5-Year Clinical and Radiographic Results of the Direct Anterior Approach for Total Hip Arthroplasty Using a Collared Cementless Femoral Short-Stem Prosthesis
Abstract
:1. Introduction
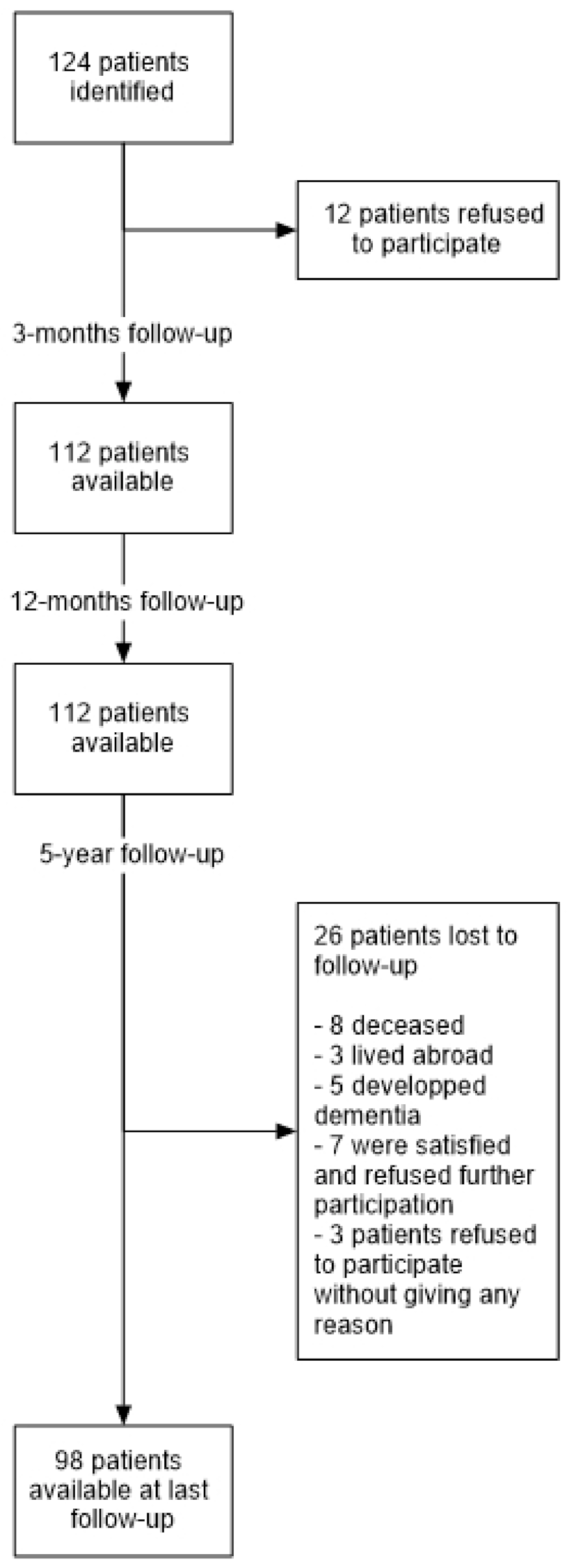
2. Materials and Methods
2.1. Ethics Approval
2.2. Statistical Analysis
3. Results
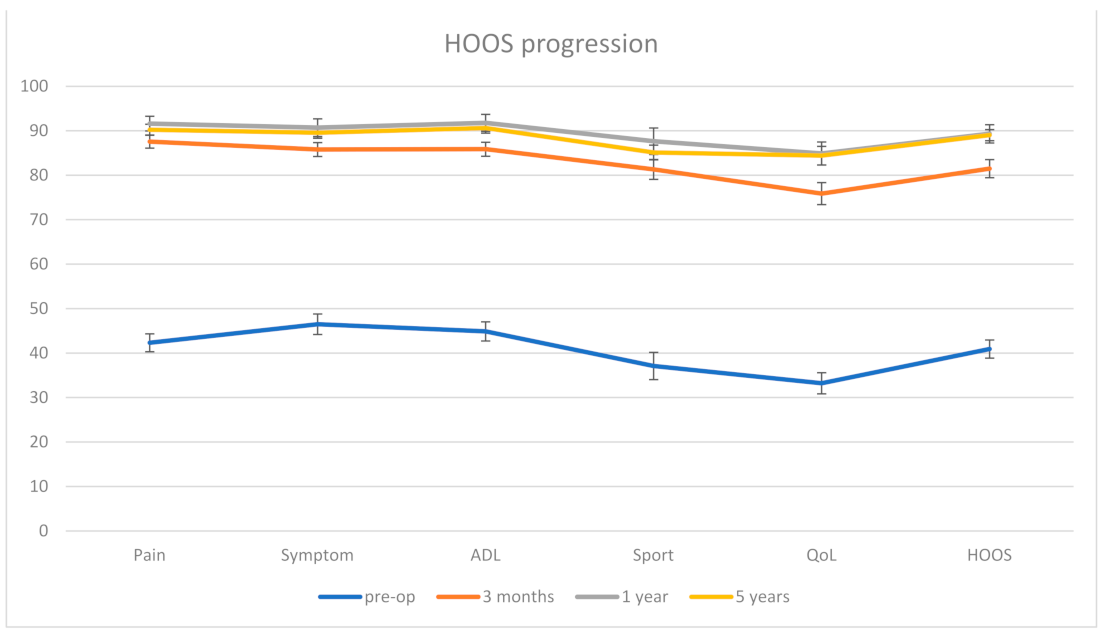
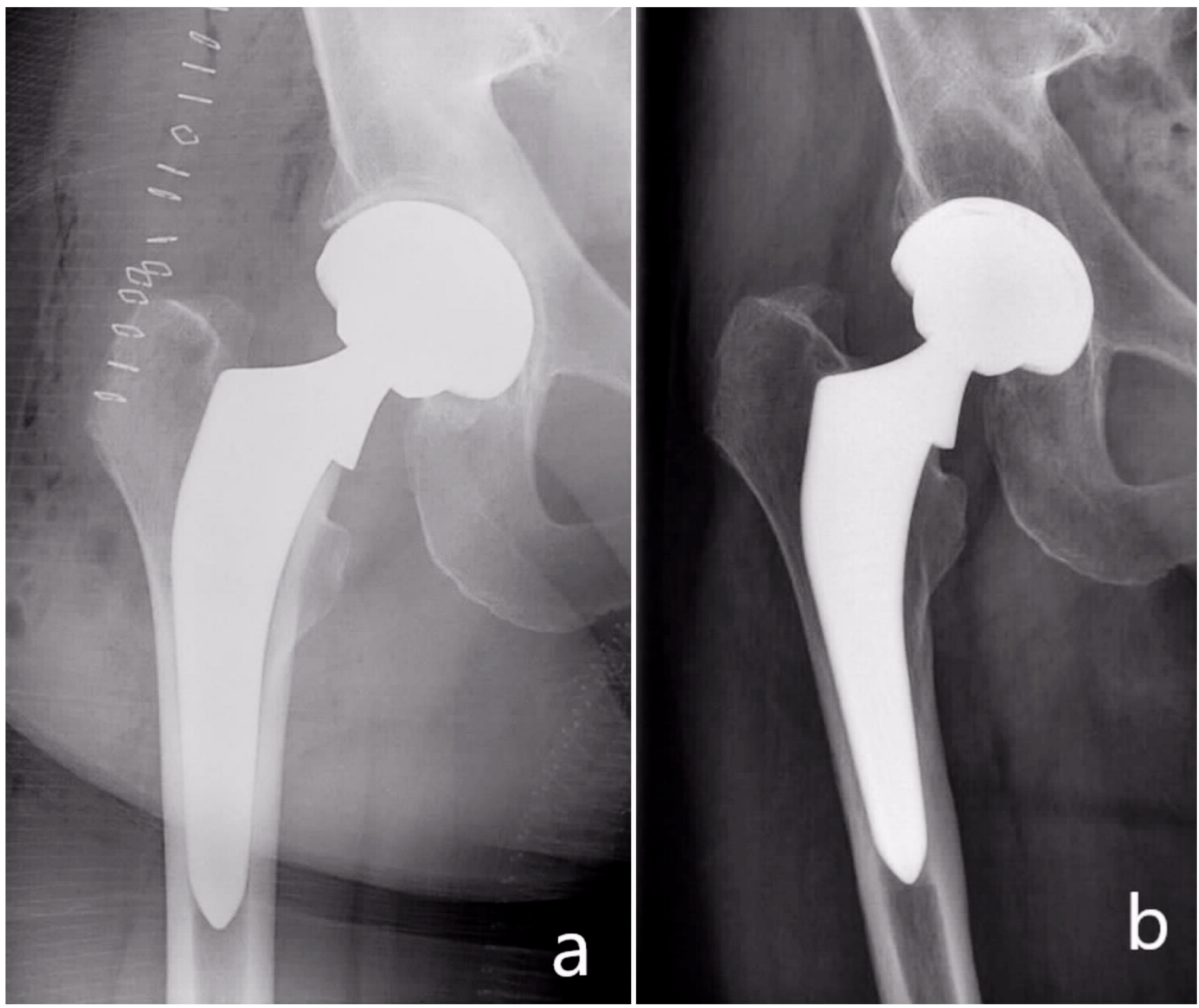
Clinical and Radiological Outcome
4. Discussion
4.1. Revision Rates
4.2. Radiological Outcome
4.3. Subsidence
4.4. Periprosthetic Fracture
4.5. Clinical Outcome
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Putananon, C.; Tuchinda, H.; Arirachakaran, A.; Wongsak, S.; Narinsorasak, T.; Kongtharvonskul, J. Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: Network meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 255–267. [Google Scholar] [CrossRef]
- Yue, C.; Kang, P.; Pei, F. Comparison of Direct Anterior and Lateral Approaches in Total Hip Arthroplasty: A Systematic Review and Meta-Analysis (PRISMA). Medicine 2015, 94, e2126. [Google Scholar] [CrossRef]
- Barrett, W.P.; Turner, S.E.; Leopold, J.P. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J. Arthroplast. 2013, 28, 1634–1638. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.M.; Vaughn, J.J.; Ritterman, S.A.; Eisenson, D.L.; Rubin, L.E. Intraoperative Femur Fracture Risk During Primary Direct Anterior Approach Cementless Total Hip Arthroplasty With and Without a Fracture Table. J. Arthroplast. 2017, 32, 2847–2851. [Google Scholar] [CrossRef] [PubMed]
