The Impact of Prehospital and Hospital Care on Clinical Outcomes in Out-of-Hospital Cardiac Arrest
Abstract
1. Introduction
2. Methods
2.1. Clinical Setting
2.2. Prehospital Care Data Collection
2.3. Hospital Care Data Collection
2.4. Primary End Point
2.5. Secondary Endpoint
2.6. Statistical Analysis
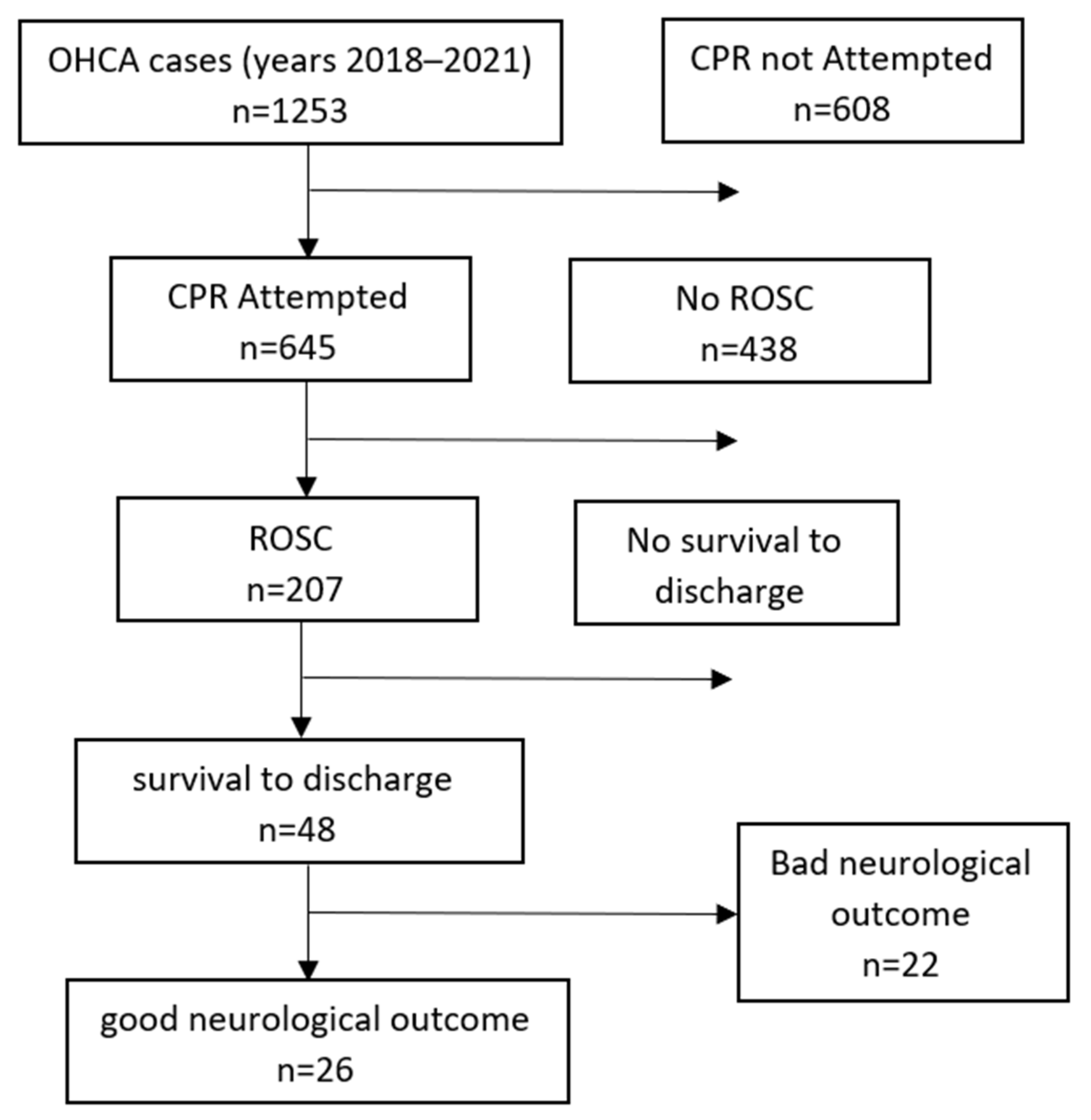
3. Results
3.1. Pre-Hospital and Hospital Care
3.2. ROSC
3.3. Survival to Discharge
3.4. Neurological Outcome
3.5. First Year of the COVID-19 Pandemic
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Gan, Y.; Jiang, N.; Wang, R.; Chen, Y.; Luo, Z.; Zong, Q.; Chen, S.; Lv, C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: A systematic review and meta-analysis. Crit. Care 2020, 24, 61. [Google Scholar] [CrossRef] [PubMed]
- Sasson, C.; Rogers, M.A.; Dahl, J.; Kellermann, A.L. Predictors of Survival From Out-of-Hospital Cardiac Arrest. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 63–81. [Google Scholar] [CrossRef]
- Fridman, M.; Barnes, V.; Whyman, A.; Currell, A.; Bernard, S.; Walker, T.; Smith, K.L. A model of survival following pre-hospital cardiac arrest based on the Victorian Ambulance Cardiac Arrest Register. Resuscitation 2007, 75, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Tagami, T.; Matsui, H.; Fushimi, K.; Yasunaga, H. Changes in Therapeutic Hypothermia and Coronary Intervention Provision and In-Hospital Mortality of Patients With Out-of-Hospital Cardiac Arrest. Crit. Care Med. 2016, 44, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.K.; Meng, H.; Parikh, P.B. Trends in Management and Mortality in Adults Hospitalized With Cardiac Arrest in the United States. J. Intensiv. Care Med. 2017, 34, 252–258. [Google Scholar] [CrossRef]
- Phelps, R.; Dumas, F.; Maynard, C.; Silver, J.; Rea, T. Cerebral Performance Category and Long-Term Prognosis Following Out-of-Hospital Cardiac Arrest*. Crit. Care Med. 2013, 41, 1252–1257. [Google Scholar] [CrossRef]
- Ginsberg, G.M.; Kark, J.D.; Einav, S. Cost–utility analysis of treating out of hospital cardiac arrests in Jerusalem. Resuscitation 2015, 86, 54–61. [Google Scholar] [CrossRef]
- Blom, M.T.; Oving, I.; Berdowski, J.; van Valkengoed, I.G.M.; Bardai, A.; Tan, H.L. Women have lower chances than men to be resuscitated and survive out-of-hospital cardiac arrest. Eur. Hear. J. 2019, 40, 3824–3834. [Google Scholar] [CrossRef]
