Integrating High-Intensity Interval Training into a School Setting Improve Body Composition, Cardiorespiratory Fitness and Physical Activity in Children with Obesity: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
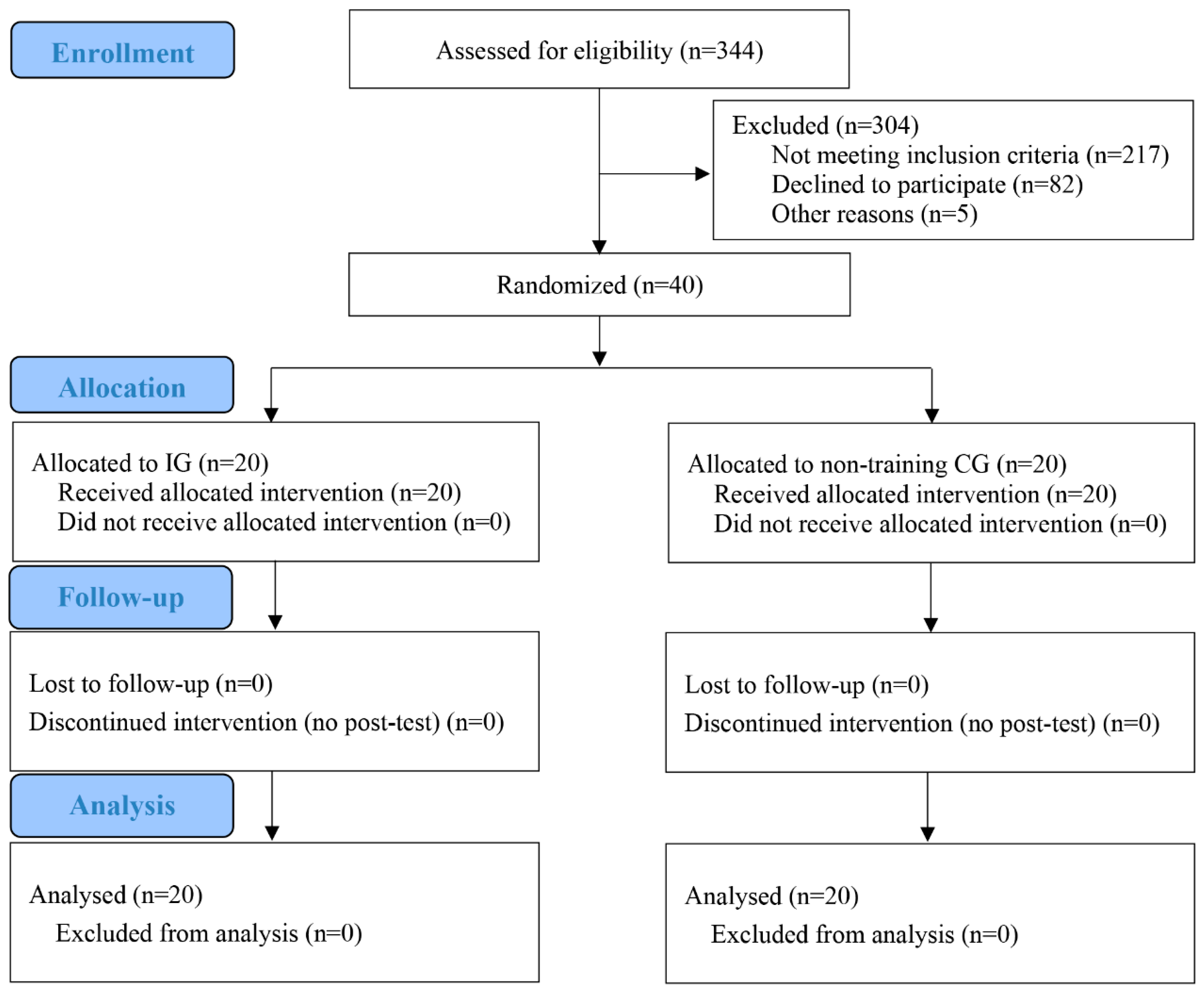
2.1. Study Design and Participants
2.2. Sample Size
2.3. Randomization and Blinding
2.4. Anthropometrics and Body Composition
2.5. Cardiorespiratory Fitness
2.6. Heart Rate
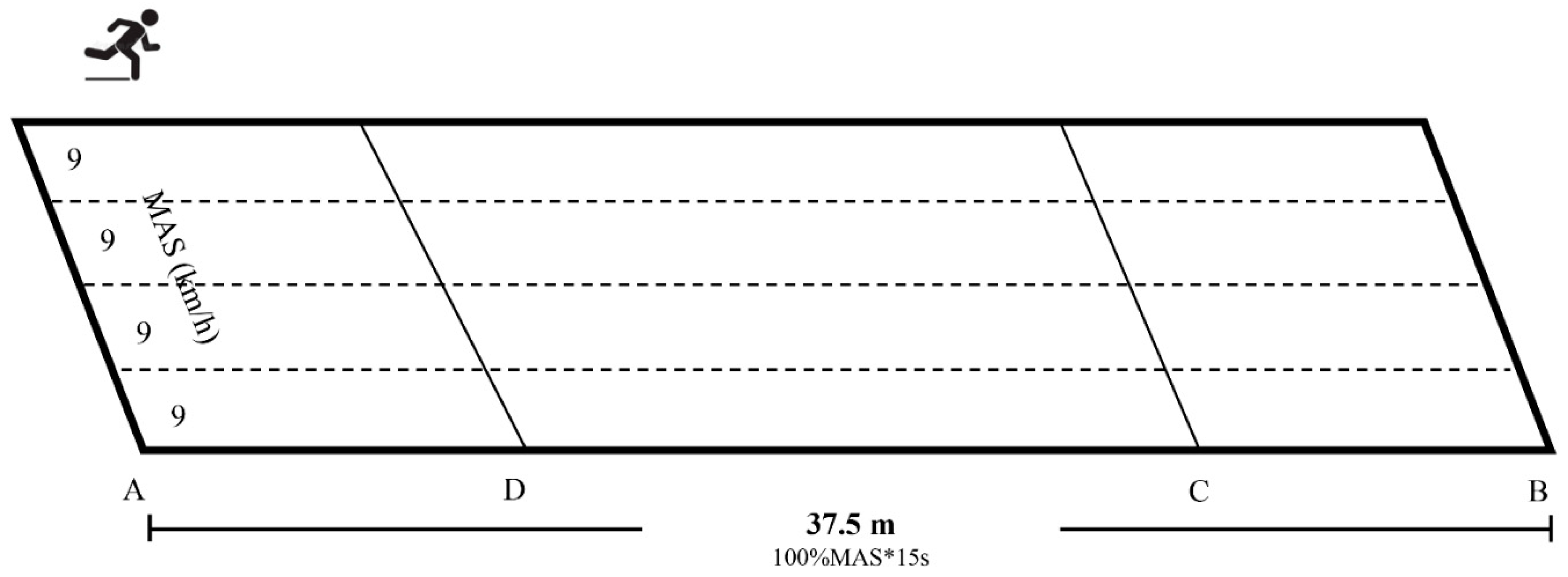
2.7. Exercise Interventions
2.8. Statistical Analysis
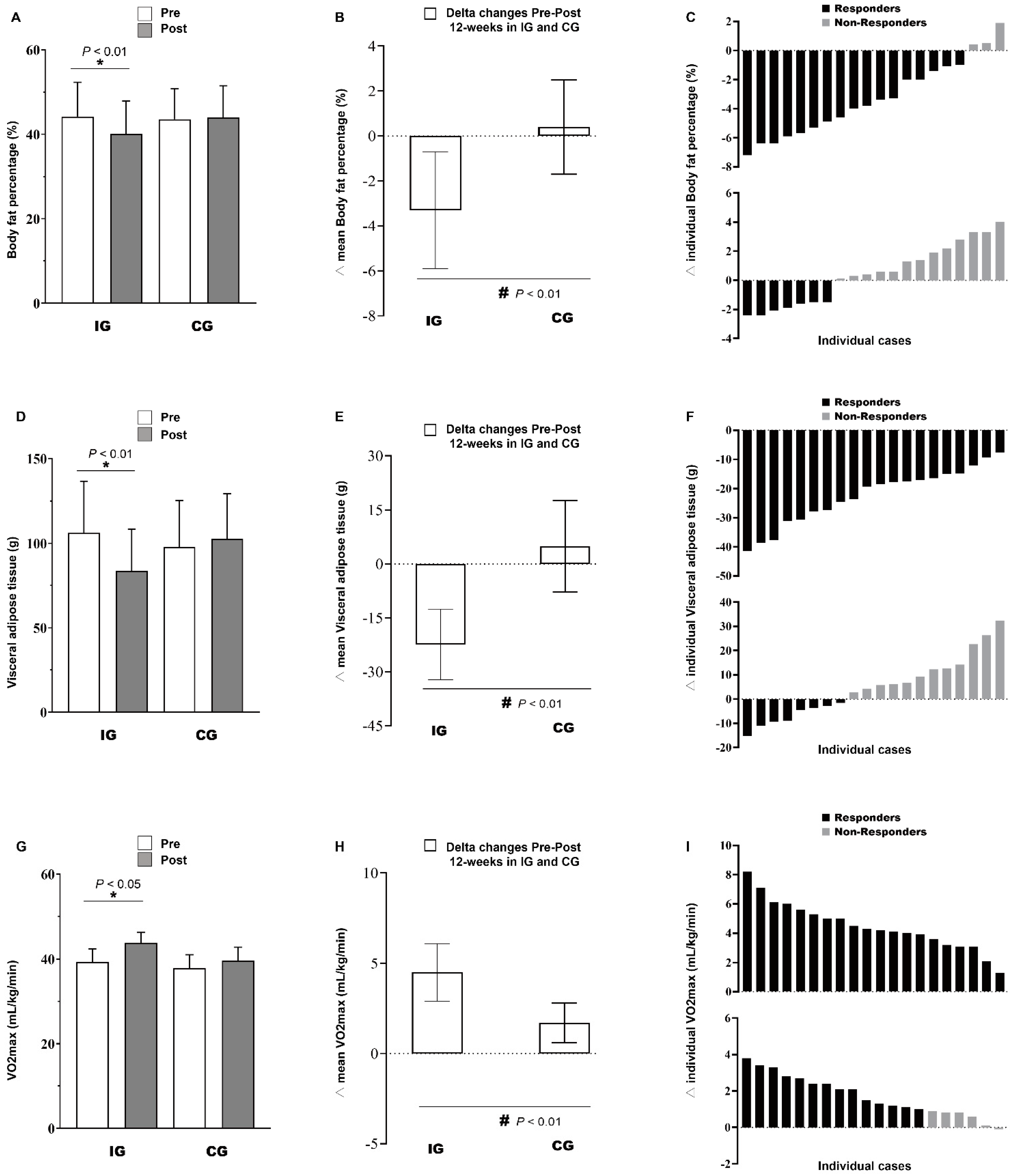
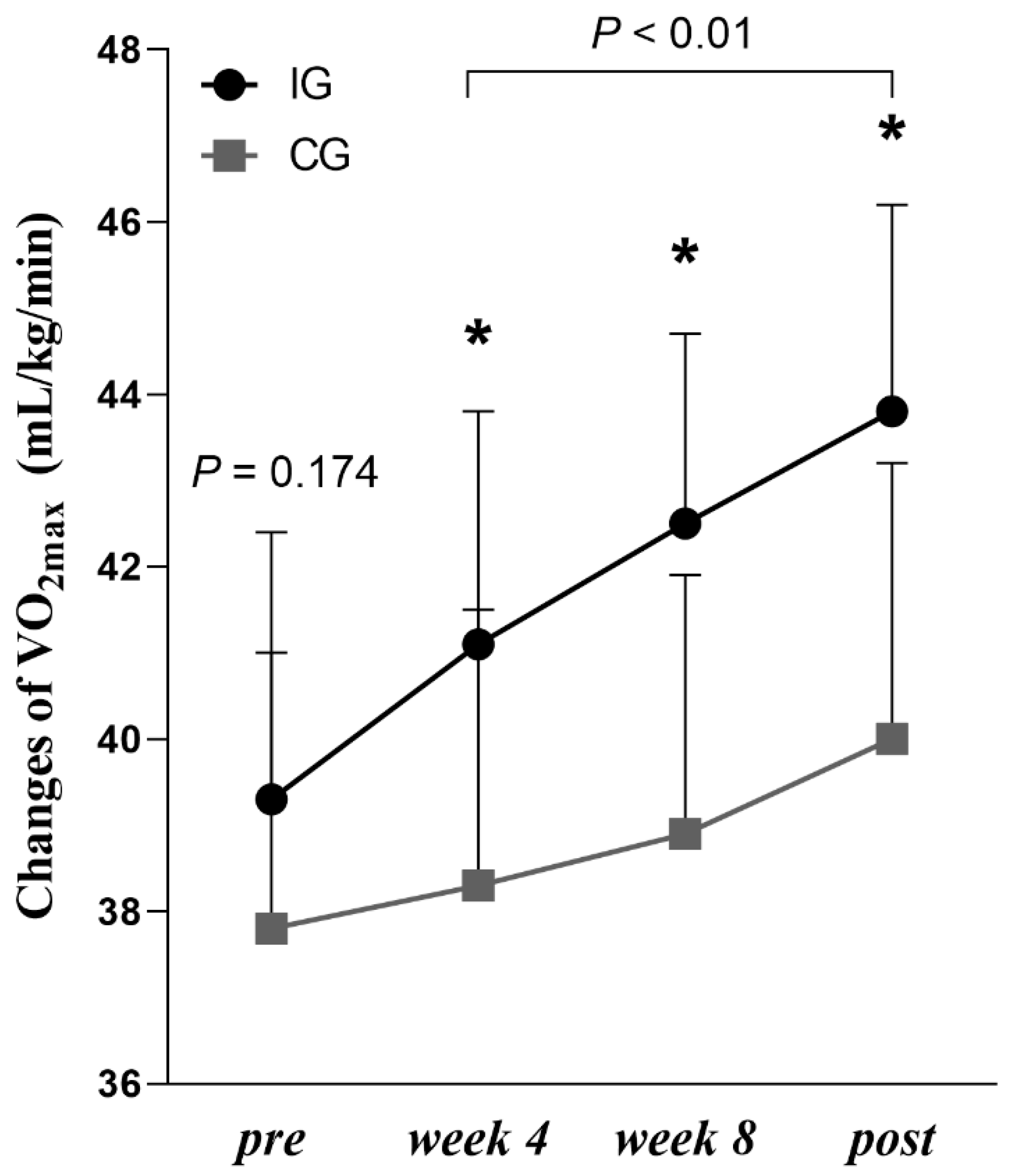
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Lobstein, T.; Jackson-Leach, R.; Moodie, M.; Hall, K.; Gortmaker, S.; Swinburn, B.; James, W.; Wang, Y.; McPherson, K. Child and adolescent obesity: Part of a bigger picture. Lancet 2015, 385, 2510–2520. [Google Scholar] [CrossRef]
- Brisbois, T.D.; Farmer, A.P.; McCargar, L.J. Early markers of adult obesity: A review. Obes. Rev. 2012, 13, 347–367. [Google Scholar] [CrossRef]
- Carbone, S.; Del Buono, M.G.; Ozemek, C.; Lavie, C.J. Obesity, risk of diabetes and role of physical activity, exercise training and cardiorespiratory fitness. Prog. Cardiovasc. Dis. 2019, 62, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Weihrauch-Bluher, S.; Wiegand, S. Risk Factors and Implications of Childhood Obesity. Curr. Obes. Rep. 2018, 7, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Neeland, I.J.; Ross, R.; Despres, J.P.; Matsuzawa, Y.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: A position statement. Lancet Diabetes Endocrinol. 2019, 7, 715–725. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Batacan, R.B., Jr.; Duncan, M.J.; Dalbo, V.J.; Tucker, P.S.; Fenning, A.S. Effects of high-intensity interval training on cardiometabolic health: A systematic review and meta-analysis of intervention studies. Br. J. Sports Med. 2017, 51, 494–503. [Google Scholar] [CrossRef]
