Abstract
Post-concussion symptoms often occur after TBI, persist and cause disabilities. The Rivermead Post-Concussion Symptoms Questionnaire (RPQ) is widely used in this population, but little is known about the comparability of the symptoms over time, i.e., longitudinal measurement invariance (MI). The objectives of this study were to analyze the longitudinal MI of RPQ symptoms from three to twelve months after TBI and to find factors related to RPQ symptoms. The study involved 1023 individuals after TBI who took part in the Collaborative European NeuroTrauma Effectiveness Research in TBI (CENTER-TBI) study and completed the RPQ at three, six and twelve months post-injury. Longitudinal confirmatory factor analysis showed that the three-factor structure (somatic, emotional and cognitive) remains stable within one year after TBI. Linear mixed models revealed that sex, injury cause and prior psychiatric problems were related to the RPQ three-factor structure as well as to the RPQ total score. The study strengthens evidence for the RPQ’s factorial structure stability within one year after TBI and identifies sex, injury cause and prior psychiatric problems as important factors that may help clinicians to prevent future complications of symptomatology after TBI.
1. Introduction
Traumatic brain injury (TBI) is one of the main causes of disability and death in young people and adults between the ages of 18 and 35, affecting 69 million people each year worldwide [1]. In Europe, the incidence of TBI varies by country, from 47.3 per 100,000 population per year (Spain) to 694 per 100,000 population per year (Republic of San Marino) [2]. Advancements in emergency and intensive care services in recent decades have increased survival. Evaluation and diagnostic protocols identifying problems shortly after a TBI can facilitate timely intervention to prevent future complications or sequelae.
TBI can cause physical, cognitive and emotional consequences in the short and the long term. Physical problems usually include headaches [3,4,5,6,7,8], nausea [9,10,11,12,13], dizziness [3,4,5,14,15,16], sensitivity to light or noise [9,12,15,17], blurred or double vision [3,5,11,15,18,19,20] and fatigue [4,8,15,16,21,22,23,24,25]. Cognitive alterations include problems in processing speed, attention and concentration [9,13,15,24,26,27,28,29,30]; executive functions [20,28,31,32,33,34]; learning and memory [13,17,20,26,34,35,36,37]; and language [26]. Individuals after TBI usually report symptoms of depression [5,15,19,28,30,38,39,40,41,42,43,44,45,46], suicidal ideation [47,48,49], anxiety [15,30,38,42,43,45,46] and post-traumatic stress [50]. Furthermore, emotional lability and apathy have been noted [5,25,30,51,52]. Regarding the behavioral consequences of TBI, individuals also experience irritability [4,28,38,45,53,54,55], aggressiveness [55], and, in some cases, personality changes [25,56,57], restlessness [3,11,45,58] and insomnia [16,23,28,59,60,61].
These symptoms are referred as to post-concussion symptoms. They often occur after mild to moderate TBI [62]. However, individuals after severe TBI also suffer from comparable deficits [45]. These TBI-related complaints usually resolve within a period of three months [63]. Nevertheless, some deficits may persist for up to one year after injury [64]. If not treated in time, they could last longer than expected and negatively impact other areas of the patient’s life to the point of causing disability [65,66]. For example, individuals after TBI are known to have a poorer quality of life compared to people without TBI [15,67,68,69]. Furthermore, even though most individuals after mild TBI return to work [70], there is evidence that those with more severe injuries have difficulties or worse job performance [71,72]. In addition, some individuals after TBI report difficulties in returning to their daily routine [73,74] and even driving, with less anticipation of accidents compared to healthy people [75,76].
Several factors have been repeatedly found to be associated with short- and long-term prognoses of these symptoms after TBI. Some of the most important sociodemographic characteristics include age [4,5,9,16,20,24,25,29,44,45,77,78,79,80,81,82,83], gender/sex [4,5,9,16,17,19,20,24,25,29,37,44,81,82,84,85,86], living situation [15,24], employment status [5,24,80,82], marital status [5,16,19,82,86], education [9,11,20,24,28,70,82,84], ethnicity/race [9,16,19,28,30,37,80,82,87,88] and socioeconomic class [25,80]. Clinical factors including motor response [78,79,80,89], comorbidity [80,84,90], loss of consciousness (LOC) [4,15,81,91], a number of previous concussions [5,25,81,82,84], amnesia [25,28,29,81], total score on the initial Post-Concussion Scale [81,82], psychiatric history [4,5,11,25,44,70,83], alcohol abuse [16,44,82,92], illicit drug abuse [44,82,93,94], attention deficit hyperactivity disorder [25,37], TBI severity [24,34,77,82,83,95,96], depressive disorder [8,19,25,28], anxiety disorder [25,97], stress disorder [8,13,17] and the mechanism of injury [4,16,29,82,84,90,98] have been shown to be associated with symptom burden after TBI.
Post-concussion symptoms may vary depending on the time after injury and the instruments used to measure predictors and outcomes. Research has typically evaluated individuals after TBI at one time point, for instance, at one month [4,16,25,29,30,82,99], between two and six months [25,84], at six months [11,13,20,30,96] and at one year [5,30,80,99]. Furthermore, longitudinal assessments of symptoms and predictors following TBI often use unsystematic time points within a few weeks after TBI [37]. Studies use different instruments such as the Rivermead Post-Concussion Symptoms Questionnaire (RPQ) [4,15,16,22,24,29,30,39,45,80,99], Neurobehavioral Symptom Inventory (NSI) [19,20,28,82,96], Beck Depression Inventory (BDI II/BDI-III) [19,49,99], Alcohol Use Disorders Identification Test (AUDIT) [44,99] and neuropsychological batteries/tests, such as the WAIS-III (Wechsler Adult Intelligence Scale [26,34,35,36,44], Trail Making Test part A and B (TMT-A, B) [9,26,35,36], Colour-Word Interference Test [26,34,35,36], Conners’ Continuous Performance Test [35,36], Delis Kaplan Executive Function System [34,35,36] and California Verbal Learning Test–II [34,35,36], among others.
Among these instruments, the RPQ is commonly used in patients after TBI, as suggested by the Common Data Elements (CDA) recommendations [100,101] to monitor post-TBI symptoms in research and clinical practice [62]. The RPQ has been originally declared as a unidimensional measure [62] consisting of 16 symptoms rated on a five-point Likert scale (from 0 = “not experienced at all” to 4 = “a severe problem”). However, the questionnaire has been subjected to further analyses indicating the multidimensionality of the construct [102,103,104,105,106]. In a recent cross-sectional study on the comparability of the RPQ across six languages and TBI severity groups using six-month CENTER-TBI data [107], the authors found that the factorial structure of the RPQ structure proposed by Smith-Seemiller et al. [102] outperformed competing factorial solutions (i.e., [62,104,106,108]) with respect to data fit. This solution includes three factors (somatic, emotional and cognitive) that can provide additional information on impairment in individual domains. However, despite the researchers agreeing that the RPQ is a non-unidimensional measure, no consensus has been achieved on which factorial solution should be applied for the scoring.
Unfortunately, there is—to our knowledge—relatively little evidence on how RPQ scores change over predefined times after a TBI. For the clinical administration of the RPQ over time and the follow-up assessment of post-concussion symptoms, it is necessary to provide empirical evidence on whether the questionnaire retains its factorial structure over time. Whenever variables are assessed at different time points, it is assumed that changes in the variables are solely attributable to the changes in time. To verify whether this assumption holds true, it is important to ascertain measurement invariance (MI) across time, which indicates that the same construct is measured at different time points [109]. On the other hand, different constructs may be unintentionally assessed at different time points, leading to biased results and subsequent errors in diagnosis and treatment selection.
Recently, Agtarap et al. [110] explored the RPQ’s MI longitudinally in the USA using a mild TBI sample. The authors found a general model comprising 16 items and 3 factors: emotional (irritable, depressed or frustrated), cognitive (forgetfulness, concentration or a longer time to think) and vison (blurred vision, light sensitive or double vision). This four-factor model provided excellent fit to their data and explicitly challenged the often-applied unidimensional structure of the RPQ. Nevertheless, no European studies on the longitudinal assessment of RPQ symptoms has been carried out so far. Since health care systems differ in Europe and the USA (i.e., most European countries have a free social security system, whereas the USA does not), the results of TBI studies conducted in the USA cannot be generalized to Europe.
To uncover the predictors, mechanisms and sequelae of TBI, a multi-site longitudinal cohort study called Collaborative European NeuroTrauma Effectiveness Research in TBI (CENTER-TBI; clinicaltrials.gov NCT0221022) collected data from patients after TBI in Europe and Israel. Among others, self-reported TBI symptoms were assessed at different time points following the TBI using the RPQ.
Given the lack of empirical evidence on the longitudinal applications of the RPQ and the influence of sociodemographic, premorbid and injury-related factors on the (post-concussion) symptoms across time, in the present study, we aim to:
- Analyze the longitudinal measurement invariance of RPQ symptoms from three to twelve months after TBI to verify that the RPQ measures the same construct at different time points following TBI.
- Explore associations among sociodemographic, premorbid and injury-related factors and RPQ symptoms across time to model symptom trajectories for different subgroups of TBI patients.
2. Materials and Methods
2.1. Participants and Recruiting Procedure
The data were collected within the CENTER-TBI study at 63 centers across 18 countries in Europe and Israel from 19 December 2014 to 17 December 2017. Participants were included in the study whenever they received a clinical diagnosis of TBI, presented themselves within 24 h after injury and had for a positive computed tomography (CT) scan. Individuals were differentiated into three strata based on the admission type: emergency room (ER; evaluation at an ER only), admission (ADM; admission to a hospital ward), and intensive care unit (ICU; admission to an ICU). Ethical approval was obtained for each participating site (https://www.center-tbi.eu/project/ethical-approval, accessed on 12 July 2021), and informed consent was obtained from all participants or their legally authorized representatives. Further details can be found elsewhere [111].
Data were retrieved from the CENTER-TBI database using the data access tool NEUROBOT, and the 3.0 core sample comprised 4509 participants. For the present study, we focused on individuals who had completed the RPQ assessments at three, six and twelve months after TBI. Due to the study design, individuals seen in the ER and then discharged were not involved in the twelve-month assessments. The present study included participants aged 16 and above, limited to those who filled out the RPQ at all three time points, yielding a final sample of 1023 participants. For more details, see Figure 1.
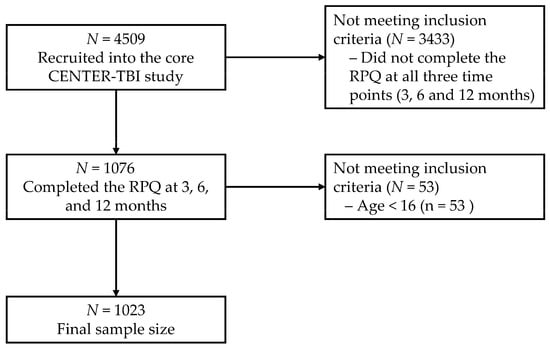
Figure 1.