- Panichkul, P.; Bavonratanavech, S.; Arirachakaran, A.; Kongtharvonskul, J. Comparative outcomes between collared versus collarless and short versus long stem of direct anterior approach total hip arthroplasty: A systematic review and indirect meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 1693–1704. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Lau, E.; Baykal, D.; Odum, S.M.; Springer, B.D.; Fehring, T.K. Are Ceramic Bearings Becoming Cost-Effective for All Patients Within a 90-Day Bundled Payment Period? J. Arthroplast. 2019, 34, 1082–1088. [Google Scholar] [CrossRef]
- Su, E.P. Ceramic-Ceramic Bearing: Too Unpredictable to Use it Regularly. HSS J. 2012, 8, 287–290. [Google Scholar] [CrossRef] [Green Version]
- Dorr, L.D.; Faugere, M.C.; Mackel, A.M.; Gruen, T.A.; Bognar, B.; Malluche, H.H. Structural and cellular assessment of bone quality of proximal femur. Bone 1993, 14, 231–242. [Google Scholar] [CrossRef]
- Gruen, T.A.; McNeice, G.M.; Amstutz, H.C. “Modes of failure” of cemented stem-type femoral components: A radiographic analysis of loosening. Clin. Orthop. Relat. Res. 1979, 141, 17–27. [Google Scholar] [CrossRef]
- Smith, T.O.; Williams, T.H.; Samuel, A.; Ogonda, L.; Wimhurst, J.A. Reliability of the radiological assessments of radiolucency and loosening in total hip arthroplasty using PACS. HIP Int. 2011, 21, 577–582. [Google Scholar] [CrossRef]
- Johnston, R.C.; Fitzgerald, R.H., Jr.; Harris, W.H.; Poss, R.; Müller, M.E.; Sledge, C.B. Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J. Bone Jt. Surg. Am. 1990, 72, 161–168. [Google Scholar] [CrossRef]
