Specialist Palliative Care Consultations in COVID-19 Patients in the ICU—A Retrospective Analysis of Patient Characteristics and Symptoms at a German University Hospital
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. COVID-19 Setting and Specialist Palliative Care
2.3. Patient Selection and Data Collection
2.4. Data Analysis
3. Results
3.1. Patient Characteristics
3.2. Specialist Palliative Care Involvement
3.3. Symptom Control
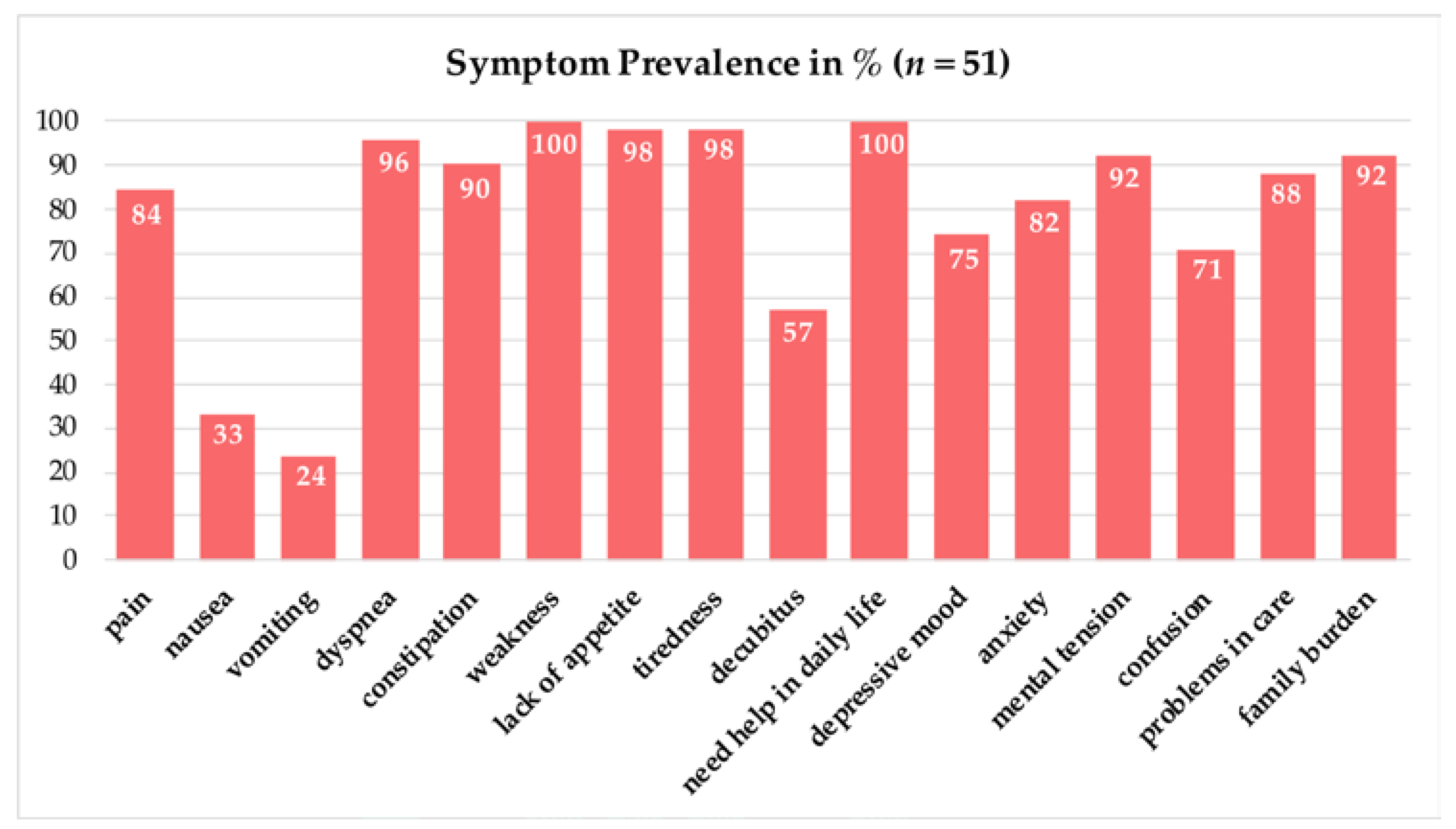
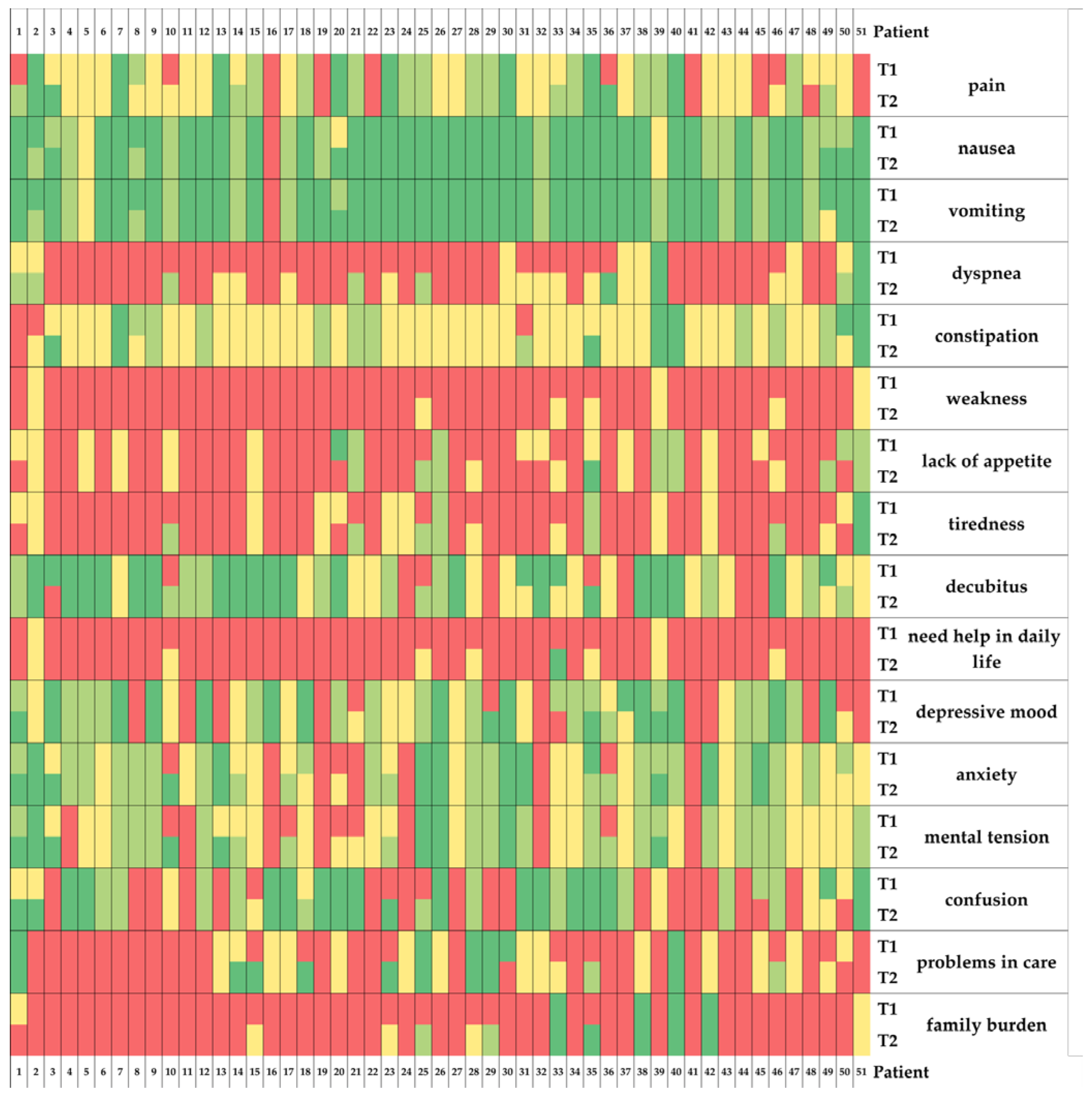
3.3.1. Symptom Burden
3.3.2. Symptom Intensity
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 27 July 2022).