Sample flow chart diagram.
2.2. Measures
Sociodemographic and premorbid health history was collected upon enrollment in the study. Participants provided sociodemographic characteristics, such as sex, age, education level, marital and employment status as well as premorbid health history, such as previous concussions or TBIs and psychiatric problems prior to the TBI.
Injury-related factors covered TBI and trauma severity. The severity of TBI was rated on the Glasgow Coma Scale (GCS) [112] in combination with the presence of CT abnormalities on the first CT scan (uncomplicated mild, GCS 13 and no CT abnormalities; complicated mild, GCS 13 and CT abnormalities present; moderate, GCS = 9–12; and severe TBI, GCS 8). The GCS was determined within the first 24 h post-injury. With the Injury Severity Score (ISS), trauma severity and polytrauma were evaluated by calculating the sum of the squares of the highest values of the three body regions measured by the Abbreviated Injury Scale score (AIS) [113].
The RPQ was used to assess 16 self-reported post-concussion symptoms (headaches, dizziness, nausea and/or vomiting, noise sensitivity, sleep disturbance, fatigue, irritability, depression, frustration, forgetfulness and poor memory, poor concentration, slow thinking, blurred vision, light sensitivity, double vision and restlessness). The RPQ total score ranges from 0 to 64 with cut-offs of 13, 25 and 33, indicating mild, moderate and severe symptoms, respectively [108].
2.3. Statistical Analyses
2.3.1. Descriptive Analyses
The mean (M), median (Mdn), standard deviation (SD), skewness (SK; values |>3.0| indicate a severely skewed distribution) and kurtosis (K; values |>10.0| suggest significant deviation from a normal distribution [114]) were calculated for each RPQ symptom at three time points. The proportions of participants that reported “not experienced at all”, “no more of a problem (than before)”, “a mild problem”, “a moderate problem” and “a severe problem” were obtained for each symptom and time point.
2.3.2. RPQ Longitudinal Measurement Invariance
A longitudinal measurement invariance (MI) approach was chosen to assess differences in reported RPQ symptoms across time points. Based on the previous findings [107], we used the three-factor model comprising somatic, emotional and cognitive domains. To assess MI across three, six and twelve months, longitudinal confirmatory factor analysis (CFA) models were run for ordered categorical data [109]. For this purpose, three models with consecutive restrictions were estimated: (1) a baseline model/configural model, (2) a loading invariance model and (3) a threshold invariance model.
First, the configural model assumes that the same general pattern of factor loadings holds across time and assumes the following constraints:
- Latent intercepts are fixed to zero.
- The common factor mean is constrained to zero, and the unique factor covariance matrix is constrained to be 1.00.
- The same observed measure is chosen as the marker variable, and the factor loading of the marker variable is constrained to be 1.00.
- A threshold for each indicator is constrained to be equal across time.
Second, the loading invariance model adds to the configural model the constraint that factor loadings are identical across time. Third and finally, the threshold invariance model incorporates the constraint for each indicator, assuming that the threshold level of going from one response category to the next is identical across time. Loading and threshold invariance models were compared to baseline models using the following fit indices: the Comparative Fit Index (CFI) and the Tucker Lewis Index (TLI), where values above 0.95 establish adequate fit; the root-mean-square error of approximation (RMSEA; with a 90% confidence interval; CI90%) and the standardized root-mean-square residual (SRMR), where values < 0.06 to 0.08 establish adequate model fit [115]; and chi-squared difference statistics . The type of estimator that was used was the diagonally weighted least square (DWLS) as an estimator commonly used with latent variable models with ordered categorical variables. This procedure was applied to each RPQ factor (somatic, emotional and cognitive), respectively.
2.3.3. Demographic and Injury Characteristics Effects
To investigate the effects of demographic and injury characteristics, we estimated linear mixed models (LMMs) for each factor (somatic, emotional and cognitive) score and the conventional total RPQ score. We considered the following set of predictors:
- Time since TBI (three, six and twelve months);
- Sociodemographic factors: sex (female vs. male), age in years, education in years and interaction between sex and age;
- Injury-related factors: TBI severity (uncomplicated mild TBI vs. more severe TBIs), injury cause (road traffic accident vs. fall vs. violent/other), admission type (ADM vs. ICU) and ISS [converted into log ISS distribution];
- Premorbid factors: previous concussions (yes vs. no) and prior psychiatric problems (yes vs. no).
Three RPQ scale scores and the RPQ total score were used as dependent variables. Additionally, quadratic and cubic functions were evaluated for the time since TBI variable as well as for injury severity as measured by the ISS, and participants were included as random effects. For all significant predictors in LMMs, Type I error probability was set to 0.05 (one-tailed for testing directed hypotheses). To estimate the parameter values for LMMs, bootstrap estimation was used. All analyses were performed using R 4.0.5 [116]. The lme4 package [117] was used for LMMs, and the lavaan package [118] was used for longitudinal CFA.
3. Results
Most participants were male (67.4%), with a mean age of 49.6 years (SD = 19.1; Mdn = 52.0; range 16 to 95). On average, they had 14.0 (SD = 4.1) years of education, and the majority were partnered (54.8%). Regarding injury characteristics, 45.0% of participants sustained complicated mild TBI, 50.8% were admitted to the ICU and the mean ISS was 22.1 (SD = 14.4). The demographic and injury characteristics of the participants are shown in Table 1.

Table 1.
Demographic characteristics of the sample.
Excluded participants (i.e., individuals younger than 16 years of age who did not complete the RPQ at all time points) did not differ systematically from participants included in analyses regarding sex (X2[1] = 2.79; p = 0.094), education level (X2[2] = 0.55; p = 0.757), age (t [2228] = −1.45; p = 0.145) or previous concussions (X2[1] = 0.17, p = 0.675). However, they differed with respect to extracranial injury severity level, according to ISS, (X2[3] = 32.36, p < 0.001), injury cause (X2[2] = 17.08, p < 0.001) and prior psychiatric problems (X2[1] = 6.26, p = 0.012). The excluded individuals more often had sustained mild injuries, were injured in road traffic accidents and had prior psychiatric problems.
3.1. Descriptive Analyses
Regarding descriptive information on individual symptoms assessed three months after TBI, arithmetic means across participants ranged from 0.27 (nausea) to 1.65 (fatigue) with asymmetry (SK) of 0.13 (fatigue) to 2.97 (nausea and double vision). The same pattern was found at six and twelve months. Nausea had the lowest average values (0.20 and 0.23 at six and twelve months, respectively), and fatigue the highest (1.49 and 1.42 at six and twelve months, respectively) (see Appendix A, Table A1).
An analysis of the proportions of each response category that was utilized indicated that the “not experienced at all” option was reported most often across all time points. The symptoms with the highest proportion in the category “mild problem” were fatigue (27% at three months and 24% at both six and twelve months), forgetfulness (21% at three months, 25% at six months and 22% at twelve months), poor concentration (21% at all three time points) and taking longer to think (20% at three months, 21% at six months and 20% at twelve months). Fatigue was the symptom with the highest proportion (8% in three months and 7% in six and twelve months) in the “severe problem” level (see Table 2).

Table 2.
Proportions for each level of response by time point (3, 6 and 12 months).
3.2. Longitudinal RPQ Measurement Invariance
The results from the MI testing for the three RPQ factors are presented in Table 3. The baseline model fit was adequate for the somatic factor (CFI = 0.942, TLI = 0.933, RMSEA = 0.059, CI90% [0.056, 0.063]), indicating that the somatic-factorial structure represented the data well across all time points. There were no significant differences (p = 0.385) between the loading (CFI = 0.944, TLI = 0.938, RMSEA = 0.057 [0.054, 0.060]) and baseline model fit; therefore, intercepts were invariant across time. However, significant differences were found between the loading and threshold model fit (p < 0.001), indicating that the number of participants who reported each severity level can change over time. For example, the number of individuals who reported not experiencing fatigue at three months was 290, but this number increased to 345 at six months and to 372 at twelve months post-injury. However, from the initial 273 people who reported mild fatigue levels at three months, the number decreased to 242 people at six and twelve months, respectively (see the proportions for each level of response by time point in Table 2).

Table 3.
Results from the longitudinal measurement invariance tests for the factors using the DWLS.
Regarding the emotional factor, CFI = 0.999, TLI = 0.998, and RMSEA 0.022, CI90% [0.009, 0.033] parameters showed adequate baseline model fit. In addition, no significant differences (p = 0.057) were found between the loading (CFI = 0.998, TLI = 0.998, RMSEA = 0.025 [0.014, 0.034]) and baseline model fit. However, significant differences (p < 0.001) were identified between the loading and threshold model fit (CFI = 0.977, TLI = 0.981, RMSEA = 0.070, CI90% [0.064, 0.077]). Despite the differences, the threshold model showed adequate fit, which was slightly worse compared to the loading model fit.
Finally, for the cognitive factor, the same pattern was observed as for the previous factors. The baseline model fit was adequate across time (CFI = 1.000, TLI = 1.000, RMSEA < 0.001, CI90% [0.000, 0.018]), and there were no significant differences between the loading and the baseline model fit (p = 0.376). Here, again, significant differences were found between the loading and threshold model fit (p < 0.001).
Table A2 in Appendix A shows the discrepancies in the predicted probabilities between the threshold and loading invariance in each model. For example, for the somatic factor, symptom fatigue had the largest discrepancies in the predicted probabilities between the retained loading invariance model and the rejected threshold invariance model at three months after TBI [“No more of a problem (than before)” and “A mild problem”] and the symptom sleep disturbance at six months (“A moderate problem” and “A severe problem”).
3.3. Demographic and Injury Predictors of Factor Scores across 3, 6 and 12 Months
The estimated models for each factor score can be found in Table 4. A significant effect of time since TBI (b = −0.79, SE = 0.17, p < 0.001) was found for the somatic factor, indicating that somatic symptom severity levels decreased linearly across time. Furthermore, sex (b = −2.55, SE = 1.10, p = 0.025), admission type (b = 1.62, SE = 0.55, p = 0.003), injury cause (b = −1.04, SE = 0.40, p = 0.014) and prior psychiatric problems (b = 2.90, SE = 0.61, p < 0.001) effects were found. Females, patients admitted to ICU, those who sustained a TBI by a road traffic accident or violence/other causes and individuals with prior psychiatric problems presented higher somatic symptom severity compared to males, patients admitted to hospital ward, those with falls as the injury cause and individuals who reported no prior psychiatric problems (see Figure 2). Similar results were found for the emotional factor (see Table 4 and Figure 3).

Table 4.
Demographic and injury predictors of factor score trajectories across 3, 6 and 12 months.
