Abstract
Objectives: To estimate stroke risk in Taiwanese patients with gout. Methods: We enrolled patients from the Taiwan National Health Insurance Database, with gout diagnosed from 2000 to 2008, and followed them up until December 2018. This cohort was propensity score-matched according to birth year, sex, the date of diagnosis of gout, comorbidities, and co-medications with individuals without gout (controls) (n = 310,820 in each group). Stroke was defined as the primary diagnosis at discharge after the index date. To evaluate ischemic and hemorrhagic stroke risks, we calculated their incidence, hazard ratio (HR), and two-year moving average incidence rate. Results: The incidence (95% CI) and HR of ischemic stroke were lower in the gout group than in the control group in the first 3 years (incidence: 4.74 [4.60–4.88] vs. 5.17 [5.03–5.32] per 1000 person-years; HR: 0.92 [0.88–0.96]), then became significantly higher than in the control group after 3 years (incidence: 4.10 [4.04–4.16] vs. 3.81 [3.75–3.87] per 1000 person-years; HR: 1.08 [1.05–1.10]). Similarly, the incidence (95% CI) and HR of hemorrhagic stroke was lower in the gout group than in the control group in the first 3 years (incidence: 1.51 [1.43–1.59] vs. 1.70 [1.62–1.79] per 1000 person-years; HR: 0.88 [0.82–0.92]), then became significantly higher than in controls after 3 years (incidence: 1.43 [1.39–1.46] vs. 1.26 [1.22–1.29] per 1000 person-years; HR: 1.14 [1.10–1.18]). Conclusions: In Taiwan, patients with gout had higher risks of ischemic and hemorrhagic stroke after 3 years.
1. Introduction
Gout, the most common form of inflammatory arthritis, is characterized by monosodium urate (MSU) crystal deposition–related manifestations. Gout diagnosis depends on clinical symptoms, laboratory testing, and imaging results [1]. The typical gout symptoms include acute swelling, pain, or tenderness in one or more peripheral joints or bursae. However, it is also associated with systemic comorbidities, such as metabolic syndromes (e.g., obesity, hypertension, diabetes mellitus [DM], and dyslipidemia), cardiovascular disease, consequences of excessive alcohol intake, and chronic kidney disease [2,3,4,5,6,7].
Stroke—defined as a neurological deficit that persists for more than 24 h resulting from a vascular cause, including cerebral infarction, intracerebral hemorrhage, and subarachnoid hemorrhage (SAH)—is a significant cause of disability and death worldwide [8]. Moreover, gout is associated with vascular diseases due to endothelial dysfunction, platelet adhesiveness, and plasma thromboembolic activity [9,10]. An animal study found hyperuricemia associated with high systemic blood pressure and COX-2–mediated, thromboxane-induced vascular disease [11]. Hyperuricemia can trigger the activation of neutrophils and the production of immune mediators associated with pro-inflammatory functions. Soluble uric acid can mediate radical generation and function as a pro-oxidant [12]. These vascular inflammatory mechanisms may contribute to vascular disease development in patients with gout. Moreover, previous studies demonstrated the importance of inflammatory pathways in the pathogenesis of ischemic stroke [13,14]. Thus, gout may potentially be one of the risk factors for stroke.
However, studies on the hyperuricemia–gout–stroke relationships have reported conflicting results. Some studies have indicated that hyperuricemia and gout increase the risks of ischemic stroke, cardiovascular disease, and ischemic stroke-related mortality [15,16,17,18,19,20,21,22,23,24,25]. In contrast, others have suggested that hyperuricemia and gout are not associated with the risks of stroke or cardiovascular disease [26,27]. Furthermore, limited studies report the relationship between gout and hemorrhagic stroke, which warrants further investigation. In the present study, we estimated the ischemic and hemorrhagic stroke risks in patients with gout compared with the matched non-gout population using the Taiwan National Health Insurance (NHI) Database.
2. Methods
Ethical approval was obtained from the Institutional Review Board (IRB) of Chang Gung Medical Foundation (IRB number: 201800242B1). Because we analyzed anonymized data, patient consent was not required.