- Menni, C.; Valdes, A.M.; Polidori, L.; Antonelli, M.; Penamakuri, S.; Nogal, A.; Louca, P.; May, A.; Figueiredo, J.C.; Hu, C.; et al. Symptom Prevalence, Duration, and Risk of Hospital Admission in Individuals Infected with SARS-CoV-2 during Periods of Omicron and Delta Variant Dominance: A Prospective Observational Study from the ZOE COVID Study. Lancet 2022, 399, 1618–1624. [Google Scholar] [CrossRef]
- Mortality Analyses—Johns Hopkins Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 28 July 2022).
- Guidet, B.; Jung, C.; Flaatten, H.; Fjølner, J.; Artigas, A.; Pinto, B.B.; Schefold, J.C.; Beil, M.; Sigal, S.; van Heerden, P.V.; et al. Increased 30-Day Mortality in Very Old ICU Patients with COVID-19 Compared to Patients with Respiratory Failure without COVID-19. Intensive Care Med. 2022, 48, 435–447. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A.; Kane, A.D.; Kursumovic, E.; Oglesby, F.C.; Cook, T.M. Mortality in Patients Admitted to Intensive Care with COVID-19: An Updated Systematic Review and Meta-Analysis of Observational Studies. Anaesthesia 2021, 76, 537–548. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, K.; Shekar, K.; Ling, R.R.; Barbaro, R.P.; Wong, S.N.; Tan, C.S.; Rochwerg, B.; Fernando, S.M.; Takeda, S.; MacLaren, G.; et al. Extracorporeal Membrane Oxygenation for COVID-19: A Systematic Review and Meta-Analysis. Crit. Care 2021, 25, 1–11. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Strassmann, S.; Merten, M.; Bein, T.; Windisch, W.; Meybohm, P.; Weber-Carstens, S. High In-Hospital Mortality Rate in Patients with COVID-19 Receiving Extracorporeal Membrane Oxygenation in Germany: A Critical Analysis. Am. J. Respir. Crit. Care Med. 2021, 204, 991–994. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Slutsky, A.S.; Bein, T.; Windisch, W.; Weber-Carstens, S.; Brodie, D. Complete Countrywide Mortality in COVID Patients Receiving ECMO in Germany throughout the First Three Waves of the Pandemic. Crit. Care 2021, 25, 1–2. [Google Scholar] [CrossRef]
- Varrassi, G.; Rekatsina, M. Clinical Medicine Updates on Palliative Medicine in the COVID-19 Era. J. Clin. Med. 2022, 11, 315. [Google Scholar] [CrossRef]
- Bakitas, M.A.; Tosteson, T.D.; Li, Z.; Lyons, K.D.; Hull, J.G.; Li, Z.; Dionne-Odom, J.N.; Frost, J.; Dragnev, K.H.; Hegel, M.T.; et al. Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III Randomized Controlled Trial. J. Clin. Oncol. 2015, 33, 1438–1445. [Google Scholar] [CrossRef]
- Ferrell, B.R.; Twaddle, M.L.; Melnick, A.; Meier, D.E. National Consensus Project Clinical Practice Guidelines for Quality Palliative Care Guidelines, 4th Edition. J. Palliat. Med. 2018, 21, 1684–1689. [Google Scholar] [CrossRef]
- Temel, J.S.; Greer, J.A.; Muzikansky, A.; Gallagher, E.R.; Admane, S.; Jackson, V.A.; Dahlin, C.M.; Blinderman, C.D.; Jacobsen, J.; Pirl, W.F.; et al. Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2010, 363, 733–742. [Google Scholar] [CrossRef]
- Costantini, M.; Sleeman, K.E.; Peruselli, C.; Higginson, I.J. Response and Role of Palliative Care during the COVID-19 Pandemic: A National Telephone Survey of Hospices in Italy. Palliat. Med. 2020, 34, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Etkind, S.N.; Bone, A.E.; Lovell, N.; Cripps, R.L.; Harding, R.; Higginson, I.J.; Sleeman, K.E. The Role and Response of Palliative Care and Hospice Services in Epidemics and Pandemics: A Rapid Review to Inform Practice During the COVID-19 Pandemic. J. Pain Symptom Manag. 2020, 60, e31. [Google Scholar] [CrossRef] [PubMed]
- Schoenmaekers, J.J.A.O.; Hendriks, L.E.L.; van den Everdingen, M.H.J.B. Palliative Care for Cancer Patients During the COVID-19 Pandemic, With Special Focus on Lung Cancer. Front. Oncol. 2020, 10, 1405. [Google Scholar] [CrossRef] [PubMed]
