Mental Health Well-Being and Attitudes on Mental Health Disorders among Family Physicians during COVID-19 Pandemic: A Connection with Resilience and Healthy Lifestyle
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Survey
2.3. Mental Health Well-Being
2.4. Statistical Analysis
3. Results
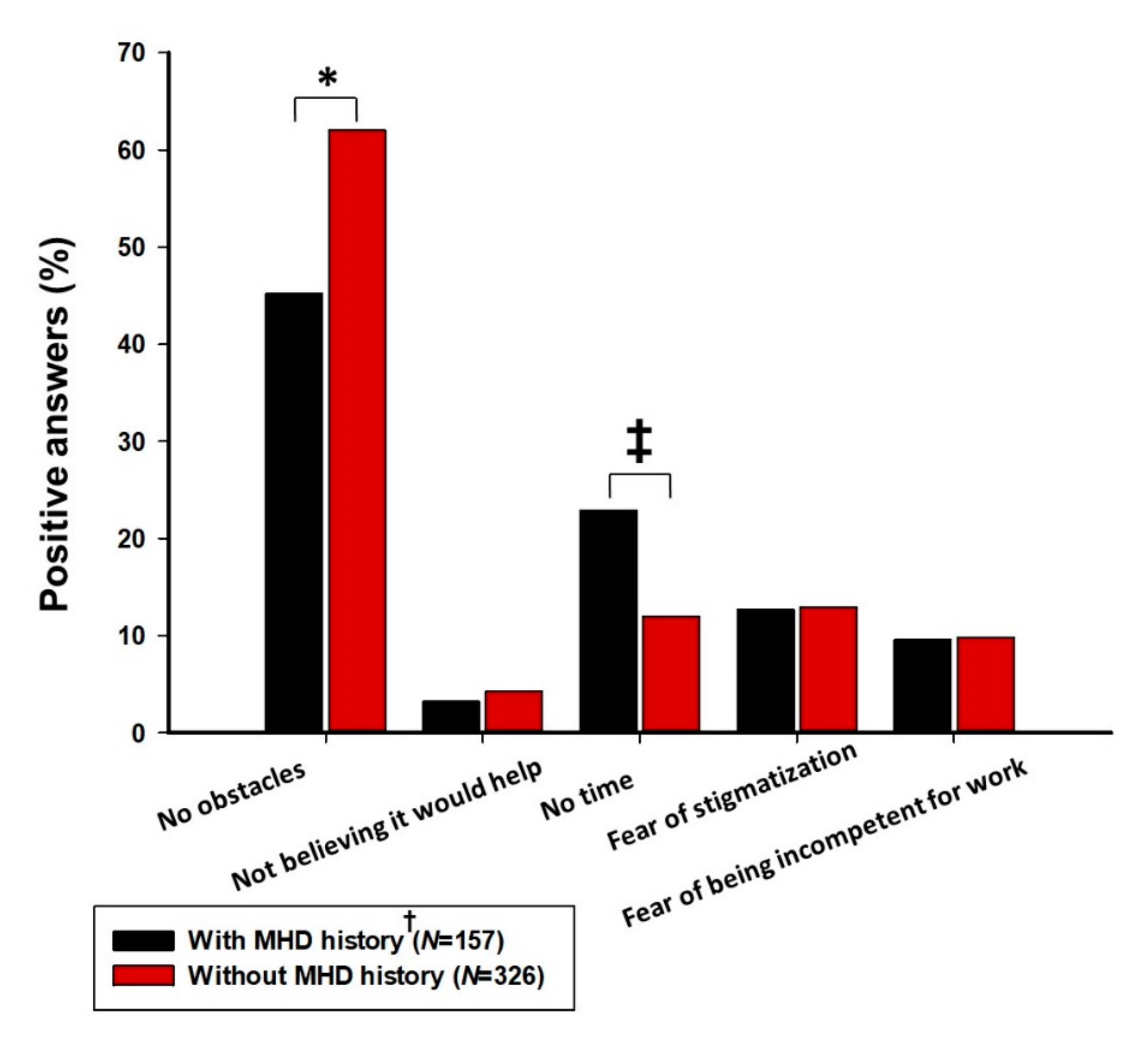
3.1. Baseline Characteristics and Mental Health Experiences and Attitudes
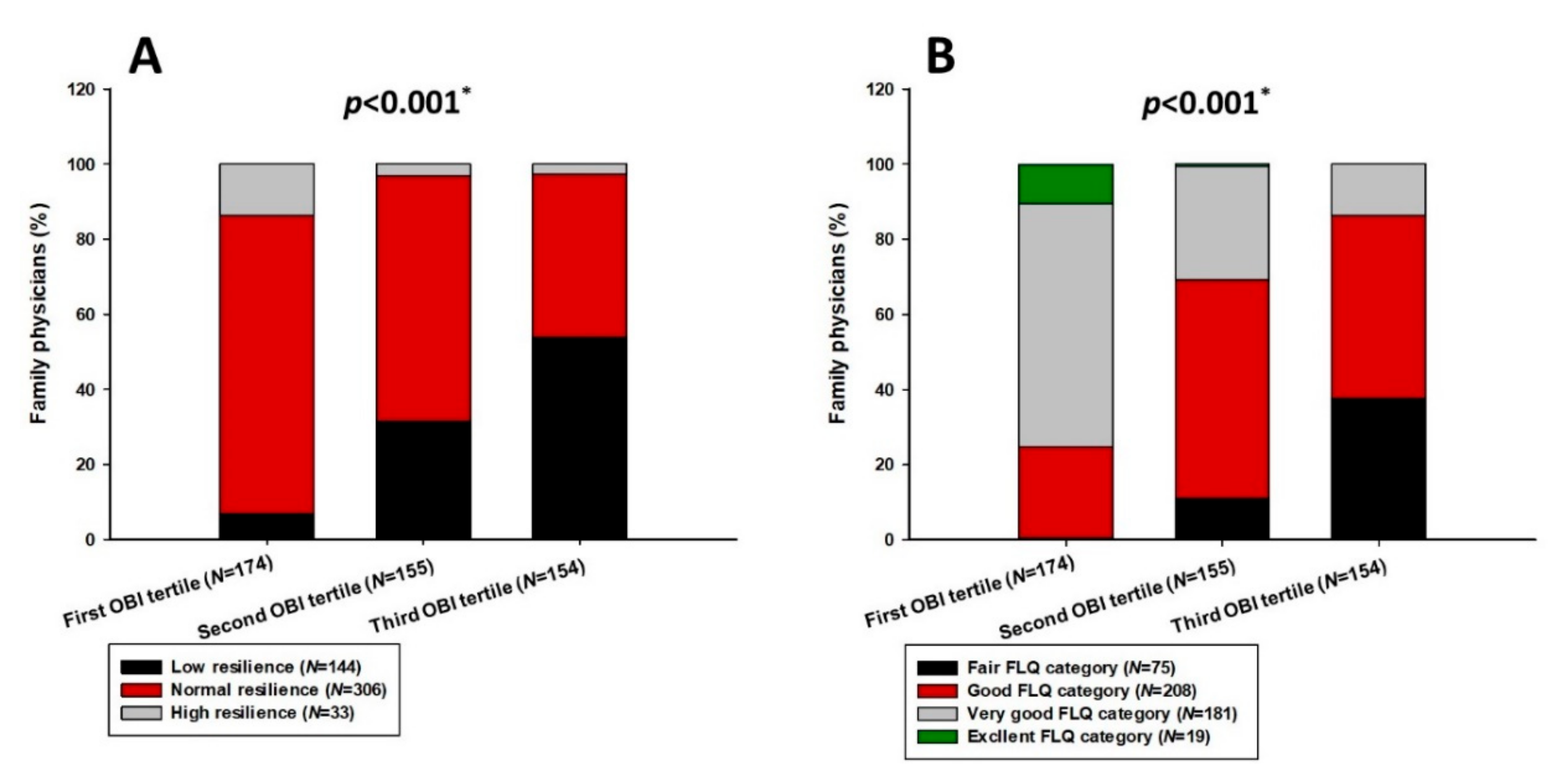
3.2. Stress-Coping Mechanisms and Current Mental Health Well-Being
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thornicroft, G. Most people with mental illness are not treated. Lancet 2007, 370, 807–808. [Google Scholar] [CrossRef]
- Clement, S.; Schauman, O.; Graham, T.; Maggioni, F.; Evans-Lacko, S.; Bezborodovs, N.; Morgan, C.; Rüsch, N.; Brown, J.S.L.; Thornicroft, G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2015, 45, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, C.S.; Erickson, J.; Deane, F.; Wright, M. Changes in attitudes toward seeking mental health services: A 40-year cross-temporal meta-analysis. Clin. Psychol. Rev. 2014, 34, 99–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Velasco, A.A.; Cruz, I.S.S.; Billings, J.; Jimenez, M.; Rowe, S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry 2020, 20, 293. [Google Scholar] [CrossRef]
- Yates, S.W. Physician Stress and Burnout. Am. J. Med. 2020, 133, 160–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mihailescu, M.; Neiterman, E. A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America. BMC Public Health 2019, 19, 1363. [Google Scholar] [CrossRef]
