Superiority of MRI for Evaluation of Sacral Insufficiency Fracture
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Image Technique
2.3. Evaluation of Images
2.4. Statistical Analysis
3. Results
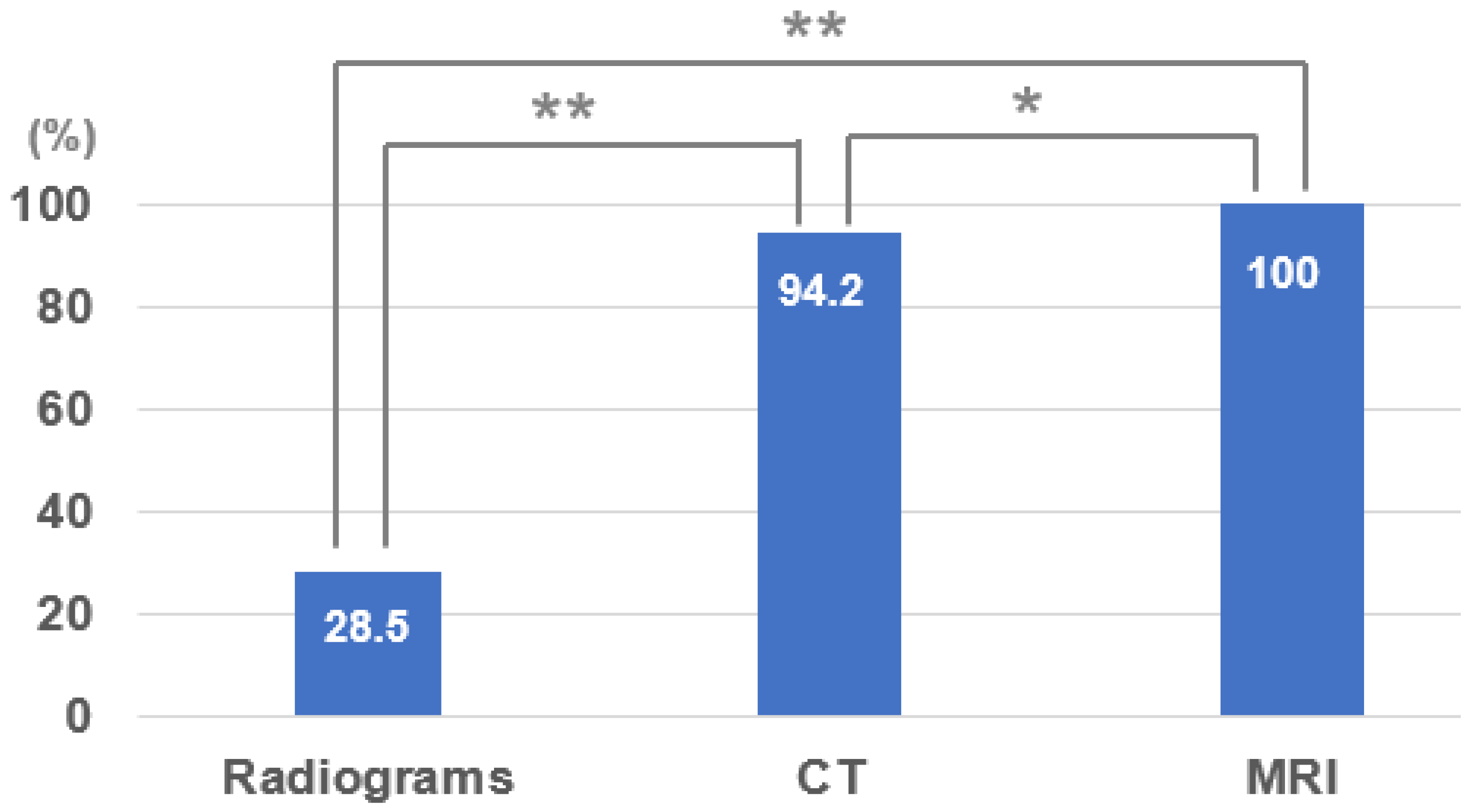
3.1. Sensitivity of Plain Radiograms, CT, and MRI
3.2. Accompanying Other Fracture
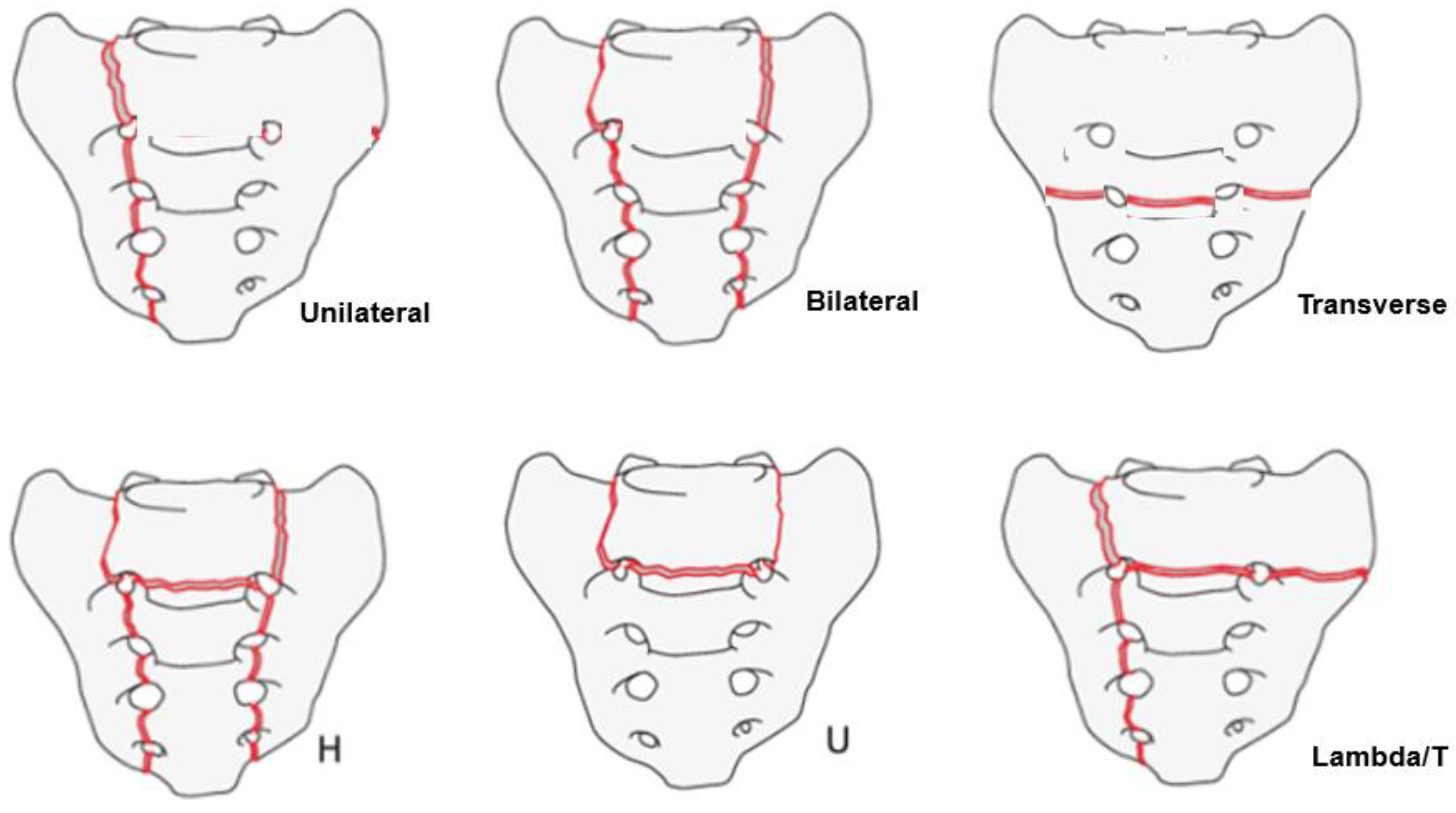
3.3. SIF Fracture Pattern
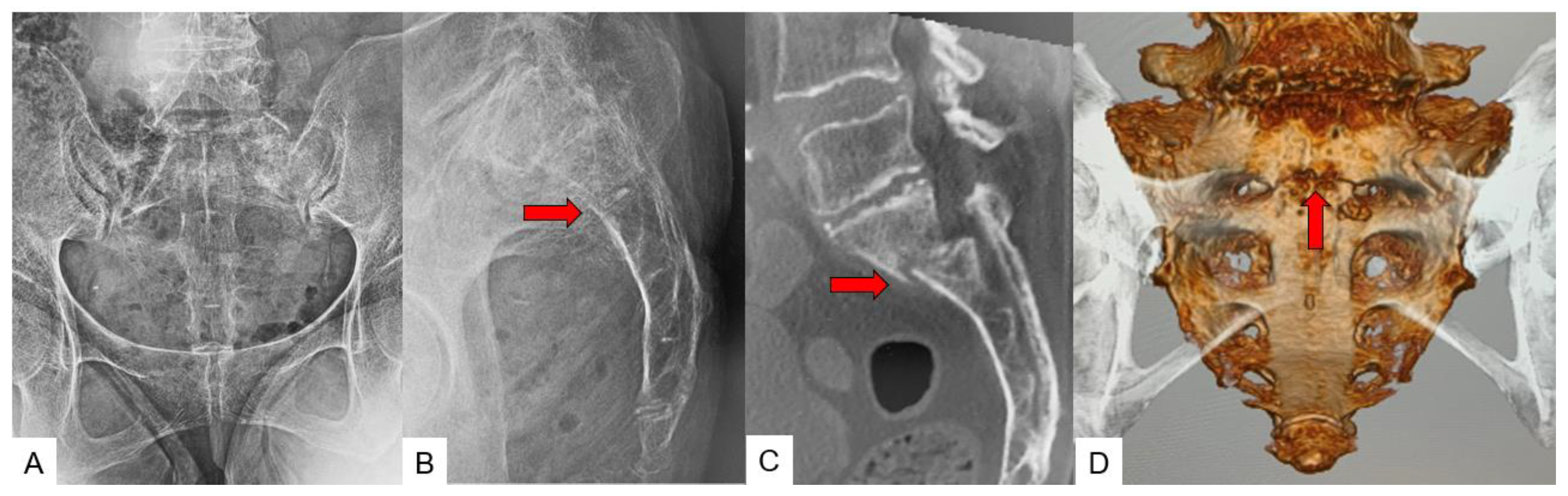
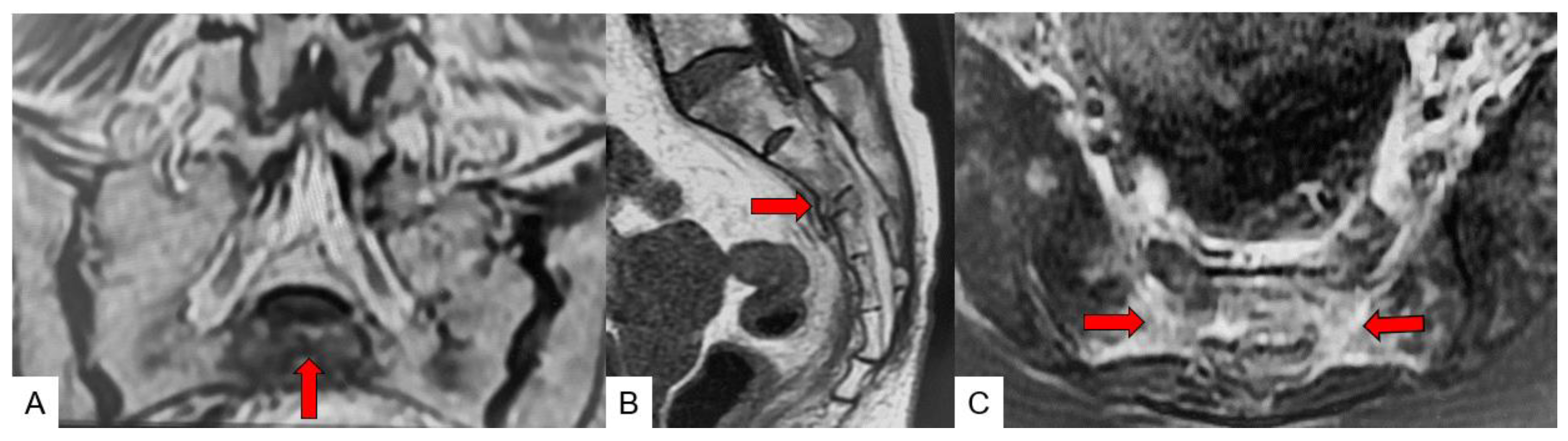
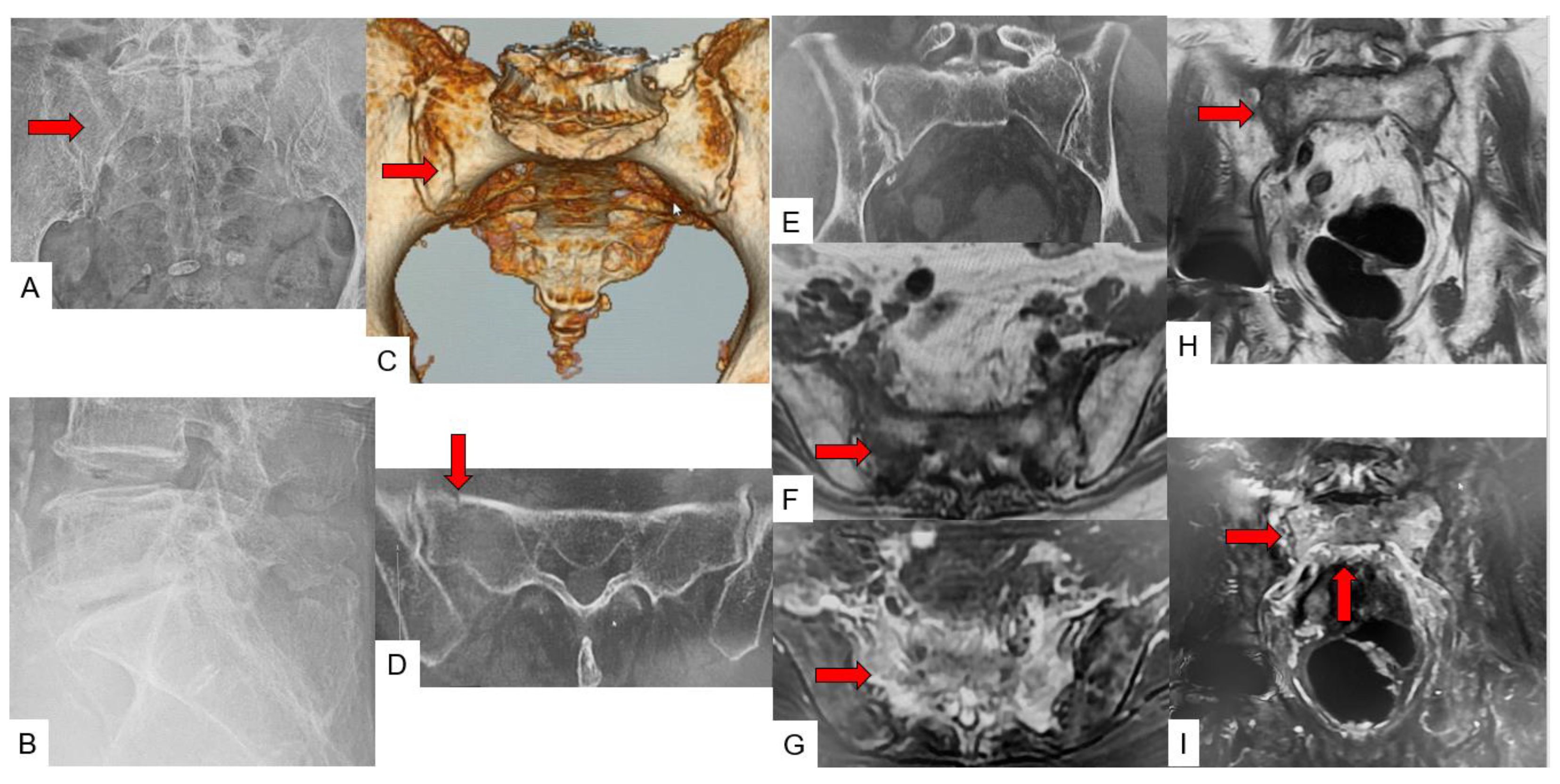
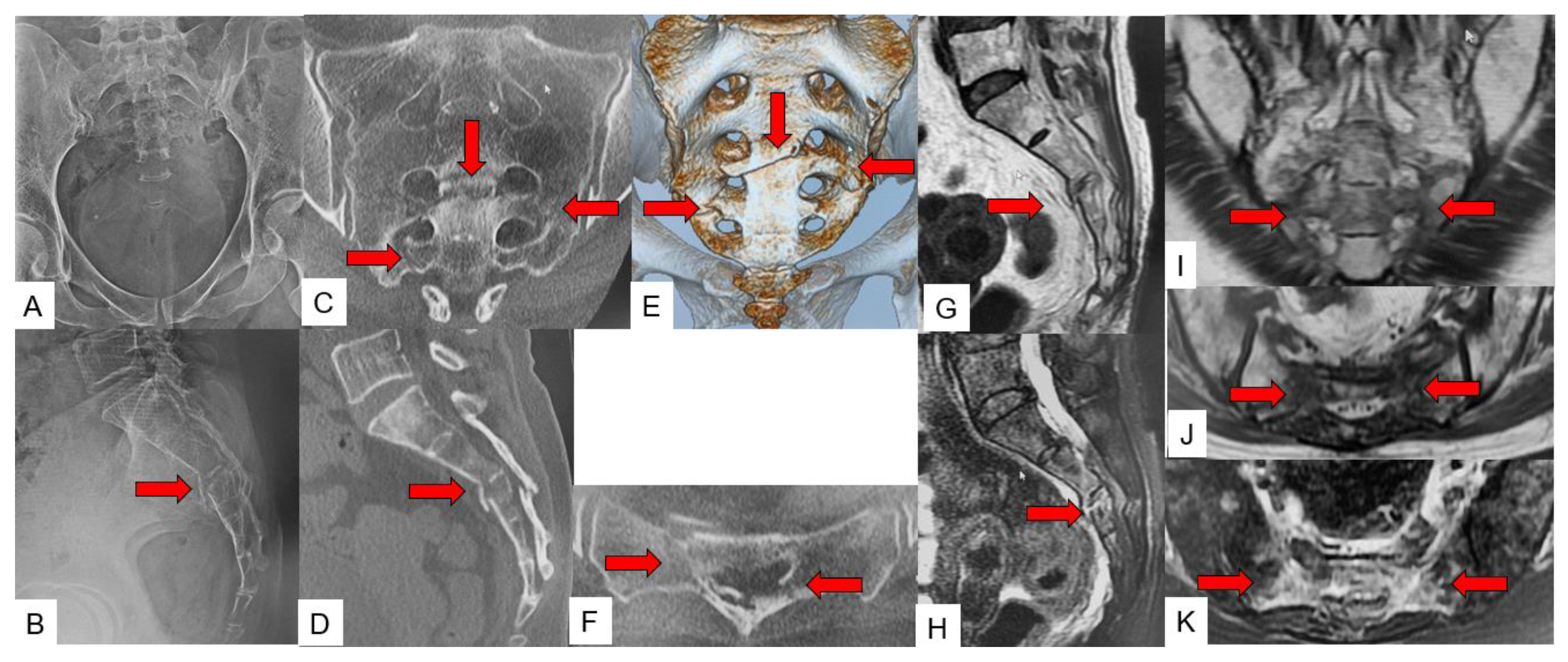
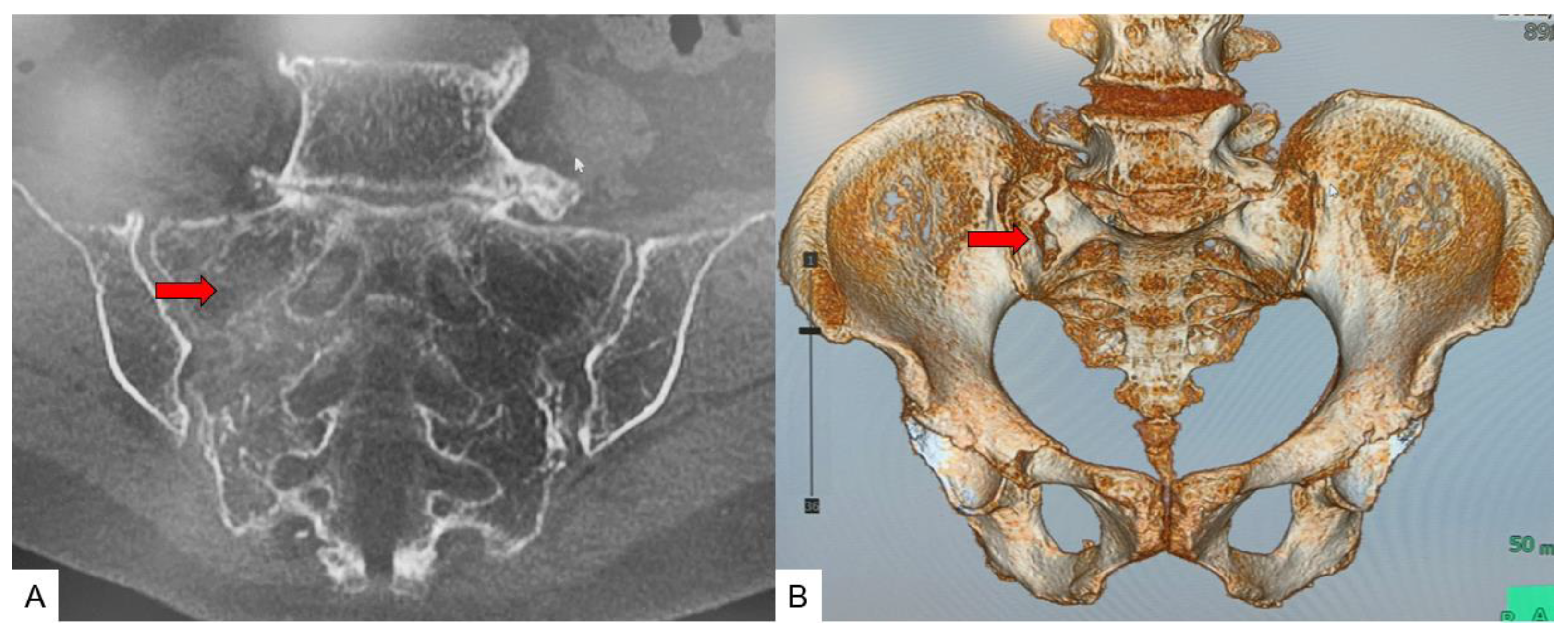