- Mushtaq, N.; To, K.; Gooding, C.; Khan, W. Radiological Imaging Evaluation of the Failing Total Hip Replacement. Front. Surg. 2019, 6, 35. [Google Scholar] [CrossRef]
- Brand, R.A.; Pedersen, D.R.; Yoder, S.A. How definition of “loosening” affects the incidence of loose total hip reconstructions. Clin. Orthop. Relat. Res. 1986, 210, 185–191. [Google Scholar] [CrossRef]
- Jacobs, C.A.; Christensen, C.P. Progressive subsidence of a tapered, proximally coated femoral stem in total hip arthroplasty. Int. Orthop. 2009, 33, 917–922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nilsdotter, A.K.; Lohmander, L.S.; Klässbo, M.; Roos, E.M. Hip disability and osteoarthritis outcome score (HOOS)—validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 2003, 4, 10. [Google Scholar] [CrossRef] [Green Version]
- Ornetti, P.; Parratte, S.; Gossec, L.; Tavernier, C.; Argenson, J.N.; Roos, E.M.; Guillemin, F.; Maillefert, J.F. Cross-cultural adaptation and validation of the French version of the Hip disability and Osteoarthritis Outcome Score (HOOS) in hip osteoarthritis patients. Osteoarthr. Cartil. 2010, 18, 522–529. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, E.L.; Meier, P. Nonparametric Estimation from Incomplete Observations. J. Am. Stat. Assoc. 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Hagel, A.; Hein, W.; Wohlrab, D. Experience with the Mayo conservative hip system. Acta Chir. Orthop. Traumatol. Cech. 2008, 75, 288–292. [Google Scholar] [PubMed]
- Falez, F.; Casella, F.; Panegrossi, G.; Favetti, F.; Barresi, C. Perspectives on metaphyseal conservative stems. J. Orthop. Traumatol. 2008, 9, 49–54. [Google Scholar] [CrossRef] [Green Version]