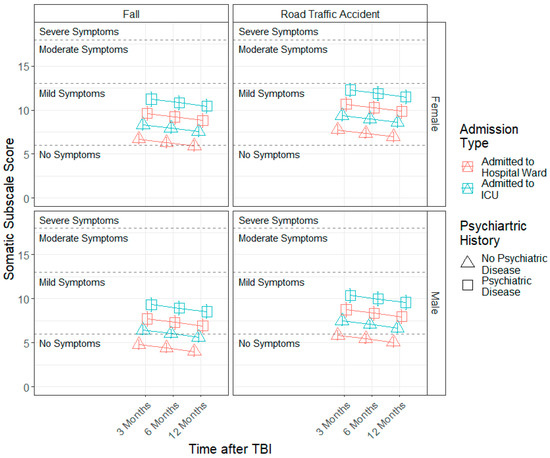
Figure 2.
Modelled trajectories for the somatic factor by significant predictors.
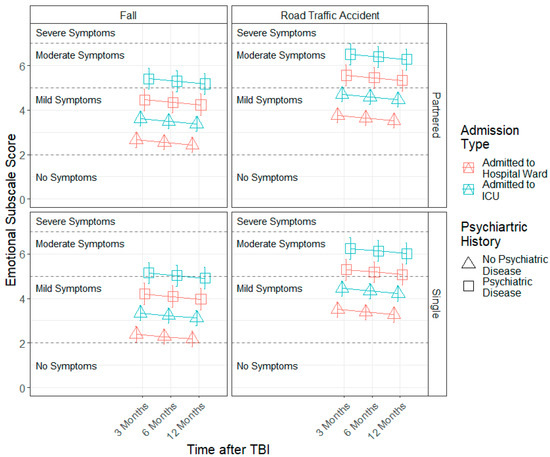
Figure 3.
Modelled trajectories for the emotional factor by significant predictors.
Regarding the cognitive factor, a significant quadratic time effect (b = 0.21, SE = 0.09, p = 0.037) was found, indicating that cognitive symptom severity levels decrease from 3 to 6 months, with an increase in severity from 6 to 12 months. Moreover, admission type (b = 0.69, SE = 0.31, p = 0.022), injury cause (b = −0.74, SE = 0.22, p = 0.001), prior concussions (b = 0.87, SE = 0.32, p = 0.010) and prior psychiatric problems (b = 1.56, SE = 0.34, p < 0.001) effects were found. Individuals who were admitted to the ICU, those who sustained a TBI as a result of a road accident and due to violence/other causes and patients with prior concussions and prior psychiatric problems presented higher cognitive symptom severity compared to patients admitted to a hospital ward, those with falls as the injury cause and patients without prior concussions and without prior psychiatric problems (see Figure 4).
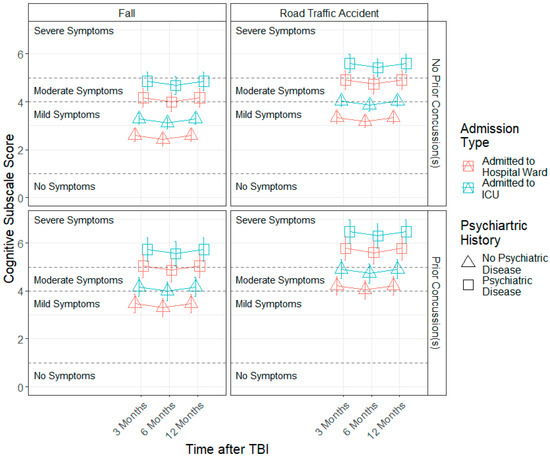
Figure 4.
Modelled trajectories for the cognitive factor by significant predictors.
Finally, a significant effect of time since TBI (b = −1.03, SE = 0.31, p = 0.001) was determined with respect to the RPQ total score, showing that symptom severity levels decrease linearly from 3 to 12 months. Moreover, sex (b = −4.60, SE = 2.20, p = 0.038), admission type (b = 3.50, SE = 1.07, p = 0.001), injury cause (b = −3.07, SE = 0.85, p < 0.001), prior concussions (b = 2.42, SE = 1.23, p = 0.049) and psychiatric problems (b = 6.02, SE = 1.25, p < 0.001) effects were found. Females, patients who were admitted to the ICU, those who sustained a TBI caused by road traffic accidents or violence/other causes, patients with prior concussions and patients with prior psychiatric problems presented higher RPQ symptom severity compared to males, patients admitted to a hospital ward, those with falls as the injury cause, patients without a prior concussion and patients without prior psychiatric problems (see Figure 5).
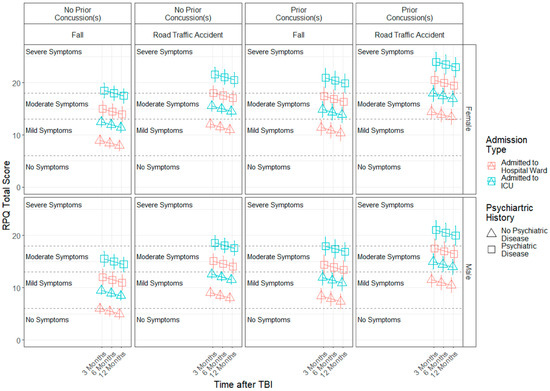
Figure 5.
Modelled trajectories for the RPQ total score by significant predictors.
4. Discussion
Given the lack of empirical evidence regarding the administration of the RPQ across time, the present study aimed to analyze patient-reported post-concussion symptoms longitudinally (three, six and twelve months). We investigated the measurement invariance assumption for the RPQ and associations between sociodemographic, premorbid and injury-related factors and RPQ symptoms within the first years after TBI using data obtained from the CENTER-TBI study.
The results showed that the basic structure of the three factors remained stable across time (i.e., was invariant). In addition, factor loading changed longitudinally, and the proportion of symptoms reduced across time, with fatigue, poor concentration and taking longer to think being the most prevalent symptoms. Furthermore, we found that sex, injury cause and prior psychiatric problems were related to the somatic, emotional and cognitive domains as well as to the RPQ total score.
Multiple scales have been used to assess post-TBI symptoms in research and clinical practice, with the RPQ being commonly applied in patients after TBI [62]. Despite its widespread use, very few studies have examined the RPQ longitudinally and using MI. Agtarap et al. [110] explored RPQ’s MI longitudinally in a mild TBI sample and found that a four-factor model provided the best model fit to their data. In our study, however, we employed the structural-factorial model defined by Smith-Seemiller et al. [102] based on theoretical considerations and the confirmation of its factorial structure in other studies using TBI sample (i.e., [62,104,106,108]). According to the MI philosophy, the structure of latent factors, which in this case is post-concussion symptomatology, should be stable or invariant, and the association between items and latent factors should not depend on group membership (e.g., a certain patient’s characteristics) or time [119]. Our results showed that post-concussion symptoms are clearly clustered in somatic, emotional and cognitive domains. Moreover, this structure was stable across the first year after TBI, regardless of its severity. Thus, even though a patient’s symptomatology changes across time, with increases or decreases in the number of symptoms and/or their intensity, clinicians and researchers can be sure that the RPQ retains its capacity to capture somatic, emotional and cognitive symptoms.
Regarding long-term symptom trajectories, the number and intensity of these symptoms tended to decline across time, although the few patients who reported severe problems concerning some symptoms at three months maintained the intensity of the problems at six and twelve months. These remaining long-term symptoms (e.g., fatigue and poor concentration) may be due to the difficulty that clinicians have with identifying and treating them, as there is a lack of scientifically proven standard protocols or strategies, [120] and it depends on the interaction of multiple factors (e.g., TBI severity, range of sequelae, patients’ coping strategies, etc.). Nevertheless, despite these change patterns in symptomatology (e.g., fatigue, sleep disturbance, forgetfulness, poor concentration and taking longer to think), the three-factor model fit was similar across time; therefore, RPQ can be considered a valid instrument to measure post-TBI symptomatology in individuals after TBI, with a broad severity range.
Poor concentration and taking longer to think were the most prevalent symptoms among mild TBI patients across time, and fatigue was presented as the most prevalent in individuals with all severities (mild, moderate, and severe) for all time points. These results are consistent with several studies that have shown fatigue [3,11,15,24,45], poor concentration [11,15,24,29] and lower processing speed [3,11] as TBI residual symptoms. It is a shortcoming of the present study that ER patients (whose majority had mTBI) were excluded from the analysis due to the lack of complete data across time based on the study design (i.e., no assessments at 12 months after TBI). Including ER patients would have helped to interpret the relation between specific symptoms and TBI severity, as patients in ER strata were often found to report fewer post-concussion symptoms with lower intensity compared to those who were admitted to the hospital ward or the ICU [24].
Females, patients who were admitted to the ICU, those who sustained a TBI caused by a road traffic accident or violence/other causes, patients with prior concussions and patients with prior psychiatric problems presented higher RPQ symptom severity compared to males, patients admitted to the hospital ward, those with falls as the injury cause, patients without prior concussions and patients without prior psychiatric problems. It is, however, hard to judge the findings on factors associated with somatic, emotional and cognitive symptoms over the course of one year because of the cross-sectional nature and variety of applied measures in previous work. Most studies found that age [24,45,80,121,122], sex [24,45,81,121,122], education [11,24,45,122,123], employment status [24,80,122], TBI severity [24] and premorbid problems [15,24,80,123] are associated with RPQ symptomology, and thus, the present study would provide an extension of findings regarding these predictors over the course of one year.
In the only longitudinal study, besides the present one, the authors found that time, sex, preinjury psychiatric disorders and race were related with RPQ measured symptomatology [110]. These results are partially consistent with our results because there was a linear decrease in the mean scores in the somatic and emotional symptoms and in the total score. However, the mean scores of the cognitive symptoms (forgetfulness, poor concentration and taking longer to think) increased slightly from 6 to 12 months, unlike the results found by Agtarap et al. [110]. This increase in cognitive symptoms may be because patients who incorporate activities into their daily life one year after injury realize their cognitive limitations and the challenges that they must face. Apart from the differing results concerning cognitive symptoms, we found that female patients and patients with prior psychiatric disorders reported higher symptom scores, which is in line with the findings of Agtarap et al. [110]. To further validate our results from the current study, the data from the TRACK-TBI study could be used. Such analyses, wherein we could also control for geographic regions, would shed more light on the longitudinal prevalence of symptoms after TBI and on potential protective and risk factors.
4.1. Limitations
We included as associated variables age, sex, etc., which are non-modifiable factors. Future studies should include modifiable predictors (e.g., the type of rehabilitation received, the number of rehabilitation hours received, and social support). Even though all patients were from Europe or Israel, the health care system varies across these countries and may impact these outcomes, so future studies should consider including country as a predictor, if the numbers of participants are high enough. Furthermore, the distribution of regions was unequal, with Eastern Europe being the most underrepresented and thus contributing minimally to the study results. Additionally, as individuals admitted to the ER were discharged before the twelve-month assessments, they were excluded from the analyses. Future studies should include information of this type of patient to verify the invariant structure of the latent factors of RPQ. Finally, we did not have information on whether patients had suffered a further TBI during the period of follow-up, which may have influenced the number of symptoms reported.
