1. Introduction
Premolar extraction is a routine orthodontic treatment for correcting severe arch discrepancies, such as severe arch protrusion and crowding. The total extraction frequency of orthodontic treatment is about 25%, and 8.9–13.4% of cases undergo four first premolar extraction (i.e., four first premolars are taken out) [
1]. During orthodontic treatment, the closure of the extraction space depends on the mesial movement of the posterior teeth and the distal movement of the anterior teeth [
2]. In the process of tooth movement, alveolar bone resorption appears as a major risk [
3,
4].
Alveolar bone resorption is a potentially adverse outcome following orthodontic treatment [
5]. Although most of the alveolar bone resorption is within the clinically acceptable range, a severe alveolar bone reduction would have a harmful impact on the periodontal tissue and cause irreversible damage, including the loss of tooth adhesion, gingival recession, and even tooth loss [
6]. A variety of risk factors can cause alveolar bone resorption and affect its severity during treatment, such as age, treatment duration, and tooth position change, among which tooth position change is a factor that could be controlled by orthodontists [
7].
However, thus far, the correlation between tooth movement and its concomitant alveolar bone resorption remains controversial and not clear enough [
8,
9,
10]. Some previous studies used 2D images (lateral cephalogram or panoramic radiographs) to evaluate the incisor movement and alveolar bone resorption. However, using 2D images to measure 3D objects would lead to unavoidable errors [
11]. Compared with 2D images, CBCT provides accurate three-dimensional (3D) performance and thus could improve the reliability and comparability of measurements of dental and skeletal structures in clinical studies [
12]. CBCT is now widely applied in dentistry and is especially useful for orthodontic treatment, including clinical diagnosis, treatment planning, avoiding treatment risks, and evaluating prognosis [
13]. The more recent studies using CBCT images for the measurements showed that after orthodontic treatment involving the extraction of premolars, the palatal alveolar bone thickness of maxillary central incisors was closely related to the changes in the position and inclination of the incisors [
14,
15,
16,
17]. However, due to the small sample size, inconsistent reference lines, and disparate methods of measurement, the level of evidence was relatively low, and thus their results were very different. Moreover, as they did not report the specific type of spatial position movement or the amount of tooth movement, the quality of the studies is not good enough [
18]. Therefore, a detailed and comprehensive analysis is still needed to better reveal the correlation between alveolar bone resorption and tooth movement in orthodontic patients treated with premolar extraction.
In clinical research, establishing proper and unified three-dimensional (3D) vectors as a reference standard is a helpful method to describe and understand the structural changes in three dimensions, which could better guide treatment decision making. Our previous study proposed a method that combined a maxilla-based coordinate system and mandibular voxel-based superimposition so that the maxillary and mandibular structural changes could be directly measured and compared with the same 3D vectors [
19]. Utilizing this method, in this study, we performed accurate and comprehensive measurements of the movement of maxillary and mandibular central incisors and their associated alveolar bone resorption and, in a detailed and systematic way, constructed their correlation in adult patients undergoing orthodontic treatment with premolar extraction.
2. Materials and Methods
2.1. Sample Collection
This is a retrospective, cohort study, and patients who received orthodontic treatment with fixed appliances in the Department of Orthodontics, the West China Hospital of Stomatology, Sichuan University (Chengdu, China), from April 2016 to January 2022, were manually filtered using a medical record database of the hospital. The recorded diagnoses and treatment characteristics of patients were browsed. The patients were selected as research samples for this study based on the following inclusion and exclusion criteria:
The inclusion criteria were (1) CBCT images taken within 2 weeks before and after orthodontic treatment; (2) the imaging field of CBCT covering the cranial and maxillofacial skeletal structures from the orbitals to the mandibular body with the imaging data being sufficiently clear and free of artifacts; (3) patients were older than 18 years with all teeth from the central incisors to the second molars and had no supernumerary tooth, tooth defect, or metallic restorations; (4) patients with four first premolars extracted during orthodontic treatment; (5) the use of fixed appliances for orthodontic treatment; (6) moderate anchorage during space closure; (7) healthy periodontal tissue confirmed by both clinical examination and CBCT images, and no pathological alveolar bone resorption; (8) no history of maxillofacial trauma; and (9) complete space closure and good functional occlusion after treatment.
