Transoral Tongue Suspension for Obstructive Sleep Apnea—A Preliminary Study
Abstract
:1. Introduction
2. Methods
2.1. Ethics Statement
2.2. Study Population
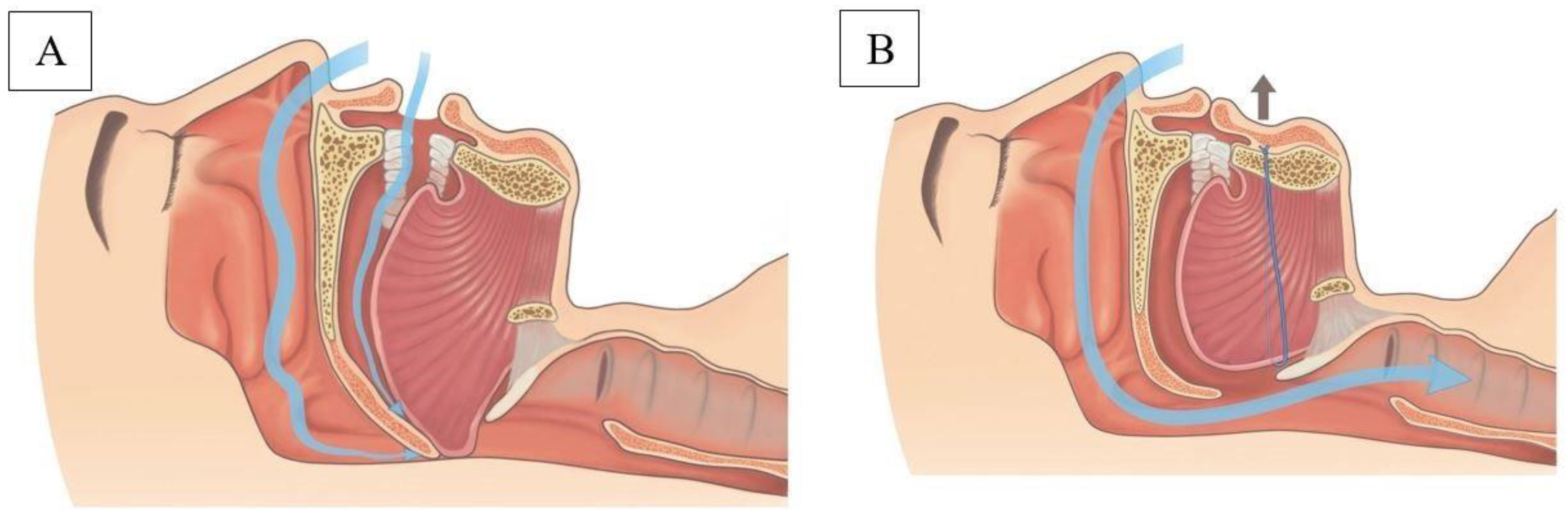
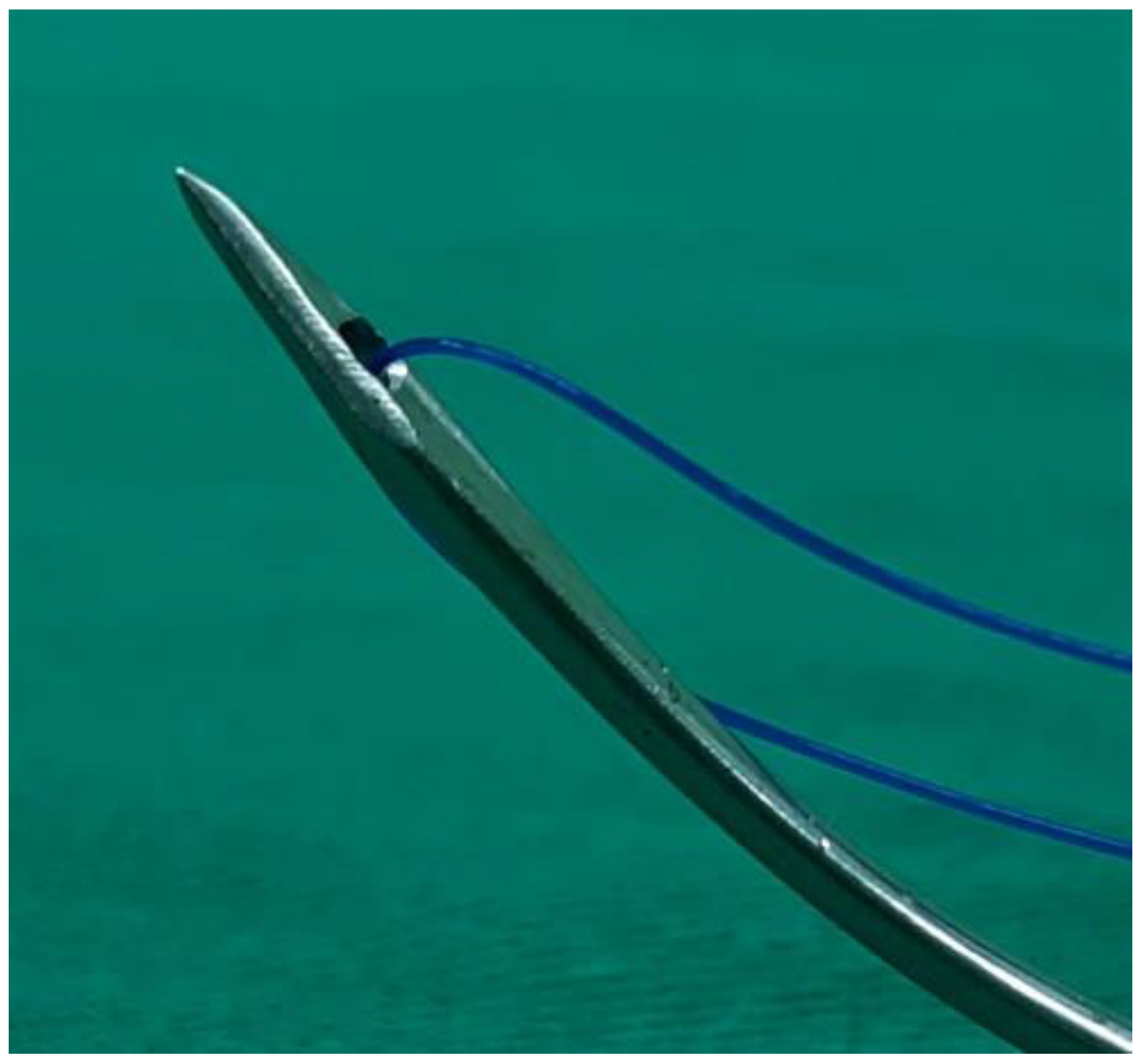
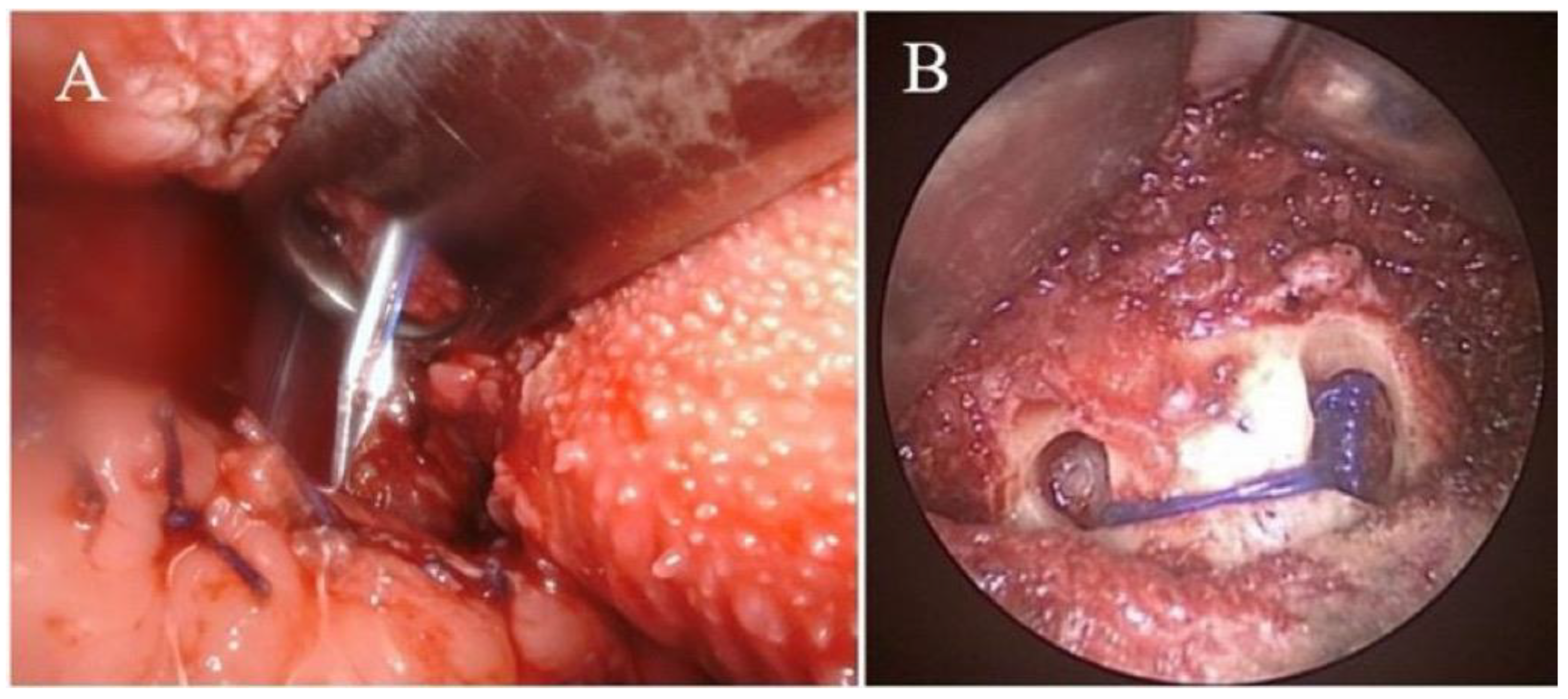
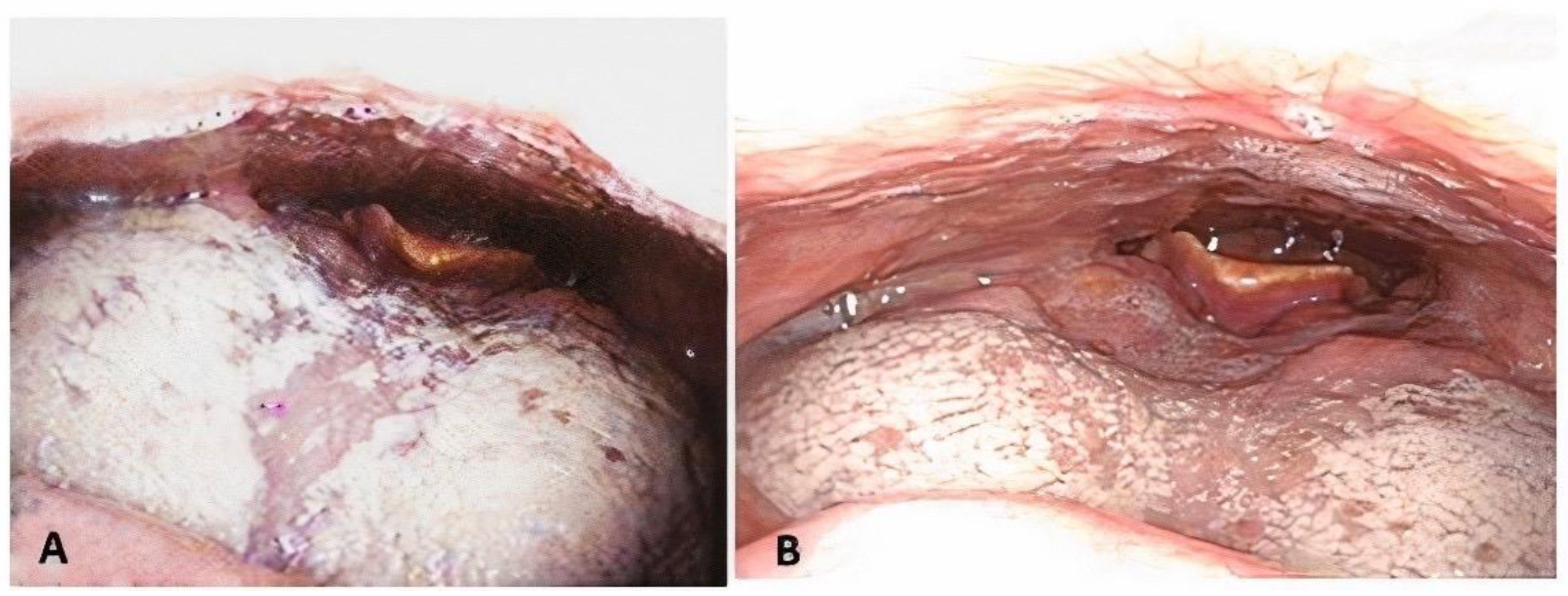
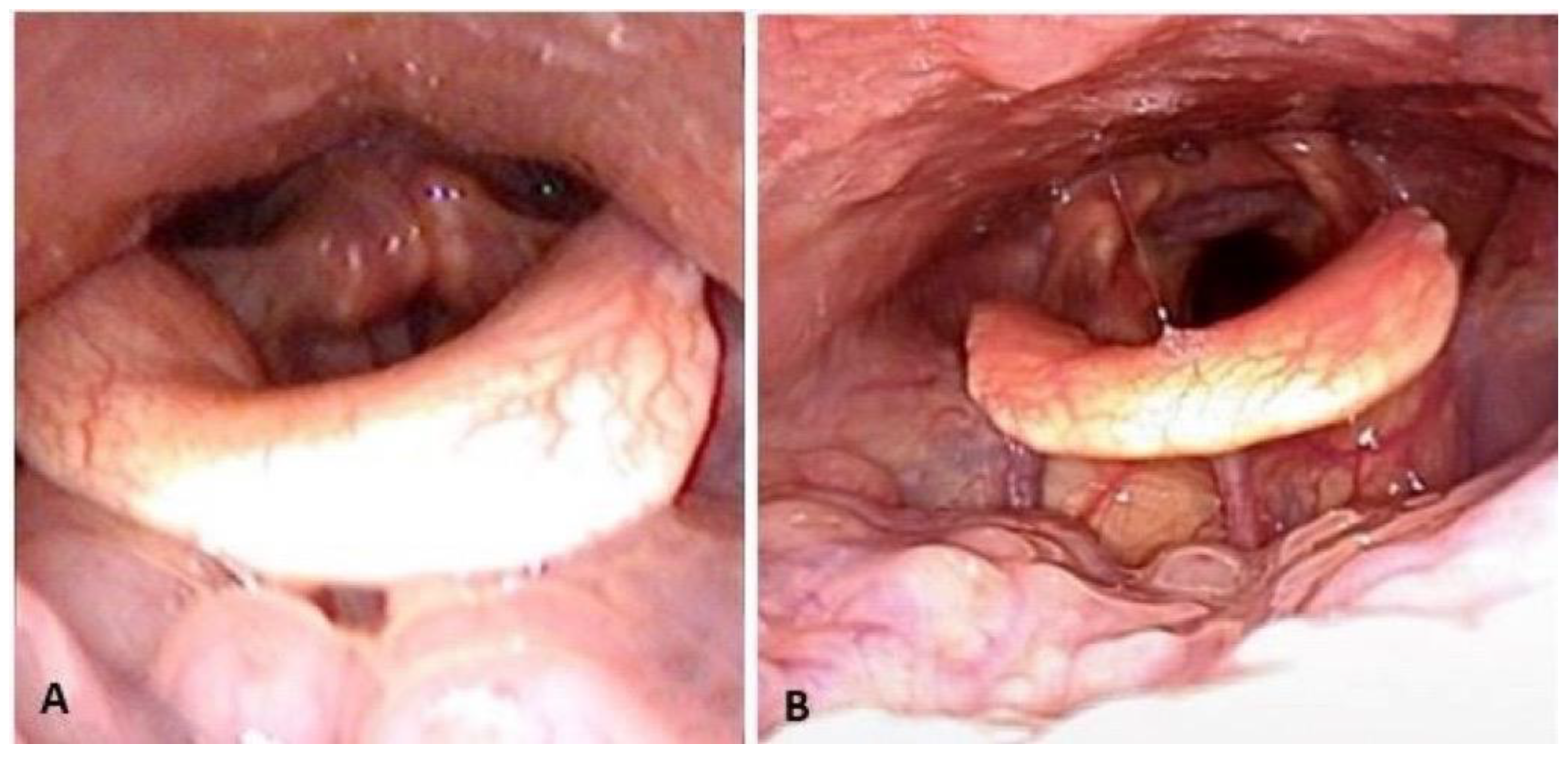
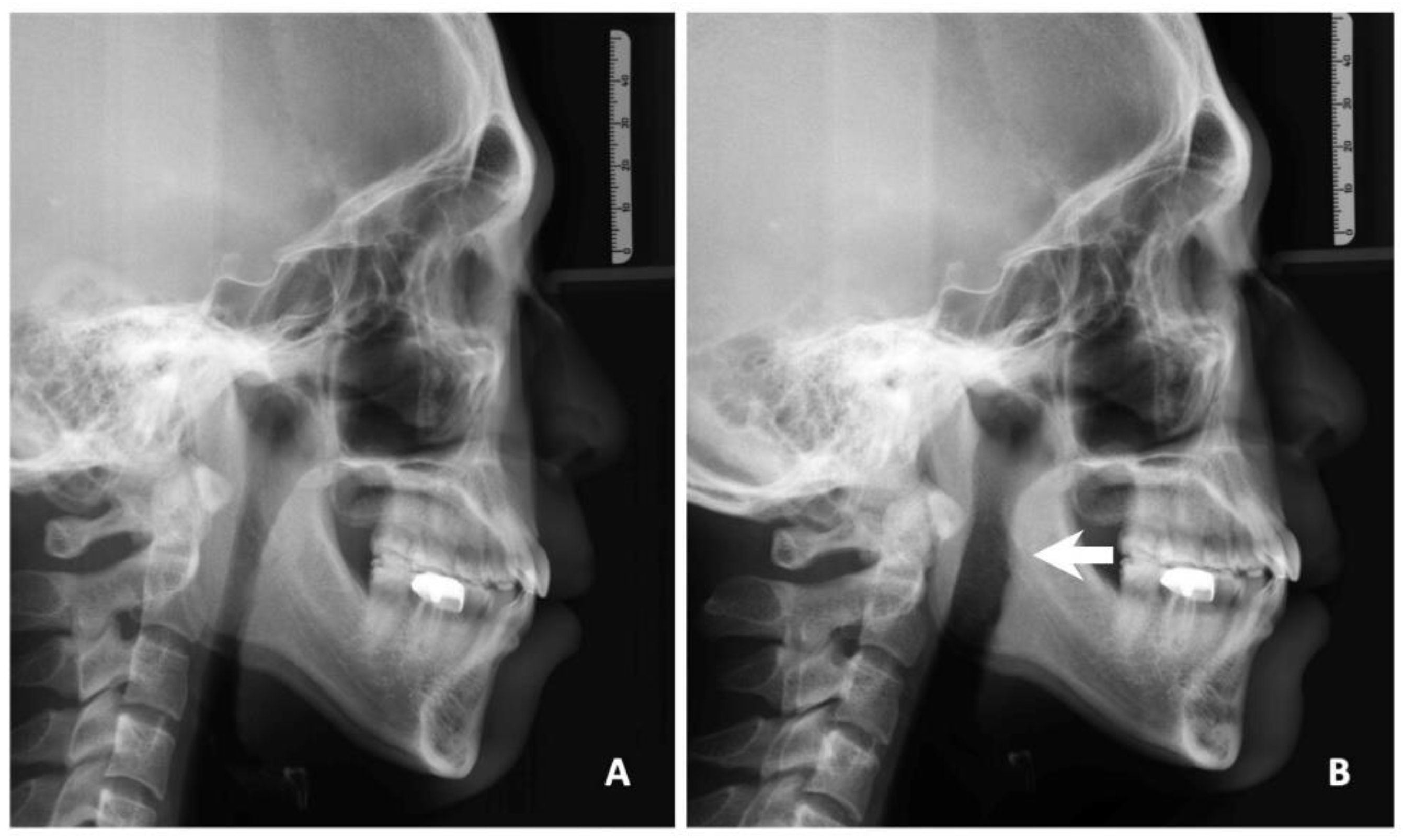
2.3. Surgical Technique of TOTS
2.4. Study Parameters
2.5. Statistical Analysis
3. Results
Surgical Outcomes
4. Discussion
4.1. Comparison of Previous Techniques
4.2. Comparison of Outcomes
4.3. Applications
4.4. Limitations
4.5. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Strollo, P.J.; Roger, R.M. Obstructive sleep apnea. N. Engl. J. Med. 1996, 334, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Garvey, J.F.; Pengo, M.F.; Drakatos, P.; Kent, B.D. Epidemiological aspects of obstructive sleep apnea. J. Thorac. Dis. 2015, 7, 920. [Google Scholar] [CrossRef] [PubMed]
- Eckert, D.J.; White, D.P.; Jordan, A.S.; Malhotra, A.; Wellman, A. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am. J. Respir. Crit. Care Med. 2013, 188, 996–1004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bin Heyat, M.B.; Akhtar, F.; Ansari, M.A. Progress in Detection of Insomnia Sleep Disorder: A Comprehensive Review. Curr. Drug Targets 2021, 22, 672–684. [Google Scholar] [CrossRef]