- Hawton, K.; Agerbo, E.; Simkin, S.; Platt, B.; Mellanby, R.J. Risk of suicide in medical and related occupational groups: A national study based on Danish case population-based registers. J. Affect. Disord. 2011, 134, 320–326. [Google Scholar] [CrossRef]
- Knaak, S.; Mantler, E.; Szeto, A. Mental illness-related stigma in healthcare: Barriers to access and care and evidence-based solutions. Heal. Manag. Forum 2017, 30, 111–116. [Google Scholar] [CrossRef] [Green Version]
- Schultz, K.; Delva, D.; Kerr, J. Emotional effects of continuity of care on family physicians and the therapeutic relationship. Can. Fam. Physician 2012, 58, 178–185. [Google Scholar]
- Allen, J.; Gay, B.; Crebolder, H.; Heyrman, J.; Svab, I.; Ram, P. The European definitions of the key features of the discipline of general practice: The role of the GP and core competencies. Br. J. Gen. Pr. 2002, 52, 526–527. [Google Scholar]
- McKinley, N.; McCain, R.S.; Convie, L.; Clarke, M.; Dempster, M.; Campbell, W.J.; Kirk, S.J. Resilience, burnout and coping mechanisms in UK doctors: A cross-sectional study. BMJ Open 2020, 10, e031765. [Google Scholar] [CrossRef] [Green Version]
- Peckham, C. Medscape Physician Lifestyle Report 2016: Bias and Burnout. Medscape, 2016. Available online: https://www.medscape.com/slideshow/lifestyle-2016-overview-6007335 (accessed on 16 November 2021).