The exclusion criteria were (1) obvious facial asymmetry; (2) the maxillary sinus floor being too low to influence teeth movement; and (3) patients with craniofacial syndrome or systemic disease.
All the CBCT images were taken with the same CBCT machine (3D Accuitomo, Morita Group, Japan), which was set according to the manufacturer’s recommendations (140 × 100 mm FOV, 85 kV, 4.0 mA, and 360° rotation). The voxel size was 125 μm. The CBCT data were then stored in DICOM multifile format.
According to the results of our preliminary experiments and previous research [
5], the sample size was calculated using the PASS software (Version 2021; NCSS, LLC; Kaysville, UT, USA; ncss.com/software/pass.). By setting the significance level at 0.05 and power at 0.9, at least 63 samples were needed with an effect size of 0.416. Designed as a before–after comparison, this study needed at least 63 maxillary and mandibular central incisors.
2.2. Data Preparation before Measurement
Before measurement, data were prepared with the method proposed in our past research [
19,
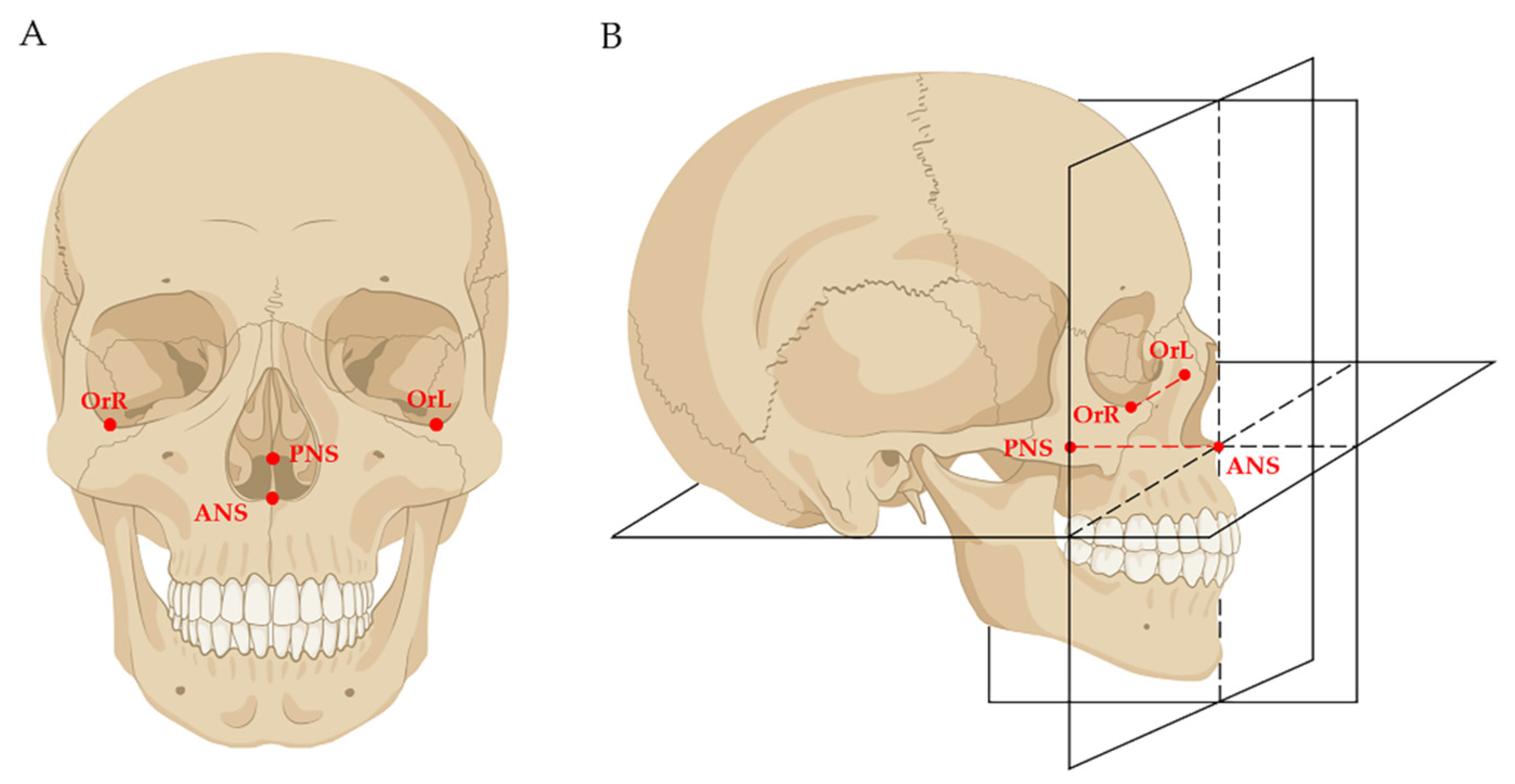
