Abstract
Background and aims: To compare the value of three commonly used cardiovascular short-term risk scoring models, the GRACE score, TIMI score, and HEART score, in predicting the long-term prognosis of patients with acute myocardial infarction. Methods: The hospitalization data of patients who were hospitalized in West China Hospital of Sichuan University from 2011 to 2013 and diagnosed with acute myocardial infarction (AMI) were collected. The patients were scored by GRACE score, TIMI score, and HEART score. The long-term follow-up of patients was conducted until the end of January 2021. All-cause death and time of death of patients were confirmed by telephone follow-up, electronic medical record query, and household registration information. The predictive ability of different risk scores for long-term prognosis was compared according to the receiver operating characteristic (ROC) area under the curve (AUC), and the ability to distinguish patients with different risk levels was compared according to Kaplan–Meier survival curves. Results: The study ultimately included 2220 patients, with a median follow-up of 8 years and 454 (20.5%) deaths until the end of follow-up. Whether in ST-segment elevation myocardial infarction (STEMI) patients or non-ST-segment elevation myocardial infarction (NSTEMI) patients, the AUC value of the GRACE score (both AUC = 0.734) was significantly higher than the TIMI score (AUC = 0.675, p < 0.01; AUC = 0.665, p < 0.01) and HEART score (AUC = 0.632, p < 0.01; AUC = 0.611, p < 0.01) until the end of follow-up. In terms of risk stratification, the Kaplan–Meier survival curve shows that both THE GRACE score and TIMI score can distinguish AMI patients with different risk levels (p < 0.01), but the risk stratification ability of the HEART score in AMI patients was poor (p > 0.05). Conclusion: The GRACE risk score could represent a more accurate model to assess long-term death of acute myocardial infarction, but further studies are required.
1. Introduction
Cardiovascular disease is the leading cause of death worldwide. In Europe, more than 4 million people die each year from cardiovascular disease, of which nearly 1.8 million die from coronary artery diseases, accounting for 20% of all deaths in Europe [1]. Of all coronary artery diseases, acute myocardial infarction (AMI) is the most serious, with approximately 700,000 Americans experiencing AMI and another approximately 300,000 experiencing recurrent events each year in the United States [2,3,4,5]. In China, the total hospitalization cost of ischemic heart disease in 2018 was USD16.296 billion including 23.567 billion yuan for AMI, and the average annual growth rate of AMI hospitalization cost was as high as 26.89% [6]. Although reperfusion therapy and early pharmacological treatment have led to a significant reduction in AMI mortality over the past 30 years, the AMI in-hospital mortality has remained higher than 4% until now [2,3,4,5]. Mortality in AMI patients is associated with many factors, and understanding the associated risk factors can help develop clinical strategies and provide valuable prognostic information to clinicians and patients. Researchers have developed many risk scoring models that are based on different risk factors over the past 20 years, and risk scoring models can help clinicians to risk stratify patients and predict the risk of death and/or the incidence of adverse events in patients [7]. Currently, risk scoring models have become an important part of clinical work and the 2018 ESC guidelines also recommend the use of risk scores for risk stratification of AMI patients [8].
The GRACE score, the TIMI score, and the HEART score are three of the most widely used scoring models [9,10,11,12]. The GRACE score focuses on in-hospital deaths of patients and its area under the curve (AUC) for predicting in-hospital death reached 0.83 and 0.84 in the model building and validation cohorts, respectively [9]. The TIMI score has two different risk models for patients with non-ST-segment elevation infarction (NSTEMI) and patients with ST-segment elevation infarction (STEMI). The TIMI score for NSTEMI predicts a composite endpoint event consisting of all-cause death, new or recurrent MI, and urgent revascularization within 14 days and has been validated in other cohorts [10,13]. The TIMI score for STEMI has an AUC value of 0.78 for predicting 30-day death and has been validated in community populations, with similar predictive accuracy in patients that are undergoing percutaneous coronary intervention (PCI) [14]. The HEART score focuses on the risk of major adverse cardiac events and death in the short term, with endpoint event rates of 2.5%, 20.3%, and 72.7% for patients that are at low, intermediate, and high-risk, respectively [12]. Its predictive power has been validated in two other studies [15,16].
In addition to the three scores that are mentioned above, other cardiovascular risk scoring models that are widely used in clinical practice also focus mostly on the in-hospital mortality and short-term adverse event rates of patients [7]. However, in addition to the short-term prognosis, the more distant prognosis of AMI also deserves our attention. Data from the ESC national registry show that the average in-hospital mortality rate of STEMI patients is approximately 5%, while data from the angiographic registry show that the 1-year mortality rate of STEMI patients reaches 10% [17,18,19]. The CHINA PEACE study showed that the in-hospital mortality rate of Chinese STEMI patients is approximately 7–9% and a 1-year mortality rate of up to 28% [20]. All of these findings suggest the importance of assessing the long-term prognosis of AMI patients. Although there are some risk scoring models that can be used to predict the long-term prognosis of patients with coronary artery disease, such as the PAMI score and the CADILLAC score, the former excludes patients with cardiogenic shock, recent stroke, end-stage renal failure, and a life expectancy <1 year, and the latter excludes patients with cardiogenic shock, complex coronary anatomy, and emergency PCI, and therefore, does not reflect the true characteristics of this patient population and is not widely used in the clinic [21,22]. Therefore, assessing the value of the short-term risk scoring model, which is currently widely used in clinical practice, in predicting the long-term prognosis of AMI patients may be a more convenient and rapid approach, while previous studies in this area are very limited, and all suffer from small study samples, short follow-up periods, and inconsistent findings [23,24,25,26].