- Goebel, D.; Schultz, W. The Mayo cementless femoral component in active patients with osteoarthritis. HIP Int. 2009, 19, 206–210. [Google Scholar] [CrossRef] [Green Version]
- Morrey, B.F.; Adams, R.A.; Kessler, M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J. Bone Jt. Surg. Br. 2000, 82, 952–958. [Google Scholar] [CrossRef]
- Hallan, G.; Lie, S.A.; Havelin, L.I. High wear rates and extensive osteolysis in 3 types of uncemented total hip arthroplasty: A review of the PCA, the Harris Galante and the Profile/Tri-Lock Plus arthroplasties with a minimum of 12 years median follow-up in 96 hips. Acta Orthop. 2006, 77, 575–584. [Google Scholar] [CrossRef]
- Heaven, S.; Perelgut, M.; Vasarhelyi, E.; Howard, J.; Teeter, M.; Lanting, B. Fully hydroxyapatite-coated collared femoral stems in direct anterior versus direct lateral hip arthroplastyFully hydroxyapatite-coated collared femoral stems in direct anterior versus direct lateral hip arthroplasty. Can. J. Surg. 2021, 64, E205–E210. [Google Scholar] [CrossRef]
- Chitnis, A.S.; Mantel, J.; Ruppenkamp, J.; Bourcet, A.; Holy, C.E. Survival analysis for all-cause revision following primary total hip arthroplasty with a medial collared, triple-tapered primary hip stem versus other implants in real-world settings. Curr. Med. Res. Opin. 2020, 36, 1839–1845. [Google Scholar] [CrossRef] [PubMed]
- Australian Orthopaedic Association National Joint Replacement Register Annual Report 2017; AOANJRR: Adelaide, SA, Australia, 2017.