4.2. Implications
First, our results indicate that the questionnaire retains its factorial structure over time and thus can be implemented into longitudinal evaluations, follow up assessments and diagnostic protocols to identify and associate RPQ symptoms during the first year post-injury in a variety of individuals with different ranges of TBI severity. Second, clinicians should pay attention to potential at-risk groups. Females, patients admitted to the ICU, those who sustained a TBI due to a road traffic accident and violence/other causes and individuals with prior psychiatric problems appear to be more likely to report persistent symptoms (post-concussion) and should be diagnosed and treated appropriately in a timely manner. Overall, the early identification of these symptoms and their associated variables may help to implement early, customizable interventions to prevent future complications, sequalae or the chronification of symptoms.
The results of our study provide evidence that the RPQ retains its factorial structure over a period of one year. This conclusion is supported by a good fitting three-factor model in both cross-sectional [107] and longitudinal studies; therefore, researchers and clinicians can use robust symptom factors in their clinical work or research studies.
5. Conclusions
The aim of this study was to analyze the RPQ’s measurement invariance within the first year after TBI and associated variables related to RPQ symptoms. The results showed that the three-factor structure comprising somatic, emotional and cognitive domains remains stable across time and that the proportion of symptoms reduced during the first year after injury, but fatigue, poor concentration and taking longer to think persisted as the most prevalent symptoms. Therefore, it is of utmost importance to ensure the adequate diagnosis and treatment of persistent symptoms to facilitate the return to daily life for those affected. Moreover, certain subgroups of patients who are at higher risk of experiencing symptoms over time should be treated in a timely and appropriate manner. Thus, researchers and clinicians now have evidence that the RPQ retains its factorial structure over a period of one year, allowing the identification of symptoms and their severity range during that period. Furthermore, the identification of associated factors may help to prevent future complications of the symptomatology after TBI.
Supplementary Materials
The following supporting information can be downloaded at: www.mdpi.com/article/10.3390/jcm11144090/s1. The full list of the CENTER-TBI participants and investigators can be found in the Online Supplement.
Author Contributions
Conceptualization, M.Z., N.v.S. and J.C.A.-L.; methodology, D.R., S.G., M.Z. and N.v.S.; software, D.R., S.G. and M.Z.; formal analysis, D.R., S.G. and M.Z.; data curation, S.G. and M.Z.; writing—original draft preparation, D.R., J.C.A.-L. and M.Z.; writing—review and editing, D.R., J.C.A.-L., M.Z., S.G. and N.v.S.; visualization, D.R.; supervision, M.Z. and N.v.S.; funding acquisition, N.v.S. All authors have read and agreed to the published version of the manuscript.
Funding
CENTER-TBI was supported by the European Union 7th Framework program (EC grant 602150). Additional funding was obtained from the Hannelore Kohl Stiftung (Germany), from OneMind (USA) and from Integra LifeSciences Corporation (USA). The funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report.
Institutional Review Board Statement
The CENTER-TBI study (EC grant 602150) was conducted in accordance with all relevant laws of the European Union (EU) if directly applicable or of direct effect and all relevant laws of the country where the recruiting sites were located. Informed consent by the patients and/or the legal representative/next of kin was obtained, according to the local legislations, for all patients recruited in the Core Dataset of CENTER-TBI and documented in the electronic case report form (e-CRF). For the full list of sites, ethical committees and ethical approval details, see the official CENTER-TBI website (https://www.center-tbi.eu/project/ethical-approval, accessed on 4 November 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All relevant data are available upon request from CENTER-TBI, and the authors are not legally allowed to share it publicly. The authors confirm that they received no special access privileges to the data. CENTER-TBI is committed to data sharing and, in particular, to responsible further use of the data. Hereto, we have a data sharing statement in place: https://www.center-tbi.eu/data/sharing (accessed on 11 July 2022). The CENTER-TBI Management Committee, in collaboration with the General Assembly, established the Data Sharing Policy and the Publication and Authorship Guidelines to assure the correct and appropriate use of the data, as the dataset is hugely complex and requires the help of experts from the Data Curation Team or Bio- Statistical Team for correct use. This means that we encourage researchers to contact the CENTER-TBI team for any research plans and the Data Curation Team for any help in the appropriate use of the data, including the sharing of scripts. Requests for data access can be submitted online: https://www.center-tbi.eu/data (accessed on 11 July 2022). The complete manual for data access is also available online: https://www.center-tbi.eu/files/SOP-Manual-DAPR-2402020.pdf (accessed on 11 July 2022).
Acknowledgments
We gratefully thank all CENTER-TBI participants and investigators. We are immensely grateful to our participants for helping us in our efforts to improve the care and outcomes for TBI. We acknowledge support by the Open Access Publication Funds of Göttingen University.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Appendix A

Table A1.
Descriptive data analyses by item and time point.
Table A1.
Descriptive data analyses by item and time point.
| Time Point | Item | Mean | SD | Median | Skew | Kurtosis | SE |
|---|---|---|---|---|---|---|---|
| 3M | Headaches | 0.99 | 1.17 | 0 | 0.82 | −0.58 | 0.04 |
| Dizziness | 0.96 | 1.22 | 0 | 0.95 | −0.31 | 0.04 | |
| Nausea | 0.27 | 0.7 | 0 | 2.97 | 9.01 | 0.02 | |
| Noise Sensitivity | 0.8 | 1.14 | 0 | 1.19 | 0.21 | 0.04 | |
| Sleep Disturbance | 1.02 | 1.25 | 0 | 0.98 | −0.25 | 0.04 | |
| Fatigue | 1.65 | 1.31 | 2 | 0.13 | −1.17 | 0.04 | |
| Irritable | 0.94 | 1.13 | 1 | 0.98 | −0.10 | 0.04 | |
| Depressed | 0.91 | 1.16 | 0 | 0.98 | −0.28 | 0.04 | |
| Frustrated | 1.06 | 1.2 | 1 | 0.81 | −0.55 | 0.04 | |
| Forgetful | 1.27 | 1.24 | 1 | 0.58 | −0.79 | 0.04 | |
| Poor Concentration | 1.16 | 1.21 | 1 | 0.65 | −0.74 | 0.04 | |
| Longer to Think | 1.05 | 1.2 | 1 | 0.78 | −0.57 | 0.04 | |
| Blurred Vision | 0.63 | 1.07 | 0 | 1.66 | 1.75 | 0.03 | |
| Light Sensitivity | 0.53 | 0.95 | 0 | 1.82 | 2.6 | 0.03 | |
| Double Vision | 0.35 | 0.9 | 0 | 2.79 | 7.07 | 0.03 | |
| Restless | 0.71 | 1.03 | 0 | 1.29 | 0.64 | 0.03 | |
| 6M | Headaches | 0.88 | 1.14 | 0 | 1 | −0.22 | 0.04 |
| Dizziness | 0.82 | 1.13 | 0 | 1.13 | 0.15 | 0.04 | |
| Nausea | 0.2 | 0.59 | 0 | 3.22 | 10.07 | 0.02 | |
| Noise Sensitivity | 0.78 | 1.14 | 0 | 1.28 | 0.5 | 0.04 | |
| Sleep Disturbance | 0.93 | 1.19 | 0 | 1.03 | −0.11 | 0.04 | |
| Fatigue | 1.49 | 1.32 | 1 | 0.31 | −1.15 | 0.04 | |
| Irritable | 0.93 | 1.13 | 0 | 0.97 | −0.13 | 0.04 | |
| Depressed | 0.85 | 1.13 | 0 | 1.09 | 0.06 | 0.04 | |
| Frustrated | 0.95 | 1.14 | 1 | 0.95 | −0.20 | 0.04 | |
| Forgetful | 1.24 | 1.19 | 1 | 0.53 | −0.79 | 0.04 | |
| Poor Concentration | 1.09 | 1.17 | 1 | 0.69 | −0.69 | 0.04 | |
| Longer to Think | 1.02 | 1.16 | 1 | 0.78 | −0.53 | 0.04 | |
| Blurred Vision | 0.6 | 1.05 | 0 | 1.77 | 2.2 | 0.03 | |
| Light Sensitivity | 0.54 | 0.98 | 0 | 1.84 | 2.54 | 0.03 | |
| Double Vision | 0.32 | 0.84 | 0 | 2.95 | 8.37 | 0.03 | |
| Restless | 0.65 | 1 | 0 | 1.5 | 1.39 | 0.03 | |
| 12M | Headaches | 0.84 | 1.14 | 0 | 1.11 | 0.07 | 0.04 |
| Dizziness | 0.76 | 1.09 | 0 | 1.26 | 0.55 | 0.03 | |
| Nausea | 0.23 | 0.63 | 0 | 3.3 | 12.02 | 0.02 | |
| Noise Sensitivity | 0.83 | 1.21 | 0 | 1.21 | 0.22 | 0.04 | |
| Sleep Disturbance | 1.01 | 1.25 | 0 | 0.99 | −0.23 | 0.04 | |
| Fatigue | 1.42 | 1.32 | 1 | 0.39 | −1.10 | 0.04 | |
| Irritable | 0.93 | 1.1 | 1 | 0.94 | −0.14 | 0.03 | |
| Depressed | 0.87 | 1.15 | 0 | 1.1 | 0.07 | 0.04 | |
| Frustrated | 0.93 | 1.14 | 0 | 1.01 | −0.05 | 0.04 | |
| Forgetful | 1.28 | 1.25 | 1 | 0.58 | −0.79 | 0.04 | |
| Poor Concentration | 1.17 | 1.22 | 1 | 0.67 | −0.67 | 0.04 | |
| Longer to Think | 1.06 | 1.2 | 1 | 0.8 | −0.49 | 0.04 | |
| Blurred Vision | 0.49 | 0.93 | 0 | 2.04 | 3.64 | 0.03 | |
| Light Sensitivity | 0.56 | 0.96 | 0 | 1.72 | 2.16 | 0.03 | |
| Double Vision | 0.28 | 0.75 | 0 | 3.15 | 10.19 | 0.02 | |
| Restless | 0.69 | 1.01 | 0 | 1.37 | 1.02 | 0.03 |
Note: SD = standard deviation; Skew = skewness; SE = standard error; 3M = three months; 6M = six months; 12M = twelve months.

Table A2.
Discrepancies in predicted probabilities based on threshold invariance vs. loading invariance models for each factor.
Table A2.