20]. Firstly, the DICOM data of both pre-treatment (T0) and post-treatment (T1) were imported into the Dolphin software (Version 11.8; Dolphin Imaging and Management Solutions; Chatsworth, CA, USA); mandibular voxel-based superimposition was conducted so that the mandibles of T0 and T1 were superimposed, and the interference of mandibular positional changes caused by orthodontic treatment was eliminated. After that, the data of T1 were reoriented and exported as the T2 data. Secondly, the T0, T1, and T2 data were imported into the Mimics Research software (Version 19.0; Materialise, Leuven, Belgium), and the 3D models were reconstructed. Thirdly, a maxilla-based coordinate system was constructed in T0 and T1 models by using four skeletal landmarks: ANS, PNS, OrL, and OrR (
Figure 1). As these four skeletal landmarks in adults were stable, the T0 and T1 coordinate systems were the same.
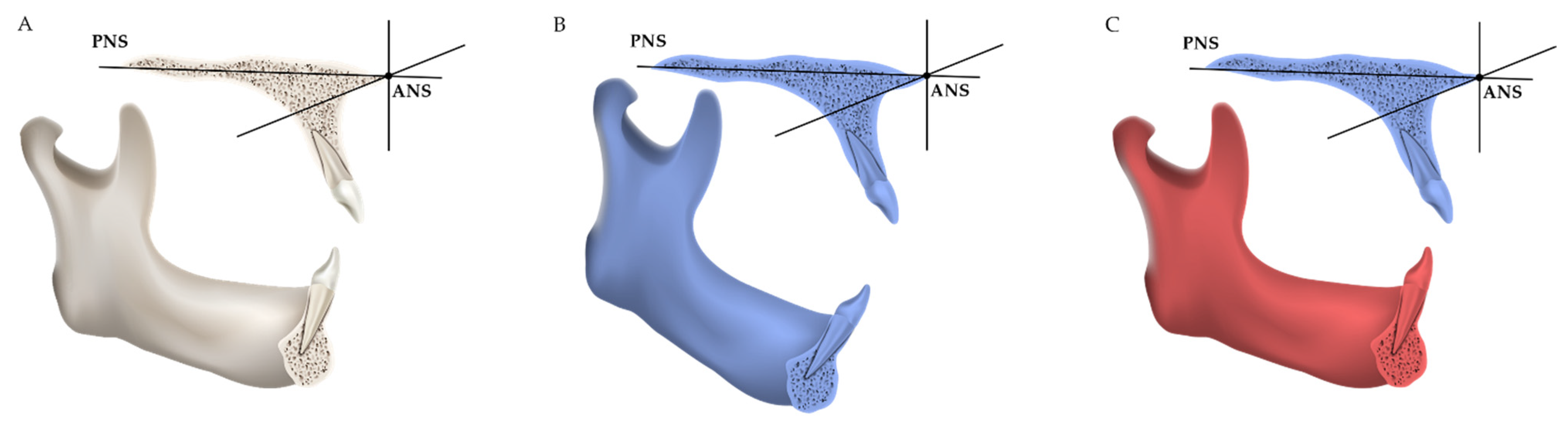
Finally, the T0 coordinate system was used for three-dimensional measurement of T0 maxillary and mandibular structures; the T1 coordinate system was used for three-dimensional measurement of T1 maxillary and T2 (i.e., the reoriented T1) mandibular structures (
Figure 2).