- Wallace, J.E.; Lemaire, J.B.; Ghali, W.A. Physician wellness: A missing quality indicator. Lancet 2009, 374, 1714–1721. [Google Scholar] [CrossRef]
- Tawfik, D.S.; Profit, J.; Morgenthaler, T.I.; Satele, D.V.; Sinsky, C.A.; Dyrbye, L.N.; Tutty, M.A.; West, C.P.; Shanafelt, T.D. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherland, 2018; Volume 93, pp. 1571–1580. [Google Scholar]
- Twenge, J.M.; Cooper, A.B.; Joiner, T.E.; Duffy, M.E.; Binau, S.G. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J. Abnorm. Psychol. 2019, 128, 185–199. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Hasan, O.; Dyrbye, L.N.; Sinsky, C.; Satele, D.; Sloan, J.; West, C.P. Changes in Burnout and Satisfaction with Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin. Proc. 2015, 90, 1600–1613. [Google Scholar] [CrossRef] [PubMed]
- Martínez-López, J.Á.; Lázaro-Pérez, C.; Gómez-Galán, J.; Fernández-Martínez, M.D.M. Psychological Impact of COVID-19 Emergency on Health Professionals: Burnout Incidence at the Most Critical Period in Spain. J. Clin. Med. 2020, 9, 3029. [Google Scholar] [CrossRef]
- Vilovic, T.; Bozic, J.; Vilovic, M.; Rusic, D.; Furlan, S.Z.; Rada, M.; Tomicic, M. Family Physicians’ Standpoint and Mental Health Assessment in the Light of COVID-19 Pandemic—A Nationwide Survey Study. Int. J. Environ. Res. Public Heal. 2021, 18, 2093. [Google Scholar] [CrossRef]
- Muller, A.E.; Hafstad, E.V.; Himmels, J.P.W.; Smedslund, G.; Flottorp, S.; Stensland, S.Ø.; Stroobants, S.; Van De Velde, S.; Vist, G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatr. Res. 2020, 293, 113441. [Google Scholar] [CrossRef]
- David, E.; DePierro, J.M.; Marin, D.B.; Sharma, V.; Charney, D.S.; Katz, C.L. COVID-19 Pandemic Support Programs for Healthcare Workers and Implications for Occupational Mental Health: A Narrative Review. Psychiatr. Q. 2021, 1–21. [Google Scholar] [CrossRef]
- Tyssen, R.; Vaglum, P.; Røvik, J.O.; Grønvold, N.T.; Ekeberg, Ø. Help-seeking for mental health problems among young physicians: Is it the most ill that seeks help?—A longitudinal and nationwide study. Soc. Psychiatry 2004, 39, 989–993. [Google Scholar] [CrossRef]
- Gold, K.J.; Andrew, L.B.; Goldman, E.B.; Schwenk, T.L. “I would never want to have a mental health diagnosis on my record”: A survey of female physicians on mental health diagnosis, treatment, and reporting. Gen. Hosp. Psychiatry 2016, 43, 51–57. [Google Scholar] [CrossRef]
- Naito, T.; Chin, J.; Kim, T.U.; Veera, S.; Jeannette, M.; Lomiguen, C.M. Further Reduction in Help-Seeking Behaviors Amidst Additional Barriers to Mental Health Treatment in Asian Populations: A Contemporary Review. Cureus 2020, 12, e11455. [Google Scholar] [CrossRef]
- Liang, S.-W.; Chen, R.-N.; Liu, L.-L.; Li, X.-G.; Chen, J.-B.; Tang, S.-Y.; Zhao, J.-B. The Psychological Impact of the COVID-19 Epidemic on Guangdong College Students: The Difference between Seeking and Not Seeking Psychological Help. Front. Psychol. 2020, 11, 2231. [Google Scholar] [CrossRef] [PubMed]
- She, R.; Wang, X.; Zhang, Z.; Li, J.; Xu, J.; You, H.; Li, Y.; Liang, Y.; Li, S.; Ma, L.; et al. Mental Health Help-Seeking and Associated Factors Among Public Health Workers During the COVID-19 Outbreak in China. Front. Public Health 2021, 9, 622677. [Google Scholar] [CrossRef]
- Smith, M.M.; Saklofske, D.H.; Keefer, K.V.; Tremblay, P.F. Coping Strategies and Psychological Outcomes: The Moderating Effects of Personal Resiliency. J. Psychol. 2016, 150, 318–332. [Google Scholar] [CrossRef] [PubMed]
