Do Men and Women Have a Different Association between Fear-Avoidance and Pain Intensity in Chronic Pain? An Experience Sampling Method Cohort-Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Experience Sampling
2.4. Baseline Variables
2.5. Statistical Analysis
3. Results
3.1. Description of the Sample
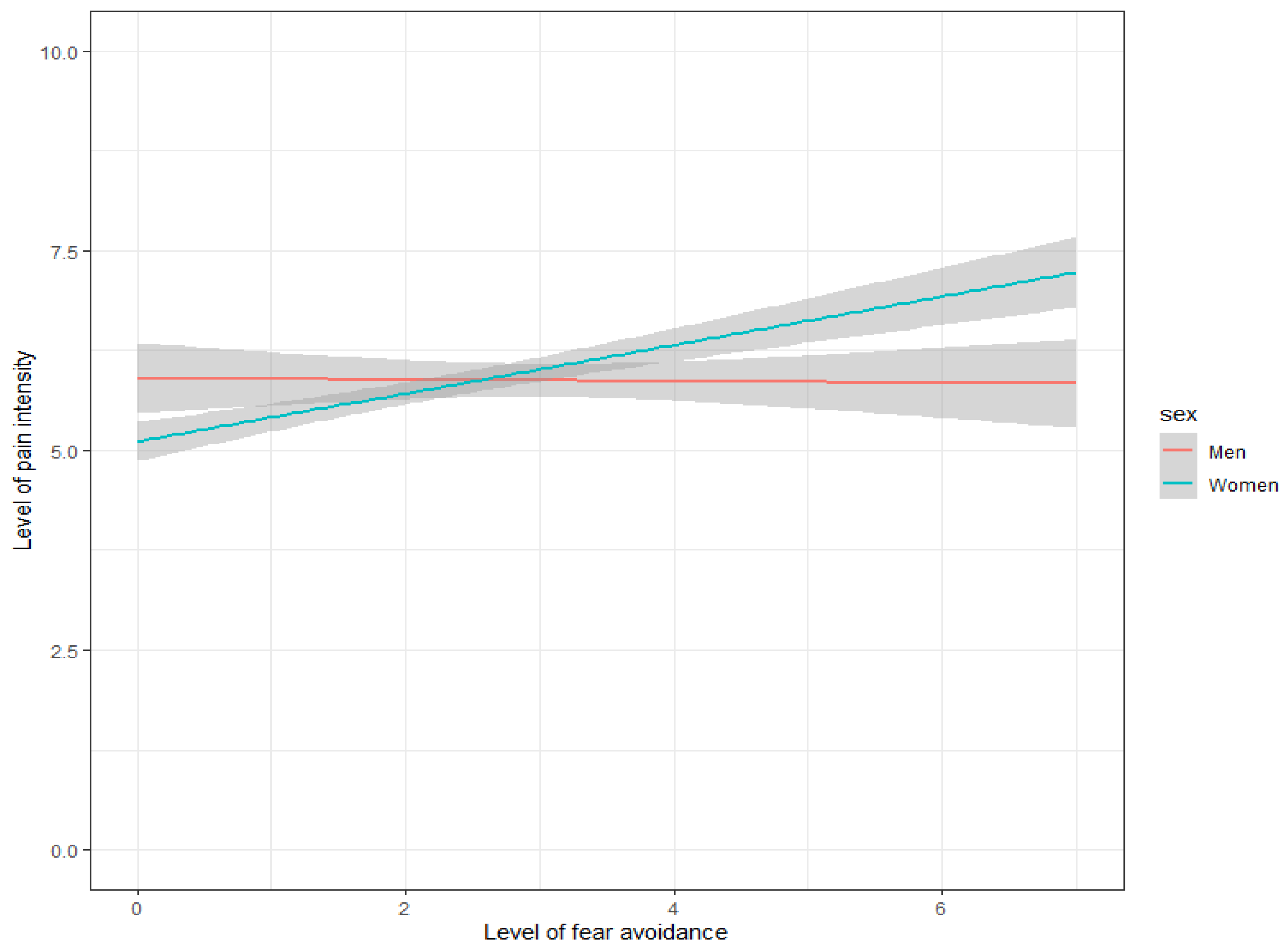
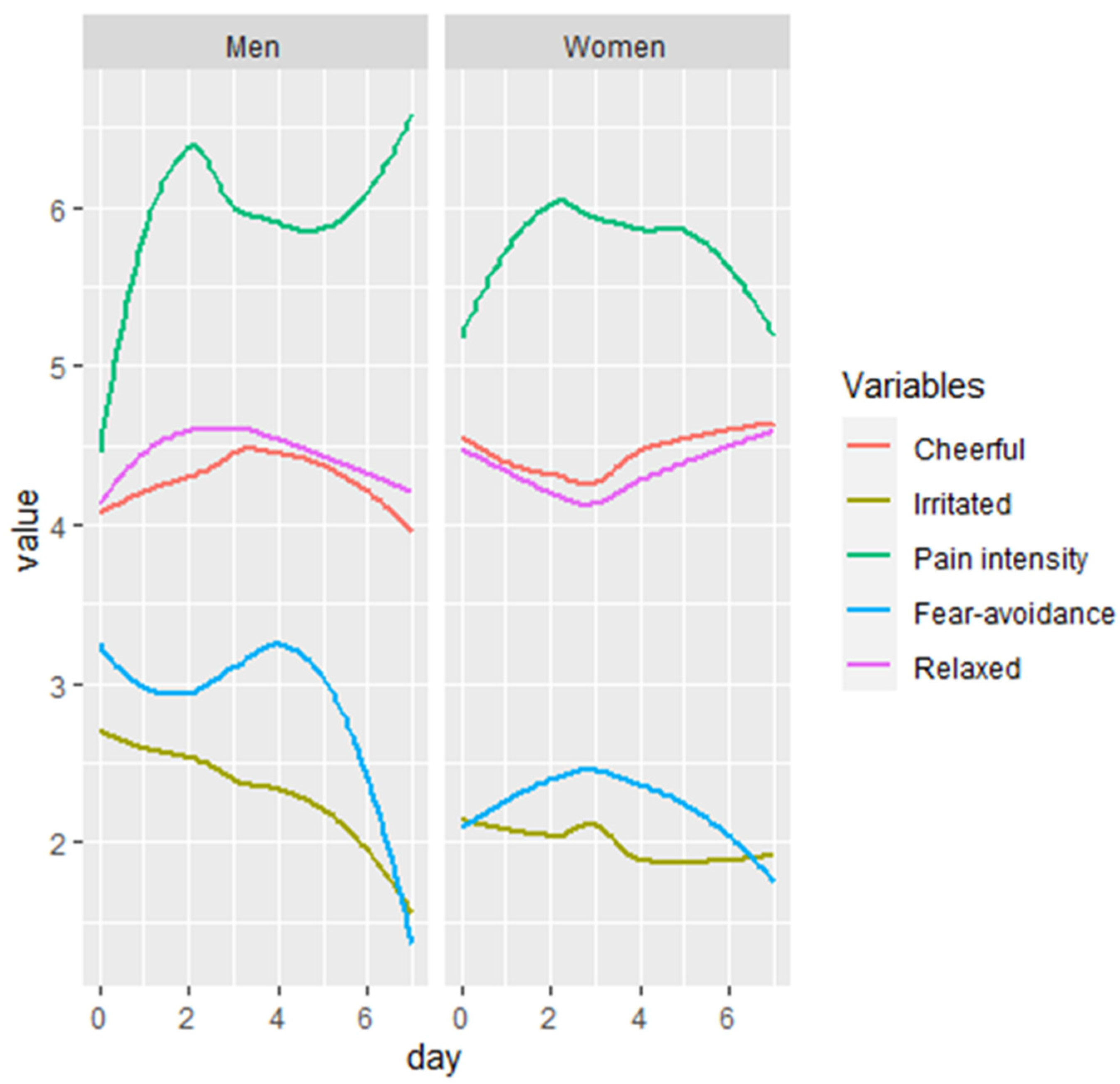
3.2. Sex Differences in the Association between Fear-Avoidance and Pain Intensity and the Influence of Affective States
4. Discussion
4.1. Summary of Main Findings
4.2. Differences in the Association of Fear-Avoidance and Pain Intensity
4.3. Sex Differences in the Association between Fear-Avoidance and Pain Intensity
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cohen, S.P.; Vase, L.; Hooten, W.M. Chronic pain: An update on burden, best practices, and new advances. Lancet 2021, 397, 2082–2097. [Google Scholar] [CrossRef]
- Nugraha, B.; Gutenbrunner, C.; Barke, A.; Karst, M.; Schiller, J.; Schäfer, P.; Falter, S.; Korwisi, B.; Rief, W.; Treede, R.-D.; et al. The IASP classification of chronic pain for ICD-11: Functioning properties of chronic pain. Pain 2019, 160, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef]
- Fillingim, R.B.; King, C.D.; Ribeiro-Dasilva, M.C.; Rahim-Williams, B.; Riley, J.L., III. Sex, Gender, and Pain: A Review of Recent Clinical and Experimental Findings. J. Pain 2009, 10, 447–485. [Google Scholar] [CrossRef] [PubMed]
- Mogil, J.S. Sex differences in pain and pain inhibition: Multiple explanations of a controversial phenomenon. Nat. Rev. Neurosci. 2012, 13, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Rhudy, J.L.; Williams, A.E. Gender differences in pain: Do emotions play a role? Gend. Med. 2005, 2, 208–226. [Google Scholar] [CrossRef]
- Myin-Germeys, I.; Kasanova, Z.; Vaessen, T.; Vachon, H.; Kirtley, O.; Viechtbauer, W.; Reininghaus, U. Experience sampling methodology in mental health research: New insights and technical developments. World Psychiatry 2018, 17, 123–132. [Google Scholar] [CrossRef]
- Bair, M.J.; Robinson, R.L.; Katon, W.; Kroenke, K. Depression and pain comorbidity: A literature review. Arch. Intern. Med. 2003, 163, 2433–2445. [Google Scholar] [CrossRef]
- Verhagen, S.J.W.; Hasmi, L.; Drukker, M.; van Os, J.; Delespaul, P.A.E.G. Use of the experience sampling method in the context of clinical trials: Table 1. Évid. Based Ment. Health 2016, 19, 86–89. [Google Scholar] [CrossRef]