Discrepancies in predicted probabilities based on threshold invariance vs. loading invariance models for each factor.
| Factor | Time Point | Indicator/Item | Not Experienced at All | No More of a Problem (Than Before) | A Mild Problem | A Moderate Problem | A Severe Problem |
|---|---|---|---|---|---|---|---|
| Somatic | 3M | Headaches | 0.02 | −0.06 | −0.02 | 0.03 | 0.02 |
| Dizziness | 0 | −0.04 | −0.01 | 0.02 | 0.03 | ||
| Nausea | −0.06 | 0.02 | 0.02 | 0.01 | 0.01 | ||
| Noise Sensitivity | −0.07 | −0.04 | 0.03 | 0.04 | 0.04 | ||
| Sleep Disturbance | −0.11 | 0.06 | −0.01 | 0.03 | 0.03 | ||
| Fatigue | 0.2 | −0.15 | −0.15 | 0.02 | 0.07 | ||
| Blurred Vision | −0.05 | −0.02 | 0.02 | 0.02 | 0.03 | ||
| Light Sensitivity | −0.12 | 0.02 | 0.05 | 0.04 | 0.02 | ||
| Double Vision | −0.06 | 0.02 | 0.02 | 0.01 | 0.02 | ||
| 6M | Headaches | 0 | 0 | 0.01 | 0 | 0 | |
| Dizziness | 0 | 0 | 0 | 0 | 0 | ||
| Nausea | −0.01 | 0.01 | 0 | 0.01 | −0.01 | ||
| Noise Sensitivity | 0 | 0 | 0 | −0.09 | 0.09 | ||
| Sleep Disturbance | 0 | −0.01 | 0 | 0.12 | −0.12 | ||
| Fatigue | 0 | 0.01 | 0 | 0.02 | −0.03 | ||
| Blurred Vision | 0 | 0.01 | −0.01 | 0 | 0.01 | ||
| Light Sensitivity | 0 | 0 | 0 | −0.01 | 0.01 | ||
| Double Vision | 0 | −0.01 | 0.01 | 0 | 0 | ||
| 12M | Headaches | −0.01 | 0.01 | 0 | 0 | 0 | |
| Dizziness | 0 | 0 | 0 | 0 | 0 | ||
| Nausea | 0.01 | −0.01 | 0 | 0 | 0 | ||
| Noise Sensitivity | 0.02 | 0 | −0.02 | 0.01 | −0.01 | ||
| Sleep Disturbance | −0.06 | 0.06 | −0.01 | −0.01 | 0 | ||
| Fatigue | 0.07 | −0.09 | 0.02 | 0.01 | −0.01 | ||
| Blurred Vision | −0.01 | 0.01 | −0.01 | 0.01 | 0 | ||
| Light Sensitivity | 0.03 | −0.03 | 0 | 0 | 0 | ||
| Double Vision | 0.01 | −0.01 | 0 | 0 | 0 | ||
| Emotional | 3M | Irritable | −0.01 | −0.09 | 0 | 0.07 | 0.03 |
| Depressed | −0.04 | −0.09 | 0.03 | 0.08 | 0.03 | ||
| Frustrated | 0.06 | −0.23 | 0.04 | 0.1 | 0.03 | ||
| Restless | −0.07 | −0.04 | 0.04 | 0.05 | 0.02 | ||
| 6M | Irritable | 0 | −0.11 | 0.03 | 0.06 | 0.02 | |
| Depressed | −0.03 | −0.10 | 0.02 | 0.08 | 0.03 | ||
| Frustrated | 0.01 | −0.20 | 0.06 | 0.1 | 0.03 | ||
| Restless | −0.09 | −0.04 | 0.07 | 0.05 | 0.01 | ||
| 12M | Irritable | 0.01 | −0.13 | 0.02 | 0.07 | 0.02 | |
| Depressed | −0.06 | −0.10 | 0.06 | 0.08 | 0.02 | ||
| Frustrated | −0.04 | −0.19 | 0.11 | 0.1 | 0.03 | ||
| Restless | −0.06 | −0.05 | 0.05 | 0.05 | 0.01 | ||
| Cognitive | 3M | Forgetful | 0 | 0 | 0 | 0 | 0 |
| Poor Concentration | 0.01 | −0.01 | 0 | 0 | 0 | ||
| Longer to Think | 0 | 0 | 0 | 0 | 0 | ||
| 6M | Forgetful | 0.09 | −0.16 | −0.07 | 0.09 | 0.04 | |
| Poor Concentration | 0.09 | −0.28 | 0.05 | 0.11 | 0.03 | ||
| Longer to Think | 0.02 | −0.18 | 0.03 | 0.09 | 0.03 | ||
| 12M | Forgetful | 0.03 | −0.01 | 0 | −0.01 | 0 | |
| Poor Concentration | 0.03 | −0.02 | −0.01 | 0 | 0 | ||
| Longer to Think | 0.03 | −0.02 | −0.01 | 0 | 0 |
Note: Bolded values are those that represent discrepancies greater than 0.10 in absolute values. The calculation of these probabilities is based on the ordered categorical confirmatory factor analysis output from the lavaan package using diagonally weighted least squares with robust correction; 3M = three months; 6M = six months; 12M = twelve months.
References
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the Global Incidence of Traumatic Brain Injury. J. Neurosurg. 2018, 130, 1080–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brazinova, A.; Rehorcikova, V.; Taylor, M.S.; Buckova, V.; Majdan, M.; Psota, M.; Peeters, W.; Feigin, V.; Theadom, A.; Holkovic, L.; et al. Epidemiology of traumatic brain injury in europe: A living systematic review. J. Neurotrauma 2021, 38, 1411–1440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Savola, O.; Hillbom, M. Early predictors of post-Concussion symptoms in patients with mild head injury. Eur. J. Neurol. 2003, 10, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Meares, S.; Shores, E.A.; Taylor, A.J.; Batchelor, J.; Bryant, R.A.; Baguley, I.J.; Chapman, J.; Gurka, J.; Dawson, K.; Capon, L.; et al. Mild traumatic brain injury does not predict acute postconcussion syndrome. J. Neurol. Neurosurg. Psychiatry 2008, 79, 300–306. [Google Scholar] [CrossRef] [Green Version]
- Dischinger, P.C.; Ryb, G.E.; Kufera, J.A.; Auman, K.M. Early predictors of postconcussive syndrome in a population of trauma patients with mild traumatic brain injury. J. Trauma Acute Care Surg. 2009, 66, 289–297. [Google Scholar] [CrossRef]
- Hoffman, J.M.; Lucas, S.; Dikmen, S.; Braden, C.A.; Brown, A.W.; Brunner, R.; Diaz-Arrastia, R.; Walker, W.C.; Watanabe, T.K.; Bell, K.R. Natural history of headache after traumatic brain injury. J. Neurotrauma 2011, 28, 1719–1725. [Google Scholar] [CrossRef] [Green Version]
- Walker, W.C.; Marwitz, J.H.; Wilk, A.R.; Ketchum, J.M.; Hoffman, J.M.; Brown, A.W.; Lucas, S. Prediction of headache severity (density and functional impact) after traumatic brain injury: A longitudinal multicenter study. Cephalalgia 2013, 33, 998–1008. [Google Scholar] [CrossRef]
- Meares, S.; Shores, E.A.; Taylor, A.J.; Batchelor, J.; Bryant, R.A.; Baguley, I.J.; Chapman, J.; Gurka, J.; Marosszeky, J.E. The prospective course of postconcussion syndrome: The role of mild traumatic brain injury. Neuropsychology 2011, 25, 454–465. [Google Scholar] [CrossRef] [Green Version]
- Merritt, V.C.; Arnett, P.A. Premorbid predictors of postconcussion symptoms in collegiate athletes. J. Clin. Exp. Neuropsychol. 2014, 36, 1098–1111. [Google Scholar] [CrossRef]
- Ling, H.; Hardy, J.; Zetterberg, H. Neurological consequences of traumatic brain injuries in sports. Mol. Cell. Neurosci. 2015, 66, 114–122. [Google Scholar] [CrossRef]
- Cnossen, M.C.; Winkler, E.A.; Yue, J.K.; Okonkwo, D.O.; Valadka, A.B.; Steyerberg, E.W.; Lingsma, H.F.; Manley, G.T.; Dams-O’Connor, K.; Gordon, W.A.; et al. Development of a prediction model for post-Concussive symptoms following mild traumatic brain injury: A Track-TBI Pilot study. J. Neurotrauma 2017, 34, 2396–2409. [Google Scholar] [CrossRef] [PubMed]
- Houck, Z.; Asken, B.; Bauer, R.; Clugston, J. Predictors of post-Concussion symptom severity in a university-Based concussion clinic. Brain Inj. 2019, 33, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Cnossen, M.C.; van der Naalt, J.; Spikman, J.M.; Nieboer, D.; Yue, J.K.; Winkler, E.A.; Manley, G.T.; von Steinbuechel, N.; Polinder, S.; Steyerberg, E.W.; et al. Prediction of persistent post-Concussion symptoms after mild traumatic brain injury. J. Neurotrauma 2018, 35, 2691–2698. [Google Scholar] [CrossRef] [PubMed]
- Chamelian, L.; Feinstein, A. Outcome after mild to moderate traumatic brain injury: The role of dizziness. Arch. Phys. Med. Rehabil. 2004, 85, 1662–1666. [Google Scholar] [CrossRef] [PubMed]
- Ponsford, J.; Nguyen, S.; Downing, M.; Bosch, M.; McKenzie, J.E.; Turner, S.; Chau, M.; Mortimer, D.; Gruen, R.L.; Knott, J.; et al. Factors associated with persistent post-Concussion symptoms following mild traumatic brain injury in adults. J. Rehabil. Med. 2019, 51, 32–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ganti, L.; Khalid, H.; Patel, P.S.; Daneshvar, Y.; Bodhit, A.N.; Peters, K.R. Who gets post-Concussion syndrome? an emergency department-Based prospective analysis. Int. J. Emerg. Med. 2014, 7, 31. [Google Scholar] [CrossRef] [Green Version]
- Stein, M.B.; Ursano, R.J.; Campbell-Sills, L.; Colpe, L.J.; Fullerton, C.S.; Heeringa, S.G.; Nock, M.K.; Sampson, N.A.; Schoenbaum, M.; Sun, X.; et al. Prognostic indicators of persistent post-Concussive symptoms after deployment-Related mild traumatic brain injury: A prospective longitudinal study in U.S. army soldiers. J. Neurotrauma 2016, 33, 2125–2132. [Google Scholar] [CrossRef] [Green Version]
- Goodrich, G.L.; Martinsen, G.L.; Flyg, H.M.; Kirby, J.; Garvert, D.W.; Tyler, C.W. Visual function, traumatic brain injury, and posttraumatic stress disorder. J. Rehabil. Res. Dev. 2014, 51, 547–558. [Google Scholar] [CrossRef] [Green Version]
- Porter, K.E.; Stein, M.B.; Martis, B.; Avallone, K.M.; McSweeney, L.B.; Smith, E.R.; Simon, N.M.; Gargan, S.; Liberzon, I.; Hoge, C.W.; et al. Postconcussive Symptoms (PCS) Following Combat-Related Traumatic Brain Injury (TBI) in Veterans with Posttraumatic Stress Disorder (PTSD): Influence of TBI, PTSD, and Depression on Symptoms Measured by the Neurobehavioral Symptom Inventory (NSI). J. Psychiatr. Res. 2018, 102, 8–13. [Google Scholar] [CrossRef]
