoperative: Paracetamol 1 g 8-hourly, and Tramadol 1 mg/kg when pain threshold exceeds 4. | No | Pain | VAS |
| 30 | Siriwardana (2019) [84] | 90 | Gender: male-female ratio LAP-TAP = 0.214; Control = 0.333; (females: 72.2%; Age: 19–80 years). | No |
|
| Postoperative: Morphine 0.1 mg/kg. | Yes | Pain | Unspecified |
| 31 | Wu (2019) [85] | 160 | Gender: (male = 124, 77.5%; female 56, 22.5%); Age: LA1 = 48.0 ± 11.4; TL = 47.6 ± 10.1; TR = 48.6 ± 12.1. | No |
|
| Intra-operative: Flurbiprofen Axetil 1.5 mg/kg, and Remifentanil 1 mcg/kg. Postoperative: Flurbiprofen Axetil 1.5 mg/kg 6-hourly. | No | Pain | VAS |
| 32 | Arik (2020) [86] | 72 | Gender: (Male = 16, 23.6%; female = 56, 76.4%); Age: TAP Block = 42.8 ± 9.2; Local Anesthetic infiltration = 42.9 ± 11.2; IV-PCA = 46.6 ± 13.8. | No |
|
| Intra-operative: Remifentanil infusion Postoperative: Tramadol 5 mg/mL, 20 mg bolus with 20 min lockout time with a maximum of 200 mg per 4 h. | Yes | Pain | NRS |
| 33 | Kharbuja (2020) [87] | 60 | Gender: (male = 16, 26.7%; female 44, 73.3%); Age: Subcostal TAP = 40.27 ± 12.57; Control (Port Site Infiltration) = 38.77 ± 9.95. | Ranitidine 150 mg. |
|
| Intra-operative: Fentanyl 2 mcg/kg and Paracetamol 1 g. Postoperative: Fentanyl 20 mcg/kg, and Paracetamol 1 g 8-hourly. | No | Pain | VAS |
| 34 | Liang (2020) [88] | 120 | Gender: (male 43, 35.8%; female 77, 64.2%); Age: Group H = 49.5 ± 12.1; Group M 50.0 ± 13.0; Group L = 47.2 ± 13.9; Group C = 51.5 ± 12.8. | No |
|
| Intra-operative: Fentanyl 3 mcg/Kg), and maintenance using Remifentanil, at a dose of 0.1 mg/kg/hour. Postoperative: Parecoxib 40 mg, Morphine 2.5 mg (rescue) for those at PACU, and 100 mg (rescue) for those at ward. | No | Pain | NRS |
| 35 | Abdelfatah (2021) [89] | 60 | Gender: (female 51, 85%; male 9, 15%); Age: US-TAP Block 1 = 32.66 ± 10; US-TAP Block 2 = 31.67 ± 10.7. | No |
|
| Intra-operative: Fentanyl 1–2 mcg/kg, Postoperative: Fixed dose of Acetaminophen 500 mg/6 h, Morphine 5 mg. | No | Pain | VAS |
| 36 | Ergin (2021) [90] | 160 | Gender: (male 41, 25.62%; female 119, 74.38%); Age = 18–74 years. | No |
|
| Intra-operative: Paracetamol 1 g Postoperative: Tramadol 50 mg, and 100 mg for those with ongoing pain, and tabs Tenoxicam 20 mg 8-hourly. | No | Pain | VAS |
| 37 | Jung (2021) [91] | 76 | Gender: (male = 32, 42.1%; female 44, 57.9%); Age: BD-TAP = 48.9 ± 8.3; Control 47.5 ± 8.7. | No |
|
| Intra-operative: Remifentanil 2–6 μg/mL, Paracetamol 1 g, and Ibuprofen 400 mg. Postoperative: Oxycodone 3 mg (rescue), Ketorolac 30 mg (Day 0–1), and Tramadol 50 mg 8-hourly (from Day 1). | No | Pain | NRS |
| 38 | Sahu (2021) [92] | 60 | Gender: (male 35, 58.3%; female 25, 41.7%); Age: US-ESP Block 41.3 ± 11.8; OSTAP Block: 40.2 ± 11.1. | Midazolam 1 mg, Glycopyrrolate 0.2 mg |
|
| Intra-operative: Nalbuphine 0.1 mg/kg. Postoperative: Paracetamol 1 g 4-hourly x 24 h, Tramadol 1 mg/kg (rescue), and when pain persists, Diclofenac 75 mg was used as second option. | No | Pain | VAS |
| 39 | Saravanan (2021) [93] | 60 | Gender: (male = 26, 43.3%, female 34, 56.7%); Age: US-Modified BRILMA Block = 47.7 ± 11.12; Subcostal TAP Block 42.8 ± 11.09. | No |
|
| Intra-operative: Fentanyl 2 μg/kg, with 1 mcg/kg as maintenance dose, and Paracetamol 1 g. Postoperative: Morphine 0.1 mg/hour with a bolus of 1 mg, and lockout time of 10 min. | Yes | Pain | VAS |