- Csikszentmihalyi, M. Handbook of Research Methods for Studying Daily Life; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Verhagen, S.J.W.; Berben, J.A.; Leue, C.; Marsman, A.; Delespaul, P.A.E.G.; van Os, J.; Lousberg, R. Demonstrating the reliability of transdiagnostic mHealth Routine Outcome Monitoring in mental health services using experience sampling technology. PLoS ONE 2017, 12, e0186294. [Google Scholar] [CrossRef]
- Daniëls, N.E.M.; Hochstenbach, L.M.J.; van Bokhoven, M.A.; Beurskens, A.J.H.M.; Delespaul, P.A.E.G. Implementing Experience Sampling Technology for Functional Analysis in Family Medicine—A Design Thinking Approach. Front. Psychol. 2019, 10, 2782. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, S.J.W.; Daniëls, N.E.M.; Bartels, S.L.; Tans, S.; Borkelmans, K.W.H.; de Vugt, M.E.; Delespaul, P.A.E.G. Measuring within-day cognitive performance using the experience sampling method: A pilot study in a healthy population. PLoS ONE 2019, 14, e0226409. [Google Scholar] [CrossRef]
- Crawford, J.R.; Henry, J.D. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2004, 43 Pt 3, 245–265. [Google Scholar] [CrossRef] [PubMed]
- Peeters, F.P.R. Affectiviteit en zelfbeoordeling van depressie en angst. Tijdschr. Voor Psychiatr. 1996, 38, 240–250. [Google Scholar]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Cleeland, C.S. The Brief Pain Inventory User Guide; The University of Texas MD Anderson Cancer Center: Houston, TX, USA, 2009; pp. 1–11. [Google Scholar]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N.; et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef]
- Hays, R.D.; Morales, L.S. The RAND-36 measure of health-related quality of life. Ann. Med. 2001, 33, 350–357. [Google Scholar] [CrossRef]
- Stern, A.F. The Hospital Anxiety and Depression Scale. Occup. Med. 2014, 64, 393–394. [Google Scholar] [CrossRef]
- Sullivan, M.J. The Pain Catastrophizing Scale: User Manual; McGill University: Montreal, QC, Canada, 2009; pp. 1–36. [Google Scholar]
- Brouwer, B.; Waardenburg, S.; Jacobs, C.; Overdijk, M.; Leue, C.; Köke, A.; van Kuijk, S.; van Kleef, M.; Van Zundert, J.; de Meij, N. Biopsychosocial baseline values of 15,000 patients suffering from chronic pain: Dutch Data Pain study. Reg. Anesth. Pain Med. 2020, 45, 774–782. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.; Kole-Snijders, A.M.; Boeren, R.G.; van Eek, H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain 1995, 62, 363–372. [Google Scholar] [CrossRef]