- Compas, B.E.; Jaser, S.S.; Bettis, A.H.; Watson, K.H.; Gruhn, M.A.; Dunbar, J.P.; Williams, E.; Thigpen, J.C. Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychol. Bull. 2017, 143, 939–991. [Google Scholar] [CrossRef] [PubMed]
- Lianov, L. A Powerful Antidote to Physician Burnout: Intensive Healthy Lifestyle and Positive Psychology Approaches. Am. J. Lifestyle Med. 2021, 15, 563–566. [Google Scholar] [CrossRef]
- Zwack, J.; Schweitzer, J. If Every Fifth Physician Is Affected by Burnout, What About the Other Four? Resilience Strategies of Experienced Physicians. Acad. Med. 2013, 88, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Aburn, G.; Gott, M.; Hoare, K. What is resilience? An Integrative Review of the empirical literature. J. Adv. Nurs. 2016, 72, 980–1000. [Google Scholar] [CrossRef]
- Nedrow, A.; Steckler, A.N.; Hardman, J. Physician resilience and burnout: Can you make the switch? Fam. Pr. Manag. 2013, 20, 25–30. [Google Scholar]
- Mosheva, M.; Hertz-Palmor, N.; Ilan, S.D.; Matalon, N.; Pessach, I.M.; Afek, A.; Ziv, A.; Kreiss, Y.; Gross, R.; Gothelf, D. Anxiety, pandemic-related stress and resilience among physicians during the COVID-19 pandemic. Depress. Anxiety 2020, 37, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Buck, K.; Williamson, M.; Ogbeide, S.; Norberg, B. Family Physician Burnout and Resilience: A Cross-Sectional Analysis. Fam. Med. 2019, 51, 657–663. [Google Scholar] [CrossRef] [Green Version]
- Penttinen, M.; Virtanen, J.; Laaksonen, M.; Erkkola, M.; Vepsäläinen, H.; Kautiainen, H.; Korhonen, P. The Association between Healthy Diet and Burnout Symptoms among Finnish Municipal Employees. Nutrients 2021, 13, 2393. [Google Scholar] [CrossRef] [PubMed]
- Koutsimani, P.; Montgomery, A.; Georganta, K. The Relationship between Burnout, Depression, and Anxiety: A Systematic Review and Meta-Analysis. Front. Psychol. 2019, 10, 284. [Google Scholar] [CrossRef] [Green Version]
- Gómez-García, R.; Bayón-Calvo, S.; Lucas-García, J. The Relationship between Burnout and Job Satisfaction in a Sample of Spanish Social Workers. Br. J. Soc. Work. 2020, 51, 3115–3134. [Google Scholar] [CrossRef]
- Kang, L.; Ma, S.; Chen, M.; Yang, J.; Wang, Y.; Li, R.; Yao, L.; Bai, H.; Cai, Z.; Yang, B.X.; et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 2020, 87, 11–17. [Google Scholar] [CrossRef]
- Louie, P.K.; Harada, G.K.; McCarthy, M.H.; Germscheid, N.; Cheung, J.P.Y.; Neva, M.H.; El-Sharkawi, M.; Valacco, M.; Sciubba, D.M.; Chutkan, N.B.; et al. The Impact of COVID-19 Pandemic on Spine Surgeons Worldwide. Glob. Spine J. 2020, 10, 534–552. [Google Scholar] [CrossRef] [PubMed]
- Shechter, A.; Diaz, F.; Moise, N.; Anstey, D.E.; Ye, S.; Agarwal, S.; Birk, J.L.; Brodie, D.; Cannone, D.E.; Chang, B.; et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry 2020, 66, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Esch, T.; Stefano, G.B. The neurobiology of stress management. Neuro Endocrinol. Lett. 2010, 31, 19–39. [Google Scholar] [PubMed]
- Baqutayan, S.M.S. Stress and Coping Mechanisms: A Historical Overview. Mediterr. J. Soc. Sci. 2015, 6, 479. [Google Scholar] [CrossRef] [Green Version]
- Saxon, L.; Makhashvili, N.; Chikovani, I.; Seguin, M.; McKee, M.; Patel, V.; Bisson, J.; Roberts, B. Coping strategies and mental health outcomes of conflict-affected persons in the Republic of Georgia. Epidemiol. Psychiatr. Sci. 2017, 26, 276–286. [Google Scholar] [CrossRef] [Green Version]