- Kezirian, E.J.; Hohenhorst, W.; de Vries, N. Drug-induced sleep endoscopy: The VOTE classification. Eur. Arch. Otorhinolaryngol. 2011, 268, 1233–1236. [Google Scholar] [CrossRef]
- Lee, L.A.; Yu, J.F.; Lo, Y.L.; Chen, N.H.; Fang, T.J.; Huang, C.G.; Cheng, W.N.; Li, H.Y. Comparative effects of snoring sound between two minimally invasive surgeries in the treatment of snoring: A randomized controlled trial. PLoS ONE 2014, 9, e97186. [Google Scholar] [CrossRef]
- Kezirian, E.J.; Goldberg, A.N. Hypopharyngeal surgery in obstructive sleep apnea: An evidence-based medicine review. Arch. Otorhinolaryngol.—Head Neck Surg. 2006, 132, 206–213. [Google Scholar] [CrossRef] [Green Version]
- Lal, C.; Strange, C.; Bachman, D. Neurocognitive impairment in obstructive sleep apnea. Chest 2012, 141, 1601–1610. [Google Scholar] [CrossRef]
- Yaggi, H.K.; Concato, J.; Kernan, W.N.; Lichtman, J.H.; Brass, L.M.; Mohsenin, V. Obstructive sleep apnea as a risk factor for stroke and death. N. Engl. J. Med. 2005, 353, 2034–2041. [Google Scholar] [CrossRef] [Green Version]
- Bradley, T.D.; Floras, J.S. Obstructive sleep apnoea and its cardiovascular consequences. Lancet 2009, 373, 82–93. [Google Scholar] [CrossRef]