3.4. Typical SIF Case
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and Economic Burden of OsteoporosisRelated Fractures in the United States, 2005–2025. J. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Tatangelo, G.; Watts, J.; Lim, K.; Connaughton, C.; Abimanyi-Ochom, J.; Borgström, F.; Nicholson, G.C.; Shore-Lorenti, C.; Stuart, A.L.; Iuliano-Burns, S.; et al. The Cost of Osteoporosis, Osteopenia, and Associated Fractures in Australia in 2017. J. Bone Miner. Res. 2019, 34, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Buccino, F.; Colombo, C.; Vergani, L.M. A Review on Multiscale Bone Damage: From the Clinical to the Research Perspective. Materials 2021, 14, 1240. [Google Scholar] [CrossRef]
- Lourie, H. Spontaneous osteoporotic fracture of the sacrum. An unrecognized syndrome of the elderly. JAMA 1982, 248, 715–717. [Google Scholar] [CrossRef]
- Buell, T.J.; Yener, U.; Wang, T.R.; Buchholz, A.L.; Yen, C.P.; Shaffrey, M.E.; Shaffrey, C.I.; Smith, J.S. Sacral insufficiency fractures after lumbosacral arthrodesis: Salvage lumbopelvic fixation and a proposed management algorithm. J. Neurosurg. Spine 2020, 27, 225–236. [Google Scholar] [CrossRef]
