The Clinical Effects of Pixel CO2 Laser on Bladder Neck and Stress Urinary Incontinence
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reynolds, W.S.; Dmochowski, R.R.; Penson, D.F. Epidemiology of stress urinary incontinence in women. Curr. Urol. Rep. 2011, 12, 370–376. [Google Scholar] [CrossRef]
- McGrother, C.W.; Donaldson, M.M.; Thompson, J.R. Re: “Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: The Boston Area Community Health (BACH) Survey”. Am. J. Epidemiol. 2008, 168, 234, author reply 234–236. [Google Scholar] [CrossRef][Green Version]
- Coyne, K.S.; Sexton, C.C.; Thompson, C.L.; Milsom, I.; Irwin, D.; Kopp, Z.S.; Chapple, C.R.; Kaplan, S.; Tubaro, A.; Aiyer, L.P.; et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: Results from the Epidemiology of LUTS (EpiLUTS) study. BJU Int. 2009, 104, 352–360. [Google Scholar] [CrossRef]
- Chang, K.-M.; Hsieh, C.-H.; Chiang, H.-S.; Lee, T.-S. Trends in inpatient female urinary incontinence surgery and costs in Taiwan, 1997–2011. Taiwan. J. Obstet. Gynecol. 2017, 56, 32–36. [Google Scholar] [CrossRef]
- Patel, P.D.; Amrute, K.V.; Badlani, G.H. Pelvic organ prolapse and stress urinary incontinence: A review of etiological factors. Indian J. Urol. 2007, 23, 135–141. [Google Scholar] [CrossRef]
- De Lancey, J.O.L. Why do women have stress urinary incontinence? Neurourol. Urodyn. 2010, 29, S13–S17. [Google Scholar] [CrossRef]
- Reisenauer, C.; Muche-Borowski, C.; Anthuber, C.; Finas, D.; Fink, T.; Gabriel, B.; Hübner, M.; Lobodasch, K.; Naumann, G.; Peschers, U.; et al. Interdisciplinary S2e Guideline for the Diagnosis and Treatment of Stress Urinary Incontinence in Women: Short version—AWMF Registry No. 015-005, July 2013. Geburtshilfe Frauenheilkd. 2013, 73, 899–903. [Google Scholar] [CrossRef]
- Kwon, J.; Kim, Y.; Kim, D.Y. Second-Line Surgical Management After Midurethral Sling Failure. Int. Neurourol. J. 2021, 25, 111–118. [Google Scholar] [CrossRef]
- Barisiene, M.; Cerniauskiene, A.; Matulevicius, A. Complications and their treatment after midurethral tape implantation using retropubic and transobturator approaches for treatment of female stress urinary incontinence. Wideochirurgia I Inne Tech. Maloinwazyjne = Videosurgery Other Miniinvasive Tech. 2018, 13, 501–506. [Google Scholar] [CrossRef]