- Sullivan, C.E.; Issa, F.G.; Berthon-Jones, M.; Eves, L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1981, 1, 862–865. [Google Scholar] [CrossRef]
- Li, H.Y.; Lee, L.A.; Tsai, M.S.; Chen, N.H.; Chuang, L.P.; Fang, T.J.; Shen, S.C.; Cheng, W.N. How to manage continuous positive airway pressure (CPAP) failure-hybrid surgery and integrated treatment. Auris Nasus Larynx 2000, 47, 335–342. [Google Scholar] [CrossRef]
- Fujita, S.; Conway, W.; Zorick, F.; Roth, T. Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: Uvulopalatopharyngoplasty. Otolaryngol.—Head Neck Surg. 1981, 89, 923–934. [Google Scholar] [CrossRef]
- Sher, A.E.; Schechtman, K.B.; Piccirillo, J.F. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 1996, 19, 156–177. [Google Scholar] [CrossRef] [Green Version]
- Li, H.Y.; Wang, P.C.; Li, L.A.; Chen, N.H.; Fang, T.J. Prediction of uvulopalatopharyngoplasty outcome: Anatomy-based staging system versus severity-based staging system. Sleep 2006, 29, 1537–1541. [Google Scholar] [CrossRef]
- Lin, H.C.; Friedman, M. Volumetric Tongue Reduction for Obstructive Sleep Apnea. Sleep Med. Clin. 2019, 14, 59–65. [Google Scholar] [CrossRef]