2.3. Measurements of Incisor Movement and Alveolar Bone Resorption
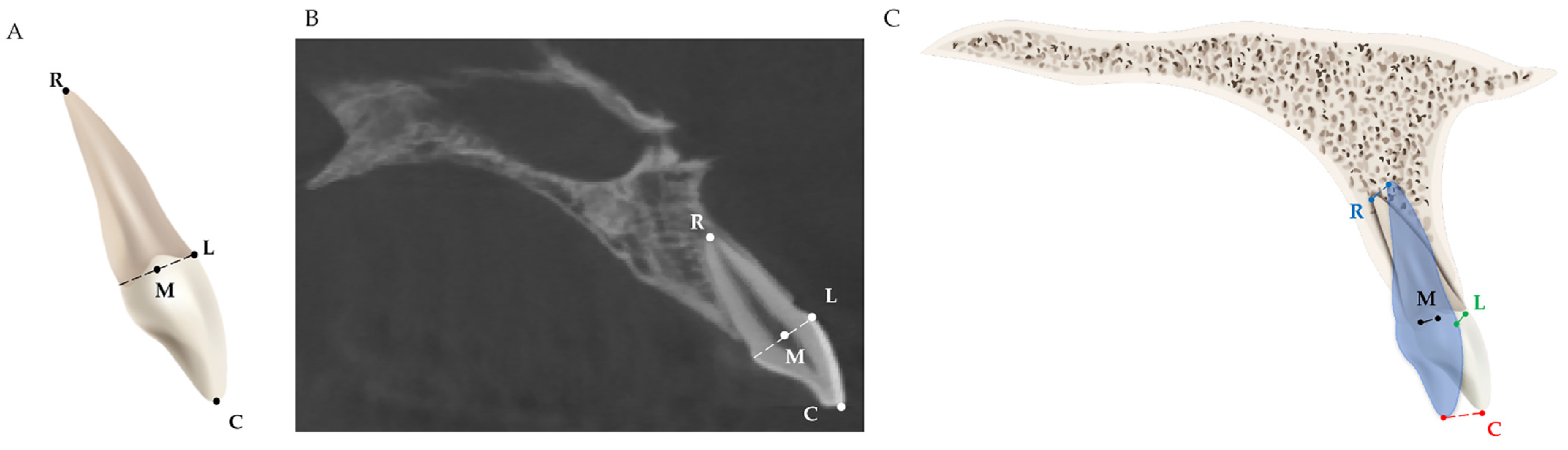
Four dental landmarks on the incisor were used for measuring the three-dimensional movement of the incisor after orthodontic treatment with premolar extraction, as shown in
Table 1 and
Figure 3.
