Reconstruction of Chronic Proximal Hamstring Tear: A Novel Surgical Technique with Semitendinosus Tendon Allograft Assisted with Autologous Plasma Rich in Growth Factors (PRGF)
Abstract
1. Introduction
2. Case Report and Description of the Technique
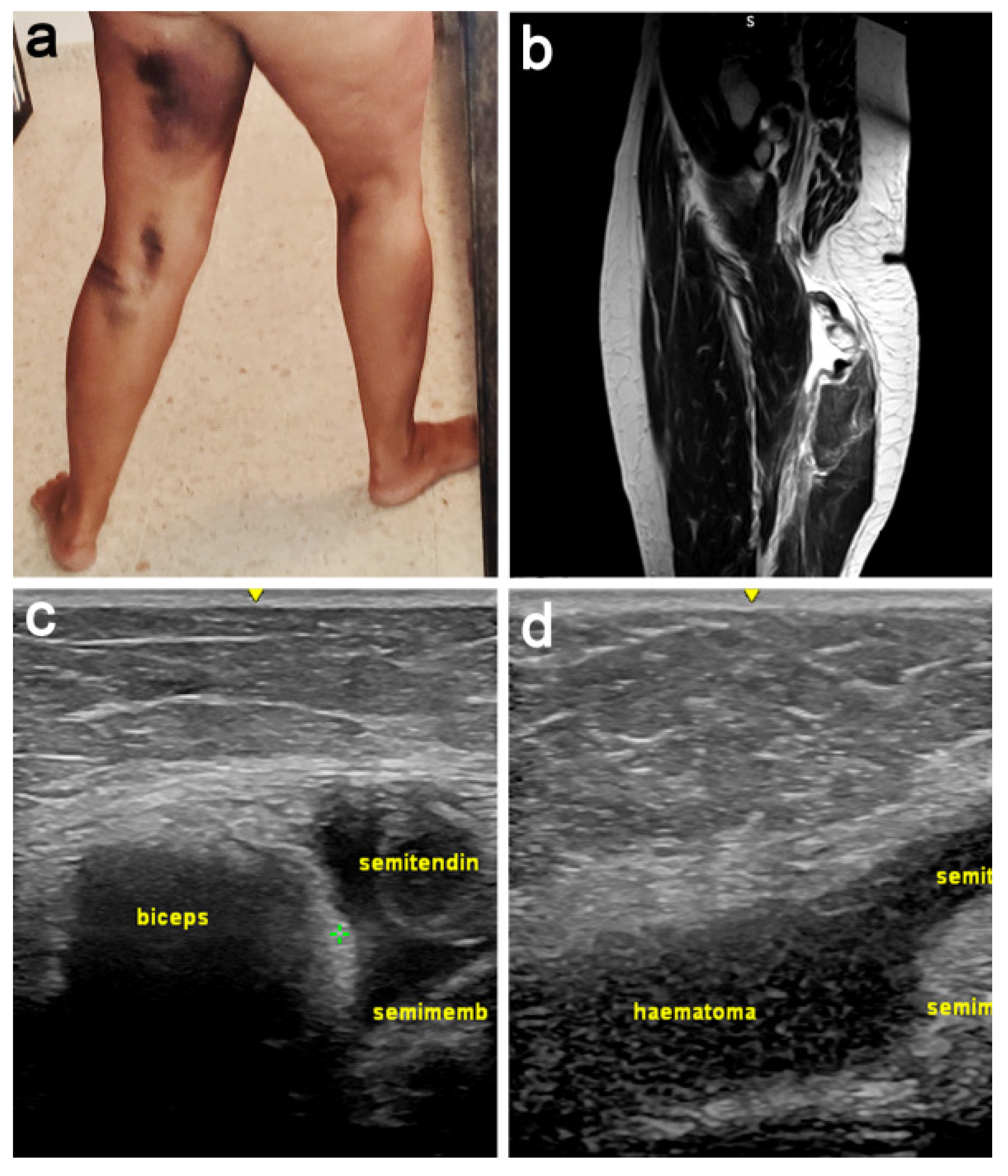
2.1. Patient Presentation and Examination
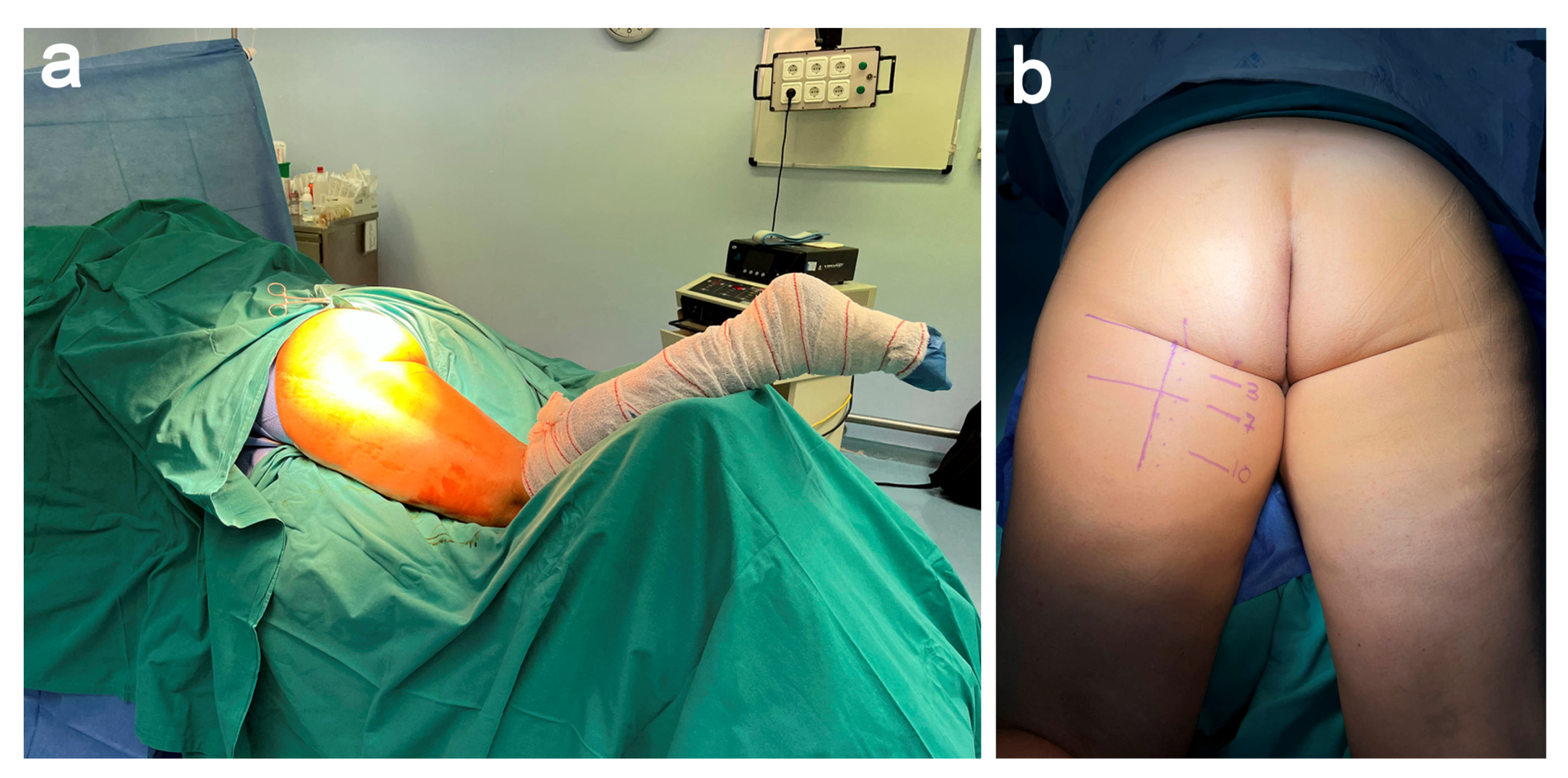
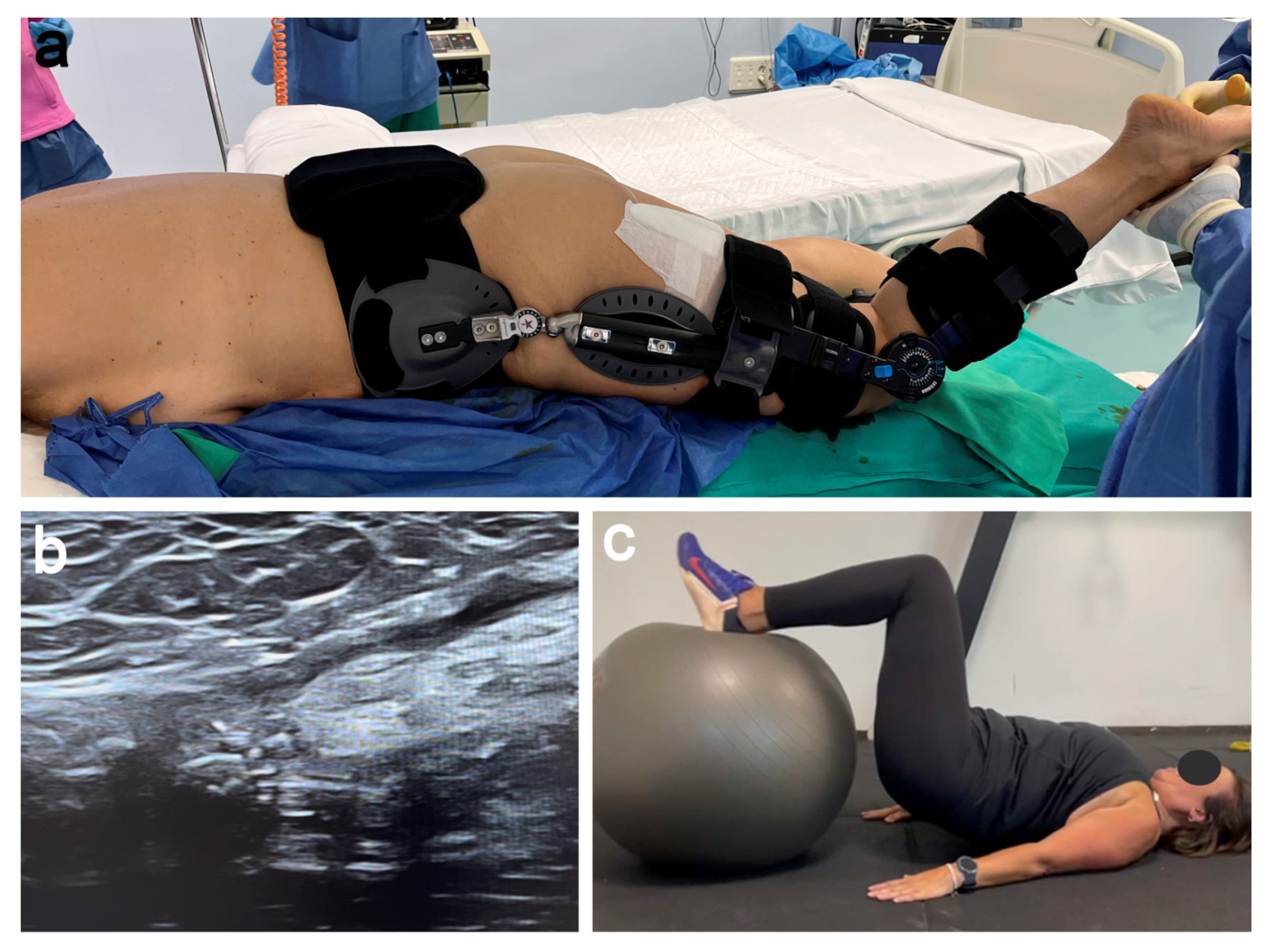
2.2. Patient Positioning
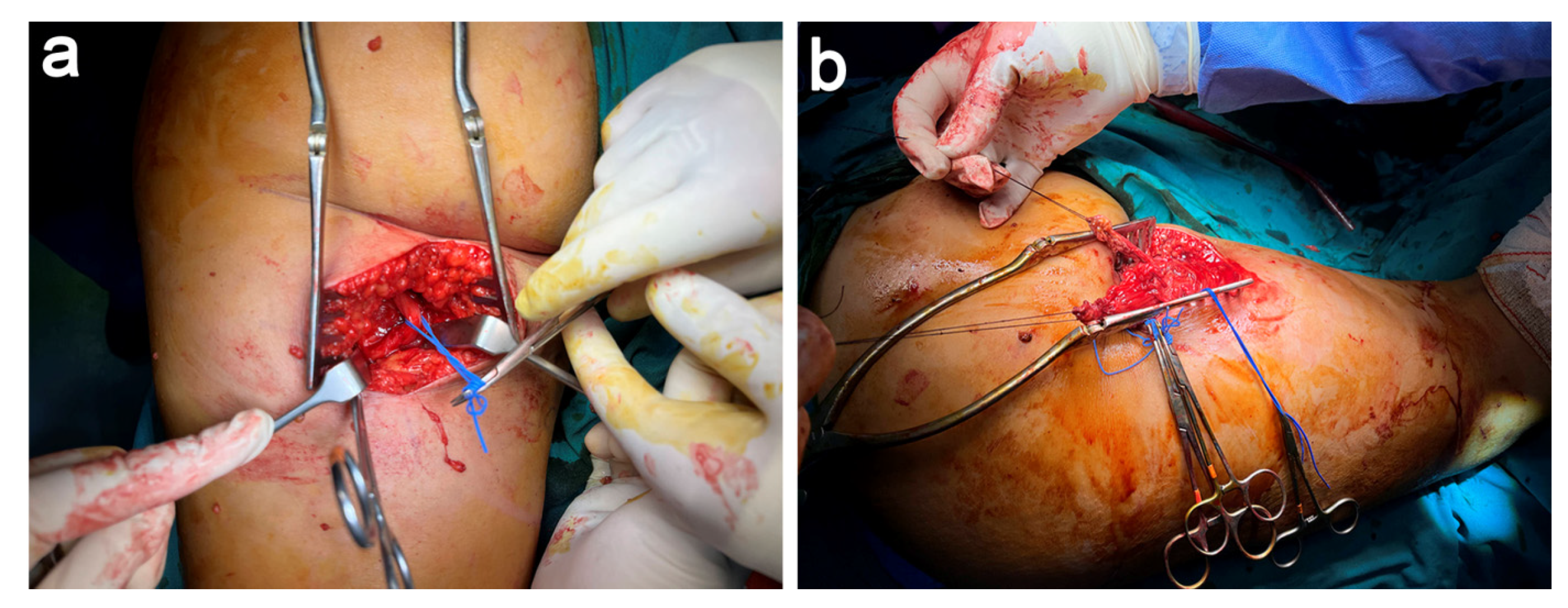
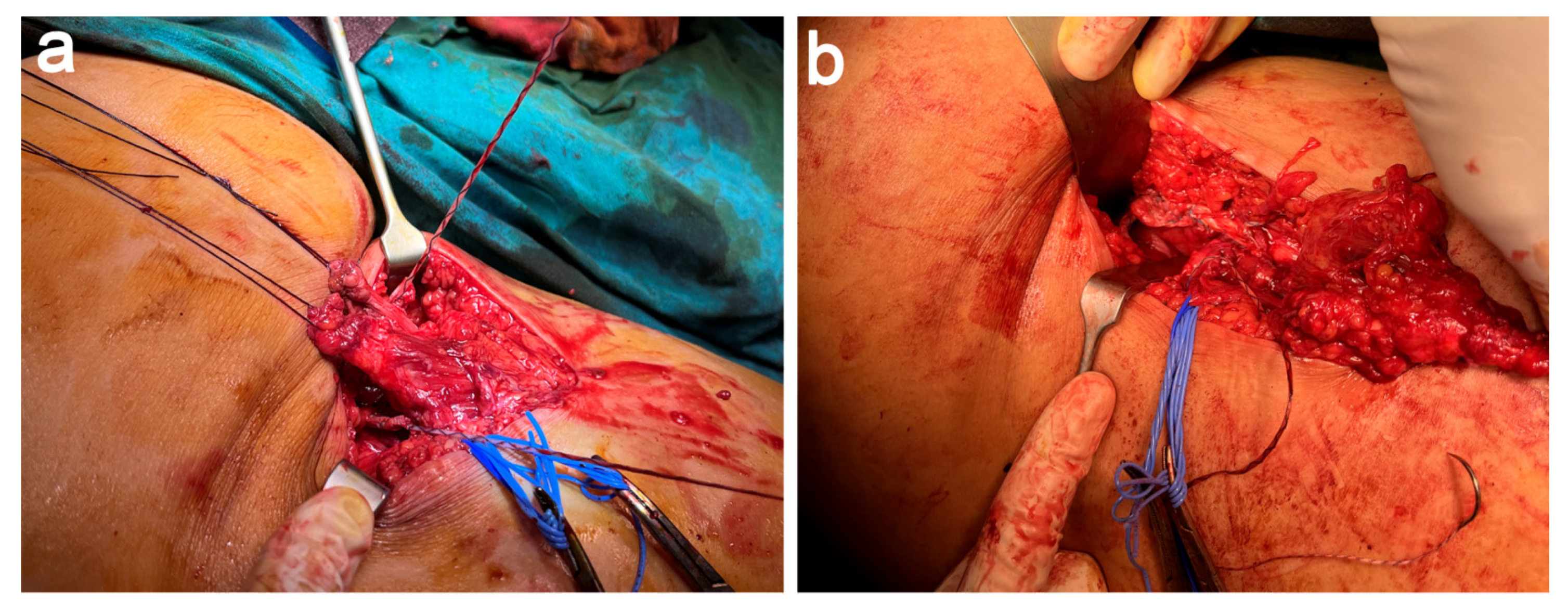
2.3. Dissection, Neurolysis, and Tenolysis
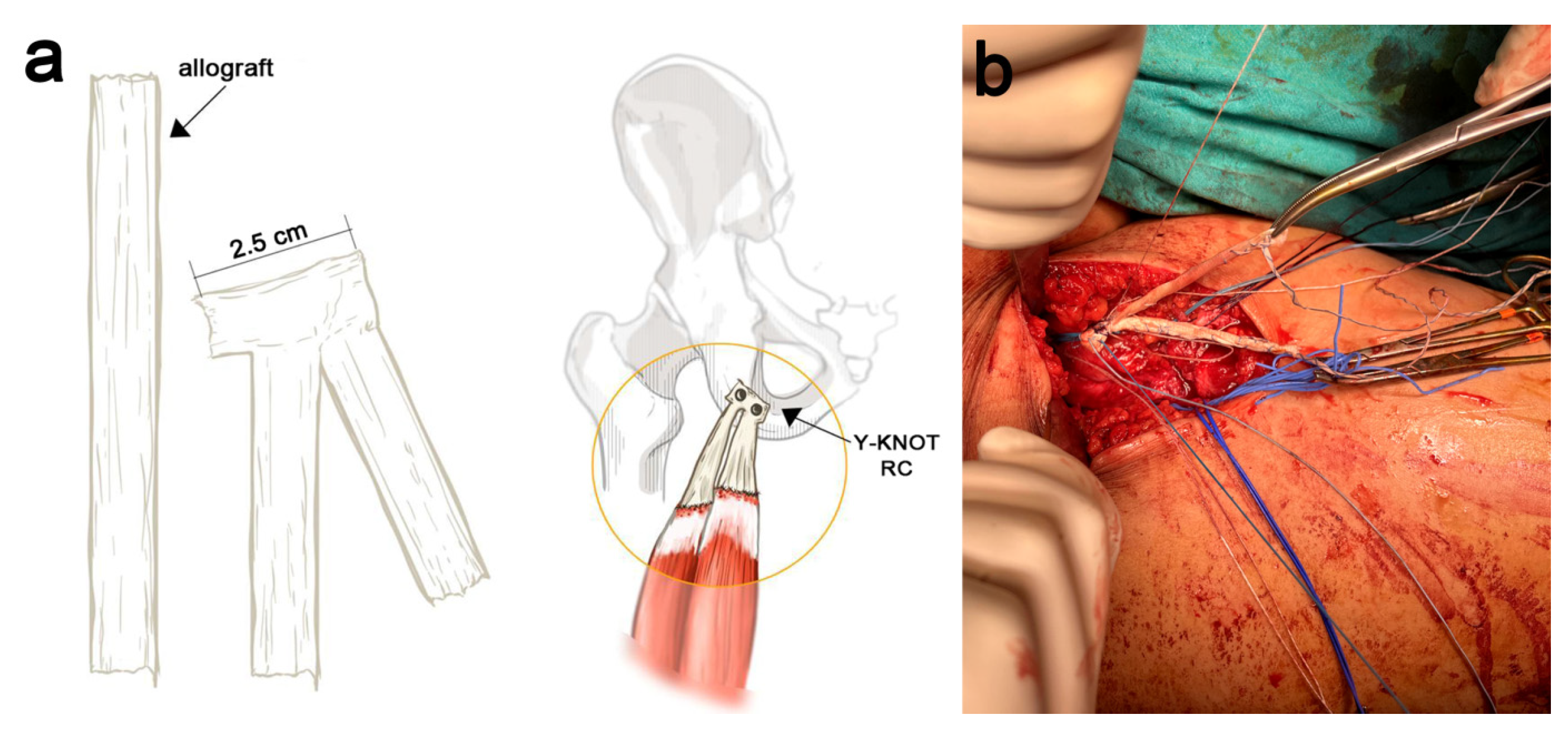
2.4. STT Allograft Preparation
2.5. STT Allograft Placement
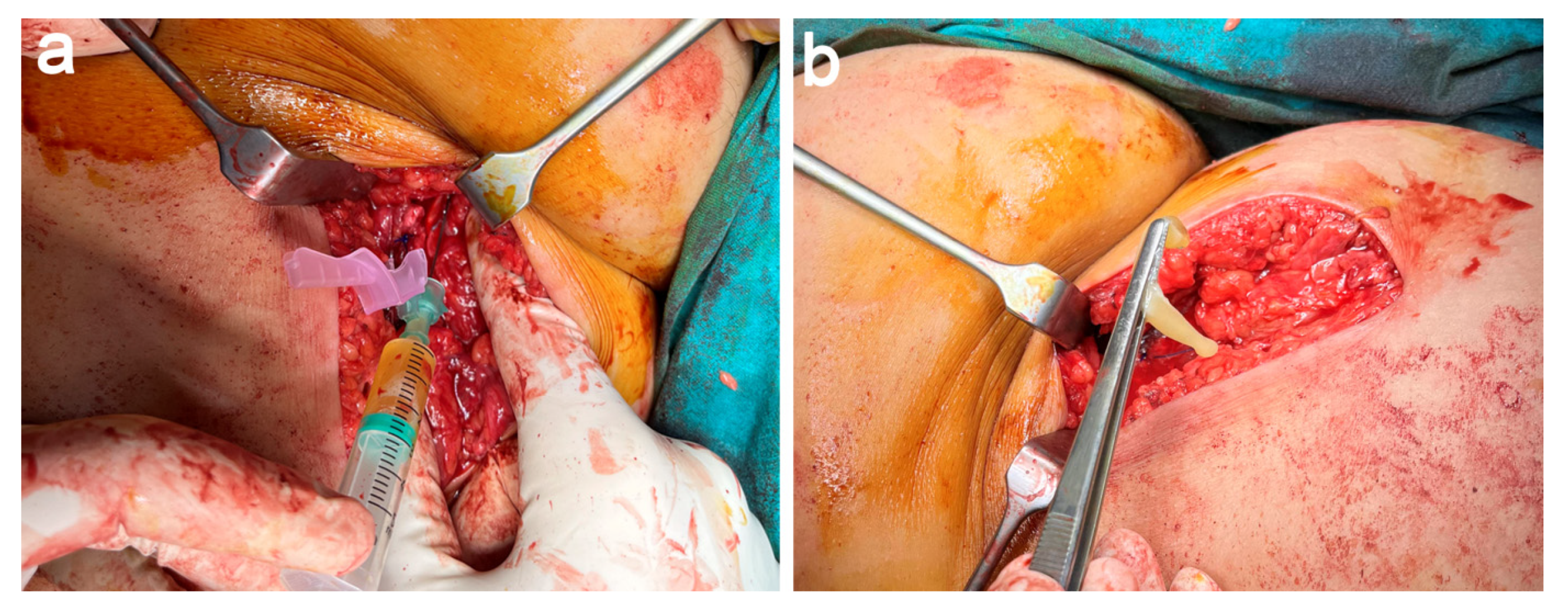
2.6. PRGF Preparation and Application