- Razavian, N.; Laucis, A.; Sun, Y.; Spratt, D.E.; Owen, D.; Schonewolf, C.; Uppal, S.; Maturen, K.E.; Jolly, S. Radiation-Induced Insufficiency Fractures after Pelvic Irradiation for Gynecologic Malignancies: A Systematic Review. Int. J. Radiat. Oncol. Biol. Phys. 2020, 108, 620–634. [Google Scholar] [CrossRef]
- Na, W.C.; Lee, S.H.; Jung, S.; Jang, H.W.; Jo, S. Pelvic insufficiency fracture in severe osteoporosis patient. Hip Pelvis 2017, 29, 120–126. [Google Scholar] [CrossRef]
- Sudhir, G.; Kalra, L.K.; Acharya, S.; Chalal, R. Sacral insufficiency fractures mimicking lumbar spine pathology. Asian Spine J. 2016, 10, 558–564. [Google Scholar] [CrossRef][Green Version]
- Lassus, J.; Tulikoura, I.; Konttinen, Y.T.; Salo, J.; Santavirta, S. Bone stress injuries of the lower extremity: A review. Acta Orthop. Scand. 2002, 73, 359–368. [Google Scholar] [CrossRef]
- Graul, I.; Vogt, S.; Strube, P.; Hölzl, A. Significance of Lumbar MRI in Diagnosis of Sacral Insufficiency Fracture. Global Spine J. 2021, 11, 1197–1201. [Google Scholar] [CrossRef]
- Norimoto, M.; Yamashita, M.; Yamaoka, A.; Yamashita, K.; Abe, K.; Eguchi, Y.; Furuya, T.; Orita, S.; Inage, K.; Shiga, Y.; et al. Early mobilization reduces the medical care cost and the risk of disuse syndrome in patients with acute osteoporotic vertebral fractures. J. Clin. Neurosci. 2021, 93, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Wagner, D.; Hofmann, A. Minimal invasive surgical treatment of fragility fractures of the pelvis. Chirurgia 2017, 112, 524–537. [Google Scholar] [CrossRef] [PubMed]
- Demographic Statistics in Japan 2021, Ministry of Health, Labour and Welfare. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/geppo/nengai21/index.html (accessed on 1 February 2022).