- Dunleavy, L.; Preston, N.; Bajwah, S.; Bradshaw, A.; Cripps, R.; Fraser, L.K.; Maddocks, M.; Hocaoglu, M.; Murtagh, F.E.M.; Oluyase, A.O.; et al. ‘Necessity Is the Mother of Invention’: Specialist Palliative Care Service Innovation and Practice Change in Response to COVID-19. Results from a Multinational Survey (CovPall). Palliat. Med. 2021, 35, 814–829. [Google Scholar] [CrossRef]
- Ritchey, K.C.; Foy, A.; McArdel, E.; Gruenewald, D.A. Reinventing Palliative Care Delivery in the Era of COVID-19: How Telemedicine Can Support End of Life Care. Am. J. Hosp. Palliat. Care 2020, 37, 992–997. [Google Scholar] [CrossRef]
- Oluyase, A.O.; Hocaoglu, M.; Cripps, R.L.; Maddocks, M.; Walshe, C.; Fraser, L.K.; Preston, N.; Dunleavy, L.; Bradshaw, A.; Murtagh, F.E.M.; et al. The Challenges of Caring for People Dying From COVID-19: A Multinational, Observational Study (CovPall). J. Pain Symptom Manag. 2021, 62, 460–470. [Google Scholar] [CrossRef]
- Tielker, J.M.; Weber, J.P.; Simon, S.T.; Bausewein, C.; Stiel, S.; Schneider, N. Experiences, Challenges and Perspectives for Ensuring End-of-Life Patient Care: A National Online Survey with General Practitioners in Germany. PLoS ONE 2021, 16, e0254056. [Google Scholar] [CrossRef]
- Weber, J.P.; Tielker, J.M.; Kamandi, N.; Simon, S.T.; Bausewein, C.; Stiel, S.; Schneider, N. Outpatient Care of Oncological Patients in Palliative Treatment Situations and Their Relatives during the COVID-19 Pandemic. Onkologe 2021, 27, 783–789. [Google Scholar] [CrossRef]
- Jansky, M.; Schade, F.; Rieder, N.; Lohrmann, D.; Gebel, C.; Kloppenburg, L.; Wedding, U.; Simon, S.T.; Bausewein, C.; Nauck, F. ‘It Felt like a Black Hole, Great Uncertainty, but We Have to Take Care for Our Patients’-Qualitative Findings on the Effects of the COVID-19 Pandemic on Specialist Palliative Home Care. PLoS ONE 2021, 16, e0260767. [Google Scholar] [CrossRef]
- Schwartz, J.; Reuters, M.C.; Schallenburger, M.; Meier, S.; Roch, C.; Ziegaus, A.; Werner, L.; Fischer, M.; van Oorschot, B.; Neukirchen, M. General Palliative Care during the Pandemic. Onkologe 2021, 27, 686–690. [Google Scholar] [CrossRef]
- Schallenburger, M.; Reuters, M.C.; Schwartz, J.; Fischer, M.; Roch, C.; Werner, L.; Bausewein, C.; Simon, S.T.; van Oorschot, B.; Neukirchen, M. Inpatient Generalist Palliative Care during the SARS-CoV-2 Pandemic—Experiences, Challenges and Potential Solutions from the Perspective of Health Care Workers. BMC Palliat. Care 2022, 21, 63. [Google Scholar] [CrossRef] [PubMed]
- Schloesser, K.; Simon, S.T.; Pauli, B.; Voltz, R.; Jung, N.; Leisse, C.; van der Heide, A.; Korfage, I.J.; Pralong, A.; Bausewein, C.; et al. Saying Goodbye All Alone with No Close Support Was Difficult—Dying during the COVID-19 Pandemic: An Online Survey among Bereaved Relatives about End-of-Life Care for Patients with or without SARS-CoV2 Infection. BMC Health Serv. Res. 2021, 21, 998. [Google Scholar] [CrossRef] [PubMed]
- Janssen, D.J.A. Palliative Care in COVID-19. Curr. Opin. Support. Palliat. Care 2021, 15, 199. [Google Scholar] [CrossRef]
- Janssen, D.J.A.; Ekström, M.; Currow, D.C.; Johnson, M.J.; Maddocks, M.; Simonds, A.K.; Tonia, T.; Marsaa, K. COVID-19: Guidance on Palliative Care from a European Respiratory Society International Task Force. Eur. Respir. J. 2020, 56, 2002583. [Google Scholar] [CrossRef] [PubMed]
- Andreas, M.; Piechotta, V.; Skoetz, N.; Grummich, K.; Becker, M.; Joos, L.; Becker, G.; Meissner, W.; Boehlke, C. Interventions for Palliative Symptom Control in COVID-19 Patients. Cochrane Database Syst. Rev. 2021, 8, CD015061. [Google Scholar] [CrossRef]
- Beng, T.S.; Kim, C.L.C.; Shee, C.C.; Ching, D.N.L.; Liang, T.J.; Kumar, M.K.N.; Guan, N.C.; Khuen, L.P.; Loong, L.C.; Chin, L.E.; et al. COVID-19, Suffering and Palliative Care: A Review. Am. J. Hosp. Palliat. Care 2022, 39, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Schallenburger, M.; Thyson, T.; Meier, S.; Neukirchen, M. Psychische Belastung Des Intensivpersonals: Kommunikationsseminare Helfen. Available online: https://www.aerzteblatt.de/pdf.asp?id=222589 (accessed on 9 March 2022).