- Tugade, M.M.; Fredrickson, B.L. Resilient Individuals Use Positive Emotions to Bounce Back From Negative Emotional Experiences. J. Pers. Soc. Psychol. 2004, 86, 320–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carver, C.S. Resilience and thriving: Issues, models, and linkages. J. Soc. Issues 1998, 54, 245–266. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Chmitorz, A.; Wenzel, M.; Stieglitz, R.-D.; Kunzler, A.; Bagusat, C.; Helmreich, I.; Gerlicher, A.; Kampa, M.; Kubiak, T.; Kalisch, R.; et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE 2018, 13, e0192761. [Google Scholar] [CrossRef] [Green Version]
- Soer, R.; Dijkstra, M.W.M.C.; Bieleman, H.J.; Stewart, R.E.; Reneman, M.F.; Oosterveld, F.G.J.; Schreurs, K.M.G. Measurement properties and implications of the Brief Resilience Scale in healthy workers. J. Occup. Heal. 2019, 61, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Sliskovic, A.; Buric, I.; Cubela Adoric, V.; Nikolic, M.; Tucak Junakovic, I. Collection of Psychological Scales and Questionnaires, 9th ed.; University of Zadar: Zadar, Croatia, 2018. [Google Scholar]
- Sinclair, V.G.; Wallston, K.A. The Development and Psychometric Evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef]
- Kocalevent, R.-D.; Zenger, M.; Hinz, A.; Klapp, B.; Brähler, E. Resilient coping in the general population: Standardization of the brief resilient coping scale (BRCS). Heal. Qual. Life Outcomes 2017, 15, 251. [Google Scholar] [CrossRef] [PubMed]
- Fung, S.-F. Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample. Int. J. Environ. Res. Public Health 2020, 17, 1265. [Google Scholar] [CrossRef] [Green Version]
- Demerouti, E.; Bakker, A.B. The Oldenburg Burnout Inventory: A good alternative to measure burnout and engagement. In Stress and Burnout in Health Care; Halbesleben, J., Ed.; Nova Sciences: Hauppage, NY, USA, 2008; pp. 65–78. [Google Scholar]
- Bakker, A.B.; Demerouti, E.; Verbeke, W. Using the job demands-resources model to predict burnout and performance. Hum. Resour. Manag. 2004, 43, 83–104. [Google Scholar] [CrossRef] [Green Version]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Morrison, M.; Tay, L.; Diener, E. Subjective Well-Being and National Satisfaction Findings from a Worldwide Survey. Psychol. Sci. 2011, 22, 166–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warr, P.; Cook, J.; Wall, T. Scales for the measurement of some work attitudes and aspects of psychological well-being. J. Occup. Psychol. 1979, 52, 129–148. [Google Scholar] [CrossRef]
- Rout, U.; Cooper, C.; Rout, J. Job stress among british general practitioners: Predictors of job dissatisfaction and mental ill-health. Stress Med. 1996, 12, 155–166. [Google Scholar] [CrossRef]
- Wilson, D.M.C.; Nielsen, E.; Ciliska, N. Lifestyle Assessment: Testing the FANTASTIC Instrument. Can. Fam. Physician 1984, 30, 1863–1866. [Google Scholar]
- CSEF—Canadian Society for Exercise Physiology. The Canadian Physical Activity, Fitness and Lifestyle Appraisal: CSEP’s Guide to Health Active Living, 2nd ed.; CSEF: Ottawa, ON, Canada, 2003. [Google Scholar]
- Machul, M.; Bieniak, M.; Chałdaś-Majdańska, J.; Bąk, J.; Chrzan-Rodak, A.; Mazurek, P.; Pawłowski, P.; Makuch-Kuśmierz, D.; Obuchowska, A.; Bartoszek, A.; et al. Lifestyle Practices, Satisfaction with Life and the Level of Perceived Stress of Polish and Foreign Medical Students Studying in Poland. Int. J. Environ. Res. Public Health 2020, 17, 4445. [Google Scholar] [CrossRef]