- Miguet, M.; Fearnbach, N.S.; Metz, L.; Khammassi, M.; Julian, V.; Cardenoux, C.; Pereira, B.; Boirie, Y.; Duclos, M.; Thivel, D. Effect of HIIT versus MICT on body composition and energy intake in dietary restrained and unrestrained adolescents with obesity. Appl. Physiol. Nutr. Metab. 2020, 45, 437–445. [Google Scholar] [CrossRef]
- Cao, M.; Quan, M.; Zhuang, J. Effect of high-intensity interval training versus moderate-intensity continuous training on cardiorespiratory fitness in children and adolescents: A meta-analysis. Int. J. Environ. Res. Public Health 2019, 16, 1533. [Google Scholar] [CrossRef]
- Ketelhut, S.; Roglin, L.; Martin-Niedecken, A.L.; Nigg, C.R.; Ketelhut, K. Integrating regular exergaming sessions in the exercube into a school setting increases physical fitness in elementary school children: A randomized controlled trial. J. Clin. Med. 2022, 11, 1570. [Google Scholar] [CrossRef]
- Dobbins, M.; Husson, H.; DeCorby, K.; LaRocca, R.L. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013, 2013, CD007651. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Floody, P.; Latorre-Román, P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; García-Pinillos, F. Feasibility of incorporating high-intensity interval training into physical education programs to improve body composition and cardiorespiratory capacity of overweight and obese children: A systematic review. J. Exerc. Sci. Fit. 2019, 17, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Costigan, S.; Eather, N.; Plotnikoff, R.; Taaffe, D.; Lubans, D. High-intensity interval training for improving health-related fitness in adolescents: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1253–1261. [Google Scholar] [CrossRef]