- Melloh, M.; Eggli, S.; Busato, A.; Roder, C. Predictors of early stem loosening after total hip arthroplasty: A case-control study. J. Orthop. Surg. 2011, 19, 269–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grübl, A.; Chiari, C.; Gruber, M.; Kaider, A.; Gottsauner-Wolf, F. Cementless total hip arthroplasty with a tapered, rectangular titanium stem and a threaded cup: A minimum ten-year follow-up. J. Bone Joint. Surg. Am. 2002, 84, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Delaunay, C. Effect of hydroxyapatite coating on the radio-clinical results of a grit-blasted titanium alloy femoral taper. A case-control study of 198 cementless primary total hip arthroplasty with the Alloclassic™ system. Orthop. Traumatol. Surg. Res. 2014, 100, 739–744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wick, M.; Lester, D.K. Radiological changes in second- and third-generation Zweymüller stems. J. Bone Joint. Surg. Br. 2004, 86, 1108–1114. [Google Scholar] [CrossRef] [Green Version]
- Kutzner, K.P.; Pfeil, D.; Kovacevic, M.P.; Rehbein, P.; Mai, S.; Siebert, W.; Pfeil, J. Radiographic alterations in short-stem total hip arthroplasty: A 2-year follow-up study of 216 cases. HIP Int. 2016, 26, 278–283. [Google Scholar] [CrossRef]
- Zweymüller, K. 20 Years of Cementless Hip Prostheses. In 20 Years of Zweymüller Hip Endoprosthesis; Zweymüller, K., Ed.; Huber: Bern, Switzerland, 2002; pp. 11–23. [Google Scholar]
- Munzinger, U.K.; Boldt, J.G.; Guggi, T. The Cementless Zweymüller Stem in Total Hiparthroplasty: Long-Term Study with a 13-18 Year Follow-up. In 20 Years of Zweymüller Hip Endoprosthesis; Zweymüller, K., Ed.; Huber: Bern, Switzerland, 2002; pp. 8–25. [Google Scholar]
- Lester, D.K. Cross-section radiographic analysis of 10 retrieved titanium alloy press-fit femoral endoprostheses. J. Arthroplast. 1997, 12, 930–937. [Google Scholar] [CrossRef]
- Böhm, G.; Lintner, F.; Auterith, A.; Lester, D.K.; Zweymüller, K.A. Morphometric examination of straight, tapered titanium stems: A retrieval study. Clin. Orthop. Relat. Res. 2001, 393, 13–24. [Google Scholar] [CrossRef]
- Streit, M.R.; Haeussler, D.; Bruckner, T.; Proctor, T.; Innmann, M.M.; Merle, C.; Gotterbarm, T.; Weiss, S. Early Migration Predicts Aseptic Loosening of Cementless Femoral Stems: A Long-term Study. Clin. Orthop. Relat. Res. 2016, 474, 1697–1706. [Google Scholar] [CrossRef] [PubMed]
- Australian Orthopaedic Association National Joint Replacement Register Annual Report 2019; AOANJRR: Adelaide, SA, Australia, 2019.
- National Joint Registry for England; Wales; Northern Ireland and the Isle of Man. National Joint Registry—Annual Report; National Joint Registry: Hertfordshire, UK, 2019.
- Vidalain, J.P. Twenty-year results of the cementless Corail stem. Int. Orthop. 2011, 35, 189–194. [Google Scholar] [CrossRef] [Green Version]
- Al-Najjim, M.; Khattak, U.; Sim, J.; Chambers, I. Differences in subsidence rate between alternative designs of a commonly used uncemented femoral stem. J. Orthop. 2016, 13, 322–326. [Google Scholar] [CrossRef] [Green Version]
- Syed, F.; Hussein, A.; Katam, K.; Saunders, P.; Young, S.K.; Faisal, M. Risk of subsidence and peri-prosthetic fractures using collared hydroxyapatite-coated stem for hip arthroplasty in the elderly. HIP Int. 2018, 28, 663–667. [Google Scholar] [CrossRef]