Therefore, the purpose of this study was to evaluate and compare the accuracy and risk stratification performance of three clinically widely used short-term risk scoring models, the GRACE score, the TIMI score, and the HEART score, in predicting the long-term death of patients with AMI.
2. Methods
2.1. Study Population
This study was approved by the Clinical Trials and Biomedical Ethics Committee of West China Hospital of Sichuan University, No. 2012 (243). The West China Hospital of Sichuan University is a national-level medical center in western China. It has 2 medical centers and 4300 beds. The annual number of outpatient and emergency department visits is 7.75 million, with 283,000 discharged patients and 196,000 surgeries. Patients with acute myocardial infarction that were hospitalized at West China Hospital of Sichuan University from January 2011 to December 2013 were included retrospectively and consecutively. The inclusion criteria were: (i) age > 18 years, and (ii) diagnosis of “acute ST-segment elevation myocardial infarction” or “acute non-ST-segment elevation myocardial infarction” during hospitalization, with the diagnostic criteria based on the third global definition of myocardial infarction. The exclusion criteria were: (i) the type of infarction diagnosis was unclear, (ii) in-hospital death or automatic discharge due to abandonment of treatment in critical condition, or (iii) death after less than 30 days of follow-up at discharge. All hospitalized AMI patients received standard guideline-based treatment.
2.2. Data Collection
The information system of West China Hospital of Sichuan University and the laboratory information system were used to collect the clinical data and laboratory test results of patients. The data included clinical data, past medical history, laboratory tests, and hospital medication. The clinical data included sex, age, body mass index, smoking status, blood pressure, heart rate, Killip classification, clinical diagnosis, and concomitant diseases. The past medical history included a history of previous heart attack, history of previous PCI/coronary artery bypass grafting (CABG), history of cerebrovascular disease, and a history of peripheral vascular disease. Laboratory tests include blood creatinine and troponin T (not high-sensitivity troponin T). Inpatient medications included aspirin, P2Y12 receptor inhibitors, angiotensin-converting enzyme inhibitor (ACEI)/angiotensin II receptor blocker (ARB)/angiotensin receptor neprilysin inhibitor (ARNI), statins, and beta-blockers.
2.3. Risk Scores
The GRACE, TIMI, and HEART scores were calculated based on the general condition, clinical history, physical examination, ECG performance, laboratory tests, and risk factors that were collected on admission. The GRACE score contains eight evaluation indicators of age, heart rate, systolic blood pressure, Killip classification, ECG ST-segment performance, serum creatinine concentration, troponin level, and cardiac arrest on admission, with scores ranging from 1 to 363. Patients with STEMI less than 126 are classified as low-risk, 126–154 as intermediate-risk, and greater than 154 as high-risk; patients with NSTEMI less than 109 are classified as low-risk, 109–140 as intermediate-risk, and greater than 140 as high-risk.
The TIMI score of NSTEMI contains 7 evaluation indexes of age, cardiovascular risk factors, history of coronary stenosis, ST-segment performance of ECG, severity of angina, aspirin use, and troponin level, with a score of 0–7, of which 0–2 is low-risk, 3–4 is intermediate-risk, and 5–7 is high-risk. The demographic characteristics, cardiovascular risk factors, comorbidities, and medical history were collected by a questionnaire interview at admission or search in medical records. Data on blood pressure, heart rate, laboratory data, angiographic results, medications, and revascularization therapy were obtained from medical records. The TIMI score for STEMI contains eight evaluation indicators: age, diabetes, hypertension or angina, systolic blood pressure, heart rate, Killip classification, weight, ECG performance, and time to visit, with a score of 0–14, of which 0–3 is low-risk, 4–6 is intermediate-risk, and 7–14 is high-risk.
The HEART score contains 5 evaluation indexes of medical history, electrocardiogram, age, cardiovascular risk factors, and troponin, with a score of 0–10, of which 0–3 is low-risk, 4–6 is intermediate-risk, and 7–10 is high-risk (Table 1).

Table 1.
Risk Scores.
2.4. Follow-Up and Study Endpoint
The endpoint event was all-cause death. The follow-up information was collected from the identification information and contact information that was provided by the patients in the hospital, and follow-up information was obtained through telephone follow-up, electronic medical record query, and household registration information to record the occurrence of the endpoint event of the patients in detail. The follow-up was conducted until the end of January 2021.