2.1. Data Source
Taiwan’s National Health Insurance was established in 1996 and covers almost the entire population of Taiwan. The NHI database records the sex, date of birth, residence, insurance details, family relationships, dates of inpatient and outpatient visits, medical diagnoses, medical expenditures, prescription details, vaccination status, examinations, operations, procedures, and fees incurred for all NHI beneficiaries. A unique personal identifier—encrypted before data are released to researchers upon request—is used to link, internally and externally, all the NHI database data with those from other databases. Consequently, all NHI beneficiary data, including those for major diseases (e.g., gout and stroke), are available to researchers.
2.2. Study Design and Study Population
We identified a cohort of incident patients diagnosed with gout from 2000 to 2008 in Taiwan from the NHI database (the gout cohort) and followed them up until the end of 2018. Patients with gout received a primary diagnosis of gout (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code: 274). To avoid misclassification (e.g., cellulitis or monoarthritis for gout), patients had to have at least two outpatient visits for gout diagnosis and were prescribed urate-lowering agents (e.g., allopurinol, febuxostat, benzbromarone, probenecid, or sulfinpyrazone). The non-gout control group were patients without diagnosis of gout (ICD-9-CM code: 274) in principal, additional, or other diagnoses from 2000 to 2008. In order to have the two compatible cohorts, the non-gout cohort was first 5:1 matched according to birth year, sex, and the year of diagnosis of gout, because of the substantial number (n = 26,507,678) of beneficiaries in the NHI during this study period. Next, the non-gout control cohort was 1:1 propensity score matched according to birth year, sex, the year of diagnosis of gout, comorbidities, and co-medications within a caliper width equal to 0.2, the SD of the logit of the estimated propensity score [28]. The flow of patient selection is illustrated in Figure 1.
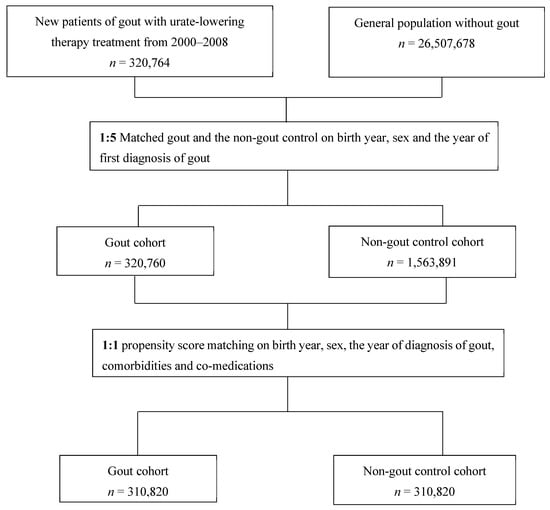
Figure 1.
Patient selection flow.
2.3. Ascertainment of Outcome, Comorbidities, and Co-Medications
The incidence of ischemic and hemorrhagic stroke was calculated separately for both cohorts. We identified stroke type according to the primary diagnosis at discharge as ischemic stroke (ICD-9-CM codes during 2000–2015: 433, 434, 436; ICD-10-CM codes since 2016: I63, I64) or hemorrhagic stroke (ICD-9-CM codes during 2000–2015: 430–432, 852, 853; ICD-10-CM codes since 2016: I60–I62). The definition of stroke necessitates a hospitalization with discharge as ischemic or hemorrhagic stroke to eliminate misclassification (e.g., focal neurological sign, TIA for stroke). The accuracy of ischemic and hemorrhagic stroke diagnosis in the NHI database has been validated previously; 97.85% of an NHI database sample was confirmed through radiology examination and clinical presentation [29].
Baseline covariates were obtained from claim records with the diagnoses, medications, or procedures codes before the index date. A history of any prescription medicine was confined to medications taken at least once within 3 months before the index date. The definition and coding of comorbidities are shown in Supplemental Table S1.
2.4. Statistical Analysis
The propensity score was obtained using the generalized boosted model (GBM), which included demographic variables, comorbidities, and co-medications (Table 1). The advantages of GBM automatically determine the best functions of covariates to achieve an optimal balance between the two cohort groups, and it is less affected by extreme weights [30]. The absolute standardized mean difference (ASMD) was used to measure the balance of demographic variables, comorbidities, and co-medications between the two cohorts. An ASMD larger than 0.1 was considered statistically significant [31].

