1. Introduction
In February 2021, the number of confirmed cases of the COVID-19 pandemic worldwide was more than one hundred million, of which more than two million had led to the death of the patient. In the same period, more than two million positive cases of SARS-CoV-2 infection were recorded in Italy, making our country the eighth in the world and the fourth in Europe for total cases [
1]. Italy was also the sixth deadliest country in the world and the second in Europe for the number of deaths with more than ninety-one thousand victims.
One of the characteristics of the SARS-CoV-2 infection observed in Italy is the large regional difference in terms of lethality and mortality due to COVID-19 [
1]. These geographical differences were very clear in the first wave and partially confirmed in the second one as well [
2]. The first death due to severe acute respiratory syndrome infection in a COVID-19 positive patient was observed in the Lombardy region (the highest populated among the 21 Italian regions) on 21 February 2020. Since February, the municipalities located in Northern Italy were the Italian regions most severely hit by the pandemic up to 31 May 2020, as represented by a noticeable or substantial excess in overall mortality [
1]. A new rise in the pandemic curve was observed from September 2020 after the end of the summer holidays. Significant outbreaks began to increase in number, starting in the largest Italian cities such as Milan, Rome, and Naples in Southern Italy [
3].
Italy’s first response to COVID-19 has been described in detail as an unprecedented challenge by the World Health Organization (WHO) in a 2020 report [
4]. In the WHO report, it is emphasized that the Italian healthcare system is a regionally based national health system, and highly decentralized. The Italian Constitution makes health protection a shared responsibility between the central government and the 21 Italian regions. The central government legislates on the principles assessed in the Italian Constitution, but the regions can adapt them to their local contexts and have the budgets to manage healthcare delivery through local health agencies [
4]. In fact, the National Health System in Italy has been strongly regionalized for over 30 years with substantial regional differences in terms of management, financing, objectives, and models adopted.
Despite such a decentralized healthcare system and the stagnation of the Italian economy and growth for decades compared to other European and most developed countries, the world’s healthiest people were those living in Italy, after Spain, based on the Bloomberg 2019 Healthiest Country Index [
5]. The National Healthcare Service has faced increasing pressure during the COVID-19 pandemic.
The aim of this study is to analyze whether any correlation between regional differences in COVID-19 mortality and different regional care models, levels of funding, and socio-economic and demographic features occurred.
3. Results
Table 1 reports the distribution of COVID-19 total deaths and COVID-19 deaths adjusted for the number of inhabitants in 21 Italian regions.
Primarily, a simple linear regression was used to test if each variable significantly predicted the COVID-19 death rate (per 10,000). Our analysis revealed two main findings.
Firstly, it was found that the number of hospital beds (per 1000) significantly predicted the COVID-19 death rate (β = 17.64346, 95% CI 9.740126 25.5468, p < 0.0001). The Italian regions with a higher number of hospital beds (×1000 inhabitants) showed a higher number of deaths. The fitted regression model was: COVID-19 death rate = −40.49563 + 17.64346 * (N of hospital beds per 1000). The overall regression was statistically significant (r2 = 0.5347, F (1, 19) = 21.83, p = 0.0002).
Secondly, the number of general practitioners (GPs) (per 10,000 inhabitants) significantly predicted the COVID-19 death rate (β = −33.48067, 95% CI −57.7291 −9.232238, p = 0.0094): the Italian regions with a higher number of GPs showed a lower number of COVID-19 deaths. The fitted regression model was: COVID-19 death rate = 45.84148–33.48067 * (N of GPs per 10,000 inhabitants). The overall regression was statistically significant (r2 = 0.3053, F (1, 19) = 8.35, p = 0.0094). No associations were found between COVID-19 mortality rate and health expenditure per capita, life expectancy, aging index, and percentage of over 65 years old subjects per Italian region in the univariate analyses.
To assess the best predictors of COVID-19 mortality rate among the considered parameters, three different multivariate linear regression analyses were performed to overcome the risk of collinearity with the percentage of 65 years old subjects, the aging index, and the life expectancy. The COVID-19 mortality rate was used as a dependent variable in all models. The results of the three models are shown in
Table 2.
All three models confirmed the results of the univariate analyses. In all three models, the number of hospital beds (×1000 inhabitants) represented the best predictors of the COVID-19 mortality rate, with a direct relationship between the number of deaths and the number of hospital beds, and an inverse relationship between the number of COVID-19 deaths and number of GPs was found. These findings suggest that the Italian regions with a higher amount of centralized healthcare, as represented by the number of hospital beds, experienced a higher number of deaths, while the regions with greater community support, as represented by the number of the GPs, faced higher survival (
Table 2).