2.5. Statistical Analysis
SPSS 22.0 statistical software was used for data processing. The measurement data obeying normal distribution were expressed using the mean ± standard deviation, and the independent samples t-test was used for comparisons between the groups. The measurement data that did not obey normal distribution are expressed as the median (lower quartile, upper quartile), and the Mann–Whitney U test was used for comparisons between groups. Count data were expressed using the number of cases, rates, or composition ratios, and the χ2 test was used for comparison between the groups. The discriminatory ability of the risk scores was assessed by the area under the receiver operating characteristic curve (AUC), and the statistical significance of the difference between the AUCs was tested by the DeLong test. The mortality rates of patients with different levels of risk were analyzed by Kaplan–Meier survival curves and log-rank tests. The Hosmer–Lemeshow test was used to evaluate the calibration ability of the risk models. All the tests were performed using a two-sided test with a test level of α = 0.05.
3. Results
A total of 2582 patients with AMI who attended West China Hospital of Sichuan University from January 2011 to December 2013, of whom 182 had an unclear type of infarction diagnosis and 161 died in-hospital or automatically requested to be discharged due to abandonment of treatment for critical illness were excluded. To further reduce the effect of acute infarction critical illness on death in the short-term, the study excluded an additional 19 people who died within 30 days of discharge follow-up (including 30 days), and finally included 2220 people (Figure 1).
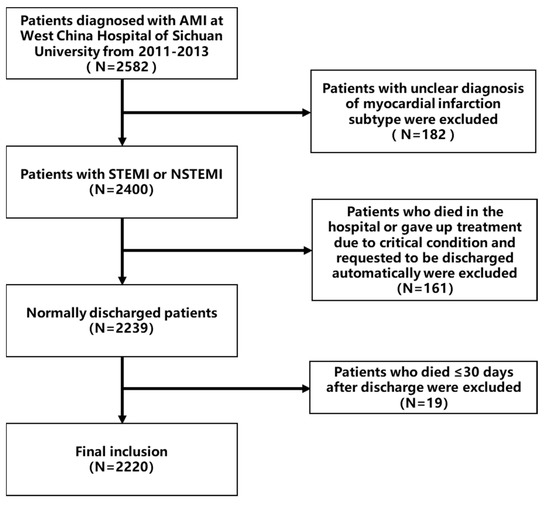
Figure 1.
Patient selection process.
The mean age of the patients was 64 years, 1752 were male (78.9%), 49.5% had hypertension, 20% had diabetes, 3% had hyperlipidemia, 61.2% were currently smoking, 11.5% had a history of MI, 1.5% had a history of PCI, and 0.2% had a history of CABG. The median follow-up was 8 years (interquartile range: 7.3–8.9 years) and there were 454 deaths (20.5%). There were 1494 STEMI patients with a median follow-up time of 8.1 years (interquartile spacing: 7.4–9 years), 30 deaths at 1 year (2.0%), 79 deaths at 3 years (5.3%), 135 deaths at 5 years (9.0%), and 236 deaths to the end of follow-up (15.8%); 726 NSTEMI patients with a median 7.9 years (interquartile range: 6.8–8.8 years), 34 (4.7%) deaths at 1 year, 73 (10.1%) deaths at 3 years, 124 (17.1%) deaths at 5 years, and 218 (30.0%) deaths by the end of follow-up (Table 2).

Table 2.
Baseline characteristics of patients.
Among the STEMI patients, the median GRACE score was 164 (interquartile range: 136–189), with 60% of patients scoring as high-risk; the median TIMI score was 5 (interquartile range: 3–7), with a predominance of intermediate-risk patients (43.5%); the median HEART score was 8 (interquartile range: 7–9), with 90.8% of patients scored as high-risk. Among the NSTEMI patients, the median GRACE score was 150 (interquartile range: 128–173), with 61.6% of patients still at high-risk; and the median TIMI score was 4 (interquartile range: 3–4), with 66.5% of patients at intermediate-risk; the median HEART score was 6 (interquartile range: 6–7), with approximately half of patients at intermediate-risk and half of patients at high-risk (54% and 45%) (Figure 2).
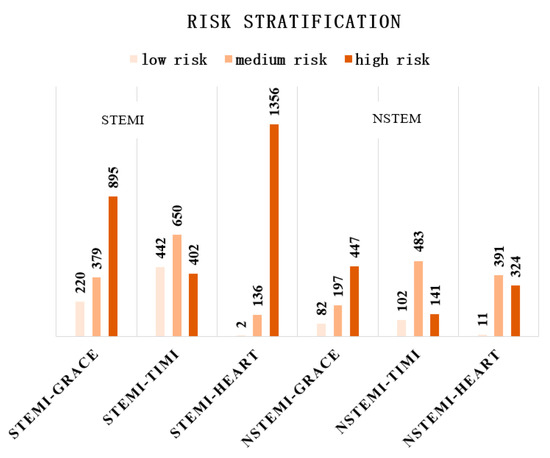
Figure 2.