- Chung, Y.K.; Lee, Y.K.; Yoon, B.H.; Suh, D.H.; Koo, K.H. Pelvic Insufficiency Fractures in Cervical Cancer after Radiation Therapy: A Meta-Analysis and Review. In Vivo 2021, 35, 1109–1115. [Google Scholar] [CrossRef] [PubMed]
- Lyders, E.M.; Whitlow, C.T.; Baker, M.D.; Morris, P.P. Imaging and treatment of sacral insufficiency fractures. AJNR Am. J. Neuroradiol. 2010, 31, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Pentecost, R.L.; Murray, R.A.; Brindley, H.H. Fatigue, insuffıcıency, and pathologıc fractures. JAMA 1964, 187, 1001–1004. [Google Scholar] [CrossRef]
- Gibbs, W.N.; Doshi, A. Sacral Fractures and Sacroplasty. Neuroimaging Clin. N Am. 2019, 29, 515–527. [Google Scholar] [CrossRef]
- Kolz, J.M.; Mitchell, S.A.; Elder, B.D.; Sebastian, A.S.; Huddleston, P.M.; Freedman, B.A. Sacral Insufficiency Fracture Following Short-Segment Lumbosacral Fusion: Case Series and Review of the Literature. Global Spine J. 2022, 12, 267–277. [Google Scholar] [CrossRef]
- Schneider, R.; Yacovone, J.; Ghelman, B. Unsuspected sacral fractures: Detection by radionuclide bone scanning. AJR 1985, 144, 337–341. [Google Scholar] [CrossRef]
- Peh, W.C.; Khong, P.L.; Yin, Y.; Ho, W.Y.; Evans, N.S.; Gilula, L.A.; Yeung, H.W.; Davies, A.M. Imaging of pelvic insufficiency fractures. Radiographics 1996, 16, 335–348. [Google Scholar] [CrossRef]
- Al-faham, Z.; Rydberg, J.N.; Oliver Wong, C.Y. Use of SPECT/CT with 99mTc-MDP bone scintigraphy to diagnose sacral insufficiency fracture. J. Nucl. Med. Technol. 2014, 42, 240–241. [Google Scholar] [CrossRef]
- Denis, F.; Davis, S.; Comfort, T. Sacral fractures: An important problem. Retrospective analysis of 236 cases. Clin. Orthop. Relat. Res. 1988, 227, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Roy-Camille, R.; Saillant, G.; Gagna, G.; Mazel, C. Transverse fracture of the upper sacrum. Suicidal jumper’s fracture. Spine 1985, 10, 838–845. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.R.; Schroeder, G.D.; Divi, S.N.; Kepler, C.K.; Kleweno, C.P.; Krieg, J.C.; Wilson, J.R.; Holstein, J.H.; Kurd, M.F.; Firoozabadi, R.; et al. Description and reliability of the AOSpine sacral classification system. J. Bone Joint Surg. 2020, 16, 1454–1463. [Google Scholar] [CrossRef]
- Cabarrus, M.C.; Ambekar, A.; Lu, Y.; Link, T.M. MRI and CT of insufficiency fractures of the pelvis and the proximal femur. AJR Am. J. Roentgenol. 2008, 191, 995–1001. [Google Scholar] [CrossRef]
- Henes, F.O.; Nuchtern, J.V.; Groth, M.; Habermann, C.R.; Regier, M.; Rueger, J.M.; Adam, G.; Großterlinden, L.G. Comparison of diagnostic accuracy of magnetic resonance imaging and multidetector computed tomography in the detection of pelvic fractures. Eur. J. Radiol. 2012, 81, 2337–2342. [Google Scholar] [CrossRef]