- Park, C.S.; Park, J.-H.; Lee, J.; Byun, H.J.; Lim, Y.; Lee, J.H.; Lee, D.-Y.; Lee, J.-H.; Yang, J.-M. Chronic Exfoliative Cheilitis Successfully Treated by Pinhole Method Using CO2 Laser. Ann. Dermatol. 2019, 31, 361–363. [Google Scholar] [CrossRef]
- Aldahan, A.S.; Shah, V.V.; Mlacker, S.; Samarkandy, S.; Alsaidan, M.; Nouri, K. Laser and Light Treatments for Striae Distensae: A Comprehensive Review of the Literature. Am. J. Clin. Dermatol. 2016, 17, 239–256. [Google Scholar] [CrossRef] [PubMed]
- Tadir, Y.; Gaspar, A.; Lev-Sagie, A.; Alexiades, M.; Alinsod, R.; Bader, A.; Calligaro, A.; Elias, J.A.; Gambaciani, M.; Gaviria, J.E.; et al. Light and energy based therapeutics for genitourinary syndrome of menopause: Consensus and controversies. Lasers Surg. Med. 2017, 49, 137–159. [Google Scholar] [CrossRef] [PubMed]
- Lapii, G.A.; Yakovleva, A.Y.; Neimark, A.I. Structural Reorganization of the Vaginal Mucosa in Stress Urinary Incontinence under Conditions of Er:YAG Laser Treatment. Bull. Exp. Biol. Med. 2017, 162, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Ruffolo, A.F.; Braga, A.; Torella, M.; Frigerio, M.; Cimmino, C.; De Rosa, A.; Sorice, P.; Castronovo, F.; Salvatore, S.; Serati, M. Vaginal Laser Therapy for Female Stress Urinary Incontinence: New Solutions for a Well-Known Issue-A Concise Review. Medicina 2022, 58, 512. [Google Scholar] [CrossRef]
- Lin, K.-L.; Chou, S.-H.; Long, C.-Y. Effect of Er:YAG Laser for Women with Stress Urinary Incontinence. BioMed Res. Int. 2019, 2019, 7915813. [Google Scholar] [CrossRef] [PubMed]
- Long, C.-Y.; Wu, P.-C.; Chen, H.-S.; Lin, K.-L.; Loo, Z.; Liu, Y.; Wu, C.-H. Changes in sexual function and vaginal topography using transperineal ultrasound after vaginal laser treatment for women with stress urinary incontinence. Sci. Rep. 2022, 12, 3435. [Google Scholar] [CrossRef]
- Trelles, M.A.; Rigau, J.; Pardo, L.; García-Solana, L.; Vélez, M. Electron microscopy comparison of CO2 laser flash scanning and pulse technology one year after skin resurfacing. Int. J. Dermatol. 1999, 38, 58–64. [Google Scholar] [CrossRef]