- Smallwood, N.; Karimi, L.; Pascoe, A.; Bismark, M.; Putland, M.; Johnson, D.; Dharmage, S.C.; Barson, E.; Atkin, N.; Long, C.; et al. Coping strategies adopted by Australian frontline health workers to address psychological distress during the COVID-19 pandemic. Gen. Hosp. Psychiatry 2021, 72, 124–130. [Google Scholar] [CrossRef]
- Cai, Q.; Feng, H.; Huang, J.; Wang, M.; Wang, Q.; Lu, X.; Xie, Y.; Wang, X.; Liu, Z.; Hou, B.; et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. J. Affect. Disord. 2020, 275, 210–215. [Google Scholar] [CrossRef]
- Ramzi, N.S.A.; Deady, M.; Petrie, K.; Crawford, J.; Harvey, S.B. Help-seeking for depression among Australian doctors. Intern. Med. J. 2020, 51, 2069–2077. [Google Scholar] [CrossRef]
- Montgomery, A.J.; Bradley, C.; Rochfort, A.; Panagopoulou, E. A review of self-medication in physicians and medical students. Occup. Med. 2011, 61, 490–497. [Google Scholar] [CrossRef] [Green Version]
- Lee, E.; Jeong, Y.M.; Yi, S.J. Nurses’ Attitudes toward Psychiatric Help for Depression: The Serial Mediation Effect of Self-Stigma and Depression on Public Stigma and Attitudes toward Psychiatric Help. Int. J. Environ. Res. Public Health 2020, 17, 5073. [Google Scholar] [CrossRef]
- Brown, S.P.; Westbrook, R.A.; Challagalla, G. Good Cope, Bad Cope: Adaptive and Maladaptive Coping Strategies Following a Critical Negative Work Event. J. Appl. Psychol. 2005, 90, 792–798. [Google Scholar] [CrossRef]
- Nutley, S.K.; Falise, A.M.; Henderson, R.; Apostolou, V.; Mathews, A.C.; Striley, C.W. Impact of the COVID-19 Pandemic on Disordered Eating Behavior: Qualitative Analysis of Social Media Posts. JMIR Ment. Health 2021, 8, e26011. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, P. Perceived stress and psychological distress among chinese physicians: The mediating role of coping style. Medicine 2019, 98, e15950. [Google Scholar] [CrossRef] [PubMed]
- Krok, D.; Zarzycka, B. Risk Perception of COVID-19, Meaning-Based Resources and Psychological Well-Being amongst Healthcare Personnel: The Mediating Role of Coping. J. Clin. Med. 2020, 9, 3225. [Google Scholar] [CrossRef]
- Cooke, E.G.P.; Doust, A.J.; Steele, M.C. A survey of resilience, burnout, and tolerance of uncertainty in Australian general practice registrars. BMC Med. Educ. 2013, 13, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, Y.-F.; Luo, Y.-H.; Lam, L.L.Y.; Cross, W.; Plummer, V.; Zhang, J.-P. Burnout and its association with resilience in nurses: A cross-sectional study. J. Clin. Nurs. 2018, 27, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Walsh, K. An Economic Argument for Investment in Physician Resilience. Acad. Med. 2013, 88, 1196. [Google Scholar] [CrossRef]
- Kunzler, A.M.; Helmreich, I.; Chmitorz, A.; König, J.; Binder, H.; Wessa, M.; Lieb, K. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst. Rev. 2020, 2020, CD012527. [Google Scholar] [CrossRef]
- La Torre, G.; Raffone, A.; Peruzzo, M.; Calabrese, L.; Cocchiara, R.A.; D’Egidio, V.; Leggieri, P.F.; Dorelli, B.; Zaffina, S.; Mannocci, A.; et al. Yoga and Mindfulness as a Tool for Influencing Affectivity, Anxiety, Mental Health, and Stress among Healthcare Workers: Results of a Single-Arm Clinical Trial. J. Clin. Med. 2020, 9, 1037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Parameter | with MHD History † (N = 157) | without MHD History (N = 326) | Total (N = 483) | p * |
|---|---|---|---|---|
| Women | 133 (84.7) | 265 (81.3) | 398 (82.4) | 0.355 |