- Safdar, B.; Stolz, U.; Stiell, I.; Cone, D.C.; Bobrow, B.J.; Deboehr, M.; Dreyer, J.; Maloney, J.; Spaite, D. Differential Survival for Men and Women from Out-of-hospital Cardiac Arrest Varies by Age: Results from the OPALS Study. Acad. Emerg. Med. 2014, 21, 1503–1511. [Google Scholar] [CrossRef]
- Sarkisian, L.; Mickley, H.; Schakow, H.; Gerke, O.; Starck, S.M.; Jensen, J.J.; Møller, J.E.; Jørgensen, G.; Henriksen, F.L. Use and coverage of automated external defibrillators according to location in out-of-hospital cardiac arrest. Resuscitation 2021, 162, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Murakami, Y.; Iwami, T.; Kitamura, T.; Nishiyama, C.; Nishiuchi, T.; Hayashi, Y.; Kawamura, T.; Project, T.U.O. Outcomes of Out-of-Hospital Cardiac Arrest by Public Location in the Public-Access Defibrillation Era. J. Am. Hear. Assoc. 2014, 3, e000533. [Google Scholar] [CrossRef]
- Rajan, S.; Folke, F.; Hansen, S.M.; Hansen, C.M.; Kragholm, K.; Gerds, T.A.; Lippert, F.K.; Karlsson, L.; Møller, S.; Køber, L.; et al. Incidence and survival outcome according to heart rhythm during resuscitation attempt in out-of-hospital cardiac arrest patients with presumed cardiac etiology. Resuscitation 2017, 114, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Majewski, D.; Ball, S.; Bailey, P.; Bray, J.; Finn, J. Long-term survival among OHCA patients who survive to 30 days: Does initial arrest rhythm remain a prognostic determinant? Resuscitation 2021, 162, 128–134. [Google Scholar] [CrossRef]
- Søholm, H.; Hassager, C.; Lippert, F.; Winther-Jensen, M.; Thomsen, J.H.; Friberg, H.; Bro-Jeppesen, J.; Køber, L.; Kjaergaard, J. Factors Associated With Successful Resuscitation After Out-of-Hospital Cardiac Arrest and Temporal Trends in Survival and Comorbidity. Ann. Emerg. Med. 2015, 65, 523–531.e2. [Google Scholar] [CrossRef]
- Oving, I.; de Graaf, C.; Karlsson, L.; Jonsson, M.; Kramer-Johansen, J.; Berglund, E.; Hulleman, M.; Beesems, S.G.; Koster, R.W.; Olasveengen, T.M.; et al. Occurrence of shockable rhythm in out-of-hospital cardiac arrest over time: A report from the COSTA group. Resuscitation 2020, 151, 67–74. [Google Scholar] [CrossRef]
- Nehme, Z.; Andrew, E.; Bernard, S.; Haskins, B.; Smith, K. Trends in survival from out-of-hospital cardiac arrests defibrillated by paramedics, first responders and bystanders. Resuscitation 2019, 143, 85–91, Epub 17 August 2019. [Google Scholar] [CrossRef] [PubMed]
- Meier, P.; Baker, P.; Jost, D.; Jacobs, I.; Henzi, B.; Knapp, G.; Sasson, C. Chest compressions before defibrillation for out-of-hospital cardiac arrest: A meta-analysis of randomized controlled clinical trials. BMC Med. 2010, 8, 52. [Google Scholar] [CrossRef]