- Ross, E.V.; McKinlay, J.R.; Anderson, R.R. Why does carbon dioxide resurfacing work? A review. Arch. Dermatol. 1999, 135, 444–454. [Google Scholar] [CrossRef]
- Li, Y.-Q.; Geng, J.; Tan, C.; Tang, J.; Yang, X. Diagnosis and classification of female stress urinary incontinence by transperineal two-dimensional ultrasound. Technol. Health Care 2017, 25, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Xiao, T.; Xiao, T.; Chen, Y.; Gan, Y.; Xu, J.; Huang, W.; Zhang, X. Can Stress Urinary Incontinence Be Predicted by Ultrasound? Am. J. Roentgenol. 2019, 213, 1163–1169. [Google Scholar] [CrossRef] [PubMed]
- Al-Saadi, W.I. Transperineal ultrasonography in stress urinary incontinence: The significance of urethral rotation angles. Arab J. Urol. 2016, 14, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.L.; Juan, Y.S.; Lo, T.S.; Liu, C.M.; Tsai, E.M.; Long, C.Y. Three-dimensional ultrasonographic assessment of compression effect on urethra following tension-free vaginal tape and transobturator tape procedures. Ultrasound Obstet. Gynecol. Off. J. Int. Soc. Ultrasound Obstet. Gynecol. 2012, 39, 452–457. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Behnia-Willison, F.; Nguyen, T.T.T.; Mohamadi, B.; Vancaillie, T.G.; Lam, A.; Willison, N.N.; Zivkovic, J.; Woodman, R.J.; Skubisz, M.M. Fractional CO(2) laser for treatment of stress urinary incontinence. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2019, 1, 100004. [Google Scholar] [CrossRef] [PubMed]
- Homma, Y.; Yoshida, M.; Seki, N.; Yokoyama, O.; Kakizaki, H.; Gotoh, M.; Yamanishi, T.; Yamaguchi, O.; Takeda, M.; Nishizawa, O. Symptom assessment tool for overactive bladder syndrome--overactive bladder symptom score. Urology 2006, 68, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Uebersax, J.S.; Wyman, J.F.; Shumaker, S.A.; McClish, D.K.; Fantl, J.A. Short forms to assess life quality and symptom distress for urinary incontinence in women: The Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program for Women Research Group. Neurourol. Urodyn. 1995, 14, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Avery, K.; Donovan, J.; Peters, T.J.; Shaw, C.; Gotoh, M.; Abrams, P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol. Urodyn. 2004, 23, 322–330. [Google Scholar] [CrossRef]