Table 1.
Demographic and clinical characteristics of gout and non-gout control cohorts in Taiwan, 2000 to 2008.
The two groups were followed from the index date until a stroke, death, or 31 December 2018, whichever occurred first. The incidence is the number of event occurrences divided by the total following person-year. A 2-year moving average of the stroke incidence rate was calculated to determine how the rate varied with time after the diagnosis of gout (index date). The 95% confidence interval (CI) of the incidence rate was based on the relationship between the F distribution and binomial distribution [32]. Cox’s proportional hazards model was used to obtain the hazard ratio (HR) with 95% (CIs) for stroke in the gout cohort, with the non-gout cohort as a reference group. Note that only the gout status vs. non-gout status was included in the Cox model because the two cohorts were compatible in demographics, comorbidities, and co-medications [33]. All statistical analyses were performed using SAS (version 9.4; SAS Institute, Cary, NC, USA).
3. Results
Table 1 presents the demographic and clinical characteristics of the gout and control cohorts. In both cohorts, the proportion of men was around 80%, and the average age was approximately 50. Most people lived in rural areas, with moderate income (quartile 3). The most common co-medications in both cohorts were nonsteroidal anti-inflammatory drugs (NSAIDs), H2-blockers, angiotensin-converting enzyme inhibitors (ACEI), angiotensin II receptor antagonists (ARB), and antiplatelet agents. The most common comorbidities were hypertension, diabetes mellitus, dyslipidemia, and chronic liver disease in both cohorts. About 1% of patients had ischemic stroke or hemorrhagic stroke.
Table 2 compares the two cohorts’ ischemic and hemorrhagic stroke incidences and HRs. The incidence (95% CI) of ischemic stroke was significantly higher in the patients with gout than in the controls (5.06 [5.00–5.13] vs. 4.87 [4.81–4.94] per 1000 person-years). The hazard ratio (HR) (95% CI) for ischemic stroke was 1.04 (1.02–1.06). However, the incidence (95% CI) and HR of ischemic stroke were lower in the gout group than in the control group in the first 3 years (incidence: 4.74 [4.60–4.88] vs. 5.17 [5.03–5.32] per 1000 person-years; HR: 0.92 [0.88–0.96]), then became significantly higher than in the controls after 3 years (Incidence: 4.10 [4.04–4.16] vs. 3.81 [3.75–3.87] per 1000 person-years; HR: 1.08 [1.05–1.10]).

Table 2.
Incidence, hazard ratios, and follow-up year for ischemic and hemorrhagic stroke among gout and non-gout cohorts in Taiwan, 2000 to 2008.
Compared with the controls, the patients with gout also had a higher incidence (95% CI) of hemorrhagic stroke (1.73 [1.69–1.77] vs. 1.60 [1.56–1.64] per 1000 person-years), and the HR (95% CI) for hemorrhagic stroke was 1.08 (1.05–1.12). However, the incidence (95% CI) and HR of hemorrhagic stroke were lower in the gout group than in the control group in the first 3 years (incidence: 1.51 [1.43–1.59] vs. 1.70 [1.62–1.79] per 1000 person-years; HR: 0.88 [0.82–0.92]), then became significantly higher than in controls after 3 years (incidence: 1.43 [1.39–1.46] vs. 1.26 [1.22–1.29] per 1000 person-years; HR: 1.14 [1.10–1.18]).
Figure 2 depicts the two-year moving average incidence rate of ischemic stroke. The incidence rate of ischemic stroke was higher in the control cohort in the first 3 years and became significantly higher in the gout cohort after 3 years. Figure 3 shows the two-year moving average incidence rate of hemorrhagic stroke. Similarly, the incidence rate of hemorrhagic stroke was higher in the control cohort in the first 3 years and then became higher in the gout cohort after 3 years.