- Bostanci, A.; Turhan, M. A systematic review of tongue base suspension techniques as an isolated procedure or combined with uvulopalatopharyngoplasty in obstructive sleep apnea. Eur. Arch. Otorhinolaryngol. 2016, 273, 2895–2901. [Google Scholar] [CrossRef]
- Handler, E.; Hamans, E.; Goldberg, A.N.; Mickelson, S. Tongue suspension: An evidence-based review and comparison to hypopharyngeal surgery for OSA. Laryngoscope 2014, 124, 329–336. [Google Scholar] [CrossRef]
- Miller, F.R.; Watson, D.; Malis, D. Role of the tongue base suspension suture with The Repose System bone screw in the multilevel surgical management of obstructive sleep apnea. Otolaryngol.—Head Neck Surg. 2002, 126, 392–398. [Google Scholar] [CrossRef]
- Omur, M.; Ozturan, D.; Elez, F.; Unver, C.; Derman, S. Tongue base suspension combined with UPPP in severe OSA patients. Otolaryngol.—Head Neck Surg. 2005, 133, 218–223. [Google Scholar] [CrossRef]
- Tsou, Y.A.; Huang, C.W.; Wu, T.F.; Hung, L.W.; Chang, W.D. The effect of tongue base suspension with uvulopalato-pharyngoplasty on sleep quality in obstructive sleep apnea. Sci. Rep. 2018, 8, 8788. [Google Scholar] [CrossRef]
- Johns, M.W. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth Sleepiness Scale. Chest 1993, 103, 30–36. [Google Scholar] [CrossRef]