- Dias, K.; Ingul, C.; Tjønna, A.; Keating, S.; Gomersall, S.; Follestad, T.; Hosseini, M.; Hollekim-Strand, S.; Ro, T.; Haram, M. Effect of high-intensity interval training on fitness, fat mass and cardiometabolic biomarkers in children with obesity: A randomised controlled trial. Sports Med. 2017, 48, 733–746. [Google Scholar] [CrossRef]
- Chuensiri, N.; Suksom, D.; Tanaka, H. Effects of High-Intensity Intermittent Training on Vascular Function in Obese Preadolescent Boys. Child Obes. 2018, 14, 41–49. [Google Scholar] [CrossRef]
- Duncombe, S.; Barker, A.; Bond, B.; Earle, R. School-based high-intensity interval training programs in children and adolescents: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0266427. [Google Scholar] [CrossRef] [PubMed]
- Meng, C.; Yucheng, T.; Shu, L.; Yu, Z. Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: A randomized controlled trial. BMC Pediatr. 2022, 22, 112. [Google Scholar] [CrossRef]
- Paahoo, A.; Tadibi, V.; Behpoor, N. Effectiveness of Continuous Aerobic Versus High-Intensity Interval Training on Atherosclerotic and Inflammatory Markers in Boys with Overweight/Obesity. Pediatr. Exerc. Sci. 2021, 33, 132–138. [Google Scholar] [CrossRef]
- Warburton, D.; Jamnik, V.; Bredin, S. Evidence-based risk assessment and recommendations for physical activity clearance: An introduction. Appl. Physiol. Nutr. Metab. 2011, 36 (Suppl. S1), S1–S2. [Google Scholar] [CrossRef]