Risk stratification of STEMI and NSTEMI patients in different risk models.
Among the STEMI patients, the AUC values of the GRACE score were 0.775, 0.762, 0.740, and 0.734 at 1, 3, and 5 years and by the end of follow-up, respectively. GRACE had significantly higher AUC values than the TIMI score and HEART score at 3 years, 5 years, and at the end of follow-up (p < 0.05). The TIMI score performed slightly worse than the GRACE score, with AUC values of 0.770, 0.719, 0.702, and 0.675 at the four time points, and significantly higher than the HEART score at 3 years, 5 years, and at the end of follow-up (p < 0.05). The HEART score performed relatively poorly, with AUC values of 0.719, 0.643, 0.617, and 0.617, respectively. The AUC values for all three scores tended to decrease over time, but the GRACE score was the most stable overall (Table 3, Figure 3a).

Table 3.
Comparison of the AUC values for the three risk scores at different time points *.
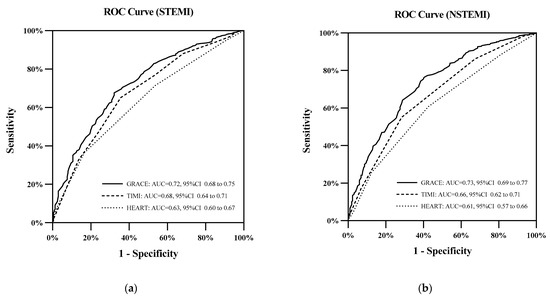
Figure 3.
(a) ROC curves for the three risk scores in STEMI patients at the end of follow-up. (b) ROC curves for the three risk scores in NSTEMI patients at the end of follow-up.
In NSTEMI patients, the GRACE score had AUC values of 0.779, 0.762, 0.738, and 0.730 at 1 year, 3 years, 5 years, and at the end of follow-up, respectively. Additionally, the GRACE score had significantly higher AUC values at 3 years, 5 years, and at the end of follow-up than the TIMI score and HEART score (p < 0.05). The AUC values of the TIMI score for predicting all-cause mortality were 0.730, 0.678, 0.656, and 0.665 at the four time points, respectively. The AUC values for the HEART score at the four time points were 0.739, 0.658, 0.629, and 0.611, which remained the lowest of the three. However, the difference in the AUC values between the TIMI score and HEART score was statistically significant only at the end of follow-up (p < 0.05) (Table 3, Figure 3b).
The Kaplan–Meier survival curves showed that among all the AMI patients, the GRACE score and TIMI score had a good discrimination between the patients with different risk levels, and the cumulative survival rate had a log rank p value < 0.01 for patients with different risk levels, while the difference in the cumulative survival rate between patients with different risk levels in the HEART score was not statistically significant (p > 0.05) (Figure 4a).
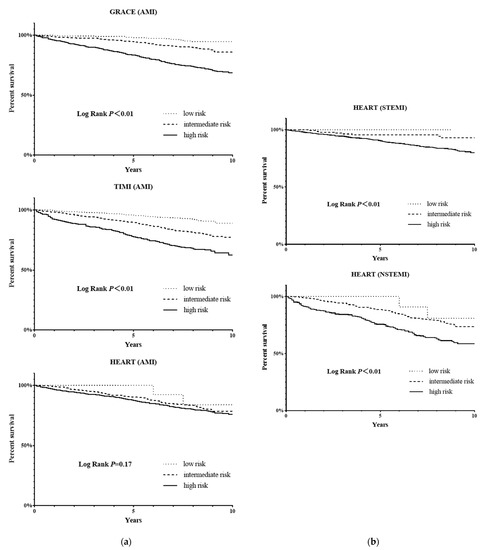
Figure 4.
(a) Kaplan–Meier survival curves for AMI patients in three risk scores. (b) Kaplan–Meier survival curves in patients with STEMI or NSTEMI in the HEART score.
At the end of follow-up, in the GRACE score the mortality rate was 5% in the low-risk patients, 11.5% in the intermediate-risk patients, and 27.8% in the high-risk patients. The risk of death was significantly higher in the intermediate-risk patients and high-risk patients than in the low-risk patients (HR = 2.402, 95% CI: 1.371–4.208, p < 0.01; HR = 6.339, 95% CI: 3.783–10.622, p < 0.01). In the TIMI score, the mortality rate was 8.6% in the low-risk patients, 20% in the intermediate-risk patients, and 33.3% in the high-risk patients. The risk of death was also significantly higher in the intermediate-risk patients and high-risk patients than in the low-risk patients (HR = 2.423, 95% CI: 1.769–3.317, p < 0.01; HR = 4.496, 95% CI: 3.261–6.198, p < 0.01). In the HEART score, the mortality rate was 15% for the low-risk patients, 18.8% for the intermediate-risk patients, and 21% for the high-risk patients. There was no statistically significant difference in the risk of death between the intermediate-risk and the high-risk patients compared with the low-risk patients (HR = 1.340, 95% CI: 0.330–5.434, p > 0.05; HR = 1.524, 95% CI: 0.380–6.119, p > 0.05).