| 40 | Vindal (2021) [94] | 100 | Gender: (male = 11, 11%; female = 89, 89%); Age: TAP Block 35(15.5); Port Site Infiltration: 35(18.25). | No |
|
| Intra-operative: NA Postoperative: Diclofenac sodium 50 mg (rescue) and 50 mg when needed. | No | Pain | VAS |
| 41 | Priyanka (2022) [95] | 80 | Gender: (male = 23, 33.3%; female 46, 66.7%); Age: US-TAP Block pre: 45.40; US-TAP Block post: 45.29. | The night before surgery: Ranitidine 150 mg, and Tabs Alprazolam 0.5 mg Prior to surgery: Glycopyrrolate 0.005 mg/kg, Midazolam 0.05 mg/kg, and Fentanyl 2 mcg/kg. |
|
| Intra-operative: Fentanyl 2 mcg/kg Postoperative: Tramadol 100 mg | No | Pain | VAS |
| 42 | Emile (2022) [96] | 110 | Gender: (male 11, 10%, female 99, 90%); Age: 40.9 ± 11.7. | No |
|
| Intra-operative: NA Postoperative: Paracetamol 1000 mg and Diclofenac were used for unsatisfactory pain relief. | No | Pain | VAS |
| 43 | Fargaly (2022) [97] | 50 | Gender: (male = 8, 16%; female 42, 84%); Age: US-TAP Block = 33.2 ± 9.1; QL Block = 32.7 ± 8.4. | No |
|
| Intra-operative: Fentanyl 1μgkg. Postoperative: Paracetamol 1 g 8-hourly, and Ketorolac30 mg 12-hourly. Morphine sulfate 3 mg bolus increments with the highest amount of 15 mg/4 h or 45 mg a day. | No | Pain | VAS |
| 44 | Han (2022) [98] | 180 | Gender: (male = 124, 68.9%; female = 56, 31.2%); Age: Group S = 45.78 ± 17.13; Group N = 44.52 ± 17.71; US-TAPB Block = 46.28 ± 13.18. | No |
|
| Intra-operative: Sufentanil 0.4–0.6 mcg/kg, Remifentanil 0.05–0.2 mcg/h. | Yes | Pain | VAS |
| 45 | Lee (2022) [99] | 53 | Gender: (male = 31, 54.5%; female = 22, 44.5%); Age: 1. US-TAPB –Block = 44.3 ± 9.8; Control = 45.7 ± 12.0. | No |
|
| Intra-operative: Remifentanil 0.5 mcg/kg and 0.1 mcg/kg/min as maintenance dose. Postoperative: Fentanyl 0.2 mcg/kg bolus and every hour with a 15 min lockout time. | Yes | Pain | VAS |
| 46 | Ozciftci (2022) [100] | 90 | Gender: (male = 24, 26.7%; female 66, 73.3%); Age: Control: 47.46 ± 11.83; TAP Block, unilateral 48.46 ± 12.05; TAP Block, bilateral: 51.90 ± 11.40. | Midazolam 0.02 mg/kg |
|
| Intra-operative: Paracetamol 1 g, Tramadol 2 mg/kg, Diclofenac sodium 75 mg. Postoperative: Paracetamol 1 g, Diclofenac sodium, and Tramadol 0.5 mg/kg hourly to a maximum of dose of 500 mg/day. | Yes | Pain | VNRS |
| 47 | Paudel (2022) [101] | 60 | Gender: (male = 14, 23.3%; female = 46, 76.7%); Age: TAP-Block: 41.63 ± 11.99; Control (local infiltration): 40.23 ± 11.42. | Ranitidine 150 mg |
|
| Intra-operative: Fentanyl 2 mcg/kg. Postoperative: NA | No | Pain | VAS |
| 48 | Rahimzadeh (2022) [102] | 76 | Gender: NR; Age: US-TAP (post-surgery) Block = 44.46 ± 8.30; US-TAP (after induction of anesthesia) = 45.0 ± 10.87. | Fentanyl 2 mcg/kg and Midazolam 0.12 mg/kg |
|
| Intra-operative: Fentanyl 2 μg/kg Postoperative: Acetaminophen20 mg/mL, and Ketorolac0.6 mg/mL bolus and 2 mL every 15 min. | Yes | Pain | NRS |
| Total study population: N = 3651; Male = 1090, 29.9%; Female = 1822, 49.9%; Unspecified genders = 739, 20.2%. Measures: VAS = 30, 62.5%; NRS = 12, 25%; VNRS = 3, 6.25%; Unspecified = 1, 2.1%; VAPA = 1, 2.1%; NA = 1, 2.1%. | ||||||||||
| No | Author/Year | Side Effects | Adverse Events | Complications | Drugs Used | Dose in mL or mg/kg |