- Towns, S.J.; Silva, M.A.; Belanger, H.G. Subjective Sleep Quality and Postconcussion Symptoms Following Mild Traumatic Brain Injury. Brain Inj. 2015, 29, 1337–1341. [Google Scholar] [CrossRef]
- Cronin, H.; O’Loughlin, E. Sleep and Fatigue after TBI. NeuroRehabilitation 2018, 43, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Andelic, N.; Røe, C.; Brunborg, C.; Zeldovich, M.; Løvstad, M.; Løke, D.; Borgen, I.M.; Voormolen, D.C.; Howe, E.I.; Forslund, M.V.; et al. Frequency of Fatigue and Its Changes in the First 6 Months after Traumatic Brain Injury: Results from the CENTER-TBI Study. J. Neurol. 2021, 268, 61–73. [Google Scholar] [CrossRef] [PubMed]
- Cantor, J.B.; Bushnik, T.; Cicerone, K.; Dijkers, M.P.; Gordon, W.; Hammond, F.M.; Kolakowsky-Hayner, S.A.; Lequerica, A.; Nguyen, M.; Spielman, L.A. Insomnia, Fatigue, and Sleepiness in the First 2 Years After Traumatic Brain Injury: An NIDRR TBI Model System Module Study. J. Head Trauma Rehabil. 2012, 27, E1. [Google Scholar] [CrossRef] [PubMed]
- Zeldovich, M.; Wu, Y.-J.; Gorbunova, A.; Mikolic, A.; Polinder, S.; Plass, A.M.; Covic, A.; Asendorf, T.; Andelic, N.; Voormolen, D.C.; et al. Influence of Sociodemographic, Premorbid, and Injury-Related Factors on Post-Concussion Symptoms after Traumatic Brain Injury. J. Clin. Med. 2020, 9, 1931. [Google Scholar] [CrossRef] [PubMed]
- Tator, C.H.; Davis, H.S.; Dufort, P.A.; Tartaglia, M.C.; Davis, K.D.; Ebraheem, A.; Hiploylee, C. Postconcussion Syndrome: Demographics and Predictors in 221 Patients. J. Neurosurg. 2016, 125, 1206–1216. [Google Scholar] [CrossRef] [Green Version]
- Rabinowitz, A.R.; Levin, H.S. Cognitive Sequelae of Traumatic Brain Injury. Psychiatr. Clin. 2014, 37, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Dockree, P.M.; Bellgrove, M.A.; O’Keeffe, F.M.; Moloney, P.; Aimola, L.; Carton, S.; Robertson, I.H. Sustained Attention in Traumatic Brain Injury (TBI) and Healthy Controls: Enhanced Sensitivity with Dual-Task Load. Exp. Brain Res. 2006, 168, 218–229. [Google Scholar] [CrossRef]
- Stewart-Willis, J.J.; Heyanka, D.; Proctor-Weber, Z.; England, H.; Bruhns, M. Premorbid IQ Predicts Postconcussive Symptoms in OEF/OIF/OND Veterans with MTBI. Arch. Clin. Neuropsychol. 2018, 33, 206–215. [Google Scholar] [CrossRef]
- Heidari, K.; Asadollahi, S.; Jamshidian, M.; Abrishamchi, S.N.; Nouroozi, M. Prediction of Neuropsychological Outcome after Mild Traumatic Brain Injury Using Clinical Parameters, Serum S100B Protein and Findings on Computed Tomography. Brain Inj. 2015, 29, 33–40. [Google Scholar] [CrossRef]
- Theadom, A.; Parag, V.; Dowell, T.; McPherson, K.; Starkey, N.; Barker-Collo, S.; Jones, K.; Ameratunga, S.; Feigin, V.L.; on behalf of the BIONIC Research Group. Persistent Problems 1 Year after Mild Traumatic Brain Injury: A Longitudinal Population Study in New Zealand. Br. J. Gen. Pract. 2016, 66, e16–e23. [Google Scholar] [CrossRef] [Green Version]
- Shah, S.A.; Goldin, Y.; Conte, M.M.; Goldfine, A.M.; Mohamadpour, M.; Fidali, B.C.; Cicerone, K.; Schiff, N.D. Executive Attention Deficits after Traumatic Brain Injury Reflect Impaired Recruitment of Resources. NeuroImage Clin. 2017, 14, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Ozga, J.E.; Povroznik, J.M.; Engler-Chiurazzi, E.B.; Haar, C.V. Executive (Dys)Function after Traumatic Brain Injury: Special Considerations for Behavioral Pharmacology. Behav. Pharmacol. 2018, 29, 617–637. [Google Scholar] [CrossRef] [PubMed]
- Pettemeridou, E.; Kennedy, M.R.T.; Constantinidou, F. Executive Functions, Self-Awareness and Quality of Life in Chronic Moderate-to-Severe TBI. NeuroRehabilitation 2020, 46, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Sigurdardottir, S.; Andelic, N.; Wehling, E.; Roe, C.; Anke, A.; Skandsen, T.; Holthe, O.O.; Jerstad, T.; Aslaksen, P.M.; Schanke, A.-K. Neuropsychological Functioning in a National Cohort of Severe Traumatic Brain Injury: Demographic and Acute Injury–Related Predictors. J. Head Trauma Rehabil. 2015, 30, E1–E12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skandsen, T.; Finnanger, T.G.; Andersson, S.; Lydersen, S.; Brunner, J.F.; Vik, A. Cognitive Impairment 3 Months After Moderate and Severe Traumatic Brain Injury: A Prospective Follow-Up Study. Arch. Phys. Med. Rehabil. 2010, 91, 1904–1913. [Google Scholar] [CrossRef]
- Finnanger, T.G.; Skandsen, T.; Andersson, S.; Lydersen, S.; Vik, A.; Indredavik, M. Differentiated Patterns of Cognitive Impairment 12 Months after Severe and Moderate Traumatic Brain Injury. Brain Inj. 2013, 27, 1606–1616. [Google Scholar] [CrossRef]
- Davis-Hayes, C.; Gossett, J.D.; Levine, W.N.; Shams, T.; Harada, J.; Mitnick, J.; Noble, J. Sex-Specific Outcomes and Predictors of Concussion Recovery. JAAOS-J. Am. Acad. Orthop. Surg. 2017, 25, 818–828. [Google Scholar] [CrossRef]
- Calvillo, M.; Irimia, A. Neuroimaging and Psychometric Assessment of Mild Cognitive Impairment After Traumatic Brain Injury. Front. Psychol. 2020, 11, 1423. [Google Scholar] [CrossRef]
- Singh, R.; Mason, S.; Lecky, F.; Dawson, J. Prevalence of Depression after TBI in a Prospective Cohort: The SHEFBIT Study. Brain Inj. 2018, 32, 84–90. [Google Scholar] [CrossRef]
- Seel, R.T.; Macciocchi, S.; Kreutzer, J.S. Clinical Considerations for the Diagnosis of Major Depression After Moderate to Severe TBI. J. Head Trauma Rehabil. 2010, 25, 99–112. [Google Scholar] [CrossRef]
- Rapoport, M.J. Depression Following Traumatic Brain Injury. CNS Drugs 2012, 26, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Ponsford, J. Anxiety and depression following TBI. In Neurobehavioural Disability and Social Handicap Following Traumatic Brain Injury; Psychology Press: London, UK, 2017; ISBN 978-1-315-68471-0. [Google Scholar]
- Scholten, A.C.; Haagsma, J.A.; Cnossen, M.C.; Olff, M.; van Beeck, E.F.; Polinder, S. Prevalence of and Risk Factors for Anxiety and Depressive Disorders after Traumatic Brain Injury: A Systematic Review. J. Neurotrauma 2016, 33, 1969–1994. [Google Scholar] [CrossRef] [PubMed]
- Clarke, L.A.; Genat, R.C.; Anderson, J.F.I. Long-Term Cognitive Complaint and Post-Concussive Symptoms Following Mild Traumatic Brain Injury: The Role of Cognitive and Affective Factors. Brain Inj. 2012, 26, 298–307. [Google Scholar] [CrossRef]
- Sigurdardottir, S.; Andelic, N.; Roe, C.; Jerstad, T.; Schanke, A.-K. Post-Concussion Symptoms after Traumatic Brain Injury at 3 and 12 Months Post-Injury: A Prospective Study. Brain Inj. 2009, 23, 489–497. [Google Scholar] [CrossRef]
- Ponsford, J.; Cameron, P.; Fitzgerald, M.; Grant, M.; Mikocka-Walus, A.; Schönberger, M. Predictors of Postconcussive Symptoms 3 Months after Mild Traumatic Brain Injury. Neuropsychology 2012, 26, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Bahraini, N.H.; Simpson, G.K.; Brenner, L.A.; Hoffberg, A.S.; Schneider, A.L. Suicidal Ideation and Behaviours after Traumatic Brain Injury: A Systematic Review. Brain Impair. 2013, 14, 92–112. [Google Scholar] [CrossRef] [Green Version]
- Mackelprang, J.L.; Bombardier, C.H.; Fann, J.R.; Temkin, N.R.; Barber, J.K.; Dikmen, S.S. Rates and Predictors of Suicidal Ideation During the First Year After Traumatic Brain Injury. Am. J. Public Health. 2014, 104, e100–e107. [Google Scholar] [CrossRef]
- Tsaousides, T.; Cantor, J.B.; Gordon, W.A. Suicidal Ideation Following Traumatic Brain Injury: Prevalence Rates and Correlates in Adults Living in the Community. J. Head Trauma Rehabil. 2011, 26, 265–275. [Google Scholar] [CrossRef]
- Rosenthal, J.F.; Erickson, J.C. Post-Traumatic Stress Disorder in U.S. Soldiers with Post-Traumatic Headache. Headache J. Head Face Pain 2013, 53, 1564–1572. [Google Scholar] [CrossRef]
- Rao, V.; Spiro, J.R.; Schretlen, D.J.; Cascella, N.G. Apathy Syndrome After Traumatic Brain Injury Compared with Deficits in Schizophrenia. Psychosomatics 2007, 48, 217–222. [Google Scholar] [CrossRef]
- Starkstein, S.E.; Pahissa, J. Apathy Following Traumatic Brain Injury. Psychiatr. Clin. 2014, 37, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-C.; Hua, M.-S.; Lin, W.-C.; Tsai, Y.-H.; Huang, S.-J. Irritability Following Traumatic Brain Injury: Divergent Manifestations of Annoyance and Verbal Aggression. Brain Inj. 2012, 26, 1185–1191. [Google Scholar] [CrossRef]
- Hammond, F.M.; Davis, C.S.; Cook, J.R.; Philbrick, P.; Hirsch, M.A. Relational Dimension of Irritability Following Traumatic Brain Injury: A Qualitative Analysis. Brain Inj. 2012, 26, 1287–1296. [Google Scholar] [CrossRef] [PubMed]