- Friedman, M.; Ibrahim, H.; Joseph, N.J. Staging of obstructive sleep apnea/hypopnea syndrome: A guide to appropriate treatment. Laryngoscope 2004, 114, 454–459. [Google Scholar] [CrossRef] [Green Version]
- Mayhew, D.; Mendonca, V.; Murthy, B.V.S. A review of ASA physical status—Historical perspectives and modern developments. Anaesthesia 2019, 74, 373–379. [Google Scholar] [CrossRef] [Green Version]
- Friedman, M.; Yalamanchali, S.; Gorelick, G.; Joseph, N.J.; Hwang, M.S. A standardized lingual tonsil grading system: Inter-examiner agreement. Otolaryngol.—Head Neck Surg. 2015, 152, 667–672. [Google Scholar] [CrossRef]
- Li, H.Y.; Lee, L.A.; Kezirian, E.J. Coblation endoscopic lingual lightening (CELL) for obstructive sleep apnea. Eur. Arch. Otorhinolaryngol. 2016, 273, 231–236. [Google Scholar] [CrossRef]
- Vicini, C.; Montevecchi, F.; Gobbi, R.; De Vito, A.; Meccariello, G. Transoral robotic surgery for obstructive sleep apnea syndrome: Principles and technique. World J. Otorhinolaryngol. Head Neck Surg. 2017, 13, 97–100. [Google Scholar] [CrossRef]
- Li, K.K.; Riley, R.W.; Powell, N.B.; Troell, R.J. Obstructive sleep apnea surgery: Genioglossus advancement revisited. J. Oral Maxillofac. Surg. 2001, 59, 1181–1184. [Google Scholar] [CrossRef]