- Faisal, M.; Thomas, G.; Young, S.K. Subsidence of the Corail femoral component in the elderly. A retrospective radiological review. HIP Int. 2011, 21, 325–329. [Google Scholar] [CrossRef]
- Ries, C.; Boese, C.K.; Dietrich, F.; Miehlke, W.; Heisel, C. Femoral stem subsidence in cementless total hip arthroplasty: A retrospective single-centre study. Int. Orthop. 2019, 43, 307–314. [Google Scholar] [CrossRef]
- Attenello, J.; Chan, S.; Naito, K.; Saruwatari, M.; Saito, S.; Andrews, S.; Nakasone, C. Early perioperative complication rates and subsidence with the Tribute® short cementless, tapered stem in primary total hip arthroplasty. J. Orthop. 2019, 16, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Ulivi, M.; Orlandini, L.C.; Meroni, V.; Lombardo, M.D.M.; Peretti, G.M. Clinical Performance, Patient Reported Outcome, and Radiological Results of a Short, Tapered, Porous, Proximally Coated Cementless Femoral Stem: Results up to Seven Years of Follow-Up. J. Arthroplast. 2018, 33, 1133–1138. [Google Scholar] [CrossRef] [PubMed]
- Garavaglia, G.; Gonzalez, A.; Barea, C.; Peter, R.; Hoffmeyer, P.; Lübbeke, A.; Hannouche, D. Short stem total hip arthroplasty with the direct anterior approach demonstrates suboptimal fixation. Int. Orthop. 2021, 45, 575–583. [Google Scholar] [CrossRef]
- Bonin, N.; Gedouin, J.E.; Pibarot, V.; Bejui-Hughues, J.; Bothorel, H.; Saffarini, M.; Batailler, C. Proximal femoral anatomy and collared stems in hip arthroplasty: Is a single collar size sufficient? J. Exp. Orthop. 2017, 4, 32. [Google Scholar] [CrossRef] [Green Version]
- Malfroy Camine, V.; Rüdiger, H.A.; Pioletti, D.P.; Terrier, A. Effect of a collar on subsidence and local micromotion of cementless femoral stems: In vitro comparative study based on micro-computerised tomography. Int. Orthop. 2018, 42, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Whiteside, L.A.; Amador, D.; Russell, K. The effects of the collar on total hip femoral component subsidence. Clin. Orthop. Relat. Res. 1988, 231, 120–126. [Google Scholar] [CrossRef]
- Cidambi, K.R.; Barnett, S.L.; Mallette, P.R.; Patel, J.J.; Nassif, N.A.; Gorab, R.S. Impact of Femoral Stem Design on Failure After Anterior Approach Total Hip Arthroplasty. J. Arthroplast. 2018, 33, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, M.; Kabelitz, M.; Dora, C.; Zingg, P.O. Perioperative Fractures in Cementless Total Hip Arthroplasty Using the Direct Anterior Minimally Invasive Approach: Reduced Risk With Short Stems. J. Arthroplast. 2018, 33, 548–554. [Google Scholar] [CrossRef]
- Lee, G.C.; Marconi, D. Complications Following Direct Anterior Hip Procedures: Costs to Both Patients and Surgeons. J. Arthroplast. 2015, 30, 98–101. [Google Scholar] [CrossRef]
- Clauss, M.; Van Der Straeten, C.; Goossens, M. Prospective five-year subsidence analysis of a cementless fully hydroxyapatite-coated femoral hip arthroplasty component. HIP Int. 2014, 24, 91–97. [Google Scholar] [CrossRef] [Green Version]
- Darwich, A.; Schüttler, V.; Obertacke, U.; Jawhar, A. Outcome Measures to Evaluate Upper and Lower Extremity: Which Scores are Valid? Z. Orthop. Unf. 2020, 158, 90–103. [Google Scholar] [CrossRef]
- Sagers, K.M.; Creech, J.D.; Shields, J.S.; Pollock, D.C.; Langfitt, M.K.; Plate, J.F. Removing Well-Fixed, Collared and Noncollared Tapered Hip Stems Without an Extended Trochanteric Osteotomy Using a Novel Stem Removal System. Arthroplast. Today 2021, 11, 146–150. [Google Scholar] [CrossRef]