- Wilson, K.G.; Sandoz, E.K.; Kitchens, J.; Roberts, M. The Valued Living Questionnaire: Defining and Measuring Valued Action within a Behavioral Framework. Psychol. Rec. 2010, 60, 249–272. [Google Scholar] [CrossRef]
- Klovning, A.; Avery, K.; Sandvik, H.; Hunskaar, S. Comparison of two questionnaires for assessing the severity of urinary incontinence: The ICIQ-UI SF versus the incontinence severity index. Neurourol. Urodyn. 2009, 28, 411–415. [Google Scholar] [CrossRef]
- Krhut, J.; Zachoval, R.; Smith, P.P.; Rosier, P.F.; Valanský, L.; Martan, A.; Zvara, P. Pad weight testing in the evaluation of urinary incontinence. Neurourol. Urodyn. 2014, 33, 507–510. [Google Scholar] [CrossRef]
- Reynard, J.M.; Yang, Q.; Donovan, J.L.; Peters, T.J.; Schafer, W.; de la Rosette, J.J.; Dabhoiwala, N.F.; Osawa, D.; Lim, A.T.; Abrams, P. The ICS-‘BPH’ Study: Uroflowmetry, lower urinary tract symptoms and bladder outlet obstruction. Br. J. Urol. 1998, 82, 619–623. [Google Scholar] [CrossRef]
- Sendag, F.; Vidinli, H.; Kazandi, M.; Itil, I.M.; Askar, N.; Vidinli, B.; Pourbagher, A. Role of perineal sonography in the evaluation of patients with stress urinary incontinence. Aust. New Zealand J. Obstet. Gynaecol. 2003, 43, 54–57. [Google Scholar] [CrossRef]
- Robinson, D.; Anders, K.; Cardozo, L.; Bidmead, J.; Dixon, A.; Balmforth, J.; Rufford, J. What Do Women Want? Interpretation of the Concept of Cure. Female Pelvic Med. Reconstr. Surg. 2003, 9, 273–277. [Google Scholar] [CrossRef]
- Imamura, M.; Hudson, J.; Wallace, S.A.; MacLennan, G.; Shimonovich, M.; Omar, M.I.; Javanbakht, M.; Moloney, E.; Becker, F.; Ternent, L.; et al. Surgical interventions for women with stress urinary incontinence: Systematic review and network meta-analysis of randomised controlled trials. BMJ 2019, 365, l1842. [Google Scholar] [CrossRef]
- Fistonić, N.; Fistonić, I.; Lukanovič, A.; Findri Guštek, Š.; Sorta Bilajac Turina, I.; Franić, D. First assessment of short-term efficacy of Er:YAG laser treatment on stress urinary incontinence in women: Prospective cohort study. Climacteric J. Int. Menopause Soc. 2015, 18 (Suppl. S1), 37–42. [Google Scholar] [CrossRef] [PubMed]