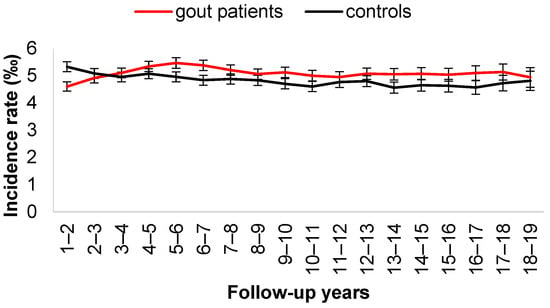
Figure 2.
Two-year moving average of incident rate of ischemic stroke.
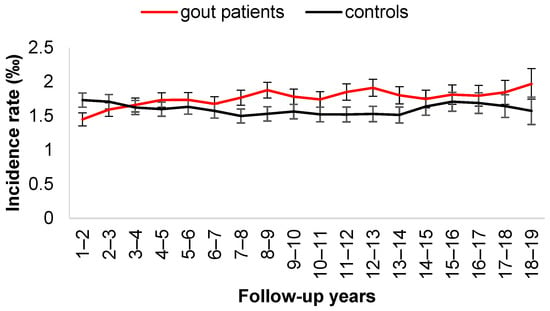
Figure 3.
Two-year moving average of incident rate of hemorrhagic stroke.
4. Discussion
For this nationwide population, we analyzed the relationship between gout and stroke. The ischemic stroke incidence was threefold higher in patients with gout than the incidence of hemorrhagic stroke. More importantly, we saw that the HR of ischemic stroke was lower in the gout group than in the control group in the first 3 years and then became significantly higher than in the controls after 3 years. A similar phenomenon was seen for hemorrhagic stroke.
The relationship between hyperuricemia, gout, and overall stroke (including ischemic and hemorrhagic stroke) has been discussed previously. Regarding overall stroke risk, Holme et al. [19] measured serum uric acid levels in 417,734 men and women during health check-ups in Sweden and found that the higher the serum uric acid levels, the higher the overall stroke risks (HR [95% CI] for overall stroke: 1.09 [1.07–1.11] in men and 1.13 [1.10–1.15] in women). Because gout is associated with MSU crystallization, which triggers downstream inflammatory responses [34,35], inflammation may also contribute to stroke [36]. Thus, investigating the gout–stroke relationship, rather than the hyperuricemia–stroke relationship, is essential. In the United Kingdom, Seminog et al. used a national dataset of hospital admissions and death records from 1999 to 2011 and found an increased overall stroke risk in patients with gout (risk ratio (RR) [95% CI]: 1.71 [1.68–1.75]) [16].
Moreover, Singh et al. used US claims data from 2007 to 2010 and reported that gout incurred an overall incident stroke risk equivalent to that of DM, indirectly demonstrating the relationship of gout with overall stroke [15]. The results of these database-based studies demonstrate that gout increases overall stroke risk. However, these results contradict those of Clarson et al., who used the data from the United Kingdom Clinical Practice Research Datalink and found HRs (95% CIs) for the overall stroke of only 0.93 (0.81–1.06) in men and 1.34 (1.15–1.57) in women [26]. However, Clarson et al. included only older patients from the United Kingdom, enrolled from 1987 to 1999, whereas the present cohort comprised a younger population from Taiwan, enrolled from 2000 to 2008. The differences can be explained further by the low prevalence of gout in older adults in earlier studies and by the high prevalence of gout in Asian-Pacific countries [37].
Among all relevant studies, the present study included the largest patient population. Furthermore, we classified patients to have overall stroke and gout only when they were hospitalized for stroke and were prescribed urate-lowering agents, respectively. Thus, the use of the relatively strict definition for the inclusion of gout cases may have contributed to the contrast between current results and the previous findings.