- Ji, C.Y. Report on childhood obesity in China (1)—body mass index reference for screening overweight and obesity in Chinese school-age children. Biomed. Environ. Sci. 2005, 18, 390–400. [Google Scholar]
- Tjønna, A.; Stølen, T.; Bye, A. Aerobic interval training reduces cardiovascular risk factors more than a multitreatment approach in overweight adolescents. Clin. Sci. (Lond.) 2009, 116, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Fujitani, K.; Tsujinaka, T. InBody 720 as a new method of evaluating visceral obesity. Hepatogastroenterology 2011, 58, 42–44. [Google Scholar] [PubMed]
- Mariana, B.; Edilson, S.; Miguel, A. Validity of equations for estimating VO2peak from the 20-m shuttle run test in adolescents aged 11-13 years. J. Strength Cond. Res. 2013, 27, 2774–2781. [Google Scholar]
- Mahar, M.T.; Guerieri, A.M.; Hanna, M.S.; Kemble, C.D. Estimation of aerobic fitness from 20-m multistage shuttle run test performance. Am. J. Prev. Med. 2011, 41 (Suppl. 2), S117–S123. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Bogataj, Š.; Trajković, N.; Cadenas-Sanchez, C.; Sember, V. Effects of school-based exercise and nutrition intervention on body composition and physical fitness in overweight adolescent girls. Nutrients 2021, 13, 238. [Google Scholar] [CrossRef]
- Plavsic, L.; Knezevic, O.M.; Sovtic, A.; Minic, P.; Vukovic, R.; Mazibrada, I.; Stanojlovic, O.; Hrncic, D.; Rasic-Markovic, A.; Macut, D. Effects of high-intensity interval training and nutrition advice on cardiometabolic markers and aerobic fitness in adolescent girls with obesity. Appl. Physiol. Nutr. Metab. 2020, 45, 294–300. [Google Scholar] [CrossRef]