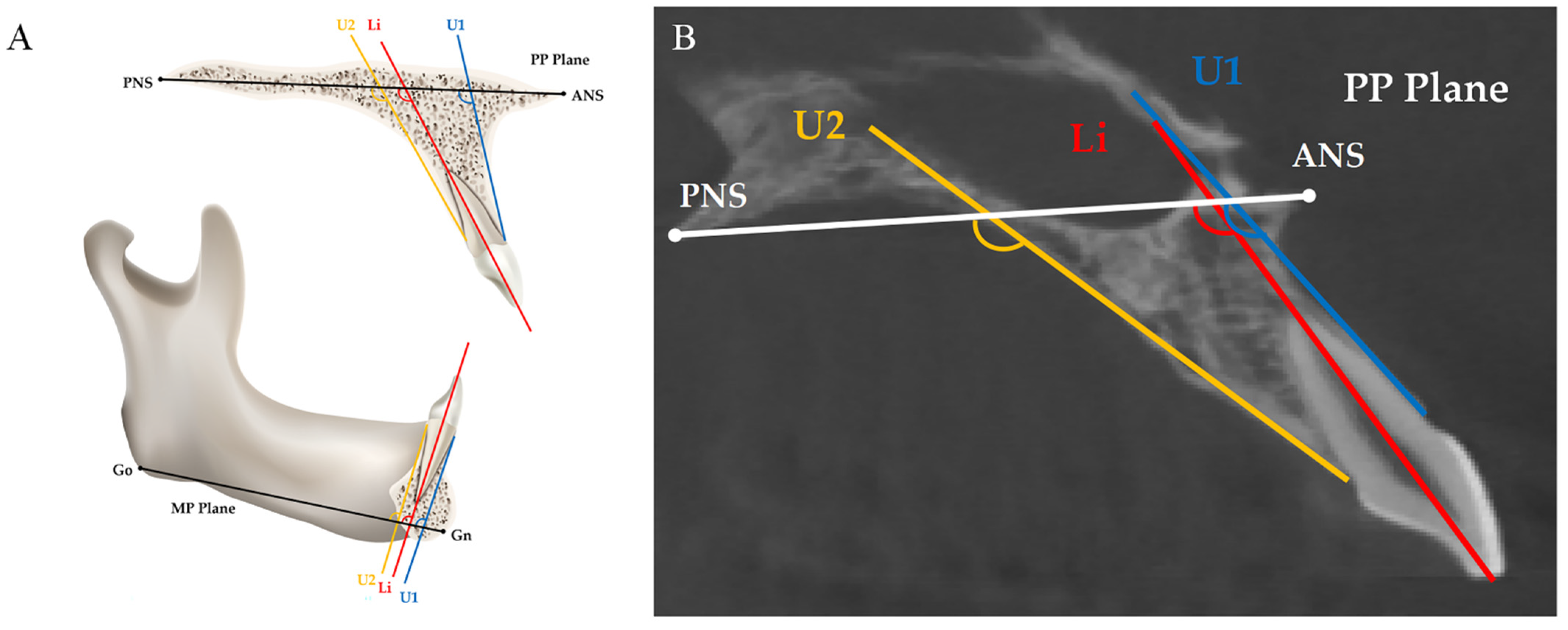
Two skeletal basic planes, the long axis of the incisor, and two measurement planes of the alveolar bone were used for evaluating the angular changes in the incisors and the alveolar ridge (
Table 2 and
Figure 4).