- Camuglia, A.C.; Randhawa, V.K.; Lavi, S.; Walters, D.L. Cardiac catheterization is associated with superior outcomes for survivors of out of hospital cardiac arrest: Review and meta-analysis. Resuscitation 2014, 85, 1533–1540. [Google Scholar] [CrossRef]
- Zanuttini, D.; Armellini, I.; Nucifora, G.; Carchietti, E.; Trillò, G.; Spedicato, L.; Bernardi, G.; Proclemer, A. Impact of Emergency Coronary Angiography on In-Hospital Outcome of Unconscious Survivors After Out-of-Hospital Cardiac Arrest. Am. J. Cardiol. 2012, 110, 1723–1728. [Google Scholar] [CrossRef]
- Onoe, A.; Kajino, K.; Daya, M.R.; Ong, M.E.H.; Nakamura, F.; Nakajima, M.; Takahashi, H.; Kishimoto, M.; Sakuramoto, K.; Muroya, T.; et al. Outcomes of patients with OHCA of presumed cardiac etiology that did not achieve prehospital restoration of spontaneous circulation: The All-Japan Utstein Registry experience. Resuscitation 2021, 162, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Fothergill, R.T.; Smith, A.L.; Wrigley, F.; Perkins, G.D. Out-of-Hospital Cardiac Arrest in London during the COVID-19 pandemic. Resusc. Plus 2020, 5, 100066. [Google Scholar] [CrossRef] [PubMed]
- Lim, Z.J.; Reddy, M.P.; Afroz, A.; Billah, B.; Shekar, K.; Subramaniam, A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: A systematic review and meta-analysis. Resuscitation 2020, 157, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Masuda, Y.; Teoh, S.E.; Yeo, J.W.; Tan, D.J.H.; Jimian, D.L.; Lim, S.L.; Ong, M.E.H.; Blewer, A.L.; Ho, A.F.W. Variation in community and ambulance care processes for out-of-hospital cardiac arrest during the COVID-19 pandemic: A systematic review and meta-analysis. Sci. Rep. 2022, 12, 800. [Google Scholar] [CrossRef]
| Characteristic | No ROSC (438) | ROSC (n = 207) | PV | |
|---|---|---|---|---|
| Gender | Male | 229 (65.6%) | 120 (34.4%) | 0.176 |
| Female | 209 (70.6%) | 87 (29.4%) | ||
| Age (years) | median (IQR) | 80 (70–88) | 75 (66–85) | 0.004 |
| Location | Public | 64 (54.3%) | 54 (45.7%) | <0.001 |
| Home | 374 (71.0%%) | 153 (29.0%) | ||
| Witnessed status | Bystanders | 191 (59.0%) | 133 (41.0%) | <0.001 |
| EMS | 68 (59.7%) | 46 (40.3%) | ||
| Unwitnessed | 164 (87.7%) | 23 (12.3%) | ||
| Unknown | 15 (75%) | 5 (25%) | ||
| BLS before MICU | No | 96 (65.3%) | 51 (34.7%) | 0.031 |
| By bystanders | 101 (61.2%) | 64 (38.8%) | ||