- Tien, Y.W.; Hsiao, S.M.; Lee, C.N.; Lin, H.H. Effects of laser procedure for female urodynamic stress incontinence on pad weight, urodynamics, and sexual function. Int. Urogynecol. J. 2017, 28, 469–476. [Google Scholar] [CrossRef] [PubMed]
- González Isaza, P.; Jaguszewska, K.; Cardona, J.L.; Lukaszuk, M. Long-term effect of thermoablative fractional CO(2) laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int. Urogynecol. J. 2018, 29, 211–215. [Google Scholar] [CrossRef]
- Petrov, A.; Pljakovska, V. Fractional Carbon Dioxide Laser in Treatment of Acne Scars. Open Access Maced. J. Med. Sci. 2015, 4, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.B.; Spencer, J. Scarring and persistent erythema after fractionated ablative CO2 laser resurfacing. J. Drugs Dermatol. JDD 2008, 7, 1072–1073. [Google Scholar]
- Salvatore, S.; Nappi, R.E.; Zerbinati, N.; Calligaro, A.; Ferrero, S.; Origoni, M.; Candiani, M.; Leone Roberti Maggiore, U. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: A pilot study. Climacteric J. Int. Menopause Soc. 2014, 17, 363–369. [Google Scholar] [CrossRef]
- Hajebrahimi, S.; Azaripour, A.; Sadeghi-Bazargani, H. Clinical and transperineal ultrasound findings in females with stress urinary incontinence versus normal controls. Pak. J. Biol. Sci. PJBS 2009, 12, 1434–1437. [Google Scholar] [CrossRef] [PubMed]
| Pre-Operation (n = 25) | Post-Operation (n = 25) | p Value | |
|---|---|---|---|
| Mean age (years) | 42.9 ± 5.6 | ||
| Mean BMI (kg/m2) | 22.6 ± 3.5 | ||
| Menopause | 1 (4%) | ||
| Pad test | 4.3 ± 12.1 | 0.7 ± 1.3 | 0.023 * |
| SUI grade by ICIQ | |||
| mild | 12 (48%) | ||
| moderate | 9 (36%) | ||
| severe | 2 (8%) | ||
| very severe | 2 (8%) | ||
| Type of SUI (Type 2) | 25 (100%) | ||
| Efficacy | 20/25 (80%) | ||
| Follow-up (months) | 6M |
| Pre-Operation (n = 25) | Post-Operation (n = 25) | p Value * | |
|---|---|---|---|
| OABSS | 3.5 ± 2.6 | 3.2 ± 2.0 | 0.481 |
| UDI-6 | 22.2 ± 14.1 | 14.2 ± 11.5 | 0.012 * |
| IIQ-7 | 12.6 ± 14.8 | 7.9 ± 11.4 | 0.049 * |
| ICIQ-SF | 5.9 ± 4.2 | 3.2 ± 3.5 | 0.022 * |