2.7. Postoperative Rehabilitation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| JT | Conjoined tendon |
| LBF | Long head of biceps femoris |
| PRGF | Plasma Rich in Growth Factors |
| PRP | Platelet-rich plasma |
| SMT | Tendon of semimembranous muscle |
| STT | Semitendinosus tendon |
References
- Matache, B.A.; Jazrawi, L. Surgical Management of Chronic Proximal Hamstring Tendon Tears. In Proximal Hamstring Tears: From Endoscopic Repair to Open Reconstruction; Youm, T., Ed.; Springer International Publishing: Cham, Switzerland, 2021. [Google Scholar]
- Grasso, M.; O’Neill, C.; Constantinescu, D.; Moatshe, G.; Vap, A. Reconstruction of Chronic Proximal Hamstring Tear: Description of a Surgical Technique. Arthrosc. Tech. 2021, 10, e1307–e1313. [Google Scholar] [CrossRef]
- Haskel, J.D. Surgical Treatment of Partial Proximal Hamstring Tendon Tears. In Proximal Hamstring Tears: From Endoscopic Repair to Open Reconstruction; Youm, T., Ed.; Springer International Publishing: Cham, Switzerland, 2021; pp. 45–55. [Google Scholar]
- Sanchez, M.; Anitua, E.; Azofra, J.; Andia, I.; Padilla, S.; Mujika, I. Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am. J. Sports Med. 2007, 35, 245–251. [Google Scholar] [CrossRef]
- Sanchez, M.; Anitua, E.; Delgado, D.; Prado, R.; Sanchez, P.; Fiz, N.; Guadilla, J.; Azofra, J.; Pompei, O.; Orive, G.; et al. Ultrasound-guided plasma rich in growth factors injections and scaffolds hasten motor nerve functional recovery in an ovine model of nerve crush injury. J. Tissue Eng. Regen. Med. 2017, 11, 1619–1629. [Google Scholar] [CrossRef]