Ischemic stroke occurs when a blood vessel supplying blood to the brain is obstructed, whereas hemorrhagic stroke occurs when a weakened blood vessel ruptures. Consequently, these two stroke types have different outcomes [38], necessitating separate calculations of their risks. However, data on ischemic and hemorrhagic stroke risks calculated separately are limited. Holme et al. reported that elevated serum uric acid levels increased ischemic and hemorrhagic stroke risks—with HRs (95% CIs) of 1.10 (1.07–1.12) and 1.07 (1.01–1.12) in men, respectively, and 1.15 (1.12–1.17) and 1.08 (1.02–1.15) in women, respectively [19]. Moreover, Seminog et al. reported that patients with gout had increased ischemic and hemorrhagic stroke risks—with RRs (95% CIs) of 1.68 (1.64–1.73) and 1.69 (1.61–1.77), respectively [16]. Another study demonstrated that hyperuricemia might increase arterial stiffness and inflammation, supporting our finding that gout increases stroke risk [39]. In this study, the gout group has a lower HR of ischemic and hemorrhagic stroke than the control group in the first 3 years and the other way around afterward. The reason for lower ischemic and hemorrhagic stroke incidence in the gout cohort in the first 3 years was unclear. Because the definition of gout in our study requires the use of a urate-lowering agent at enrolment, a previous study showed urate-lowering agents might reduce the incidence of stroke in gout patients [40]. Thus, the temporal lower incidence of stroke in the first 3 years may be because of the interference of urate-lowering agents. Moreover, strict diet control and better drug compliance may be observed in the first 3 years after the diagnosis of gout. Therefore, the loss of the protective effect of the urate-lowering agent after the first 3 years may be related to poor adherence as time passes. Further prospective or randomized studies are suggested to investigate this temporal relationship.
We previously reported that the comorbidities of gout include cardiovascular diseases, renal diseases, the consequences of total joint replacement, and cancer [41,42,43,44,45,46]. In this study, the stroke risk was high in the gout population from Taiwan, indicating the need of monitoring gout comorbidities and stroke incidents in clinical practice. Moreover, gout can induce multiple comorbidities, influencing treatment outcome and survival [2,3,4,5,6,7]. Therefore, the management of gout should include the treatment of not only arthritis, but also systemic diseases. Consequently, considering the use of a comorbidity checklist when treating patients newly diagnosed with gout and those with existing gout is crucial.
However, this study had several drawbacks that limited the generalization of our results. First, we did not adjust the data for body mass index, smoking, dietary factors, and alcohol consumption because these data were unavailable in the NHI database. Second, we could not include serum uric acid level data or tophus formation. However, a high serum uric acid level and tophus formation reflect severe gouty arthritis, which may increase stroke risk. Third, we could not investigate whether lowering serum uric acid levels by taking urate-lowering agents reduces stroke risk, and we did not identify the urate-lowering agents that may be the most effective in this context. Further relevant exploration is thus warranted. Fourth, this study’s incidence of ischemic and hemorrhagic stroke required hospitalization. In other words, the incidence rates of the two strokes did not cover those who sought treatment through the emergency department, but were not admitted to the hospital. Fifth, the propensity score matching between the gout and non-gout cohorts allows a good balance of comorbidity and medication use at the index date, but the comorbidity and medication use might change over time, which is particularly serious in our study with a long follow-up time. Perhaps, the nested case-control study might sort out this problem [47].
In conclusion, in this population-based study in Taiwan, patients with gout demonstrated an increased stroke risk, for both ischemic and hemorrhagic stroke. Moreover, ischemic stroke incidence was threefold higher in these patients with gout than the incidence of hemorrhagic stroke. Therefore, in general, physicians should be aware of the risk of stroke in gout patients and apply relevant prevention measures.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm11133779/s1, Table S1: International Classification of Disease, Ninth Revision, Code or Procedure Codes for Comorbidities.