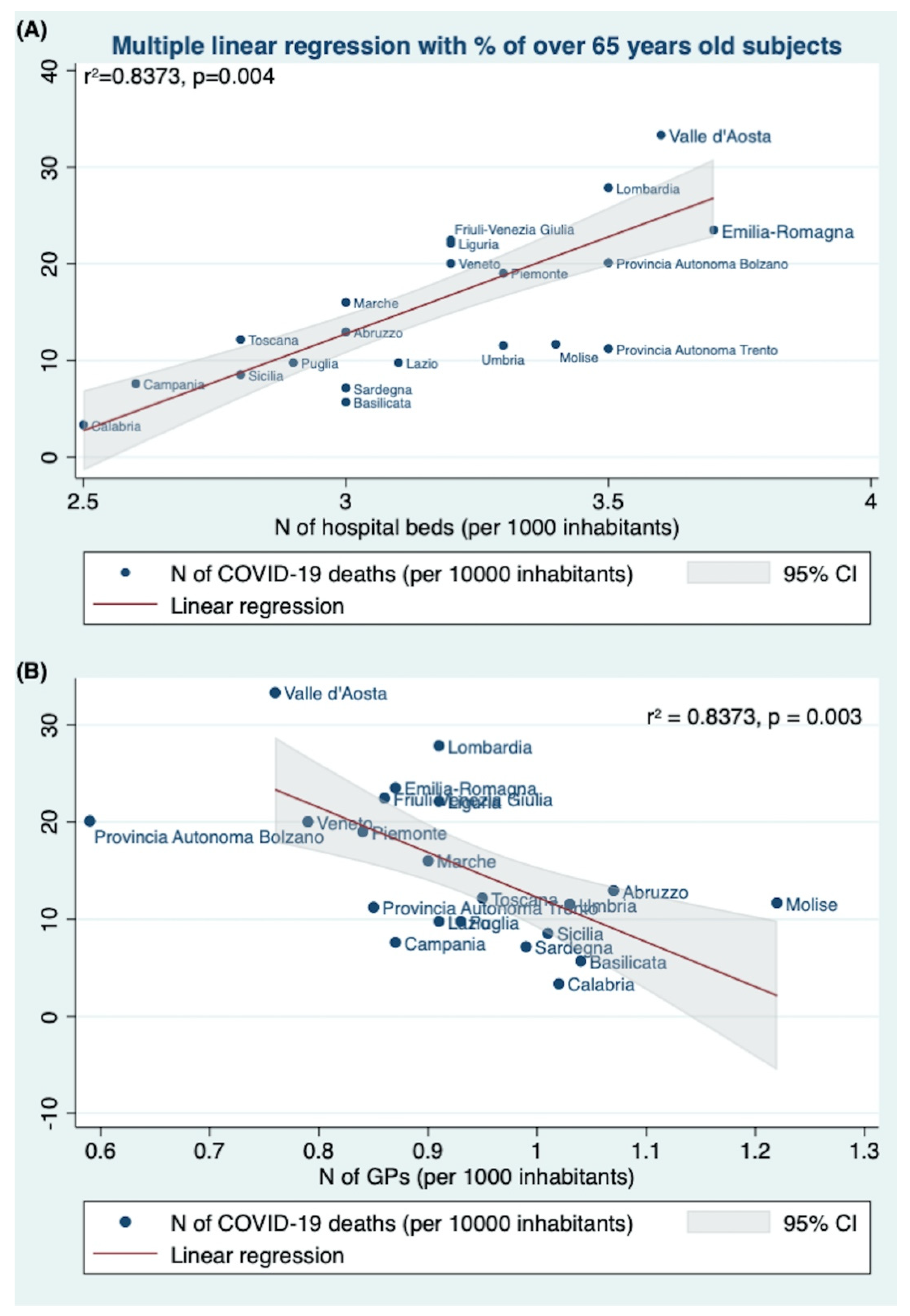
In the first model, the multiple linear regression analysis tested if the percentage of subjects ≥65 years old, the number of hospital beds (per 1000), the health expenditure per capita, the GPs per 1000, and the number of LTCF significantly predicted the COVID-19 death rate (per 100,000). The fitted regression model was: −13.01125 + 0.6861688 * (% of over65 yrs old) + 14.83807 * (N of hospital beds per 1000) − 14.83807 * (Health expenditure per capita) − 33.64296 * (N of GPs per 1000) + 0.0034141 * (N of LTCF).