| VLQ | 3.6 ± 0.7 | 4.8 ± 0.9 | 0.004 * |
| Pre-Operation (n = 25) | Post-Operation (n = 25) | p Value * | |
|---|---|---|---|
| Qmax (mL/s) | 24.7 ± 10.0 | 26.7 ± 8.8 | 0.290 |
| RU (mL) | 77.1 ± 85.6 | 53.1 ± 57.3 | 0.293 |
| Vfst (mL) | 202.9 ± 90.0 | 195.2 ± 86.6 | 0.73 |
| MCC (mL) | 444.6 ± 134.4 | 453.7 ± 155.7 | 0.530 |
| Pdet Qmax (mmHg) | 26.8 ± 15.8 | 27.4 ± 12.1 | 0.940 |
| MUCP (mmHg) | 68.3 ± 20.6 | 65.4 ± 19.1 | 0.486 |
| FUL (cm) | 30.5 ± 6.9 | 29.7 ± 4.5 | 0.631 |
| Pre-Operation (n = 25) | Post-Operation (n = 25) | p Value * | ||
|---|---|---|---|---|
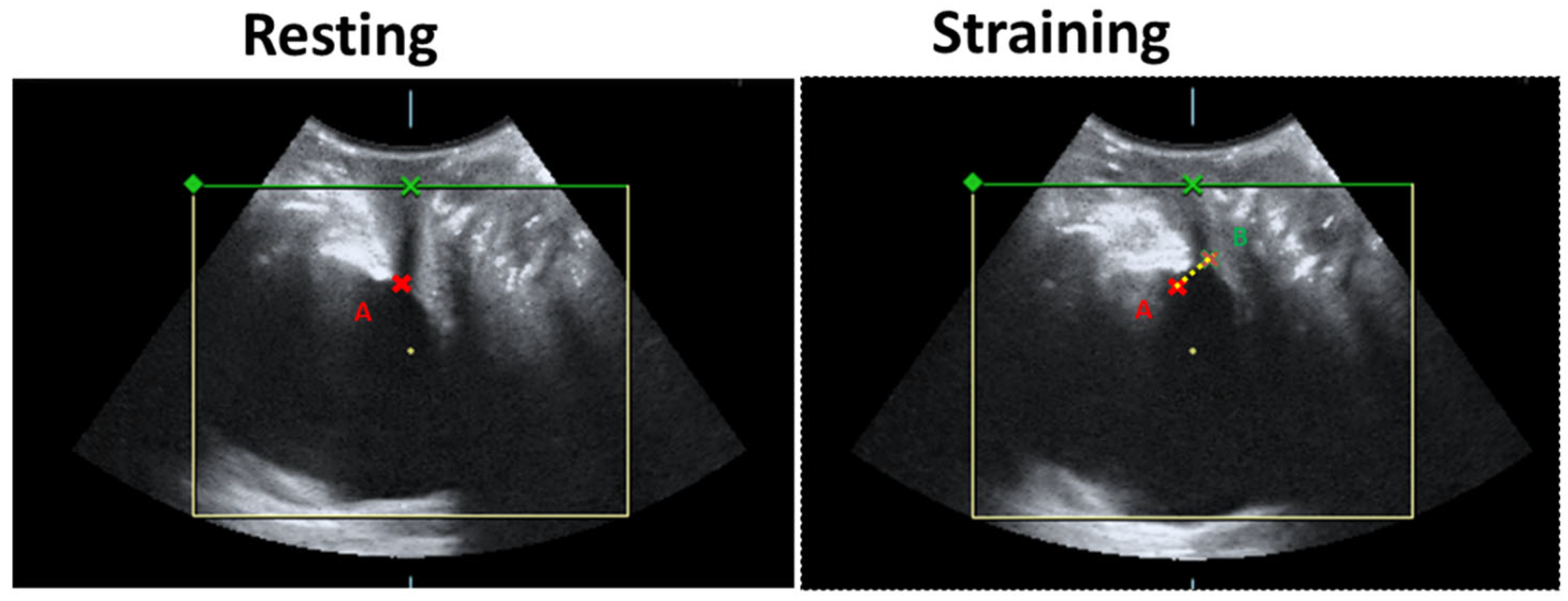
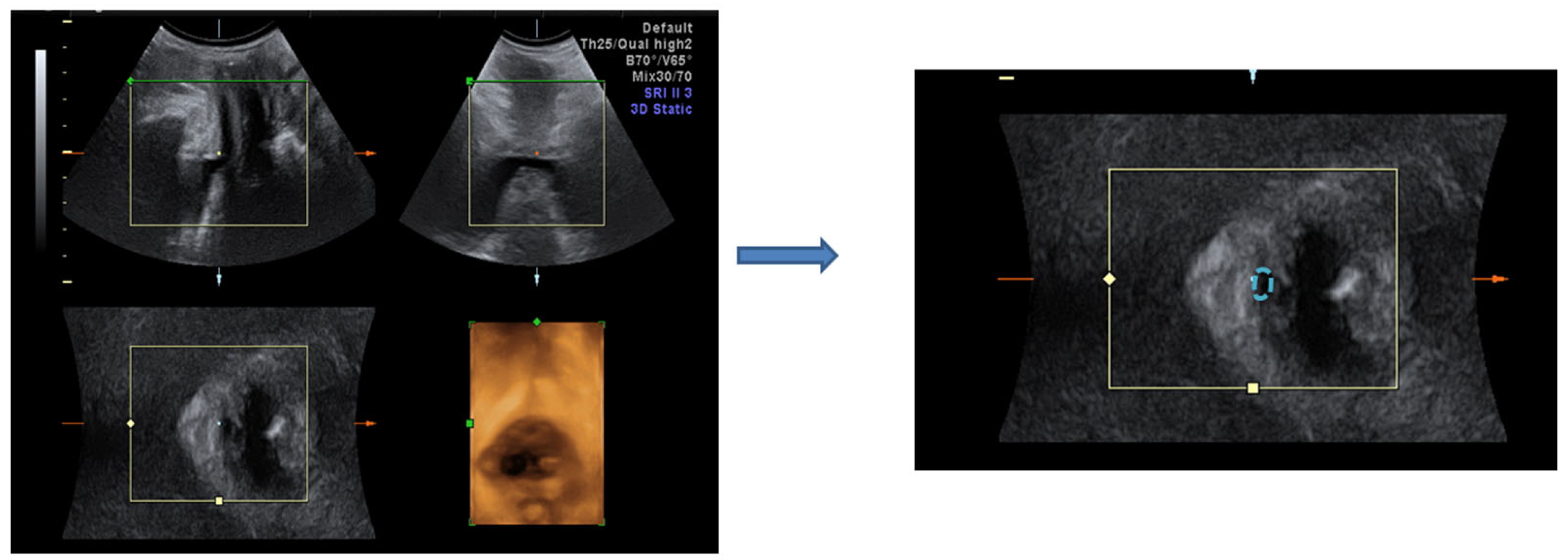
| Bladder neck mobility (mm) | 1.52 ± 0.3 | 1.27 ± 0.3 | 0.043 * | |
| Urethral area (mm2) Resting | proximal | 3.2 ± 1.8 | 2.7 ± 0.6 | 0.122 |
| middle | 2.8 ± 1.1 | 2.2 ± 0.7 | 0.045 * | |
| distal | 2.3 ± 1.0 | 2.5 ± 1.2 | 0.787 | |
| Urethral area (mm2) Straining | proximal | 4.1 ± 1.3 | 4.2 ± 1.1 | 0.574 |
| middle | 3.5 ± 1.2 | 3.2 ± 0.8 | 0.024 * | |
| distal | 2.9 ± 1.0 | 3 ± 1.5 | 0.746 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Long, C.-Y.; Lee, J.P.-N.; Loo, Z.-X.; Liu, Y.-Y.; Yeh, C.-L.; Feng, C.-W.; Lin, K.-L. The Clinical Effects of Pixel CO2 Laser on Bladder Neck and Stress Urinary Incontinence. J. Clin. Med. 2022, 11, 4971. https://doi.org/10.3390/jcm11174971
Long C-Y, Lee JP-N, Loo Z-X, Liu Y-Y, Yeh C-L, Feng C-W, Lin K-L. The Clinical Effects of Pixel CO2 Laser on Bladder Neck and Stress Urinary Incontinence. Journal of Clinical Medicine. 2022; 11(17):4971. https://doi.org/10.3390/jcm11174971
Chicago/Turabian StyleLong, Cheng-Yu, Jennifer Po-Ning Lee, Zi-Xi Loo, Yi-Yin Liu, Chang-Lin Yeh, Chien-Wei Feng, and Kun-Ling Lin. 2022. "The Clinical Effects of Pixel CO2 Laser on Bladder Neck and Stress Urinary Incontinence" Journal of Clinical Medicine 11, no. 17: 4971. https://doi.org/10.3390/jcm11174971
APA StyleLong, C.-Y., Lee, J. P.-N., Loo, Z.-X., Liu, Y.-Y., Yeh, C.-L., Feng, C.-W., & Lin, K.-L. (2022). The Clinical Effects of Pixel CO2 Laser on Bladder Neck and Stress Urinary Incontinence. Journal of Clinical Medicine, 11(17), 4971. https://doi.org/10.3390/jcm11174971