- Starkoff, B.E.; Eneli, I.U.; Bonny, A.E.; Hoffman, R.P.; Devor, S.T. Estimated aerobic capacity changes in adolescents with obesity following high intensity interval exercise. Int. J. Kinesiol. Sports Sci. 2014, 2, 2202–2946. [Google Scholar]
- Weston, K.L.; Azevedo, L.B.; Bock, S.; Weston, M.; George, K.P.; Batterham, A.M. Effect of novel, school-based high-intensity interval training (hit) on cardiometabolic health in adolescents: Project FFAB (fun fast activity blasts)-an exploratory controlled before-and-after trial. PLoS ONE 2016, 11, e0159116. [Google Scholar] [CrossRef]
- Raine, L.B.; Khan, N.A.; Drollette, E.S.; Pontifex, M.B.; Kramer, A.F.; Hillman, C.H. Obesity, visceral adipose tissue, and cognitive function in childhood. J. Pediatr. 2017, 187, 134–140. [Google Scholar] [CrossRef]
- Vissers, D.; Hens, W.; Hansen, D.; Taeymans, J. The effect of diet or exercise on visceral adipose tissue in overweight youth. Med. Sci. Sports Exerc. 2016, 48, 1415–1424. [Google Scholar] [CrossRef] [PubMed]
- Wedell-Neergaard, A.; Lehrskov, L.; Christensen, R. Exercise-induced changes in visceral adipose tissue mass are regulated by il-6 signaling: A randomized controlled trial. Cell Metab. 2019, 29, 844–855. [Google Scholar] [CrossRef] [PubMed]
- Raghuveer, G.; Hartz, J.; Lubans, D.R.; Takken, T.; Wiltz, J.L.; Mietus-Snyder, M.; Perak, A.M.; Baker-Smith, C.; Pietris, N.; Edwards, N.M.; et al. Cardiorespiratory fitness in youth: An important marker of health: A scientific statement from the american heart association. Circulation 2020, 142, e101–e118. [Google Scholar] [CrossRef] [PubMed]
- Thivel, D.; Masurier, J.; Baquet, G.; Timmons, B.W.; Pereira, B.; Berthoin, S.; Duclos, M.; Aucouturier, J. High-intensity interval training in overweight and obese children and adolescents: Systematic review and meta-analysis. J. Sports Med. Phys. Fit. 2019, 59, 310–324. [Google Scholar] [CrossRef]