The overall regression was statistically significant (r2 = 0.8373, F (5,13) = 13.38,
p = 0.0001). It was found that the number of hospital beds (×1000 inhabitants) significantly predicted the COVID-19 death rate (per 100,000) (β = 14.83807, 95%CI 5.634418 24.04171,
p = 0.004) (
Table 2).
The Italian regions with a higher number of hospital beds (×1000 inhabitants) showed a higher COVID-19 death rate (
Figure 1A). Similarly, the number of GPs also predicted the COVID-19 death rate (per 100,000) (β = −33.64296, 95%CI −53.6297 −13.6563,
p = 0.003). The Italian regions with a higher number of GPs showed a lower COVID-19 death rate (
Figure 1B).
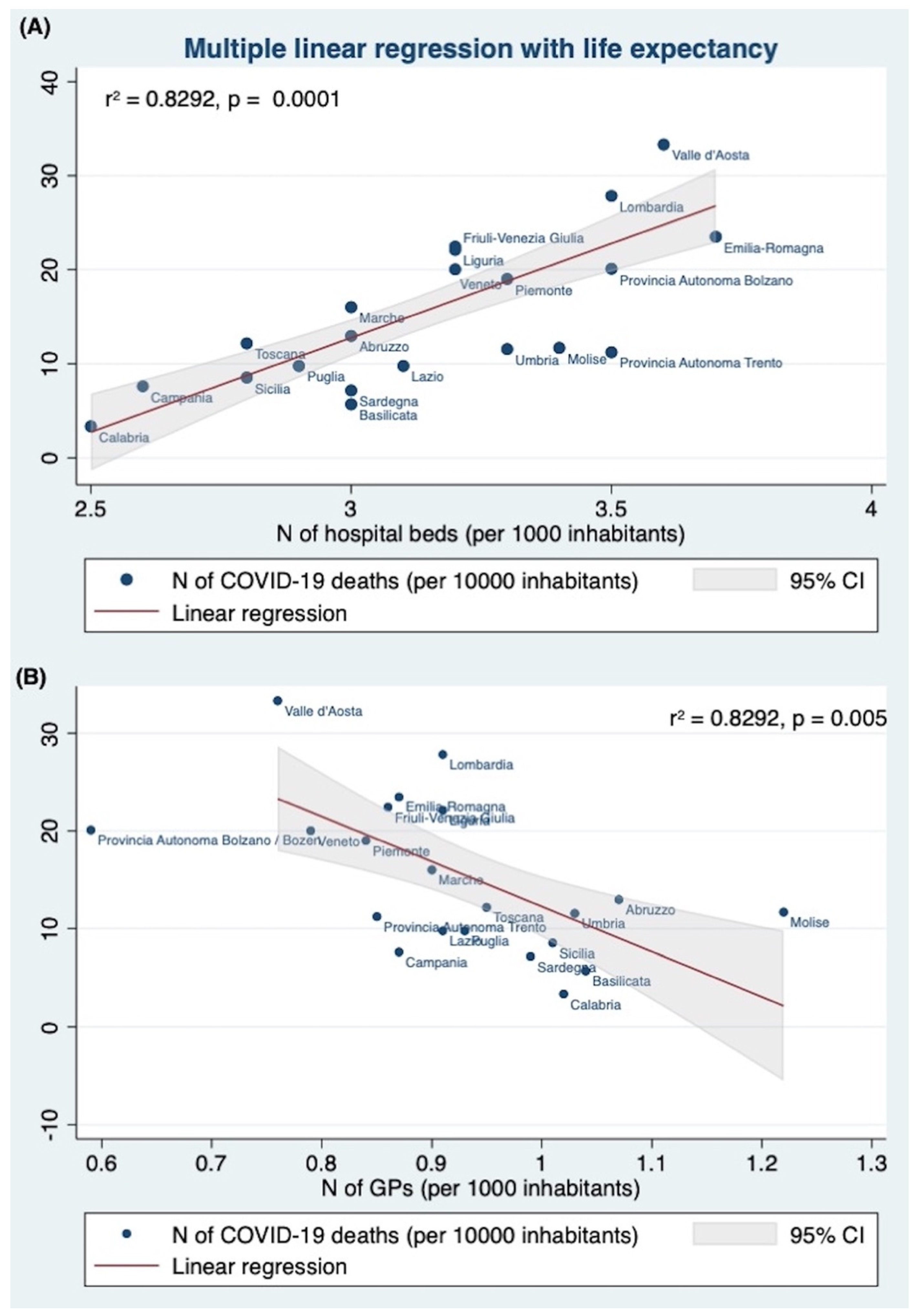
Then, the second multiple linear regression tested if the life expectancy, the number of hospital beds (per 1000), the health expenditure per capita, the GPs per 1000, and the number of LTCF significantly predicted the number of COVID-19 deaths (per 100,000 inhabitants). The fitted regression model was: 94.9212–1.3861 * (life expectancy) + 15.4037 * (N of hospital beds per 1000) + 0.0090 * (health expenditure per capita) − 32.4074 * (N of GPs per 1000) + 0.0049 * (N of LTCF).