- Foltán, R.; Hoffmannová, J.; Pretl, M.; Donev, F.; Vlk, M. Genioglossus advancement and hyoid myotomy in treating obstructive sleep apnoea syndrome–A follow-up study. J. Cranio-Maxillofac. Surg. 2007, 35, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Woodson, B.T. A Tongue Suspension Suture for Obstructive Sleep Apnea and Snorers. Otolaryngol.—Neck Surg. 2001, 124, 297–303. [Google Scholar] [CrossRef]
- Kocdor, P.; Froymovich, O.; Mickelson, S. Tongue base suspension procedures for obstructive sleep apnea syndrome. Oper. Tech. Otolaryngol.-Head Neck Surg. 2015, 26, 187–192. [Google Scholar] [CrossRef]
- Sezen, O.S.; Aydin, E.; Eraslan, G.; Haytoglu, S.; Coskuner, T.; Unver, S. Modified tongue base suspension for multilevel or single level obstructions in sleep apnea: Clinical and radiologic results. Auris Nasus Larynx. 2011, 38, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Turhan, M.; Bostanci, A.; Bozkurt, S. Predicting the outcome of modified tongue base suspension combined with uvulopalatopharyngoplasty. Eur. Arch. Otorhinolaryngol. 2015, 272, 3411–3416. [Google Scholar] [CrossRef] [PubMed]
- Anuwong, A.; Ketwong, K.; Jitpratoom, P.; Sasanakietkul, T.; Duh, Q. Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg. 2018, 153, 21–27. [Google Scholar] [CrossRef]