In the subgroup analysis of STEMI and NSTEMI patients, the HEART score could also distinguish patients with different risk levels (p < 0.01). (Figure 4b) Further analysis revealed that NSTEMI patients with an intermediate-risk had a higher death risk than the STEMI patients with a high-risk score (HR = 1.407, 95% CI:1.103–1.794, p < 0.01) in the HEART score.
Finally, the Hosmer–Lemeshow test showed that the p-values of the GRACE score, STEMI-TIMI score, NSTEMI TIMI score, and HEART score were 0.644, 0.363, 0.308, and 0.320, respectively. This means that the four risk models have a good degree of calibration. (Figure 5)
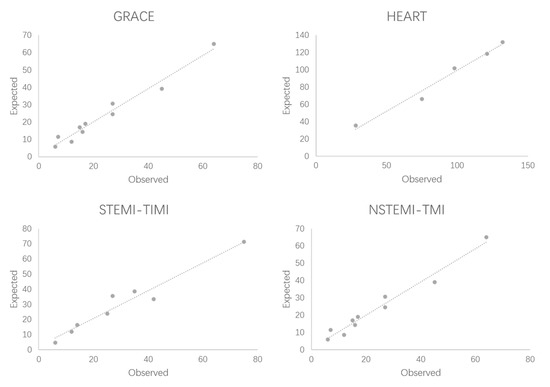
Figure 5.
Hosmer–Lemeshow test for risk models.
4. Discussion
The mortality of AMI patients is influenced by many factors, and the prognosis of patients with different levels of risk often varies greatly. Using tools such as a risk score to stratify risk in AMI patients can help to develop clinical strategies, but previous risk scoring models have focused on the short-term prognosis of patients, whereas several data show that it is equally important to assess the long-term prognosis of AMI patients. Although some risk scoring models have been developed for the long-term prognosis of AMI patients, they are still rare in the literature. Assessing the value of existing risk scoring models that have been widely used in the clinic in predicting the long-term prognosis of AMI patients may be a more convenient and rapid approach.
In this study, we found that the three most widely used risk scoring models, the GRACE score, TIMI score, and HEART score, can all predict the long-term prognosis of patients with AMI through an 8-year follow-up. Among the three risk scores, the GRACE score had the best prediction accuracy. In terms of risk stratification, both the GRACE score and the TIMI score were able to distinguish AMI patients with different risk levels, while the HEART score was only able to distinguish STEMI or NSTEMI patients with different risk levels in the subgroup analysis and performed poorly for overall AMI patient stratification. Moreover, all risk models passed the Hosmer–Lemeshow test.
There are only a few reports on the use of the GRACE score and TIMI score to predict the long-term prognosis of AMI patients, and the results of the studies are inconsistent. In one study, the AUC values of the GRACE score for predicting 3-year mortality in patients with STEMI or NSTEMI were 0.77 and 0.78, respectively, and both were higher than the TIMI score (AUC = 0.68 and 0.69, both p < 0.01) [23]. Another study that included only STEMI patients reported similar results, with the GRACE score being more accurate than the TIMI score in predicting the 3-year mortality in STEMI patients (0.77 versus 0.66, p < 0.01) [24]. However, some studies have also shown that the GRACE score is less accurate than the TIMI score in predicting 1-year mortality in STEMI patients (0.47 versus 0.75, p < 0.01) [25]. The advantage of the GRACE score over the TIMI score in predicting 1- and 5-year mortality was also not found in the study by Kozieradzka (0.81 versus 0.81, p > 0.05; 0.74 versus 0.73, p > 0.05) [26]. However, the former of the latter two studies excluded patients with cardiogenic shock and cardiac arrest, and the latter included only patients who underwent emergency PCI, which may not reflect the full picture of STEMI patients. Our study has the largest number of participants and longest follow-up to date, includes both STEMI and NSTEMI patients, and does not specifically exclude patients, which can best reflect the true performance of the risk scoring model. The AUC of the GRACE score for predicting the 1-year mortality was 0.78 for both STEMI and NSTEMI patients, and although the AUC value declined with longer follow-up, it also reached 0.73 until the end of follow-up (approximately 8 years). In contrast, the TIMI score was close to the GRACE score only at year 1, and the AUC values were lower than the GRACE score at 3 years, 5 years, and up to the end of follow-up. Therefore, the GRACE score was superior to the TIMI score in predicting long-term mortality.