|---|---|---|---|---|---|---|
| 1 | Ra (2010) [7] | |||||
| US-TAP block (0.25%) | Sleep disturbance (n = 2) | Levobupivacaine 0.25% | 30 mL | |||
| US-TAP block 0.5% | Sleep disturbance (n = 0) | Levobupivacaine 0.5% | 30 mL | |||
| Control | Sleep disturbance (n = 6) | |||||
| 2 | Petersen (2012) [21] | |||||
| US-TAP block (Ropivacaine) | Nausea scores 0–24 h (n = 0), with no difference in sedation scores. | Ropivacaine 0.5% + 2 mL of normal saline | 22 mL | |||
| US-TAP block (saline) | Nausea scores 0–24 h (n = 0), with no difference in sedation scores. | Ropivacaine 0.375% | 20 mL | |||
| 3 | Shin (2014) [61] | Ropivacaine 0.375% | 40 mL | |||
| US-OSTAP block | Nausea: none (n = 15), mild (n = 0), moderate (n = 0), severe (n = 0), and shoulders pain (n = 2). | |||||
| US-TAP block | Nausea: none (n = 12), mild (n = 2), moderate (n = 1), severe (n = 0), and shoulders pain (n = 0). | |||||
| Control | Nausea: none (n = 11), mild (n = 1), moderate (n = 3), severe (n = 0), and shoulders pain (n = 1). | |||||
| 4 | Huang (2016) [67] | |||||
| Control | Nausea (n = 3, vomiting n = 2, and abnormal sedation n = 2) | |||||
| US-TAP Block, bilateral | Nausea (n = 1, vomiting n = 0, and abnormal sedation n = 0) | Ropivacaine 0.375% | 30 mL | |||
| US-TAP block + 2 mL of Dexamethasone | Nausea (n = 0, vomiting n = 0, and abnormal sedation n = 0) | Ropivacaine 0.375% | 32 mL | |||
| 5 | Choi (2017) [71] | |||||
| US-TAP block (indwelling catheter inserted) | Nausea (n = 11), vomiting (n = 2), dizziness (n = 2), headache (n = 0), urinary retention (n = 11), pain at the needle insertion site (n = 0), and hematoma (n = 0). | Ropivacaine 0.2% | 20 mL | |||
| US-TAP block + PCA | Nausea (n = 15), vomiting (n = 2), dizziness (n = 1), headache (n = 3), urinary retention (n = 3), pain at the needle insertion site (n = 0), and hematoma (n = 1). | Ropivacaine 0.2% | 20 mL | |||
| Control (PCA only) | Nausea (n = 9), vomiting (n = 2), dizziness (n = 2), headache (n = 1), urinary retention (n = 0), pain at the needle insertion site (n = 2), and hematoma (n = 1). | 100 mL of normal saline + 40 mg Oxycodone and 180 mg of Ketorolac | ||||
| 6 | Houben (2019) [79] | |||||
| US-TAP block (Levobupivacaine) |
| Levobupivacaine 0.375% + Epinephrine 5 mcg/mL | 40 mL | |||
| US-TAP block (saline) |
| 40 mL 0.9% normal saline + Epinephrine 5 mcg/mL | 40 mL | |||
| 7 | Janjua (2019) [80] | |||||
| US-TAP block, unilateral | Respiratory depression (7.89%); others unclear | Bupivacaine 0.25% | 0.4 mL/kg | |||
| Control (port site infiltration) | Respiratory depression (2.56%); others unclear | Bupivacaine 0.25% | 0.4 mL/kg | |||
| 8 | Siriwardana (2019) [84] | |||||
| LAP-TAP + port site infiltration (× 4) | Vomiting episodes 0(0–4) | Bupivacaine 0.25% | 40 mL + 12 − 20 mL | |||
| Control (port site infiltration × 4) | Vomiting episodes 0(0–2) | Bupivacaine 0.25% | 12–20 mL | |||
| 9 | Liang (2020) [88] | |||||
| Group H | Postoperative nausea and vomiting were not significantly different between the 4 groups at 24 h (p = 0.180, p = 0.644). | Ropivacaine 0.75% | 20 mL | |||
| Group M | Ropivacaine 0.5% | 20 mL | ||||
| Group L | Ropivacaine 0.2% | 20 mL | ||||
| Group C | Normal saline 0.9% | 20 mL | ||||
| 10 | Ergin (2021) [90] | |||||