- Turhan, M.; Bostanci, A.; Akdag, M. The impact of modified tongue base suspension on CPAP levels in patients with severe OSA. Eur. Arch. Otorhinolaryngol. 2015, 272, 995–1000. [Google Scholar] [CrossRef]
- Chen, L.W.; Razavi, C.R.; Hong, H.; Fondong, A.; Ranganath, R.; Khatri, S.; Mydlarz, W.K.; Mathur, A.; Ishii, M.; Nellis, J.; et al. Cosmetic outcomes following transoral versus transcervical thyroidectomy. Head Neck 2020, 42, 3336–3344. [Google Scholar] [CrossRef]
- Vicente, E.; Marín, J.M.; Carrizo, S.; Naya, M.J. Tongue-base suspension in conjunction with uvulopalatopharyngoplasty for treatment of severe obstructive sleep apnea: Long-term follow-up results. Laryngoscope 2006, 116, 1223–1227. [Google Scholar] [CrossRef]
- Woodson, B.T.; Derowe, A.; Hawke, M. Pharyngeal suspension suture with repose bone screw for obstructive sleep apnea. Otolaryngol.—Head Neck Surg. 2000, 122, 395–401. [Google Scholar] [CrossRef]
- Yüksel, A.; Ugur, K.S.; Kizilbulut, G. Long-term results of one staged multilevel surgery with tongue suspension surgery or one level palatal surgery for treatment of moderate and severe obstructive sleep apnea. Eur. Arch. Otorhinolaryngol. 2016, 273, 1227–1234. [Google Scholar] [CrossRef]


| Variables | Preoperative | Postoperative | p-Value |
|---|---|---|---|
| ESS | 11.4 ± 3.2 | 5.7 ± 1.6 | 0.0006 |