There is only one report on the HEART score in predicting long-term prognosis in patients with ACS, which showed that patients with a score ≥ 4 had a much higher mortality rate than those with a score ≤ 3 at 5 years of follow-up (48.2% versus 10.6%, p < 0.01), but the AUC value of the HEART score in predicting the long-term mortality was not given in their study [15]. Our results showed that the HEART score was equally predictive of distant prognosis in STEMI patients and NSTEMI patients (AUC value > 0.5), but the predictive accuracy was inferior to both the GRACE score and the TIMI score. This result is not difficult to understand, as the HEART score is an emergency score for patients with chest pain whose diagnosis is still unclear. Its primary aim is to distinguish patients that are at high-risk in the short-term as soon as possible, so applicability and simplicity come first, and some data that are less readily available during the emergency period are then excluded [12]. Meanwhile, the assessment of the degree of suspicious medical history in the HEART score is somewhat subjective, which may also affect its predictive accuracy.
The higher accuracy of the GRACE score among the three scores may be related to some unique indicators. For example, creatinine has been previously shown to be a risk factor for long-term cardiovascular complications and long-term mortality in patients with AMI. At eGFR below 81 mL/1.73 min*m2, the risk of death and nonfatal cardiovascular outcomes in patients rises by 10% for every 10 unit decrease in eGFR (RR = 1.1, 95% CI:1.08–1.12) [27]. The Killip classification is also a factor that is associated with long-term prognosis in AMI patients. A higher Killip classification of AMI patients tends to have a combination of more severe coronary lesions and larger infarct size, which implies more myocardial cell necrosis, and the necrotic cells are subsequently replaced by fibrotic scars. Fibrous scar formation is difficult to reverse afterwards and has a range of adverse effects on the long-term prognosis of patients through its effect on cardiac contractility and interference with normal cardiac electrical activity leading to arrhythmias [28,29,30,31]. Although the TIMI score for STEMI patients includes the Killip classification, the model for NSTEMI patients does not include this factor, which may be one of the reasons why the TIMI score has a higher predictive accuracy for STEMI patients than for NSTEMI patients. In addition, the GRACE score treats risk factors such as age, heart rate, and blood pressure as continuous variables, which allows for a more refined risk assessment. In contrast, the TIMI score and HEART score consist of only dichotomous variables and provide limited feedback.
In terms of risk stratification, an interesting result is that the HEART score does not allow risk stratification of all AMI patients but performs well in the evaluation of STEMI patients or NSTEMI patients alone. This may be related to electrocardiographic performance as an evaluation metric. Typical ST-segment elevation accounts for 2 points in the HEART score, which is only a maximum of 10 points. This would result in lower scores for NSTEMI patients compared to STEMI patients, causing a proportion of high-risk NSTEMI patients to be assigned to the intermediate-risk group with a score of 7 or less and a proportion of intermediate-risk STEMI patients to the high-risk group. Thus, in the overall AMI grouping, patients in the intermediate-risk and high-risk groups are a mix of patients with both risk levels, resulting in poor stratification.
A clearer perception of the long-term prognosis of AMI patients may guide clinicians to make more effective interventions in clinical practice, while increasing patients’ perception of their own risk level may also increase their medication adherence to some extent. When assessing the short-term prognosis of patients with AMI, simplicity and ease of use may be a higher priority due to the need to determine the patient’s level of risk as soon as possible. However, when assessing the long-term prognosis of patients, the emphasis may be more on the accuracy of prediction. Therefore, the GRACE score, although more cumbersome than the TIMI score and HEART score, remains the score of choice for assessing the long-term prognosis of patients with AMI.
5. Limitations
First, only the GRACE score, TIMI score, and HEART score were compared in this study, and although many other risk scores are currently available, most of them are not widely used in clinical practice and were excluded. Second, because these data were not collected prospectively, the assessment of the degree of suspicion of medical history in the HEART score could only be calculated by a proxy for clinical suspicion of ACS, and the score results might have been different if the data had been collected prospectively. Finally, this study is a single-center retrospective study with a predominantly Chinese population, which may introduce some population bias.
6. Conclusions
In this study, a comparison of the GRACE score, TIMI score, and HEART score revealed that the GRACE risk score could represent a more accurate model to assess long-term death of acute myocardial infarction. The higher accuracy of the GRACE score may be related to its unique index and continuous variables, but further studies are required.
Author Contributions
B.Y. designed the study, collected the data, analyzed the data, and drafted the article. L.B., Y.Z. and Y.C. collected the data and revised the article. C.Z. polished the language. B.H. and M.C. designed the study, drafted the article, and revised it. All authors have read and agreed to the published version of the manuscript.
Funding
B.H. reported a grant from the Key Research and Development Projects of Science & Technology Department of Sichuan Province (2019YFS0351).
Institutional Review Board Statement
The study protocol was approved by the institutional review boards of West China Hospital, Sichuan University, an institutional ethics committee.
Informed Consent Statement
All subjects provided written informed consent before enrolment.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
ACS: acute coronary syndrome; AMI: acute myocardial infarction. BBB: bundle branch block. BMI: body mass index. CABG: coronary arterial bypass grafting. CVA: cerebrovascular attack. LVH: left ventricular hypertrophy. MACEs: major adverse cardiac events. NSTEMI: non-ST-segment elevation myocardial infarction. PCI: percutaneous coronary intervention. STEMI: ST-segment elevation myocardial infarction. TIA: transient ischemic attack.