- Lovell, N.; Maddocks, M.; Etkind, S.N.; Taylor, K.; Carey, I.; Vora, V.; Marsh, L.; Higginson, I.J.; Prentice, W.; Edmonds, P.; et al. Characteristics, Symptom Management, and Outcomes of 101 Patients With COVID-19 Referred for Hospital Palliative Care. J. Pain Symptom Manag. 2020, 60, e77–e81. [Google Scholar] [CrossRef]
- Haydar, A.; Lo, K.B.; Goyal, A.; Gul, F.; Peterson, E.; Bhargav, R.; DeJoy, R.; Salacup, G.; Pelayo, J.; Albano, J.; et al. Palliative Care Utilization Among Patients With COVID-19 in an Underserved Population: A Single-Center Retrospective Study. J. Pain Symptom Manag. 2020, 60, e18. [Google Scholar] [CrossRef]
- Golob, S.; Zilinyi, R.; Godfrey, S.; Defilippis, E.M.; Fried, J.; Sayer, G.; Blinderman, C.D.; Uriel, N.; Nakagawa, S. The Prevalence of Palliative Care Consultation in Deceased COVID-19 Patients and Its Association with End-of-Life Care. J. Palliat. Med. 2022, 25, 70–74. [Google Scholar] [CrossRef]
- Obata, R.; Maeda, T.; Rizk, D.; Kuno, T. Palliative Care Team Involvement in Patients With COVID-19 in New York City. Am. J. Hosp. Palliat. Care 2020, 37, 869–872. [Google Scholar] [CrossRef]
- Sheehan, J.; Ho, K.S.; Poon, J.; Sarosky, K.; Fung, J.Y. Palliative Care in Critically Ill COVID-19 Patients: The Early New York City Experience. BMJ Support. Palliat. Care 2020. [Google Scholar] [CrossRef] [PubMed]
- Cheruku, S.R.; Barina, A.; Kershaw, C.D.; Goff, K.; Reisch, J.; Hynan, L.S.; Ahmed, F.; Armaignac, D.L.; Patel, L.; Belden, K.A.; et al. Palliative Care Consultation and End-of-Life Outcomes in Hospitalized COVID-19 Patients. Resuscitation 2022, 170, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Frydman, J.L.; Aldridge, M.; Moreno, J.; Singer, J.; Zeng, L.; Chai, E.; Morrison, R.S.; Gelfman, L.P. Access to Palliative Care Consultation for Hospitalized Adults with COVID-19 in an Urban Health System: Were There Disparities at the Peak of the Pandemic? J. Palliat. Med. 2022, 25, 124–129. [Google Scholar] [CrossRef]
- Almeida, L.K.R.; Avelino-Silva, T.J.; de Lima e Silva, D.C.L.; Campos, B.A.; Varela, G.; Fonseca, C.M.B.; Amorim, V.L.; de Toledo Piza, F.M.; Aliberti, M.J.; Degani-Costa, L.H. Palliative Care in Hospitalized Middle-Aged and Older Adults With COVID-19. J. Pain Symptom Manag. 2022, 63, 680–688. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Schilling, J.; Buda, S.; Tolksdorf, K. Zweite Aktualisierung Der Retrospektiven Phaseneinteilung Der COVID-19- Pandemie in Deutschland. Epid. Bull. 2022, 10, 3–5. [Google Scholar] [CrossRef]
- Radbruch, L.; Sabatowski, R.; Loick, G.; Jonen-Thielemann, I.; Elsner, F.; Hörmann, E. MIDOS--Validation of a Minimal Documentation System for Palliative Medicine. Schmerz 2000, 14, 231–239. [Google Scholar] [CrossRef]