| Age (years) | 48.0 (33.0–58.0) | 46.5 (33.0–58.0) | 47.0 (33.0–58.0) | 0.992 ‡ |
| Work experience (years) | 20.0 (5.0–30.0) | 13.0 (6.0–28.0) | 15.0 (6.0–30.0) | 0.842 ‡ |
| Occupation | ||||
| Family physician | 132 (84.1) | 256 (78.5) | 388 (80.3) | 0.151 |
| Family medicine resident | 25 (15.9) | 70 (21.5) | 95 (19.7) | |
| Region of work | ||||
| Adriatic region | 62 (39.5) | 144 (44.2) | 206 (42.7) | 0.579 |
| North-West region | 38 (24.2) | 77 (23.6) | 115 (23.8) | |
| Central and East region | 57 (36.3) | 105 (32.2) | 162 (33.5) | |
| Practice localization | ||||
| Urban area | 104 (66.2) | 225 (69.0) | 329 (68.1) | 0.540 |
| Rural area/islands | 53 (33.8) | 101 (31.0) | 154 (33.8) | |
| Patients in practice | ||||
| <1000 | 7 (4.5) | 21 (6.4) | 28 (5.8) | 0.311 |
| 1000–1500 | 40 (25.5) | 90 (27.6) | 130 (26.9) | |
| 1500–2000 | 73 (46.5) | 126 (38.7) | 199 (41.2) | |
| >2000 | 30 (19.1) | 80 (24.5) | 110 (22.8) | |
| Not answered | 7 (4.5) | 9 (2.8) | 16 (3.3) | |
| Family history of MHD | 84 (53.5) | 77 (23.6) | 161 (33.3) | <0.001 |
| Increased COVID-19 risk § | 74 (47.1) | 109 (33.4) | 183 (37.9) | 0.004 |
| Recovered from COVID-19 | 38 (24.2) | 87 (26.7) | 125 (25.9) | 0.559 |
| Parameter | with MHD History † (N = 157) | without MHD History (N = 326) | Total (N = 483) | p * |
|---|---|---|---|---|
| Actions regarding knowledge of MHD ‡ | ||||
| Taking medication | 95 (60.5) | 151 (46.3) | 246 (50.9) | 0.003 |
| Going to psychotherapies | 41 (26.1) | 108 (33.1) | 149 (30.8) | 0.118 |
| Consultation with psychiatrist | 47 (29.9) | 144 (44.2) | 191 (39.5) | 0.003 |
| Trying to solve the problem alone | 85 (54.1) | 165 (50.6) | 250 (51.8) | 0.468 |
| Ignore the problem | 7 (4.5) | 2 (0.6) | 9 (1.9) | 0.006 |
| Talking with colleagues about it | 0 (0.0) | 5 (1.5) | 5 (1.0) | 0.179 |
| Best thing to acutely tackle mental health state | ||||
| Psychiatrist consultation | 38 (24.2) | 18 (5.5) | 56 (11.6) | <0.001 |
| Help not needed | 9 (5.7) | 69 (21.2) | 78 (16.1) | <0.001 |
| Long vacation | 96 (61.1) | 216 (66.3) | 312 (64.6) | 0.272 |
| Self-help seminars | 27 (17.2) | 38 (11.7) | 65 (13.5) | 0.095 |
| Something else | 9 (5.7) | 12 (3.7) | 21 (4.3) | 0.301 |
| Parameter | with MHD History † (N = 157) | without MHD History (N = 326) | Total (N = 483) | p * |
|---|---|---|---|---|
| Working out | 62 (39.5) | 162 (49.7) | 224 (46.4) | 0.035 |
| Listening to music | 61 (38.9) | 136 (41.7) | 197 (40.8) | 0.549 |
| Smoking | 21 (13.4) | 35 (10.7) | 56 (11.6) | 0.396 |
| Drinking alcoholic drinks | 17 (10.8) | 16 (4.9) | 31 (6.4) | 0.016 |
| Spending time with family | 61 (38.9) | 173 (53.1) | 234 (48.4) | 0.003 |
| Working on business projects | 7 (4.5) | 18 (5.5) | 25 (5.2) | 0.621 |
| Religious/Spiritual activities | 22 (14.0) | 44 (13.5) | 66 (13.7) | 0.877 |
| Reading | 47 (29.9) | 108 (33.1) | 155 (32.1) | 0.482 |
| Watching television | 69 (43.9) | 111 (34.0) | 180 (37.3) | 0.035 |
| Communication with friends | 40 (25.5) | 78 (23.9) | 118 (24.4) | 0.710 |
| Eating food | 57 (36.3) | 65 (19.9) | 122 (25.3) | <0.001 |
| Parameter | with MHD History † (N = 157) | without MHD History (N = 326) | Total (N = 483) | p * |
|---|---|---|---|---|
| BRCS score | 15.0 (12.0–16.0) | 16.0 (14.0–17.0) | 15.0 (14.0–17.0) | <0.001 |
| BRS score | 2.83 (2.33–3.5) | 3.33 (3.0–3.83) | 3.33 (2.83–3.79) | <0.001 |
| FLQ score | 61.0 (51.0–71.0) | 68.0 (62.0–77.0) | 68.0 (59.0–75.0) | <0.001 |