- Bränström, H.; Fahlström, M. Kinesiophobia in patients with chronic musculoskeletal pain: Differences between men and women. J. Rehabil. Med. 2008, 40, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Rovner, G.S.; Sunnerhagen, K.S.; Björkdahl, A.; Gerdle, B.; Börsbo, B.; Johansson, F.; Gillanders, D. Chronic pain and sex-differences; women accept and move, while men feel blue. PLoS ONE 2017, 12, e0175737. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Maestre, C.; Esteve, R. The Role of Sex/Gender in the Experience of Pain: Resilience, Fear, and Acceptance as Central Variables in the Adjustment of Men and Women with Chronic Pain. J. Pain 2014, 15, 608–618.e1. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Maestre, C.; Martínez, A.E.L.; Zarazaga, R.E. Personality characteristics as differential variables of the pain experience. J. Behav. Med. 2004, 27, 147–165. [Google Scholar] [CrossRef] [PubMed]
- De Baets, L.; Matheve, T.; Meeus, M.; Struyf, F.; Timmermans, A. The influence of cognitions, emotions and behavioral factors on treatment outcomes in musculoskeletal shoulder pain: A systematic review. Clin. Rehabil. 2019, 33, 980–991. [Google Scholar] [CrossRef]
- Huber, M.; van Vliet, M.; Giezenberg, M.; Winkens, B.; Heerkens, Y.; Dagnelie, P.C.; Knottnerus, J.A. Towards a ‘patient-centred’ operationalisation of the new dynamic concept of health: A mixed methods study. BMJ Open 2016, 6, e010091. [Google Scholar] [CrossRef]
- Mujagic, Z.; Leue, C.; Vork, L.; Lousberg, R.; Jonkers, D.M.A.E.; Keszthelyi, D.; Hesselink, M.A.; Van Schagen, T.J.C.; Van Os, J.; Masclee, A.A.M.; et al. The Experience Sampling Method—A new digital tool for momentary symptom assessment in IBS: An exploratory study. Neurogastroenterol. Motil. 2015, 27, 1295–1302. [Google Scholar] [CrossRef]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–3. [Google Scholar] [CrossRef]
- van Os, J.; Verhagen, S.; Marsman, A.; Peeters, F.; Bak, M.; Marcelis, M.; Drukker, M.; Reininghaus, U.; Jacobs, N.; Lataster, T.; et al. The experience sampling method as an mHealth tool to support self-monitoring, self-insight, and personalized health care in clinical practice. Depress. Anxiety 2017, 34, 481–493. [Google Scholar] [CrossRef]