- Miles, S.R.; Hammond, F.M.; Neumann, D.; Silva, M.A.; Tang, X.; Kajankova, M.; Dillahunt-Aspillaga, C.; Nakase-Richardson, R. Evolution of Irritability, Anger, and Aggression after Traumatic Brain Injury: Identifying and Predicting Subgroups. J. Neurotrauma 2021, 38, 1827–1833. [Google Scholar] [CrossRef] [PubMed]
- Gracia-Garcia, P.; Mielke, M.M.; Rosenberg, P.; Bergey, A.; Rao, V. Personality Changes in Brain Injury. JNP 2011, 23, E14. [Google Scholar] [CrossRef]
- Rush, B.K.; Malec, J.F.; Brown, A.W.; Moessner, A.M. Personality and Functional Outcome Following Traumatic Brain Injury. Rehabil. Psychol. 2006, 51, 257–264. [Google Scholar] [CrossRef]
- Lippert-Grüner, M.; Kuchta, J.; Hellmich, M.; Klug, N. Neurobehavioural Deficits after Severe Traumatic Brain Injury (TBI). Brain Inj. 2006, 20, 569–574. [Google Scholar] [CrossRef]
- Wolfe, L.F.; Sahni, A.S.; Attarian, H. Sleep Disorders in Traumatic Brain Injury. NeuroRehabilitation 2018, 43, 257–266. [Google Scholar] [CrossRef]
- Ouellet, M.-C.; Beaulieu-Bonneau, S.; Morin, C.M. Insomnia in Patients with Traumatic Brain Injury: Frequency, Characteristics, and Risk Factors. J. Head Trauma Rehabil. 2006, 21, 199–212. [Google Scholar] [CrossRef]
- Jain, A.; Mittal, R.S.; Sharma, A.; Sharma, A.; Gupta, I.D. Study of Insomnia and Associated Factors in Traumatic Brain Injury. Asian J. Psychiatry 2014, 8, 99–103. [Google Scholar] [CrossRef]
- King, N.S.; Crawford, S.; Wenden, F.J.; Moss, N.E.G.; Wade, D.T. The Rivermead Post Concussion Symptoms Questionnaire: A Measure of Symptoms Commonly Experienced after Head Injury and Its Reliability. J Neurol. 1995, 242, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Carroll, L.; Cassidy, J.D.; Peloso, P.; Borg, J.; von Holst, H.; Holm, L.; Paniak, C.; Pépin, M. Prognosis for Mild Traumatic Brain Injury: Results of the Who Collaborating Centre Task Force on Mild Traumatic Brain Injury. J. Rehabil. Med. 2004, 36, 84–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Røe, C.; Sveen, U.; Alvsåker, K.; Bautz-Holter, E. Post-Concussion Symptoms after Mild Traumatic Brain Injury: Influence of Demographic Factors and Injury Severity in a 1-Year Cohort Study. Disabil. Rehabil. 2009, 31, 1235–1243. [Google Scholar] [CrossRef] [PubMed]
- King, N. Permanent Post Concussion Symptoms after Mild Head Injury: A Systematic Review of Age and Gender Factors. NeuroRehabilitation 2014, 34, 741–748. [Google Scholar] [CrossRef]
- Hiploylee, C.; Dufort, P.A.; Davis, H.S.; Wennberg, R.A.; Tartaglia, M.C.; Mikulis, D.; Hazrati, L.-N.; Tator, C.H. Longitudinal Study of Postconcussion Syndrome: Not Everyone Recovers. J. Neurotrauma 2017, 34, 1511–1523. [Google Scholar] [CrossRef] [Green Version]
- Gorgoraptis, N.; Zaw-Linn, J.; Feeney, C.; Tenorio-Jimenez, C.; Niemi, M.; Malik, A.; Ham, T.; Goldstone, A.P.; Sharp, D.J. Cognitive Impairment and Health-Related Quality of Life Following Traumatic Brain Injury. NeuroRehabilitation 2019, 44, 321–331. [Google Scholar] [CrossRef] [Green Version]
- Polinder, S.; Haagsma, J.A.; van Klaveren, D.; Steyerberg, E.W.; van Beeck, E.F. Health-Related Quality of Life after TBI: A Systematic Review of Study Design, Instruments, Measurement Properties, and Outcome. Popul. Health Metr. 2015, 13, 4. [Google Scholar] [CrossRef] [Green Version]
- Dijkers, M.P. Quality of Life after Traumatic Brain Injury: A Review of Research Approaches and Findings11No Commercial Party Having a Direct Financial Interest in the Results of the Research Supporting This Article Has or Will Confer a Benefit upon the Authors(s) or upon Any Organization with Which the Author(s) Is/Are Associated. Arch. Phys. Med. Rehabil. 2004, 85, 21–35. [Google Scholar] [CrossRef]
- Wäljas, M.; Iverson, G.L.; Lange, R.T.; Liimatainen, S.; Hartikainen, K.M.; Dastidar, P.; Soimakallio, S.; Öhman, J. Return to Work Following Mild Traumatic Brain Injury. J. Head Trauma Rehabil. 2014, 29, 443–450. [Google Scholar] [CrossRef]
- van Velzen, J.M.; van Bennekom, C.A.M.; Edelaar, M.J.A.; Sluiter, J.K.; Frings-Dresen, M.H.W. How Many People Return to Work after Acquired Brain Injury?: A Systematic Review. Brain Inj. 2009, 23, 473–488. [Google Scholar] [CrossRef]
- Sigurdardottir, S.; Andelic, N.; Wehling, E.; Anke, A.; Skandsen, T.; Holthe, O.O.; Manskow, U.S.; Roe, C. Return to Work after Severe Traumatic Brain Injury: A National Study with a One-Year Follow-Up of Neurocognitive and Behavioural Outcomes. Neuropsychol. Rehabil. 2020, 30, 281–297. [Google Scholar] [CrossRef] [PubMed]
- Toglia, J.; Golisz, K. Traumatic Brain Injury (TBI) and the impact on daily life. In Changes in the Brain: Impact on Daily Life; Chiaravalloti, N.D., Goverover, Y., Eds.; Springer: New York, NY, USA, 2017; pp. 117–143. ISBN 978-0-387-98188-8. [Google Scholar]
- García-Molina, A.; Bernabeu Guitart, M.; Roig-Rovira, T. Traumatic brain injury and daily life: The role of executive function. Psicothema 2010, 22, 430–435. [Google Scholar] [PubMed]
- Bivona, U.; D’Ippolito, M.; Giustini, M.; Vignally, P.; Longo, E.; Taggi, F.; Formisano, R. Return to Driving After Severe Traumatic Brain Injury: Increased Risk of Traffic Accidents and Personal Responsibility. J. Head Trauma Rehabil. 2012, 27, 210–215. [Google Scholar] [CrossRef]
- Preece, M.H.W.; Geffen, G.M.; Horswill, M.S. Return-To-Driving Expectations Following Mild Traumatic Brain Injury. Brain Inj. 2013, 27, 83–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, R.; Liu, W.; Dong, J.; Zhang, J.; Xu, L.; Zhang, B.; Tao, X.; Li, J.; Liu, B. Prognostic Predictors of Early Outcomes and Discharge Status of Patients Undergoing Decompressive Craniectomy After Severe Traumatic Brain Injury. World Neurosurg. 2019, 126, e101–e108. [Google Scholar] [CrossRef]
- Gritti, P.; Zangari, R.; Carobbio, A.; Zucchi, A.; Lorini, F.L.; Ferri, F.; Agostinis, C.; Lanterna, L.A.; Brembilla, C.; Foresti, C.; et al. Acute and Subacute Outcome Predictors in Moderate and Severe Traumatic Brain Injury: A Retrospective Monocentric Study. World Neurosurg. 2019, 128, e531–e540. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Mushkudiani, N.; Perel, P.; Butcher, I.; Lu, J.; McHugh, G.S.; Murray, G.D.; Marmarou, A.; Roberts, I.; Habbema, J.D.F.; et al. Predicting Outcome after Traumatic Brain Injury: Development and International Validation of Prognostic Scores Based on Admission Characteristics. PLoS Med. 2008, 5, e165. [Google Scholar] [CrossRef] [Green Version]
- Booker, J.; Sinha, S.; Choudhari, K.; Dawson, J.; Singh, R. Description of the Predictors of Persistent Post-Concussion Symptoms and Disability after Mild Traumatic Brain Injury: The SHEFBIT Cohort. Br. J. Neurosurg. 2019, 33, 367–375. [Google Scholar] [CrossRef]
- Brown, N.J.; Mannix, R.C.; O’Brien, M.J.; Gostine, D.; Collins, M.W.; Meehan, W.P. III Effect of Cognitive Activity Level on Duration of Post-Concussion Symptoms. Pediatrics 2014, 133, e299–e304. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, K.A.; Edmed, S.L.; Greenslade, J.H.; White, M.; Chu, K.; Lukin, B.; Lange, R.T.; Lurie, J.K. Psychological Predictors of Postconcussive Symptoms Following Traumatic Injury. J. Head Trauma Rehabil. 2018, 33, E47–E60. [Google Scholar] [CrossRef]
- Seagly, K.S.; O’Neil, R.L.; Hanks, R.A. Pre-Injury Psychosocial and Demographic Predictors of Long-Term Functional Outcomes Post-TBI. Brain Inj. 2018, 32, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Yue, J.K.; Cnossen, M.C.; Winkler, E.A.; Deng, H.; Phelps, R.R.L.; Coss, N.A.; Sharma, S.; Robinson, C.K.; Suen, C.G.; Vassar, M.J.; et al. Pre-Injury Comorbidities Are Associated with Functional Impairment and Post-Concussive Symptoms at 3- and 6-Months After Mild Traumatic Brain Injury: A TRACK-TBI Study. Front. Neurol. 2019, 10, 343. [Google Scholar] [CrossRef] [PubMed]
- Kraus, J.F.; Peek-Asa, C.; McArthur, D. The Independent Effect of Gender on Outcomes Following Traumatic Brain Injury: A Preliminary Investigation. Neurosurg. Focus 2000, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Wood, R.L.; Rutterford, N.A. Demographic and Cognitive Predictors of Long-Term Psychosocial Outcome Following Traumatic Brain Injury. J. Int. Neuropsychol. Soc. 2006, 12, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Arango-Lasprilla, J.C.; Kreutzer, J.S. Racial and Ethnic Disparities in Functional, Psychosocial, and Neurobehavioral Outcomes After Brain Injury. J. Head Trauma Rehabil. 2010, 25, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Gary, K.W.; Arango-Lasprilla, J.C.; Stevens, L.F. Do Racial/Ethnic Differences Exist in Post-Injury Outcomes after TBI? A Comprehensive Review of the Literature. Brain Inj. 2009, 23, 775–789. [Google Scholar] [CrossRef] [PubMed]