| OBI exhaustion | 23.0 (20.0–26.0) | 21.0 (18.0–24.0) | 21.0 (19.0–25.0) | <0.001 |
| OBI disengagement | 21.0 (18.0–23.0) | 19.0 (17.0–21.0) | 19.0 (17.0–21.0) | <0.001 |
| OBI total | 44.0 (40.0–49.2) | 40.0 (35.0–44.0) | 41.0 (36.0–46.0) | <0.001 |
| SWLS score | 22.0 (16.0–26.0) | 26.0 (22.0–30.0) | 25.0 (19.0–29.0) | <0.001 |
| WCW-JSS score | 43.0 (36.7–50.0) | 48.0 (40.0–55.0) | 47.0 (39.2–54.0) | <0.001 |
| Parameter | 1. Tertile (N = 174) | 2. Tertile (N = 155) | 3. Tertile (N = 154) | p * |
|---|---|---|---|---|
| Age (years) | 41.0 (33.0–57.0) | 46.0 (33.0–58.0) | 50.0 (39.0–58.0) | 0.041 ‡ |
| Women | 131 (75.3) | 131 (84.5) | 136 (88.3) | 0.006 |
| With MHD history † | 35 (20.1) | 49 (31.6) | 73 (47.4) | <0.001 |
| Increased COVID-19 risk § | 43 (24.7) | 66 (42.6) | 74 (48.1) | <0.001 |
| Practice localization | ||||
| Urban area | 119 (68.4) | 95 (61.3) | 115 (74.7) | 0.041 |
| Rural area/islands | 55 (31.6) | 60 (38.7) | 39 (25.3) | |
| Occupation | ||||
| Family physician | 136 (78.2) | 115 (74.2) | 137 (89.0) | 0.003 |
| Family medicine resident | 38 (21.8) | 40 (25.8) | 17 (11.0) | |
| BRCS categories | ||||
| Low resilient coping | 17 (9.8) | 36 (23.2) | 55 (35.7) | <0.001 |
| Medium resilient coping | 83 (47.7) | 88 (56.8) | 82 (53.2) | |
| High resilient coping | 74 (42.5) | 31 (20.0) | 17 (11.0) | |
| SWLS categories | ||||
| Dissatisfied/Extremely dissatisfied | 8 (4.6) | 16 (10.3) | 38 (24.7) | <0.001 |
| Average/Slightly below average | 31 (17.8) | 61 (39.4) | 70 (45.5) | |
| Satisfied/Highly satisfied | 135 (77.6) | 78 (50.3) | 46 (29.9) | |
| Selected coping mechanisms | ||||
| Eating food | 31 (17.8) | 45 (29.0) | 46 (29.9) | 0.018 |
| Smoking | 12 (6.9) | 21 (13.5) | 23 (14.9) | 0.049 |
| Watching television | 53 (30.5) | 59 (38.1) | 68 (44.2) | 0.036 |
| Spending time with family | 102 (58.6) | 75 (48.4) | 57 (37.0) | <0.001 |
| Working out | 90 (51.7) | 64 (41.3) | 72 (46.8) | 0.166 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vilovic, T.; Bozic, J.; Zuzic Furlan, S.; Vilovic, M.; Kumric, M.; Martinovic, D.; Rusic, D.; Rada, M.; Tomicic, M. Mental Health Well-Being and Attitudes on Mental Health Disorders among Family Physicians during COVID-19 Pandemic: A Connection with Resilience and Healthy Lifestyle. J. Clin. Med. 2022, 11, 438. https://doi.org/10.3390/jcm11020438
Vilovic T, Bozic J, Zuzic Furlan S, Vilovic M, Kumric M, Martinovic D, Rusic D, Rada M, Tomicic M. Mental Health Well-Being and Attitudes on Mental Health Disorders among Family Physicians during COVID-19 Pandemic: A Connection with Resilience and Healthy Lifestyle. Journal of Clinical Medicine. 2022; 11(2):438. https://doi.org/10.3390/jcm11020438
Chicago/Turabian StyleVilovic, Tina, Josko Bozic, Sanja Zuzic Furlan, Marino Vilovic, Marko Kumric, Dinko Martinovic, Doris Rusic, Marko Rada, and Marion Tomicic. 2022. "Mental Health Well-Being and Attitudes on Mental Health Disorders among Family Physicians during COVID-19 Pandemic: A Connection with Resilience and Healthy Lifestyle" Journal of Clinical Medicine 11, no. 2: 438. https://doi.org/10.3390/jcm11020438
APA StyleVilovic, T., Bozic, J., Zuzic Furlan, S., Vilovic, M., Kumric, M., Martinovic, D., Rusic, D., Rada, M., & Tomicic, M. (2022). Mental Health Well-Being and Attitudes on Mental Health Disorders among Family Physicians during COVID-19 Pandemic: A Connection with Resilience and Healthy Lifestyle. Journal of Clinical Medicine, 11(2), 438. https://doi.org/10.3390/jcm11020438