- Astorino, T.; Edmunds, R.; Clark, A. High-intensity interval training increases cardiac output and VO2max. Med. Sci. Sports Exerc. 2017, 49, 265–273. [Google Scholar] [CrossRef]
| Total (n = 40) | IG (n = 20) | CG (n = 20) | |
|---|---|---|---|
| Boys/Girls (n) | 20/20 | 10/10 | 10/10 |
| Age (years) | 11.0 ± 0.6 | 11.2 ± 0.7 | 10.9 ± 0.4 |
| Height (m) | 1.52 ± 0.07 | 1.53 ± 0.08 | 1.51 ± 0.05 |
| Body Mass (kg) | 54.6 ± 5.7 | 55.9 ± 6.9 | 53.3 ± 4.0 |
| Body Mass Index (kg/m2) | 23.6 ± 1.5 | 23.4 ± 1.6 | 23.8 ± 1.5 |
| Outcomes | IG (n = 20) | CG (n = 20) | p-Value | Interaction η2 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Δ | Pre | Post | Δ | Group | Time | Interaction | ||
| BM (kg) | 55.9 ± 6.9 | 52.5 ± 6.2 * | −3.4 ± 1.4 # | 53.3 ± 4.0 | 53.6 ± 4.3 | 0.2 ± 1.5 | 0.655 | 0.001 | 0.001 | 0.625 |
| BMI (kg/m2) | 23.4 ± 1.6 | 21.7 ± 1.5 *, # | −1.7 ± 0.5 # | 23.8 ± 1.5 | 23.5 ± 1.7 | −0.3 ± 0.7 | 0.037 | 0.001 | 0.001 | 0.575 |
| %BF (%) | 44.2 ± 8.1 | 40.1 ± 7.8 *, # | −3.3 ± 2.6 # | 43.6 ± 7.2 | 44.0 ± 7.5 | 0.4 ± 2.1 | 0.497 | 0.001 | 0.001 | 0.541 |
| FM (kg) | 24.8 ± 6.0 | 21.2 ± 5.1 * | −3.2 ± 1.4 # | 23.3 ± 4.6 | 23.7 ± 5.0 | 0.4 ± 1.3 | 0.756 | 0.001 | 0.001 | 0.691 |
| FFM (kg) | 21.3 ± 5.0 | 21.3 ± 5.3 | 0.1 ± 1.5 | 21.2 ± 2.9 | 21.8 ± 3.1 | 0.6 ± 0.6 | 0.858 | 0.074 | 0.142 | 0.056 |
| VAT (cm2) | 106.2 ± 30.6 | 83.8 ± 24.6 *, # | −22.4 ± 9.8 # | 97.8 ± 27.5 | 102.7 ± 26.6 | 4.9 ± 12.7 | 0.539 | 0.001 | 0.001 | 0.605 |
| 20-mSRT (m) | 483.0 ± 139.8 | 690.0 ±100.2 *, # | 207.0 ± 90.4 # | 414.0 ± 126.0 | 500.0 ± 137.2 * | 86.0 ± 60.2 | 0.002 | 0.001 | 0.001 | 0.395 |