- Gotis-Graham, I.; McGuigan, L.; Diamond, T.; Portek, I.; Quinn, R.; Sturgess, A.; Tulloch, R. Sacral insufficiency fractures in the elderly. J. Bone Joint Surg. Br. 1994, 76, 882–886. [Google Scholar] [CrossRef]
- Pulley, B.R.; Cotman, S.B.; Fowler, T.T. Surgical Fixation of Geriatric Sacral U-Type Insufficiency Fractures: A Retrospective Analysis. J. Orthop. Trauma. 2018, 32, 617–622. [Google Scholar] [CrossRef]
- Balling, H. Navigated Transsacral Screw Fixation for the Treatment of Bilateral Sacral Insufficiency Fractures. Clin Spine Surg. 2021, 34, 286–290. [Google Scholar] [CrossRef]
- Deen, H.G.; Nottmeier, E.W. Balloon kyphoplasty for treatment of sacral insufficiency fractures: Report of three cases. Neurosurg. Focus 2005, 18, e7. [Google Scholar] [CrossRef]
- Shah, R.V. Sacral kyphoplasty for the treatment of painful sacral insufficiency fractures and metastases. Spine J. 2012, 12, 113–120. [Google Scholar] [CrossRef]


| N = 77 | |
|---|---|
| Gender (Men:Women) | 11:66 |
| Age (mean ± S.D.) (year) | 80.3 ± 10.4 |
| Height (mean ± S.D.) (cm) | 150.6 ± 8.6 |
| Body weight (mean ± S.D.) (kg) | 47.4 ± 9.2 |
| Body mass index (mean ± S.D.) (kg/m2) | 21.0 ± 3.9 |
| Bone mineral density lumbar (g/cm2) T-score lumbar | 0.747 ± 0.16 −2.4 ± 0.5 |
| Bone mineral density hip (g/cm2) T-score hip | 0.583 ± 0.10 −2.3 ± 1.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamauchi, T.; Sharma, S.; Chandra, S.; Tanaka, M.; Fujiwara, Y.; Arataki, S.; Sharma, A.; Yokoyama, Y.; Oomori, T.; Kanamaru, A.; et al. Superiority of MRI for Evaluation of Sacral Insufficiency Fracture. J. Clin. Med. 2022, 11, 4968. https://doi.org/10.3390/jcm11174968
Yamauchi T, Sharma S, Chandra S, Tanaka M, Fujiwara Y, Arataki S, Sharma A, Yokoyama Y, Oomori T, Kanamaru A, et al. Superiority of MRI for Evaluation of Sacral Insufficiency Fracture. Journal of Clinical Medicine. 2022; 11(17):4968. https://doi.org/10.3390/jcm11174968
Chicago/Turabian StyleYamauchi, Taro, Sagar Sharma, Sarath Chandra, Masato Tanaka, Yoshihiro Fujiwara, Shinya Arataki, Ayush Sharma, Yusuke Yokoyama, Toshinori Oomori, Akihiro Kanamaru, and et al. 2022. "Superiority of MRI for Evaluation of Sacral Insufficiency Fracture" Journal of Clinical Medicine 11, no. 17: 4968. https://doi.org/10.3390/jcm11174968
APA StyleYamauchi, T., Sharma, S., Chandra, S., Tanaka, M., Fujiwara, Y., Arataki, S., Sharma, A., Yokoyama, Y., Oomori, T., Kanamaru, A., Masuda, S., Shimizu, N., Torigoe, K., & Honda, O. (2022). Superiority of MRI for Evaluation of Sacral Insufficiency Fracture. Journal of Clinical Medicine, 11(17), 4968. https://doi.org/10.3390/jcm11174968