References
- Nichols, M.; Townsend, N.; Scarborough, P.; Rayner, M. Cardiovascular disease in Europe 2014: Epidemiological update. Eur. Heart J. 2014, 35, 2950–2959. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef] [PubMed]
- Rogers, W.J.; Frederick, P.D.; Stoehr, E.; Canto, J.G.; Ornato, J.P.; Gibson, C.M.; Pollack, C.V., Jr.; Gore, J.M.; Chandra-Strobos, N.; Peterson, E.D.; et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am. Heart J. 2008, 156, 1026–1034. [Google Scholar] [CrossRef]
- Krumholz, H.M.; Normand, S.L.; Wang, Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation 2014, 130, 966–975. [Google Scholar] [CrossRef]
- Roe, M.T.; Messenger, J.C.; Weintraub, W.S.; Cannon, C.P.; Fonarow, G.C.; Dai, D.; Chen, A.Y.; Klein, L.W.; Masoud, F.A.; McKay, C.; et al. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J. Am. Coll. Cardiol. 2010, 56, 254–263. [Google Scholar] [CrossRef]
- China Cardiovascular Health and Disease Report Writing Group. China Cardiovascular Health and Disease Report 2020 Summary. Report on Cardiovascular Health and Diseases Burden in China: An Updated Summary of 2020. Chin. Circ. J. 2021, 36, 521–545. (In Chinese) [Google Scholar]
- Castro-Dominguez, Y.; Dharmarajan, K.; Mcnamara, R.L. Predicting death after acute myocardial infarction. Trends Cardiovasc. Med. 2018, 28, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar]
- Granger, C.B.; Goldberg, R.J.; Dabbous, O.; Pieper, K.S.; Eagle, K.A.; Cannon, C.P. Predictors of hospital mortality in the global registry of acute coronary events. Arch. Intern. Med. 2003, 163, 2345–2353. [Google Scholar] [CrossRef]
- Antman, E.M.; Cohen, M.; Bernink, P.J.; McCabe, C.H.; Horacek, T.; Papuchis, G.; Mautner, B.; Corbalan, R.; Radley, D.; Braunwald, E. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA 2000, 284, 835–842. [Google Scholar] [CrossRef]
- Morrow, D.A.; Antman, E.M.; Charlesworth, A.; Cairns, R.; Murphy, S.A.; de Lemos, J.A.; Giugliano, R.P.; McCabe, C.H.; Braunwald, E. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation 2000, 102, 2031–2037. [Google Scholar] [CrossRef] [PubMed]
- Six, A.J.; Backus, B.E.; Kelder, J.C. Chest pain in the emergency room: Value of the HEART score. Neth. Heart J. 2008, 16, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Soiza, R.L.; Leslie, S.J.; Williamson, P.; Wai, S.; Harrild, K.; Peden, N.R.; Hargreaves, A.D. Risk stratification in acute coronary syndromes—does the TIMI risk score work in unselected cases? QJM 2006, 99, 81–87. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morrow, D.A.; Antman, E.M.; Parsons, L.; de Lemos, J.A.; Cannon, C.P.; Giugliano, R.P.; McCabe, C.H.; Barron, H.V.; Braunwald, E. Application of the TIMI risk score for ST-elevation MI in the National Registry of Myocardial Infarction 3. JAMA 2001, 286, 1356–1359. [Google Scholar] [CrossRef]
- Jain, T.; Nowak, R.; Hudson, M.; Frisoli, T.; Jacobsen, G.; McCord, J. Short- and Long-Term Prognostic Utility of the HEART Score in Patients Evaluated in the Emergency Department for Possible Acute Coronary Syndrome. Crit. Pathw. Cardiol. 2016, 15, 40–45. [Google Scholar] [CrossRef]
- Poldervaart, J.M.; Langedijk, M.; Backus, B.E.; Dekker, I.M.C.; Six, A.J.; Doevendans, P.A.; Hoes, A.W.; Reitsma, J.B. Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. Int. J. Cardiol. 2017, 227, 656–661. [Google Scholar] [CrossRef]
- Kristensen, S.D.; Laut, K.G.; Fajadet, J.; Kaifoszova, Z.; Kala, P.; Di Mario, C.; Wijns, W.; Clemmensen, P.; Agladze, V.; Antoniades, L.; et al. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011: Current status in 37 ESC countries. Eur. Heart J. 2014, 35, 1957–1970. [Google Scholar] [CrossRef]
- Pedersen, F.; Butrymovich, V.; Kelbæk, H.; Wachtell, K.; Helqvist, S.; Kastrup, J.; Holmvang, L.; Clemmensen, P.; Engstrøm, T.; Grande, P.; et al. Short- and long-term cause of death in patients treated with primary PCI for STEMI. J. Am. Coll. Cardiol. 2014, 64, 2101–2118. [Google Scholar] [CrossRef]