| AHI (event/H) | 42.2 ± 21.8 | 19.5 ± 16.2 | <0.001 |
| Mini-SAT (%) | 77.1 ± 12.2 | 81.7 ± 8.1 | 0.026 |
| SI (event/H) | 207 ± 141 | 101 ± 91 | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsin, L.-J.; Lee, Y.-C.; Lin, W.-N.; Lu, Y.-A.; Lee, L.-A.; Tsai, M.-S.; Cheng, W.-N.; Chiang, Y.-T.; Li, H.-Y. Transoral Tongue Suspension for Obstructive Sleep Apnea—A Preliminary Study. J. Clin. Med. 2022, 11, 4960. https://doi.org/10.3390/jcm11174960
Hsin L-J, Lee Y-C, Lin W-N, Lu Y-A, Lee L-A, Tsai M-S, Cheng W-N, Chiang Y-T, Li H-Y. Transoral Tongue Suspension for Obstructive Sleep Apnea—A Preliminary Study. Journal of Clinical Medicine. 2022; 11(17):4960. https://doi.org/10.3390/jcm11174960
Chicago/Turabian StyleHsin, Li-Jen, Yi-Chan Lee, Wan-Ni Lin, Yi-An Lu, Li-Ang Lee, Ming-Shao Tsai, Wen-Nuan Cheng, Yen-Ting Chiang, and Hsueh-Yu Li. 2022. "Transoral Tongue Suspension for Obstructive Sleep Apnea—A Preliminary Study" Journal of Clinical Medicine 11, no. 17: 4960. https://doi.org/10.3390/jcm11174960
APA StyleHsin, L.-J., Lee, Y.-C., Lin, W.-N., Lu, Y.-A., Lee, L.-A., Tsai, M.-S., Cheng, W.-N., Chiang, Y.-T., & Li, H.-Y. (2022). Transoral Tongue Suspension for Obstructive Sleep Apnea—A Preliminary Study. Journal of Clinical Medicine, 11(17), 4960. https://doi.org/10.3390/jcm11174960