| Sex n (%) | Males | 72 (58%) |
| Females | 52 (42%) | |
| Dorr Classification [8] n (%) | Type A | 39 (29%) |
| Type B | 85 (63%) | |
| Type C | 11 (8%) | |
| Age at Time of Surgery (mean ± SD (range)) | 67.7 ± 11.3 years (range 39–88 years) | |
| BMI * at Time of Surgery (mean ± SD (range)) | 27.4 ± 4.4 kg/m2 (range 17.4–41.8 kg/m2) | |
| Implant Details | Number of Hips n (%) | |
|---|---|---|
| AMIStem® size | 0–2 3–5 6–7 | 46 (34%) 79 (59%) 10 (7%) |
| Head diameter (mm) | 28 32 36 | 46 (34%) 81 (60%) 8 (6%) |
| Neck length | S * M ** L *** | 59 (44%) 59 (44%) 17 (12%) |
| Parameter | Relevant Radiolucencies | p-Value | |
|---|---|---|---|
| Present | Absent | ||
| Age (mean ± SD) | 63.7 ± 6.1 years | 67.5 ± 11.4 years | 0.329 |
| Dorr classification | 0.771 | ||
| Type A | 75% | 68% | |
| Type B | 25% | 32% | |
| BMI (mean ± SD) | 31 ± 5.3 kg/m2 | 27.5 ± 3.9 kg/m2 | 0.284 |
| HOOS total (mean ± SD) | 92.5 ± 7.1% | 88.9 ± 14.3% | 0.625 |
| Pain | 96.3 ± 5.3% | 90 ± 12.3% | 0.371 |
| Symptoms | 90 ± 7.1% | 89.5 ± 14.8% | 0.944 |
| ADL * | 95.6 ± 6.2% | 90.4 ± 14% | 0.477 |
| Sport/recreation | 84.4 ± 13.3% | 85.2 ± 20.9% | 0.952 |
| QoL ** | 90.7 ± 4.5% | 84.1 ± 18.4% | 0.257 |
| Study | Prosthesis Stem | Stem Type | Approach | Revision Rates (%) | Follow-Up (Months) |
|---|---|---|---|---|---|
| Hagel et al. [19] | Mayo® prosthesis (Zimmer Inc., Warsaw, IN, USA) | Collarless | Anterior | 2 | 83.6 |
| Falez et al. [20] | Anterior | 2 | 56.4 | ||
| Goebel et al. [21] | Posterior | 10 | 81 | ||
| Morrey et al. [22] | Anterolateral | 9 | 78 | ||
| Hallan et al. [23] | Profile® (DePuy, Warsaw, IN, USA) | Collarless | Lateral | 12 | 144 |
| Profile® hydroxyapatite- (HA-) coated stem (DePuy, Warsaw, IN, USA) | Collarless | Lateral | 4 | 144 | |
| Heaven et al. [24] | Corail® AMT collared (DePuy, Warsaw, IN, USA) | Collared | Anterior | 2.5 | 24 |
| Lateral | 2.4 | 24 | |||
| Chitnis et al. [25] | ACTIS® total hip system collared (DePuy, Warsaw, IN, USA) | Collared | Anterior | 1.08 | 36 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Darwich, A.; Pankert, K.; Ottersbach, A.; Betsch, M.; Gravius, S.; Bdeir, M. 5-Year Clinical and Radiographic Results of the Direct Anterior Approach for Total Hip Arthroplasty Using a Collared Cementless Femoral Short-Stem Prosthesis. J. Clin. Med. 2022, 11, 346. https://doi.org/10.3390/jcm11020346
Darwich A, Pankert K, Ottersbach A, Betsch M, Gravius S, Bdeir M. 5-Year Clinical and Radiographic Results of the Direct Anterior Approach for Total Hip Arthroplasty Using a Collared Cementless Femoral Short-Stem Prosthesis. Journal of Clinical Medicine. 2022; 11(2):346. https://doi.org/10.3390/jcm11020346
Chicago/Turabian StyleDarwich, Ali, Kim Pankert, Andreas Ottersbach, Marcel Betsch, Sascha Gravius, and Mohamad Bdeir. 2022. "5-Year Clinical and Radiographic Results of the Direct Anterior Approach for Total Hip Arthroplasty Using a Collared Cementless Femoral Short-Stem Prosthesis" Journal of Clinical Medicine 11, no. 2: 346. https://doi.org/10.3390/jcm11020346
APA StyleDarwich, A., Pankert, K., Ottersbach, A., Betsch, M., Gravius, S., & Bdeir, M. (2022). 5-Year Clinical and Radiographic Results of the Direct Anterior Approach for Total Hip Arthroplasty Using a Collared Cementless Femoral Short-Stem Prosthesis. Journal of Clinical Medicine, 11(2), 346. https://doi.org/10.3390/jcm11020346