- Fokkema, M.L.; James, S.K.; Albertsson, P.; Akerblom, A.; Calais, F.; Eriksson, P.; Jensen, J.; Nilsson, T.; de Smet, B.J.; Sjögren, I.; et al. Population trends in percutaneous coronary intervention: 20-year results from the SCAAR (Swedish Coronary Angiography and Angioplasty Registry). J. Am. Coll. Cardiol. 2013, 61, 1222–1230. [Google Scholar] [CrossRef]
- Li, J.; Li, X.; Wang, Q.; Hu, S.; Wang, Y.; Masoudi, F.A.; Spertus, J.A.; Krumholz, H.M.; Jiang, L.; China PEACE Collaborative Group. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE-Retrospective Acute Myocardial Infarction Study): A retrospective analysis of hospital data. Lancet 2015, 385, 441–451. [Google Scholar] [CrossRef]
- Addala, S.; Grines, C.L.; Dixon, S.R.; Stone, G.W.; Boura, J.A.; Ochoa, A.B.; Pellizzon, G.; O’Neill, W.W.; Kahn, J.K. Predicting mortality in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention (PAMI risk score). Am. J. Cardiol. 2004, 93, 629–632. [Google Scholar] [CrossRef] [PubMed]
- Halkin, A.; Singh, M.; Nikolsky, E.; Grines, C.L.; Tcheng, J.E.; Garcia, E.; Cox, D.A.; Turco, M.; Stuckey, T.D.; Na, Y.; et al. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: The CADILLAC risk score. J. Am. Coll. Cardiol. 2005, 45, 1397–1405. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Huang, S.S.; Lin, S.J. TIMI and GRACE Risk Scores Predict Both Short-Term and Long-Term Outcomes in Chinese Patients with Acute Myocardial Infarction. Acta Cardiol. Sin. 2018, 34, 4–12. [Google Scholar] [PubMed]
- Littnerova, S.; Kala, P.; Jarkovsky, J.; Kubkova, L.; Prymusova, K.; Kubena, P.; Tesak, M.; Toman, O.; Poloczek, M.; Spinar, J.; et al. GRACE Score among Six Risk Scoring Systems (CADILLAC, PAMI, TIMI, Dynamic TIMI, Zwolle) Demonstrated the Best Predictive Value for Prediction of Long-Term Mortality in Patients with ST-Elevation Myocardial Infarction. PLoS ONE 2015, 10, e0123215. [Google Scholar]
- Lev, E.I.; Kornowski, R.; Vaknin-Assa, H.; Porter, A.; Teplitsky, I.; Ben-Dor, I.; Brosh, D.; Fuchs, S.; Battler, A.; Assali, A. Comparison of the predictive value of four different risk scores for outcomes of patients with ST-elevation acute myocardial infarction undergoing primary percutaneous coronary intervention. Am. J. Cardiol. 2008, 102, 6–11. [Google Scholar] [CrossRef]
- Kozieradzka, A.; Kamiński, K.A.; Maciorkowska, D.; Olszewska, M.; Dobrzycki, S.; Nowak, K.; Kralisz, P.; Prokopczuk, P.; Musial, W.J. GRACE, TIMI, Zwolle and CADILLAC risk scores--do they predict 5-year outcomes after ST-elevation myocardial infarction treated invasively? Int. J. Cardiol. 2011, 148, 70–75. [Google Scholar] [CrossRef]
- Anavekar, N.S.; Mcmurray, J.J.; Velazquez, E.J.; Solomon, S.D.; Kober, L.; Rouleau, J.L.; White, H.D.; Nordlander, R.; Maggioni, A.; Dickstein, K.; et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl. J. Med. 2004, 351, 1285–1295. [Google Scholar] [CrossRef]
- Nesković, A.N.; Otasević, P.; Bojić, M.; Popović, A.D. Association of Killip class on admission and left ventricular dilatation after myocardial infarction: A closer look into an old clinical classification. Am. Heart J. 1999, 137, 361–367. [Google Scholar] [CrossRef]
- Khot, U.N.; Jia, G.; Moliterno, D.J.; Lincoff, A.M.; Khot, M.B.; Harrington, R.A.; Topol, E.J. Prognostic importance of physical examination for heart failure in non-ST-elevation acute coronary syndromes: The enduring value of Killip classification. Jama 2003, 290, 2174–2181. [Google Scholar] [CrossRef]
- Sutton, M.G.; Sharpe, N. Left ventricular remodeling after myocardial infarction: Pathophysiology and therapy. Circulation 2000, 101, 2981–2988. [Google Scholar] [CrossRef]
- Francis Stuart, S.D.; De Jesus, N.M.; Lindsey, M.L.; Lindsey, M.L.; Ripplinger, C.M. The crossroads of inflammation, fibrosis, and arrhythmia following myocardial infarction. J. Mol. Cell Cardiol. 2016, 91, 114–122. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).