| By professionals | 241 (72.3%) | 92 (27.6%) | ||
| AED use | No | 158 (64.2%) | 88 (35.8%) | <0.001 |
| Yes and shock | 34 (50.0%) | 34 (50.0%) | ||
| Yes and no shock | 163 (75.5%) | 53 (24.5%) | ||
| Unknown | 83 (72.2%) | 32 (27.8%) | ||
| AED user | Bystanders | 4 (40.0%) | 6 (60.0%) | |
| On-calls | 91 (69.0%) | 41 (31.0%) | 0.136 | |
| EMS | 98 (69.0%) | 44 (31.0%) | ||
| Unknown | 89 (74.2%) | 31 (25.8%) | ||
| Didn’t use | 156 (64.7%) | 85 (35.3%) | ||
| First documented rhythm by MICU | VT/VF | 23 (41.0%) | 33 (59.0%) | <0.001 |
| PEA/Asystole | 401 (71.2%) | 162 (28.8%) | ||
| All others | 14 (53.9%) | 12 (46.1%) | ||
| Minute to arrival | median (IQR) | 6 (4–8) | 6 (4–8) | 0.836 |
| DA-CPR | didn’t try (1) | 230 (75.2%) | 76 (24.8%) | <0.001 |
| tried but didn’t do (2) | 8 (80%) | 2 (20%) | ||
| done (3) | 145 (62.2%) | 88 (37.8%) | ||
| Arrest witnessed by EMS (4) | 55 (57.3%) | 41 (42.7%) | ||
| Characteristic | ROSC | |||
|---|---|---|---|---|
| Adjusted OR | CI 95% | PV | ||
| Gender | Male (reference) | |||
| Female | 1.084 | 0.743–1.582 | 0.674 | |
| Location | Public (reference) | |||
| Home | 0.594 | 0.369–0.957 | 0.032 | |
| Witnessed status | Bystanders (reference) | |||
| EMS | 0.562 | 0.214–1.480.244 | 0.244 | |
| Unwitnessed | 0.226 | 0.369–0.957 | 0.032 | |
| Unknown | 0.512 | 0.173–1.510 | 0.225 | |
| BLS before MICU | No (reference) | |||
| By bystanders | 1.102 | 0.527–2.301 | 0.795 | |
| By professionals | 0.903 | 0.469–1.738 | 0.76 | |
| AED Use | No (reference) | |||
| Yes and shock | 1.09676 | 0.530–2.265 | 0.803 | |
| Yes and no shock | 0.88338 | 0.494–1.577 | 0.675 | |
| Unknown | 0.96074 | 0.506–1.823 | 0.902 | |
| First documented rhythm by MICU | VT/VF (reference) | |||
| PEA/asystula | 0.5 | 0.257–0.980 | 0.043 | |
| All others | 0.745 | 0.271–2.044 | 0.568 | |
| DA-CPR | Did not try (reference) | |||
| Tried but didn’t do | 0.758 | 0.148–3.867 | 0.739 | |
| Done | 1.63 | 1.007–2.650 | 0.046 | |
| Collapse by EMS | 2.141 | 0.801–5.727 | 0.129 | |
| Characteristic | Did not Survive to Discharge (n = 167) | Survived to Discharge (n = 48) | PV | |
|---|---|---|---|---|
| Gender | Male | 88 (70.4%) | 37 (29.6%) | 0.0025 |
| Female | 79 (87.8%) | 11 (12.2%) | ||
| Age (years) | median (IQR) | 77 (67–86) | 64 (52.25–75.5) | <0.0001 |
| Location | Public | 49 (70.0%) | 21 (30.0%) | 0.0604 |
| Home | 118 (81.4%) | 27 (18.6%) | ||
| Witnessed status | Bystanders | 81 (72.3%) | 31 (27.7%) | 0.1311 |