Author Contributions
P.-H.T. and W.-Y.T. contributed to the conception, design of the study, and interpretation; P.-H.T. wrote the first draft; L.-C.S. and C.-F.K. contributed to data acquisition, analysis, and interpretation of the data, and drafted and critically revised the manuscript; P.-R.L. and J.-S.C. contributed to the statistical analysis. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the Chang Gung Memorial Hospital (Project CMRPG2K0172 and CMRPG2K0402). The sponsor (the Chang Gung Memorial Hospital) mainly funded the acquisition costs for the National Health Insurance Database, as well as and research assistants’ personnel costs. They had no role in the design or conduct of the study, in the collection, management, analysis, or interpretation of the data, in the preparation, review, or approval of the manuscript; or in the decision to submit the manuscript for publication.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (IRB) of Chang Gung Medical Foundation (IRB number: 201800242B1).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank the statistical assistants and wish to acknowledge the support of the Maintenance Project of the Center for Artificial Intelligence in Medicine (Grant CIRPG3H0014) at Chang Gung Memorial Hospital for facilitating the study design and monitoring, as well as data analysis and interpretation. This study is based partly on the National Health Insurance (NHI) Database data provided by the Applied Health Research Data Integration Service from the NHI Administration.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Neogi, T.; Jansen, T.L.; Dalbeth, N.; Fransen, J.; Schumacher, H.R.; Berendsen, D.; Brown, M.; Choi, H.; Edwards, N.L.; Janssens, H.J.; et al. 2015 Gout Classification Criteria: An American College of Rheumatology/European League against Rheumatism Collaborative Initiative. Ann. Rheum. Dis. 2015, 74, 1789–1798. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Ford, E.S.; Li, C.; Curhan, G. Prevalence of the metabolic syndrome in patients with gout: The Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2007, 57, 109–115. [Google Scholar] [CrossRef]
- Choi, H.K.; Atkinson, K.; Karlson, E.W.; Curhan, G. Obesity, weight change, hypertension, diuretic use, and risk of gout in men: The health professionals follow-up study. Arch. Intern. Med. 2005, 165, 742–748. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.F.; See, L.C.; Luo, S.F.; Ko, Y.S.; Lin, Y.S.; Hwang, J.S.; Lin, C.M.; Chen, H.W.; Yu, K.H. Gout: An independent risk factor for all-cause and cardiovascular mortality. Rheumatology 2010, 49, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Curhan, G. Independent impact of gout on mortality and risk for coronary heart disease. Circulation 2007, 116, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.K.; Atkinson, K.; Karlson, E.W.; Willett, W.; Curhan, G. Alcohol intake and risk of incident gout in men: A prospective study. Lancet 2004, 363, 1277–1281. [Google Scholar] [CrossRef]
- Sheane, B.J.; Cunnane, G. Tophaceous gout and chronic kidney disease. J. Clin. Rheumatol. 2007, 13, 293. [Google Scholar] [CrossRef]
- Sacco, R.L.; Kasner, S.E.; Broderick, J.P.; Caplan, L.R.; Connors, J.J.; Culebras, A.; Elkind, M.S.; George, M.G.; Hamdan, A.D.; Higashida, R.T.; et al. An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 2064–2089. [Google Scholar] [CrossRef]
- Butler, R.; Morris, A.D.; Belch, J.J.; Hill, A.; Struthers, A.D. Allopurinol normalizes endothelial dysfunction in type 2 diabetics with mild hypertension. Hypertension 2000, 35, 746–751. [Google Scholar] [CrossRef]
- Mustard, J.F.; Murphy, E.A.; Ogryzlo, M.A.; Smythe, H.A. Blood Coagulation and Platelet Economy in Subjects with Primary Gout. Can. Med. Assoc. J. 1963, 89, 1207–1211. [Google Scholar]