The overall regression was statistically significant (r2 = 0.8292, F (5,13) = 12.62,
p < 0.0001). It was found that again the number of hospital beds (×1000 inhabitants) (β = 14.83807, 95%CI 26.0161 24.7913,
p = 0.004), and the number of GPs (β = −32.4074, 95%CI −53.31456 −11.5003,
p = 0.005), significantly predicted the number of COVID-19 deaths (per 100,000 inhabitants) (
Table 2).
The Italian regions with a higher number of hospital beds (×1000 inhabitants,
Figure 2A) and a lower number of GPs (per 1000),
Figure 2B) experienced a higher number of COVID-19 deaths.
Finally, the third multiple linear regression tested if the aging index, the number of hospital beds (per 1000), the health expenditure per capita, the GPs per 1000, and the number of LTCF significantly predicted the number of COVID-19 deaths (per 100,000 inhabitants). The fitted regression model was: −4.7326 + 0.0413 * (aging index) + 15.5586 * (N of hospital beds per 1000) − 0.0022 (health expenditure per capita) − 34.8603 (N of GPs per 1000) + 0.0032 (N of LTCF).
The overall regression was statistically significant (r2 = 0.8292, F (5,13) = 12.62,
p = 0.0001). It was found that the number of hospital beds (×1000 inhabitants) significantly predicted the number of COVID-19 deaths (per 100,000) (β = 15.5587, 95%CI 6.1525 24.9648,
p = 0.003) (
Table 2).
The Italian regions with a higher number of hospital beds (×1000 inhabitants) showed a higher COVID-19 death rate (
Figure 3A). Similarly, the number of GPs also predicted the COVID-19 death rate (per 100,000) (β = −34.86028, 95%CI −55.43874 −14.28183,
p = 0.003). The Italian regions with a higher number of GPs showed a lower COVID-19 death rate (
Figure 3B).
4. Discussion
In March 2020, the COVID-19 outbreak spread across all of Italy. From 1 March 2020 to 1 March 2021, about 3 million positive confirmed cases and over 100,000 deaths were recorded in Italy [
8]. Large differences in COVID-19 mortality have been demonstrated between the 21 Italian regions. Saglietto and collaborators [
9], analyzing the number of deaths related to COVID-19 in relation to the number of tests performed for SARS-CoV-2 among the most affected Italian regions, showed that the Italian regions with the highest number of tests had the lowest rate of mortality per 100,000 population. This evidence suggested that early identification and isolation of active cases (including asymptomatic or mildly symptomatic subjects) could have had an important effect in reducing COVID-19 mortality, by hypothesizing that these differences could explain the wide differences in mortality among the Italian regions [
9]. Moreover, Saglietto et al. [
9] also underlined that different COVID-19 mortality experienced by Italian regions was only partially explained by differences in the population age structure.
Some additional confounding factors, not analyzed in our study, could limit the real impact of these results on the different COVID-19 mortality among the Italian regions. During the first and the second wave of the pandemic, the number of autopsies dramatically declined in Italy due to the concerns about the management of corpses who died by or with COVID-19, as also included in the first recommendations provided by the Italian Health Ministry to pathologists and morgue workers [
10]. The excess of mortality could be higher (maybe triple) than the one reported in the official epidemiological surveys [
11,
12]. Missing autopsies as well as false negative cases of antigenic and molecular tests of first generation may have produced a distorting effect on the assessment of the real mortality rate and the excess mortality [
13].