- Wood, D.G.; Packham, I.; Trikha, S.P.; Linklater, J. Avulsion of the proximal hamstring origin. J. Bone Joint Surg. Am. 2008, 90, 2365–2374. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Prado, R.; Nurden, A.T.; Nurden, P. Characterization of Plasma Rich in Growth Factors (PRGF): Components and formulations. In Platelet Rich Plasma in Orthopaedics and Sports Medicine; Anitua, E., Cugat, R., Sánchez, M., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 29–45. [Google Scholar]
- Ebert, J.R.; Gormack, N.; Annear, P.T. Reconstruction of chronic proximal hamstring avulsion injuries using ipsilateral distal hamstring tendons results in good clinical outcomes and patient satisfaction. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2958–2966. [Google Scholar] [CrossRef] [PubMed]
- Rust, D.A.; Giveans, M.R.; Stone, R.M.; Samuelson, K.M.; Larson, C.M. Functional Outcomes and Return to Sports After Acute Repair, Chronic Repair, and Allograft Reconstruction for Proximal Hamstring Ruptures. Am. J. Sports Med. 2014, 42, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Moatshe, G.; Chahla, J.; Vap, A.R.; Ferrari, M.; Sanchez, G.; Mitchell, J.J.; LaPrade, R.F. Repair of Proximal Hamstring Tears: A Surgical Technique. Arthrosc. Tech. 2017, 6, e311–e317. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Nurden, P.; Prado, R.; Nurden, A.T.; Padilla, S. Autologous fibrin scaffolds: When platelet- and plasma-derived biomolecules meet fibrin. Biomaterials 2019, 192, 440–460. [Google Scholar] [CrossRef] [PubMed]