- Kang, D.H.; Nakagawa, T.; Feng, L.; Watanabe, S.; Han, L.; Mazzali, M.; Truong, L.; Harris, R.; Johnson, R.J. A role for uric acid in the progression of renal disease. J. Am. Soc. Nephrol. 2002, 13, 2888–2897. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.; Yang, F.; Yang, I.; Yin, Y.; Luo, J.J.; Wang, H.; Yang, X.F. Uric acid, hyperuricemia and vascular diseases. Front. Biosci. 2012, 17, 656–669. [Google Scholar] [CrossRef]
- Elkind, M.S.; Cheng, J.; Rundek, T.; Boden-Albala, B.; Sacco, R.L. Leukocyte count predicts outcome after ischemic stroke: The Northern Manhattan Stroke Study. J. Stroke Cerebrovasc. Dis. 2004, 13, 220–227. [Google Scholar] [CrossRef]
- Libby, P. Inflammation in atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 2045–2051. [Google Scholar] [CrossRef]
- Singh, J.A.; Ramachandaran, R.; Yu, S.; Yang, S.; Xie, F.; Yun, H.; Zhang, J.; Curtis, J.R. Is gout a risk equivalent to diabetes for stroke and myocardial infarction? A retrospective claims database study. Arthritis Res. Ther. 2017, 19, 228. [Google Scholar] [CrossRef]
- Seminog, O.O.; Goldacre, M.J. Gout as a risk factor for myocardial infarction and stroke in England: Evidence from record linkage studies. Rheumatology 2013, 52, 2251–2259. [Google Scholar] [CrossRef]
- Li, M.; Hou, W.; Zhang, X.; Hu, L.; Tang, Z. Hyperuricemia and risk of stroke: A systematic review and meta-analysis of prospective studies. Atherosclerosis 2014, 232, 265–270. [Google Scholar] [CrossRef]
- Kim, S.Y.; Guevara, J.P.; Kim, K.M.; Choi, H.K.; Heitjan, D.F.; Albert, D.A. Hyperuricemia and risk of stroke: A systematic review and meta-analysis. Arthritis Rheum. 2009, 61, 885–892. [Google Scholar] [CrossRef]
- Holme, I.; Aastveit, A.H.; Hammar, N.; Jungner, I.; Walldius, G. Uric acid and risk of myocardial infarction, stroke and congestive heart failure in 417,734 men and women in the Apolipoprotein MOrtality RISk study (AMORIS). J. Intern. Med. 2009, 266, 558–570. [Google Scholar] [CrossRef]
- Lehto, S.; Niskanen, L.; Ronnemaa, T.; Laakso, M. Serum uric acid is a strong predictor of stroke in patients with non-insulin-dependent diabetes mellitus. Stroke 1998, 29, 635–639. [Google Scholar] [CrossRef]
- Mazza, A.; Pessina, A.C.; Pavei, A.; Scarpa, R.; Tikhonoff, V.; Casiglia, E. Predictors of stroke mortality in elderly people from the general population. The CArdiovascular STudy in the ELderly. Eur. J. Epidemiol. 2001, 17, 1097–1104. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.J.; Muir, S.W.; Walters, M.R.; Lees, K.R. Serum urate as an independent predictor of poor outcome and future vascular events after acute stroke. Stroke 2003, 34, 1951–1956. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Alderman, M.H. Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971-1992. National Health and Nutrition Examination Survey. JAMA 2000, 283, 2404–2410. [Google Scholar] [CrossRef] [PubMed]
- Hozawa, A.; Folsom, A.R.; Ibrahim, H.; Nieto, F.J.; Rosamond, W.D.; Shahar, E. Serum uric acid and risk of ischemic stroke: The ARIC Study. Atherosclerosis 2006, 187, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.F.; Yu, K.H.; See, L.C.; Chou, I.J.; Tseng, W.Y.; Chang, H.C.; Shen, Y.M.; Luo, S.F. Elevated risk of mortality among gout patients: A comparison with the national population in Taiwan. Jt. Bone Spine 2011, 78, 577–580. [Google Scholar] [CrossRef]
- Clarson, L.E.; Hider, S.L.; Belcher, J.; Heneghan, C.; Roddy, E.; Mallen, C.D. Increased risk of vascular disease associated with gout: A retrospective, matched cohort study in the UK clinical practice research datalink. Ann. Rheum. Dis. 2015, 74, 642–647. [Google Scholar] [CrossRef]
- Culleton, B.F.; Larson, M.G.; Kannel, W.B.; Levy, D. Serum uric acid and risk for cardiovascular disease and death: The Framingham Heart Study. Ann. Intern. Med. 1999, 131, 7–13. [Google Scholar] [CrossRef]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Cheng, C.L.; Kao, Y.H.; Lin, S.J.; Lee, C.H.; Lai, M.L. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol. Drug Saf. 2011, 20, 236–242. [Google Scholar] [CrossRef]