| EMS | 59 (80.8%) | 14 (19.2%) | ||
| Unwitnessed | 23 (92.0%) | 2 (8.0%) | ||
| Unknown | 4 (80.0%) | 1 (20.0%) | ||
| BLS before MICU | No | 62 (87.3%) | 9 (12.7%) | 0.039 |
| By bystanders | 43 (69.4%) | 19 (30.6%) | ||
| By professionals | 62 (75.6%) | 20 (24.4%) | ||
| AED Use | No | 82 (80.4%) | 20 (19.6%) | <0.001 |
| Yes and shock | 18 (48.6%) | 19 (51.4%) | ||
| Yes and no shock | 39 (86.7%) | 6 (13.3%) | ||
| Unknown | 28 (90.3%) | 3 (9.7%) | ||
| AED user | Bystanders | 1 (16.7%) | 5 (83.3%) | <0.001 |
| On-calls | 24 (60.0%) | 16 (40.0%) | ||
| EMS | 33 (84.6%) | 6 (15.4%) | ||
| Unknown | 27 (90.0%) | 3 (10.0%) | ||
| Didn’t use | 82 (82.0%) | 18 (18.0%) | ||
| First documented rhythm by MICU | VT/VF | 12 (35.3%) | 22 (64.7%) | <0.001 |
| PEA/asystula | 148 (87.6%) | 21 (12.4%) | ||
| All others | 7 (58.3%) | 5 (41.7%) | ||
| Minutes to arrival | median (IQR) | 6 (4–9) | 5.5 (4–7.75) | 0.23682 |
| DA-CPR | Did not try | 53 (81.5%) | 12 (18.5%) | 0.5803 |
| Tried but didn’t do | 2 (100%) | 0 (0%) | ||
| Done | 59 (72.8%) | 22 (27.2%) | ||
| Collapse by EMS | 53 (79.1%) | 14 (20.9%) | ||
| STEMI | Yes | 25 (48.1%) | 27 (51.9%) | <0.001 |
| No | 89 (87.3%) | 13 (12.7%) | ||
| No ECG | 53 (86.9%) | 8 (13.1%) | ||
| Catheterization | NO | 155 (88.6%) | 20 (11.4%) | <0.001 |
| Yes | 12 (30.0%) | 28 (70.0%) | ||
| CV Comorbidities | No | 12 (50%) | 12 (50%) | <0.001 |
| Yes | 155 (81.2%) | 36 (18.8%) | ||
| Basic function | Dependent | 101 (90.2%) | 11 (9.8%) | <0.001 |
| Independent | 66 (64.1%) | 37 (35.9%) | ||
| Characteristic | Survival to Discharge | |||
|---|---|---|---|---|
| Adjusted OR | CI 95% | PV | ||
| BLS before MICU | No (reference) | |||
| By bystanders | 1.916 | 0.749–4.9 | 0.17423 | |
| By professionals | 1.633 | 0.656–1.063 | 0.29131 | |
| AED Use | No (reference) | |||
| Yes and shock | 2.629 | 1.109–6.229 | 0.028 | |
| Yes and no shock | 0.569 | 0.203–1.596 | 0.284 | |
| Unknown | 0.347 | 0.091–1.323 | 0.121 | |
| AED User | Bystanders | 12 | 1.24–116.2 | 0.03 |
| On-calls | 2.54 | 1.07–6 | 0.03 | |
| EMS | 0.059 | 02–1.71 | 0.33 | |
| Unknown | 0.387 | 0.09–1.5 | 0.17 | |
| Did not use (reference) | ||||
| First documented rhythm by MICU | VT/VF (reference) | |||
| PEA/asystole | 0.114 | 0.046–0.280 | <0.001 | |
| All others | 0.499 | 0.125–1.994 | 0.325 | |
| STEMI | Yes (reference) | |||
| No | 0.171 | 0.074–0.390 | <0.001 | |
| No ECG | 0.2 | 0.076–0.523 | 0.001 | |
| Catheterization | No (reference) | |||