- Stiel, S.; Matthes, M.E.; Bertram, L.; Ostgathe, C.; Elsner, F.; Radbruch, L. Validierung Der Neuen Fassung Des Minimalen Dokumentationssystems (MIDOS2) Für Patienten in Der Palliativmedizin: Deutsche Version Der Edmonton Symptom Assessment Scale (ESAS). Schmerz 2010, 24, 596–604. [Google Scholar] [CrossRef]
- Simon, S.T.; Altfelder, N.; Alt-Epping, B.; Bausewein, C.; Weingärtner, V.; Voltz, R.; Ostgathe, C.; Radbruch, L.; Lindena, G.; Nauck, F. Charakteristika von Palliativpatienten Mit Atemnot: Ergebnisse Der Deutschlandweiten Hospiz- Und Palliativerhebung. Pneumologie 2017, 71, 40–47. [Google Scholar] [CrossRef]
- Bausewein, C.; Hodiamont, F.; Berges, N.; Ullrich, A.; Gerlach, C.; Oechsle, K.; Pauli, B.; Weber, J.; Stiel, S.; Schneider, N.; et al. National Strategy for Palliative Care of Severely Ill and Dying People and Their Relatives in Pandemics (PallPan) in Germany—Study Protocol of a Mixed-Methods Project. BMC Palliat. Care 2022, 21, 10. [Google Scholar] [CrossRef]
- Scoping Review und Literaturverzeichnis—PallPan. Available online: https://pallpan.de/review-und-literatur/ (accessed on 4 August 2022).
- Mercadante, S.; Gregoretti, C.; Cortegiani, A. Palliative Care in Intensive Care Units: Why, Where, What, Who, When, How. BMC Anesthesiol 2018, 18, 106. [Google Scholar] [CrossRef] [PubMed]
- Giri, S.; Chenn, L.M.; Romero-Ortuno, R. Nursing Homes during the COVID-19 Pandemic: A Scoping Review of Challenges and Responses. Eur. Geriatr. Med. 2021, 12, 1127–1136. [Google Scholar] [CrossRef] [PubMed]
- de Heer, G.; Saugel, B.; Sensen, B.; Rübsteck, C.; Pinnschmidt, H.O.; Kluge, S. Advance Directives and Powers of Attorney in Intensive Care Patients. Dtsch. Arzteblatt Int. 2017, 114, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Bertini, P.; Guarracino, F.; Falcone, M.; Nardelli, P.; Landoni, G.; Nocci, M.; Paternoster, G. ECMO in COVID-19 Patients: A Systematic Review and Meta-Analysis. J. Cardiothorac. Vasc. Anesth. 2022, 36, 2700–2706. [Google Scholar] [CrossRef]
- Haji, J.Y.; Mehra, S.; Doraiswamy, P. Awake ECMO and Mobilizing Patients on ECMO. Indian J. Thorac. Cardiovasc. Surg. 2021, 37, 309. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Wittenberg, E.; Sullivan, S.S.; Lorenz, R.A.; Chang, Y.P. The Experiences of Family Members of Ventilated COVID-19 Patients in the Intensive Care Unit: A Qualitative Study. Am. J. Hosp. Palliat. Care 2021, 38, 869–876. [Google Scholar] [CrossRef]
- Schneider, J.N.; Hiebel, N.; Kriegsmann-Rabe, M.; Schmuck, J.; Erim, Y.; Morawa, E.; Jerg-Bretzke, L.; Beschoner, P.; Albus, C.; Hannemann, J.; et al. Moral Distress in Hospitals During the First Wave of the COVID-19 Pandemic: A Web-Based Survey Among 3,293 Healthcare Workers Within the German Network University Medicine. Front. Psychol. 2021, 12, 775204. [Google Scholar] [CrossRef] [PubMed]
- Living Guidance for Clinical Management of COVID-19. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 (accessed on 28 July 2022).