| VO2max (mL/kg/min) | 39.3 ± 3.1 | 43.8 ± 2.4 *, # | 4.5 ± 1.6 # | 37.8 ± 3.2 | 39.6 ± 3.2 * | 1.7 ± 1.1 | 0.004 | 0.001 | 0.001 | 0.505 |
| HRmax (b.p.m) | 201.4 ± 5.2 | 198.4 ± 5.3 * | −3.0 ± 3.2 | 200.3 ± 3.5 | 199.2 ± 4.4 | −1.1 ± 3.7 | 0.849 | 0.053 | 0.089 | 0.074 |
| HRrest (b.p.m) | 76.9 ± 4.0 | 74.3 ± 3.3 * | −2.7 ± 2.6 # | 75.6 ± 3.0 | 74.9 ± 2.1 | −0.7 ± 1.6 | 0.624 | 0.023 | 0.005 | 0.186 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, M.; Tang, Y.; Zou, Y. Integrating High-Intensity Interval Training into a School Setting Improve Body Composition, Cardiorespiratory Fitness and Physical Activity in Children with Obesity: A Randomized Controlled Trial. J. Clin. Med. 2022, 11, 5436. https://doi.org/10.3390/jcm11185436
Cao M, Tang Y, Zou Y. Integrating High-Intensity Interval Training into a School Setting Improve Body Composition, Cardiorespiratory Fitness and Physical Activity in Children with Obesity: A Randomized Controlled Trial. Journal of Clinical Medicine. 2022; 11(18):5436. https://doi.org/10.3390/jcm11185436
Chicago/Turabian StyleCao, Meng, Yucheng Tang, and Yu Zou. 2022. "Integrating High-Intensity Interval Training into a School Setting Improve Body Composition, Cardiorespiratory Fitness and Physical Activity in Children with Obesity: A Randomized Controlled Trial" Journal of Clinical Medicine 11, no. 18: 5436. https://doi.org/10.3390/jcm11185436
APA StyleCao, M., Tang, Y., & Zou, Y. (2022). Integrating High-Intensity Interval Training into a School Setting Improve Body Composition, Cardiorespiratory Fitness and Physical Activity in Children with Obesity: A Randomized Controlled Trial. Journal of Clinical Medicine, 11(18), 5436. https://doi.org/10.3390/jcm11185436