- McCaffrey, D.F.; Griffin, B.A.; Almirall, D.; Slaughter, M.E.; Ramchand, R.; Burgette, L.F. A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat. Med. 2013, 32, 3388–3414. [Google Scholar] [CrossRef]
- Austin, P.C. Using the Standardized Difference to Compare the Prevalence of a Binary Variable between Two Groups in Observational Research. Commun. Stat. Simul. Comput. 2009, 38, 1228–1234. [Google Scholar] [CrossRef]
- Zar, J.H. Biostatistical Analysis, 4th ed.; Prentice-Hall Inc.: Hoboken, NJ, USA, 1999. [Google Scholar]
- Austin, P.C. The use of propensity score methods with survival or time-to-event outcomes: Reporting measures of effect similar to those used in randomized experiments. Stat. Med. 2014, 33, 1242–1258. [Google Scholar] [CrossRef] [PubMed]
- Chhana, A.; Lee, G.; Dalbeth, N. Factors influencing the crystallization of monosodium urate: A systematic literature review. BMC Musculoskelet. Disord. 2015, 16, 296. [Google Scholar] [CrossRef]
- Terkeltaub, R. What makes gouty inflammation so variable? BMC Med. 2017, 15, 158. [Google Scholar] [CrossRef] [PubMed]
- Lindsberg, P.J.; Grau, A.J. Inflammation and infections as risk factors for ischemic stroke. Stroke 2003, 34, 2518–2532. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.F.; Grainge, M.J.; Zhang, W.; Doherty, M. Global epidemiology of gout: Prevalence, incidence and risk factors. Nat. Rev. Rheumatol. 2015, 11, 649–662. [Google Scholar] [CrossRef]
- Bhalla, A.; Wang, Y.; Rudd, A.; Wolfe, C.D. Differences in outcome and predictors between ischemic and intracerebral hemorrhage: The South London Stroke Register. Stroke 2013, 44, 2174–2181. [Google Scholar] [CrossRef]
- Tomiyama, H.; Shiina, K.; Vlachopoulos, C.; Iwasaki, Y.; Matsumoto, C.; Kimura, K.; Fujii, M.; Chikamori, T.; Yamashina, A. Involvement of Arterial Stiffness and Inflammation in Hyperuricemia-Related Development of Hypertension. Hypertension 2018, 72, 739–745. [Google Scholar] [CrossRef]
- Niu, S.W.; Hung, C.C.; Lin, H.Y.; Kuo, I.C.; Huang, J.C.; He, J.S.; Wen, Z.H.; Liang, P.I.; Chiu, Y.W.; Chang, J.M.; et al. Reduced Incidence of Stroke in Patients with Gout Using Benzbromarone. J. Pers. Med. 2022, 12, 28. [Google Scholar] [CrossRef]
- Kuo, C.F.; Yu, K.H.; See, L.C.; Chou, I.J.; Ko, Y.S.; Chang, H.C.; Chiou, M.J.; Luo, S.F. Risk of myocardial infarction among patients with gout: A nationwide population-based study. Rheumatology 2013, 52, 111–117. [Google Scholar] [CrossRef]
- Yu, K.H.; Kuo, C.F.; Luo, S.F.; See, L.C.; Chou, I.J.; Chang, H.C.; Chiou, M.J. Risk of end-stage renal disease associated with gout: A nationwide population study. Arthritis Res. Ther. 2012, 14, R83. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.F.; Chou, I.J.; See, L.C.; Chen, J.S.; Yu, K.H.; Luo, S.F.; Hsieh, A.H.; Zhang, W.; Doherty, M. Urate-lowering treatment and risk of total joint replacement in patients with gout. Rheumatology 2018, 57, 2129–2139. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.F.; Grainge, M.J.; Mallen, C.; Zhang, W.; Doherty, M. Impact of gout on the risk of atrial fibrillation. Rheumatology 2016, 55, 721–728. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kuo, C.F.; Luo, S.F.; See, L.C.; Chou, I.J.; Fang, Y.F.; Yu, K.H. Increased risk of cancer among gout patients: A nationwide population study. Jt. Bone Spine 2012, 79, 375–378. [Google Scholar] [CrossRef]
- Kuo, C.F.; See, L.C.; Yu, K.H.; Chou, I.J.; Chiou, M.J.; Luo, S.F. Significance of serum uric acid levels on the risk of all-cause and cardiovascular mortality. Rheumatology 2013, 52, 127–134. [Google Scholar] [CrossRef]
- Thillemann, T.M.; Pedersen, A.B.; Mehnert, F.; Johnsen, S.P.; Soballe, K. The risk of revision after primary total hip arthroplasty among statin users: A nationwide population-based nested case-control study. JBJS 2010, 92, 1063–1072. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).