- Zador, Z.; Sperrin, M.; King, A.T. Predictors of Outcome in Traumatic Brain Injury: New Insight Using Receiver Operating Curve Indices and Bayesian Network Analysis. PLoS ONE 2016, 11, e0158762. [Google Scholar] [CrossRef]
- Colantonio, A.; Escobar, M.D.; Chipman, M.; McLellan, B.; Austin, P.C.; Mirabella, G.; Ratcliff, G. Predictors of Postacute Mortality Following Traumatic Brain Injury in a Seriously Injured Population. J. Trauma Acute Care Surg. 2008, 64, 876–882. [Google Scholar] [CrossRef] [Green Version]
- Traylor, J.I.; El Ahmadieh, T.Y.; Bedros, N.M.; Al Adli, N.; Stutzman, S.E.; Venkatachalam, A.M.; Pernik, M.N.; Collum, C.M.; Douglas, P.M.; Aiyagari, V.; et al. Quantitative Pupillometry in Patients with Traumatic Brain Injury and Loss of Consciousness: A Prospective Pilot Study. J. Clin. Neurosci. 2021, 91, 88–92. [Google Scholar] [CrossRef]
- De Guise, E.; Leblanc, J.; Dagher, J.; Lamoureux, J.; Jishi, A.A.; Maleki, M.; Marcoux, J.; Feyz, M. Early Outcome in Patients with Traumatic Brain Injury, Pre-Injury Alcohol Abuse and Intoxication at Time of Injury. Brain Inj. 2009, 23, 853–865. [Google Scholar] [CrossRef]
- Andelic, N.; Jerstad, T.; Sigurdardottir, S.; Schanke, A.-K.; Sandvik, L.; Roe, C. Effects of Acute Substance Use and Pre-Injury Substance Abuse on Traumatic Brain Injury Severity in Adults Admitted to a Trauma Centre. J Trauma Manag. Outcomes 2010, 4, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolakowsky-Hayner, S.A.; Kreutzer, J.S. Pre-Injury Crime, Substance Abuse, and Neurobehavioural Functioning after Traumatic Brain Injury. Brain Inj. 2001, 15, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.A.; Choudhary, M.; Sinha, V.D.; Gora, N.; Bairwa, M. Predictors of Outcome After Traumatic Brain Injuries: Experience of a Tertiary Health Care Institution in Northwest India. World Neurosurg. 2019, 126, e699–e705. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, K.A.; Edmed, S.L.; Allan, A.C.; Smith, S.S.; Karlsson, L.J.E. The Role of Psychological Resilience and MTBI as Predictors of Postconcussional Syndrome Symptomatology. Rehabil. Psychol. 2015, 60, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Mallya, S.; Sutherland, J.; Pongracic, S.; Mainland, B.; Ornstein, T.J. The Manifestation of Anxiety Disorders after Traumatic Brain Injury: A Review. J. Neurotrauma 2015, 32, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Lange, R.T.; French, L.M.; Lippa, S.M.; Bailie, J.M.; Brickell, T.A. Posttraumatic Stress Disorder Is a Stronger Predictor of Long-Term Neurobehavioral Outcomes Than Traumatic Brain Injury Severity. J. Trauma. Stress 2020, 33, 318–329. [Google Scholar] [CrossRef]
- Wäljas, M.; Iverson, G.L.; Lange, R.T.; Hakulinen, U.; Dastidar, P.; Huhtala, H.; Liimatainen, S.; Hartikainen, K.; Öhman, J. A Prospective Biopsychosocial Study of the Persistent Post-Concussion Symptoms Following Mild Traumatic Brain Injury. J. Neurotrauma 2015, 32, 534–547. [Google Scholar] [CrossRef]
- Wilde, E.A.; Whiteneck, G.G.; Bogner, J.; Bushnik, T.; Cifu, D.X.; Dikmen, S.; French, L.; Giacino, J.T.; Hart, T.; Malec, J.F.; et al. Recommendations for the Use of Common Outcome Measures in Traumatic Brain Injury Research. Arch. Phys. Med. Rehabil. 2010, 91, 1650–1660.e17. [Google Scholar] [CrossRef]
- NINDS Project Overview. Available online: https://www.commondataelements.ninds.nih.gov/Traumatic%20Brain%20Injury (accessed on 17 May 2022).
- Smith-Seemiller, L.; Fow, N.R.; Kant, R.; Franzen, M.D. Presence of Post-Concussion Syndrome Symptoms in Patients with Chronic Pain vs Mild Traumatic Brain Injury. Brain Inj. 2003, 17, 199–206. [Google Scholar] [CrossRef]
- Eyres, S.; Carey, A.; Gilworth, G.; Neumann, V.; Tennant, A. Construct Validity and Reliability of the Rivermead Post-Concussion Symptoms Questionnaire. Clin. Rehabil. 2005, 19, 878–887. [Google Scholar] [CrossRef]
- Herrmann, N.; Rapoport, M.J.; Rajaram, R.D.; Chan, F.; Kiss, A.; Ma, A.K.; Feinstein, A.; McCullagh, S.; Lanctôt, K.L. Factor Analysis of the Rivermead Post-Concussion Symptoms Questionnaire in Mild-to-Moderate Traumatic Brain Injury Patients. JNP 2009, 21, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Lannsjö, M.; Borg, J.; Björklund, G.; Af Geijerstam, J.-L.; Lundgren-Nilsson, A. Internal Construct Validity of the Rivermead Post-Concussion Symptoms Questionnaire. J. Rehabil. Med. 2011, 43, 997–1002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, M.; Skilbeck, C.; Cannan, P.; Slatyer, M. The Structure of the Rivermead Post-Concussion Symptoms Questionnaire in Australian Adults with Traumatic Brain Injury. Brain Impair. 2018, 19, 166–182. [Google Scholar] [CrossRef]
- Zeldovich, M.; Bockhop, F.; Plass, A.M.; Covic, A.; Mueller, I.; Polinder, S.; Mikolic, A.; van der Vlegel, M.; Steinbuechel, N. CENTER-TBI participants and investigators Comparability of the Six Rivermead Post-Concussion Symptoms Questionnaire Translations: Results from the CENTER-TBI Study. PLoS ONE 2021. under revision. [Google Scholar]
- Potter, S.; Leigh, E.; Wade, D.; Fleminger, S. The Rivermead Post Concussion Symptoms Questionnaire. J. Neurol. 2006, 253, 1603–1614. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Millsap, R.E.; West, S.G.; Tein, J.-Y.; Tanaka, R.; Grimm, K.J. Testing Measurement Invariance in Longitudinal Data with Ordered-Categorical Measures. Psychol. Methods 2017, 22, 486–506. [Google Scholar] [CrossRef] [PubMed]
- Agtarap, S.; Kramer, M.D.; Campbell-Sills, L.; Yuh, E.; Mukherjee, P.; Manley, G.T.; McCrea, M.A.; Dikmen, S.; Giacino, J.T.; Stein, M.B.; et al. Invariance of the Bifactor Structure of Mild Traumatic Brain Injury (MTBI) Symptoms on the Rivermead Postconcussion Symptoms Questionnaire Across Time, Demographic Characteristics, and Clinical Groups: A TRACK-TBI Study. Assessment 2021, 28, 1656–1670. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Wiegers, E.; Sewalt, C.; Buki, A.; Citerio, G.; De Keyser, V.; Ercole, A.; Kunzmann, K.; Lanyon, L.; Lecky, F.; et al. Case-Mix, Care Pathways, and Outcomes in Patients with Traumatic Brain Injury in CENTER-TBI: A European Prospective, Multicentre, Longitudinal, Cohort Study. Lancet Neurol. 2019, 18, 923–934. [Google Scholar] [CrossRef]
- Teasdale, G.; Jennett, B. Assessment of coma and impaired consciousness: A Practical Scale. Lancet 1974, 304, 81–84. [Google Scholar] [CrossRef]
- Gennarelli, T.A.; Wodzin, E. The Abbreviated Injury Scale 2005. Available online: https://www.nazl.nl/sites/nazl/files/2021-06/AIS0508_codeboek.pdf (accessed on 11 July 2022).
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; Guilford Publications: New York, NY, USA, 2015; ISBN 978-1-4625-2335-1. [Google Scholar]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting Structural Equation Modeling and Confirmatory Factor Analysis Results: A Review. J. Educ. Res. 2006, 99, 323–338. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Soft. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Soft. 2012, 48, 1–36. [Google Scholar] [CrossRef] [Green Version]
- Van De Schoot, R.; Schmidt, P.; De Beuckelaer, A.; Lek, K.; Zondervan-Zwijnenburg, M. Editorial: Measurement Invariance. Front. Psychol. 2015, 6, 1064. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renga, V. Clinical Evaluation and Treatment of Patients with Postconcussion Syndrome. Neurol. Res. Int. 2021, 2021, e5567695. [Google Scholar] [CrossRef]
- Gozt, A.; Licari, M.; Halstrom, A.; Milbourn, H.; Lydiard, S.; Black, A.; Arendts, G.; Macdonald, S.; Song, S.; MacDonald, E.; et al. Towards the Development of an Integrative, Evidence-Based Suite of Indicators for the Prediction of Outcome Following Mild Traumatic Brain Injury: Results from a Pilot Study. Brain Sci. 2020, 10, 23. [Google Scholar] [CrossRef] [Green Version]
- Roy, D.; Peters, M.E.; Everett, A.; Leoutsakos, J.-M.; Yan, H.; Rao, V.; Bechtold, K.; Sair, H.; Van Meter, T.E.; Falk, H.; et al. Loss of Consciousness and Altered Mental State Predicting Depressive and Post-Concussive Symptoms after Mild Traumatic Brain Injury. Brain Inj. 2019, 33, 1064–1069. [Google Scholar] [CrossRef]
- Voormolen, D.C.; Cnossen, M.C.; Polinder, S.; von Steinbuechel, N.; Vos, P.E.; Haagsma, J.A. Divergent Classification Methods of Post-Concussion Syndrome after Mild Traumatic Brain Injury: Prevalence Rates, Risk Factors, and Functional Outcome. J. Neurotrauma 2018, 35, 1233–1241. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).