Analyzing the data recorded by the Italian Health Ministry, we found a strong direct association between COVID-19 deaths and the number of hospital beds (
p = 0.003): the Italian regions with a higher number of hospital beds (x 1000 inhabitants) showed a higher number of deaths, and this evidence was confirmed by all the multiple regression analyses we performed (
Figure 1,
Figure 2 and
Figure 3 panels A,
Table 2).
This finding could be related to the greater severity of the COVID-19 patients, which was not considered in this study because of the lack of information provided from the official report of the Italian Health Ministry, concerning the clinical history of the victims by regional distribution.
However, the absence of a reliable statistical relationship between the aging index, or percentage of over 65 years old subjects (
Figures S1–S3), the most affected by comorbidity, and the deaths support the hypothesis that the different regional mortality rates should be also ascribed to different management choices for the organization and delivery of health services. The coronavirus pandemic exposed the weaknesses and dysfunctionality of our current decentralized healthcare system. According to Armocida et al. [
14], healthcare systems’ capacity and financing need to be more flexible to take into account exceptional emergencies, and stronger national coordination should be in place to provide more sustainable and efficient health services.
Then, our findings suggest that the choice to concentrate the healthcare services in the hospitals should be reconsidered toward a more community-centered approach, as was recently also recommended by the World Health Organization [
15]. In most populated European countries, even if the hospital beds were efficiently managed, the concentration of hospitalized patients and the scarcity of beds have put pressure on the hospital systems [
16]. Considering the use of the hospital resources, Pecoraro et al. [
16] demonstrated that, whereas Germany counts a high availability of hospital beds per 100,000 inhabitants, it is the country with the lowest number of hospitalizations in the general wards (N = 40.8) compared with the other countries (Italy, N = 91.1; France, N = 105.4; and Spain, N = 220.7). The authors underlined how this finding was associated with lower mortality in Germany (where the number of deaths per 100.000 inhabitants was 10.9 in contrast to the data reported in France (N = 30.0), Italy (N = 57.8), and Spain (N = 60.4) [
16].
In our study, the need for a more community-centered approach seems to be also supported by the strong association (confirmed by the multivariate linear regression analyses) between COVID-19 deaths (×10,000 inhabitants) and the number of GPs (per 10,000 inhabitants) per Italian region. In all models: the Italian regions with a higher number of GPs showed a lower number of COVID-19 deaths (
Figure 1,
Figure 2 and
Figure 3 panels B,
Table 2).
Recently, the great interest in this topic was also shown by the discussion on the national and regional government decisions taken to counteract COVID-19 dissemination [
13]. Italy has mistreated its primary healthcare system in the last decades with an availability of 89 GPs per 100,000 inhabitants, compared to 167. in Germany, and 155.5 in France [
17,
18].
According to Plagg et al. [
18], increasing the number of available hospital beds without appropriate staff and reinforcement of the primary care services cannot be considered the answer, as represented by increased mortality.
As reported in a letter in the Lancet Journal [
19], the contribution to documenting and analyzing the social and political effects of epidemiological events has been crucial for other infectious diseases. Sams et al. [
19] underlined that, as in the occasion of other epidemics (e.g., Ebola virus disease and AIDS), networks have become central to addressing issues such as vaccine hesitancy, misinformation, and trust; all problems also experienced in the Italian pandemic [
20].
Limitations and Strengths
The present study suffers some limitations. Firstly, because of the retrospective design, the analyzed data did not permit the definition of the COVID-19 severity, and the impact of other factors on the total mortality rate. In particular, the impact of hospitalization on mortality, and the viral characteristics, such as the SARS-CoV-2 viral load and replication rate, could represent other possible confounders.
However, the used data represent the official ones provided by the Italian Health Ministry, and, to our knowledge, this represents the first study that analyzes the relationship between the number of GPs and COVID-19 mortality rate, accordingly also to the hospital bed number.
5. Conclusions
This study analyzes, for the first time, the relationship between COVID-19 mortality rates, the number of hospital beds, the number of GPs, and, therefore, the regional healthcare system organization. In the future, a more flexible hospital system cooperating with primary medical care might show better efficiency in containing viral spread and managing patients. Noteworthily, the hospitals still represent the most reliable resource of healthcare assistance in Italy, and our findings do not advise against hospitalization but encourage better management and optimization of healthcare sources.
Moreover, a better understanding of the social and political factors affecting the outcomes of pandemic emergencies should represent a priority, also for the increasing number of elderly, and a rise in healthcare requests. Surely further studies are needed to better clarify these aspects, also considering the different distribution of healthcare sources by country.