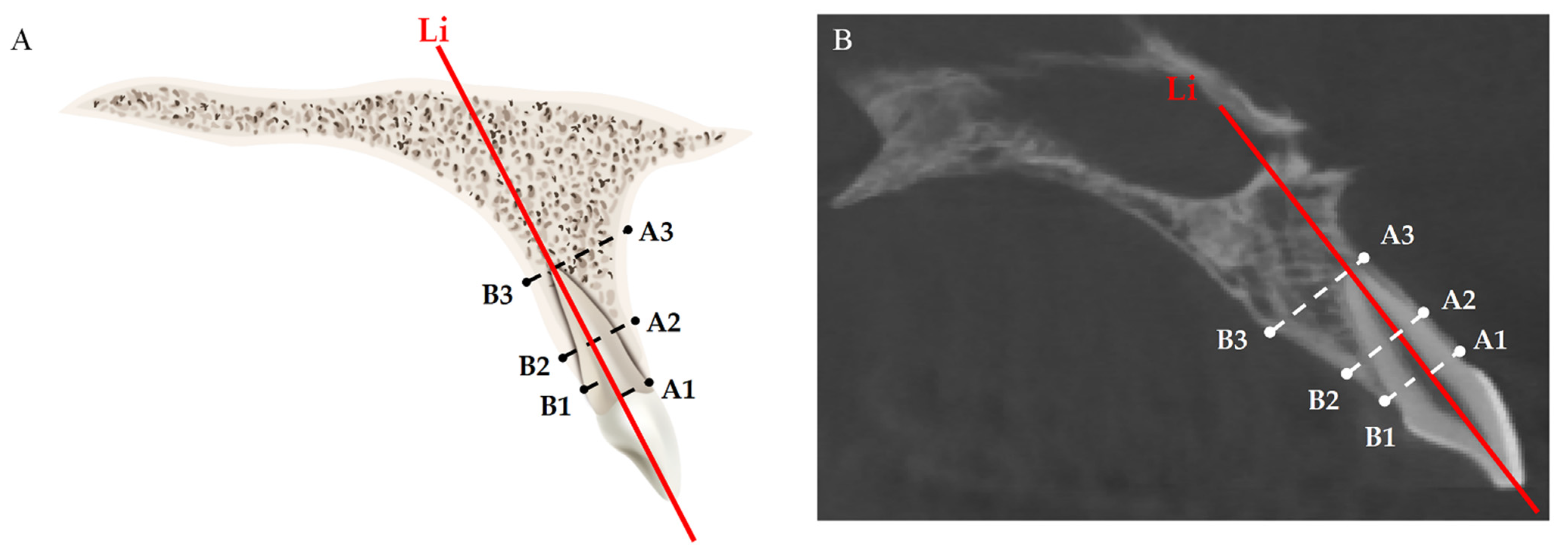
Six measurement landmarks on alveolar bone were used for evaluating the changes in alveolar bone thickness at the crestal, mid-root, and apical levels (
Table 3 and
Figure 5).
2.4. Data Analysis and Statistics
Each of the operations and measurements were conducted three times and independently by two operators under identical conditions. The intraclass correlation coefficient (ICC) was used to assess the inter-observer agreement. Statistical analysis was performed with the SPSS software (Version 22.0; IBM, Armonk, NY, USA).
The distribution types of all variables were examined by performing the Kolmogorov–Smirnov test. Normally distributed data (
p > 0.05) are described by means and standard deviations (x ± s), and non-normally distributed data are described by medians and quartile intervals (M ± Q). The Mann–Whitney U test was used to assess and compare the differences in age and treatment duration between sex groups. Paired
t-tests were performed to evaluate the incisor movement and changes in the alveolar bone thickness before and after treatment. The threshold of statistical significance was set at 0.05. The associations between the movements of different incisor landmarks and changes in the alveolar bone thickness at different levels were evaluated with Spearman’s correlations. Among these associations, the statistically significant ones were further explored with multiple linear regression analysis. Since conducting multiple analyses on the same dependent variable may result in an increased chance of committing a Type I error, the
p-value adjusted by Bonferroni’s correction is additionally indicated [
25,
26].
4. Discussion
Our results reveal the detailed and comprehensive associations between the changes in the spatial position of maxillary and mandibular central incisors and the resorption of the anterior alveolar bones at different levels in adult patients treated with orthodontic premolar extraction. These results were analyzed and established by using Spearman’s correlation and further confirmed by performing multiple linear regression.