- Vork, L.; Mujagic, Z.; Drukker, M.; Keszthelyi, D.; Conchillo, J.M.; Hesselink, M.A.M.; Van Os, J.; Masclee, A.A.M.; Leue, C.; Kruimel, J.W. The Experience Sampling Method—Evaluation of treatment effect of escitalopram in IBS with comorbid panic disorder. Neurogastroenterol. Motil. 2019, 31, e13515. [Google Scholar] [CrossRef]
- Stone, A.A.; Obbarius, A.; Junghaenel, D.U.; Wen, C.K.; Schneider, S. High-resolution, field approaches for assessing pain: Ecological Momentary Assessment. Pain 2021, 162, 4–9. [Google Scholar] [CrossRef] [PubMed]


| Patient Baseline Characteristics | Total Cohort, n = 45 | Men, n = 13 | Women, n = 32 | p-Value |
|---|---|---|---|---|
| Demographic Characteristics | ||||
| Age in years, mean (SD) | 47.6 (12.8) | 52.8 (13.8) | 45.5 (12.0) | 0.086 |
| Marital status, n (%) | 0.411 | |||
| Relationship | 36 (80.0) | 9 (69.2) | 27 (84.4) | |
| No relationship | 9 (20.0) | 4 (30.8) | 5 (15.6) | |
| Education, n (%) | 0.287 | |||
| Low (<9 years of education) | 32 (71.1) | 11 (84.6) | 21 (65.6) | |
| High (≥9 years of education) | 13 (28.9) | 2 (15.4) | 11 (34.4) | |
| Employment, n (%) | 1.000 | |||
| Unemployed (no paid job) | 29 (64.4) | 8 (61.5) | 21 (65.6) | |
| Employed (paid job) | 16 (35.6) | 5 (38.5) | 11 (34.4) | |
| Pain Characteristics | ||||
| Pain duration in months, mean (SD) | 73.2 (81.1) | 45.9 (55.5) | 84.3 (87.8) | 0.088 |
| Pain location, n (%) | ||||
| Head | 5 (11.1) | 1 (7.7) | 4 (12.5) | 1.000 |
| Neck | 15 (33.3) | 3 (23.1) | 12 (37.5) | 0.492 |
| Arm | 7 (15.6) | 1 (7.7) | 6 (18.8) | 0.654 |
| Lower back | 25 (55.6) | 10 (76.9) | 15 (46.9) | 0.066 |
| Upper leg | 19 (42.2) | 5 (38.5) | 14 (43.8) | 0.745 |
| Lower leg | 12 (26.7) | 3 (23.1) | 9 (28.1) | 1.000 |
| Chest/abdomen | 4 (8.9) | 2 (15.4) | 2 (6.3) | 0.567 |
| Other | 10 (22.2) | 2 (15.4) | 8 (25.0) | 0.698 |
| PROMs Scores | ||||
| NRS, mean (SD) | 7.1 (1.7) | 6.8 (1.9) | 7.3 (1.6) | 0.391 |
| PCS, mean (SD) | 23.2 (11.9) | 26.8 (14.1) | 21.8 (10.9) | 0.207 |
| BPI REM mean (SD) | 11.6 (8.1) | 14.2 (9.6) | 10.5 (7.2) | 0.095 |
| BPI WAW, mean (SD) | 24.7 (10.0) | 25.6 (9.2) | 24.3 (10.5) | 0.440 |
| TSK, mean (SD) | 36.2 (6.0) | 39.6 (6.5) | 34.8 (5.2) | 0.013 * |
| TSK > 37, n (%) | 21 (46.7) | 9 (69.2) | 12 (37.5) | 0.053 |