| Yes | 12.95 | 5.426–30.918 | <0.001 | |
| CV comorbidities | Yes (reference) | |||
| No | 2.073 | 0.757–5.678 | 0.155 | |
| Basic function | Dependent (reference) | |||
| Independent | 2.869 | 1.228–6.702 | 0.014 | |
| Characteristic | Non-Favorable Neurological Outcome (n = 189) | Favorable Neurological Outcome (n = 26) | PV | |
|---|---|---|---|---|
| Gender | Male | 105 (84.0%) | 20 (16.0%) | 0.038 |
| Female | 84 (93.3%) | 6 (6.7%) | ||
| Age (years) | median (IQR) | 76 (65.5–86) | 58.5 (51.25–72) | <0.001 |
| Location | Public | 57 (81.4%) | 13 (18.6%) | 0.042 |
| Home | 132 (91.0%) | 13 (9.0%) | ||
| Witnessed status | Bystanders | 95 (84.8%) | 17 (15.2%) | 0.436 |
| EMS | 65 (89.0%) | 8 (11.0%) | ||
| Unwitnessed | 24 (96.0%) | 1 (4.0%) | ||
| Unknown | 5 (100%) | 0 (0%) | ||
| BLS before MICU | No | 69 (97.2%) | 2 (2.8%) | 0.006 |
| By bystanders | 54 (87.1%) | 8 (12.9%) | ||
| By professionals | 66 (80.5%) | 16 (19.5%) | ||
| AED Use | No | 94 (92.2%) | 8 (7.8%) | <0.001 |
| Yes and shock | 24 (64.9%) | 13 (35.1%) | ||
| Yes and no shock | 42 (93.3%) | 3 (6.7%) | ||
| Unknown | 29 (93.5%) | 2 (6.5%) | ||
| AED user | Bystanders | 1 (16.7%) | 5 (83.3%) | <0.001 |
| On-calls | 30 (75%) | 10 (25%) | ||
| EMS | 36 (92.3%) | 3 (7.7%) | ||
| Unknown | 28 (93.3%) | 2 (6.7%) | ||
| Did not use | 94 (94.0%) | 6 (6.0%) | ||
| First documented rhythm by MICU | VT/VF | 17 (50%) | 17 (50%) | <0.001 |
| PEA/asystula | 164 (97.0) | 5 (3.0%) | ||
| All others | 8 (66.7%) | 4 (33.3%) | ||
| Minutes to arrival | median (IQR) | 6 (4–9) | 6 (4–7.25) | 0.536 |
| DA-CPR | Did not try | 58 (9.2%) | 7 (10.8%) | 0.922 |
| Tried but did not do | 2 (100%) | 0 (0%) | ||
| Done | 70 (86.4%) | 11 (13.6%) | ||
| Collapse by EMS | 59 (88.1%) | 8 (11.9%) | ||
| STEMI | Yes | 36 (69.2%) | 16 (30.8%) | <0.001 |
| No | 96 (94.1%) | 6 (5.9%) | ||
| No ECG | 57 (93.4%) | 4 (6.6%) | ||
| Catheterization | NO | 169 (96.6%) | 6 (3.4%) | <0.001 |
| Yes | 20 (50.0%) | 20 (50.0%) | ||
| CV Comorbidities | No | 176 (92.1%) | 15 (7.9%) | <0.001 |
| Yes | 13 (54.2%) | 11 (45.8%) | ||
| Basic function | Dependent | 112 (100%) | 0 (0%) | <0.001 |
| Independent | 77 (74.8%) | 26 (25.2%) | ||
| Characteristic | Good Neurological Outcome | |||
|---|---|---|---|---|
| Adjusted OR | CI 95% | PV | ||
| Location | Public (reference) | |||
| Home | 0.674 | 0.264–1.585 | 0.341 | |
| BLS before MICU | No (reference) | |||
| By bystanders | 2.9 | 0.563–14.939 | 0.202 | |
| By professionals | 6.026 | 1.283–28.3 | 0.022 | |