- Padilla, S.; Sanchez, M.; Vaquerizo, V.; Malanga, G.A.; Fiz, N.; Azofra, J.; Rogers, C.J.; Samitier, G.; Sampson, S.; Seijas, R.; et al. Platelet-Rich Plasma Applications for Achilles Tendon Repair: A Bridge between Biology and Surgery. Int. J. Mol. Sci. 2021, 22, 824. [Google Scholar] [CrossRef] [PubMed]
- De Vitis, R.; Passiatore, M.; Perna, A.; Fioravanti Cinci, G.; Taccardo, G. Comparison of Shape Memory Staple and Gelled Platelet-Rich Plasma versus Shape Memory Staple alone for the Treatment of Waist Scaphoid Nonunion: A Single-Center Experience. Joints 2019, 7, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, M.; Delgado, D.; Sanchez, P.; Fiz, N.; Azofra, J.; Orive, G.; Anitua, E.; Padilla, S. Platelet rich plasma and knee surgery. Biomed. Res. Int. 2014, 2014, 890630. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ríos Luna, A.; Fahandezh-Saddi Díaz, H.; Villanueva Martínez, M.; Bueno Horcajadas, Á.; Prado, R.; Anitua, E.; Padilla, S. Reconstruction of Chronic Proximal Hamstring Tear: A Novel Surgical Technique with Semitendinosus Tendon Allograft Assisted with Autologous Plasma Rich in Growth Factors (PRGF). J. Clin. Med. 2022, 11, 5443. https://doi.org/10.3390/jcm11185443
Ríos Luna A, Fahandezh-Saddi Díaz H, Villanueva Martínez M, Bueno Horcajadas Á, Prado R, Anitua E, Padilla S. Reconstruction of Chronic Proximal Hamstring Tear: A Novel Surgical Technique with Semitendinosus Tendon Allograft Assisted with Autologous Plasma Rich in Growth Factors (PRGF). Journal of Clinical Medicine. 2022; 11(18):5443. https://doi.org/10.3390/jcm11185443
Chicago/Turabian StyleRíos Luna, Antonio, Homid Fahandezh-Saddi Díaz, Manuel Villanueva Martínez, Ángel Bueno Horcajadas, Roberto Prado, Eduardo Anitua, and Sabino Padilla. 2022. "Reconstruction of Chronic Proximal Hamstring Tear: A Novel Surgical Technique with Semitendinosus Tendon Allograft Assisted with Autologous Plasma Rich in Growth Factors (PRGF)" Journal of Clinical Medicine 11, no. 18: 5443. https://doi.org/10.3390/jcm11185443
APA StyleRíos Luna, A., Fahandezh-Saddi Díaz, H., Villanueva Martínez, M., Bueno Horcajadas, Á., Prado, R., Anitua, E., & Padilla, S. (2022). Reconstruction of Chronic Proximal Hamstring Tear: A Novel Surgical Technique with Semitendinosus Tendon Allograft Assisted with Autologous Plasma Rich in Growth Factors (PRGF). Journal of Clinical Medicine, 11(18), 5443. https://doi.org/10.3390/jcm11185443