| HADS-A, mean (SD) | 6.8 (3.8) | 8.2 (4.2) | 6.2 (3.6) | 0.125 |
| HADS-D, mean (SD) | 7.5 (4.9) | 9.2 (5.2) | 6.8 (4.7) | 0.127 |
| PHS, mean (SD) | 29.4 (6.8) | 29.6 (6.4) | 29.2 (7.0) | 0.862 |
| MHS, mean (SD) | 45.7 (12.1) | 43.1 (12.5) | 46.8 (12.0) | 0.367 |
| Model 2 AIC = 4476.42 | Model 5 a AIC = 4376.42 | |||||
|---|---|---|---|---|---|---|
| Estimate | CI | Sig. | Estimate | CI | Sig. | |
| Intercept | 9.08 | 6.47, 11.7 | 0.000 *** | 9.52 | 6.86, 12,18 | <0.001 *** |
| Fear-avoidance | −0.02 | −0.12, 0.09 | 0.78 | −0.04 | −0.14, 0.06 | 0.48 |
| Sex (men = 0; women = 1) | −0.53 | −1.96, 0.89 | 0.45 | −0.4 | −1.82, 1.02 | 0.57 |
| Fear-avoidance x sex | 0.18 | 0.05,0.31 | 0.005 ** | 0.18 | 0.06, 0.30 | 0.003 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waardenburg, S.; Visseren, L.; van Daal, E.; Brouwer, B.; van Zundert, J.; van Kuijk, S.M.J.; Lousberg, R.; Jongen, E.M.M.; Leue, C.; de Meij, N. Do Men and Women Have a Different Association between Fear-Avoidance and Pain Intensity in Chronic Pain? An Experience Sampling Method Cohort-Study. J. Clin. Med. 2022, 11, 5515. https://doi.org/10.3390/jcm11195515
Waardenburg S, Visseren L, van Daal E, Brouwer B, van Zundert J, van Kuijk SMJ, Lousberg R, Jongen EMM, Leue C, de Meij N. Do Men and Women Have a Different Association between Fear-Avoidance and Pain Intensity in Chronic Pain? An Experience Sampling Method Cohort-Study. Journal of Clinical Medicine. 2022; 11(19):5515. https://doi.org/10.3390/jcm11195515
Chicago/Turabian StyleWaardenburg, Sophie, Lars Visseren, Elke van Daal, Brigitte Brouwer, Jan van Zundert, Sander M. J. van Kuijk, Richel Lousberg, Ellen M. M. Jongen, Carsten Leue, and Nelleke de Meij. 2022. "Do Men and Women Have a Different Association between Fear-Avoidance and Pain Intensity in Chronic Pain? An Experience Sampling Method Cohort-Study" Journal of Clinical Medicine 11, no. 19: 5515. https://doi.org/10.3390/jcm11195515
APA StyleWaardenburg, S., Visseren, L., van Daal, E., Brouwer, B., van Zundert, J., van Kuijk, S. M. J., Lousberg, R., Jongen, E. M. M., Leue, C., & de Meij, N. (2022). Do Men and Women Have a Different Association between Fear-Avoidance and Pain Intensity in Chronic Pain? An Experience Sampling Method Cohort-Study. Journal of Clinical Medicine, 11(19), 5515. https://doi.org/10.3390/jcm11195515