| AED Use | No (reference) | |||
| Yes and shock | 3.96 | 1.389–11.289 | 0.01 | |
| Yes and no shock | 0.732 | 0.175–3.059 | 0.669 | |
| Unknown | 0.609 | 0.115–3.211 | 0.559 | |
| AED User | Bystanders | 44.614 | 4.154–479.15 | 0.001 |
| On-calls | 4.64 | 1.476–14.626 | 0.008 | |
| EMS | 0.93 | 0.209–4.133 | 0.924 | |
| Unknown | 0.833 | 0.149–4.647 | 0.835 | |
| Did not use (reference) | ||||
| First documented rhythm by MICU | VT/VF (reference) | |||
| PEA/asystole | 0.035 | 0.009–0.127 | <0.001 | |
| All others | 0.612 | 0.141–2.66 | 0.513 | |
| STEMI | Yes (reference) | |||
| No | 0.177 | 0.061–0.51 | 0.001 | |
| No ECG | 0.233 | 0.067–0.801 | 0.02 | |
| Catheterization | No (reference) | |||
| Yes | 23.12 | 7.33–72.87 | <0.001 | |
| CV comorbidities | Yes (reference) | |||
| No | 4.956 | 1.62–15.159 | 0.005 | |
| Basic function | Dependent (reference) | |||
| Independent | >10,000 | 173.91–10,000+ | 0.001 | |
| COVID-19 Period | Non-COVID-19 Period | PV | ||
|---|---|---|---|---|
| ROSC | No | 214 (67.72%) | 224 (68.09%) | 0.92 |
| Yes | 102 (32.28%) | 105 (31.91%) | ||
| Survival to discharge | No | 81 (76.41%) | 88 (79.27%) | 0.61 |
| Yes | 25 (23.58%) | 23 (20.72%) | ||
| Neurological outcome | Favorable | 93 (87.73%) | 98 (88.28%) | 0.9 |
| Unfavorable | 13 (12.26%) | 13 (11.71%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deri, Y.; Berzon, B.; West, D.; Machloof, M.; Strugo, R.; Kaplan, T.; Soffer, S. The Impact of Prehospital and Hospital Care on Clinical Outcomes in Out-of-Hospital Cardiac Arrest. J. Clin. Med. 2022, 11, 6851. https://doi.org/10.3390/jcm11226851
Deri Y, Berzon B, West D, Machloof M, Strugo R, Kaplan T, Soffer S. The Impact of Prehospital and Hospital Care on Clinical Outcomes in Out-of-Hospital Cardiac Arrest. Journal of Clinical Medicine. 2022; 11(22):6851. https://doi.org/10.3390/jcm11226851
Chicago/Turabian StyleDeri, Yotam, Baruch Berzon, Debra West, Matan Machloof, Refael Strugo, Tomer Kaplan, and Shelly Soffer. 2022. "The Impact of Prehospital and Hospital Care on Clinical Outcomes in Out-of-Hospital Cardiac Arrest" Journal of Clinical Medicine 11, no. 22: 6851. https://doi.org/10.3390/jcm11226851
APA StyleDeri, Y., Berzon, B., West, D., Machloof, M., Strugo, R., Kaplan, T., & Soffer, S. (2022). The Impact of Prehospital and Hospital Care on Clinical Outcomes in Out-of-Hospital Cardiac Arrest. Journal of Clinical Medicine, 11(22), 6851. https://doi.org/10.3390/jcm11226851