| Characteristic | Mean (SD) | n (%) |
|---|---|---|
| Age, years | 69.51 (15.84) | |
| Sex, male/female | 32 (62.7)/19 (37.3) | |
| Place of living | ||
| Home | 42 (82.4) | |
| Nursing home | 7 (13.7) | |
| Missing data | 2 (3.9) | |
| Relatives available, yes/no | 48 (94.1)/3 (5.9) | |
| Comorbidities | ||
| Arterial hypertension | 36 (70.6) | |
| Coronary artery disease | 20 (39.2) | |
| Obesity | 16 (31.4) | |
| Oncological disease | 13 (25.5) | |
| Diabetes mellitus | 10 (19.6) | |
| Dementia | 6 (11.76) | |
| Chronic lung disease | 5 (9.8) | |
| Care planning | ||
| Advance directive | 13 (25.5) | |
| Health care proxy | 23 (45.1) |
| Characteristic | Median (IQR) | n (%) |
|---|---|---|
| ECOG * | ||
| 2 | 1 (2) | |
| 3 | 7 (13.7) | |
| 4 | 43 (84.3) | |
| COVID-19 treatment | ||
| Noninvasive ventilation | 36 (70.6) | |
| Mechanical ventilation | 23 (45.1) | |
| ECMO * | 23 (45.1) | |
| Intravenous catecholamines | 23 (45.1) | |
| Dialysis | 17 (33.3) | |
| Opioids | 29 (56.9) | |
| Durations in days (d) or minutes (min) | ||
| COVID-19 confirmation until sPC contact (d) | 14 (11) | |
| sPC treatment in total (d) | 13.5 (10.5) | |
| Contact with physicians (min) | 140 (82.5) | |
| Contact with nurses (min) | 120 (82.5) | |
| Contact with psychologists (min) | 50 (82.5) | |
| Contact with physiotherapists (min) | 110 (257.5) | |
| Contact with relatives to psychologists (min) | 30 (50) | |
| Outcomes | ||
| Deceased | 32 (62.8) | |
| Palliative care unit | 2 (3.9) | |
| Discharge | 15 (29.4) | |
| Missing data | 2 (3.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tenge, T.; Brimah, S.; Schlieper, D.; Roesel, A.; Schwartz, J.; Schallenburger, M.; Meier, S.; Brandenburger, T.; Kindgen-Milles, D.; Kienbaum, P.; et al. Specialist Palliative Care Consultations in COVID-19 Patients in the ICU—A Retrospective Analysis of Patient Characteristics and Symptoms at a German University Hospital. J. Clin. Med. 2022, 11, 5925. https://doi.org/10.3390/jcm11195925
Tenge T, Brimah S, Schlieper D, Roesel A, Schwartz J, Schallenburger M, Meier S, Brandenburger T, Kindgen-Milles D, Kienbaum P, et al. Specialist Palliative Care Consultations in COVID-19 Patients in the ICU—A Retrospective Analysis of Patient Characteristics and Symptoms at a German University Hospital. Journal of Clinical Medicine. 2022; 11(19):5925. https://doi.org/10.3390/jcm11195925
Chicago/Turabian StyleTenge, Theresa, Sebastian Brimah, Daniel Schlieper, Antje Roesel, Jacqueline Schwartz, Manuela Schallenburger, Stefan Meier, Timo Brandenburger, Detlef Kindgen-Milles, Peter Kienbaum, and et al. 2022. "Specialist Palliative Care Consultations in COVID-19 Patients in the ICU—A Retrospective Analysis of Patient Characteristics and Symptoms at a German University Hospital" Journal of Clinical Medicine 11, no. 19: 5925. https://doi.org/10.3390/jcm11195925
APA StyleTenge, T., Brimah, S., Schlieper, D., Roesel, A., Schwartz, J., Schallenburger, M., Meier, S., Brandenburger, T., Kindgen-Milles, D., Kienbaum, P., & Neukirchen, M. (2022). Specialist Palliative Care Consultations in COVID-19 Patients in the ICU—A Retrospective Analysis of Patient Characteristics and Symptoms at a German University Hospital. Journal of Clinical Medicine, 11(19), 5925. https://doi.org/10.3390/jcm11195925