The association between tooth movement and alveolar bone resorption in maxillary central incisors is different from that in mandibular central incisors. Their association in the mandibular central incisor showed regularity according to the Spearman correlation analysis: the movement of the incisor point is more likely to affect the alveolar bone whose level is closer to it. To be specific, the palatal alveolar bone resorption at the mid-root was correlated with the movement of the mid-point of the incisor neck, while the palatal alveolar bone resorption at the apical level with the root apex point; and although the labial alveolar bone resorption at the apical level was associated with all four points, the correlation coefficients increased with the point being closer (rR = 0.495 > rM = 0.485 > rL = 0.349 > rC = 0.280). However, this regularity was not observed in the maxillary central incisor. This could be explained by the fact that the movement types of the maxillary and mandibular central incisors are normally not the same in extraction cases with moderate anchorage. Maxillary central incisors tend to present movement between crown tipping and bodily movement because of the positive torque moment in the brackets, while mandibular central incisors present the tipping movement with little root movement [
27,
28].
There has been a consensus that during orthodontic tooth movement (OTM), alveolar bone remodeling is a balance between bone resorption and regeneration, and as shown in some previous studies, after incisor retraction, a rise in the thickness of the labial or palatal alveolar bone may occur [
29,
30,
31,
32]. Admittedly, in this study, the alveolar bone changes were all bone resorption, and no bone regeneration was observed, neither on the labial nor on the palatal side nor at any of the levels. However, this phenomenon could be explained from two aspects. The first aspect to consider is the temporal sequences of OTM. The mechanism of alveolar bone remodeling involves responding to the stimulation of orthodontic force: on the compression side, osteoclasts would appear, and the alveolar bone would be resorbed; while on the tension side, osteoblasts would appear, and the alveolar bone would regenerate [
33]. However, cell activation and differentiation are not simultaneous; cathepsins and matrix metalloproteases (MMPs), the two enzymes that contribute to bone resorption, would increase on the compression side at the early stage of OTM [
34]. Hence, alveolar bone formation tends to be slower than bone resorption. In this study, CBCT images were obtained within only two weeks after finishing treatment, which was a too short period of time for bone regeneration; therefore, alveolar bone regeneration was not observed in all the data. The other aspect pertains to the average alveolar bone loss in adults. As has been revealed in previous studies, there is an overall rate of alveolar bone loss of about 0.02–0.09 mm per year in general populations [
35,
36]. Alveolar bone loss is closely related to smoking, age, gender, etc. [
37,
38]. Even in patients taking orthodontic treatment without premolar extraction, alveolar bone loss was also observed [
39].
This study has several advantages. Firstly, it innovatively uses four landmarks to describe the movement of the incisor, which help better understand its three-dimensional movement. Secondly, compared with other similar studies that include several tens of samples, our sample size is considerably larger, which potentially increases the reliability of the results. Thirdly, because the method we used for data preparation in this study has a stable maxillary-based coordinate system and mandibular voxel-based superimposition, which eliminates the interference of mandibular position change, we could accurately locate the landmarks and conduct three-dimensional measurements.
This study has a few limitations. One limitation was the sex distribution in the samples. Only ten males were selected, probably due to the disparate willingness between adult males and females to receive orthodontic treatment [
40]. Secondly, as mentioned, the alveolar bone level was evaluated within a very short period of time after finishing treatment; thus, further studies are still needed to understand the alveolar bone changes after periodontal reconstruction and stabilization. Thirdly, as the voxel size we used for CBCT images in this study was 125 μm, according to previous studies, linear measurements might show more or less overestimation or underestimation [
41]. Hence, we remind readers that potential measurement errors may be encountered with CBCT, which should be taken into consideration.
Our findings revealed a relatively regular and concrete pattern of how alveolar bone changes follow the incisor retraction in adults with premolar extraction. This is clinically meaningful for orthodontic treatment. On the one hand, it is instrumental for orthodontists to have a relatively accurate prediction of alveolar bone resorption based on the specific movements of central incisors. On the other hand, it may help orthodontists to reduce the risk of undesirable alveolar bone resorption via better analyzing and adjusting the three-dimensional movement types of incisors.