| LAI Group | 39 (97.5%) | Bupivacaine 0.5% | 20 mL | |||
| TAPB Group | 40 (100%) | Bupivacaine 0.5% + 20 cc of physiologic saline | 40 mL (20 + 20) | |||
| IPLA Group | 39 (97.5%) | Bupivacaine 0.5% | 20 mL | |||
| Control | 40 (100%) | |||||
| 11 | Jung (2021) [91] | |||||
| BD-TAP block, bilateral | Nausea (n = 4), and desaturation (n = 3). | Ropivacaine 0.25% | 60 mL | |||
| Control (sham block), bilateral | Nausea (n = 7), and desaturation (n = 2). | Normal saline 0.9% | 60 mL | |||
| 12 | Han (2022) [98] | |||||
| US-TAP block | Nausea and vomiting (n = 1), skin itching (n = 0), dizziness (n = 0), respiratory depression (n = 1), and puncture site hematoma (n = 0). | Ropivacaine 0.4% + 10 mg Tropisetron + 100 mL normal saline | 142 mL | |||
| Group S | Sufentanil 2 mg/kg via PCA + 10 mg Tropisetron + 100 mL normal saline | 100 mL | ||||
| Group N | Nausea and vomiting (n = 8), skin itching (n = 1), dizziness (n = 0), respiratory depression (n = 2), and puncture site hematoma (n = 0). | Nalbuphine 2 mg/kg via PCA + 10 mg Tropisetron + 100 mL normal saline | 100 mL | |||
| 13 | Lee (2022) [99] | |||||
| US-TAP block (Ropivacaine) | 1 h: nausea (n = 5), vomiting (n = 0); 8 h: nausea (n = 3), vomiting (n = 0); 24 h: nausea (n = 0), vomiting (n = 0). | Ropivacaine 0.375% | 40 mL | |||
| US-TAP block (normal saline) | 1 h: nausea (n = 12), vomiting (n = 1); 8 h: nausea (n = 8), vomiting (n = 2); 24 h: nausea (n = 3), vomiting (n = 0). | Normal saline 0.9% | 40 mL | |||
| 14 | Paudel (2022) [101] | |||||
| US-TAP block | Nausea (n = 0), and vomiting (n = 0). | Bupivacaine 0.25% | 40 mL | |||
| Control (port site infiltration) | Nausea (n = 1), and vomiting (n = 2). | Bupivacaine 0.25% | 20 mL |
| No | Author (Year) | Drugs Used | Meanpost | Meanpre | SDpre | Effect Size Index |
|---|---|---|---|---|---|---|
| 1 | Ortiz (2012) [20] | Morphine 24 h | ||||
| US-TAP block | 16.1 | 1.5 | 1.8 | 8.1 | ||
| Port infiltration | 15.4 | 0.9 | 2.0 | 7.3 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsharari, A.F.; Abuadas, F.H.; Alnassrallah, Y.S.; Salihu, D. Transversus Abdominis Plane Block as a Strategy for Effective Pain Management in Patients with Pain during Laparoscopic Cholecystectomy: A Systematic Review. J. Clin. Med. 2022, 11, 6896. https://doi.org/10.3390/jcm11236896
Alsharari AF, Abuadas FH, Alnassrallah YS, Salihu D. Transversus Abdominis Plane Block as a Strategy for Effective Pain Management in Patients with Pain during Laparoscopic Cholecystectomy: A Systematic Review. Journal of Clinical Medicine. 2022; 11(23):6896. https://doi.org/10.3390/jcm11236896
Chicago/Turabian StyleAlsharari, Abdalkarem Fedgash, Faud Hamdi Abuadas, Yaser Salman Alnassrallah, and Dauda Salihu. 2022. "Transversus Abdominis Plane Block as a Strategy for Effective Pain Management in Patients with Pain during Laparoscopic Cholecystectomy: A Systematic Review" Journal of Clinical Medicine 11, no. 23: 6896. https://doi.org/10.3390/jcm11236896
APA StyleAlsharari, A. F., Abuadas, F. H., Alnassrallah, Y. S., & Salihu, D. (2022). Transversus Abdominis Plane Block as a Strategy for Effective Pain Management in Patients with Pain during Laparoscopic Cholecystectomy: A Systematic Review. Journal of Clinical Medicine, 11(23), 6896. https://doi.org/10.3390/jcm11236896





