Comparison of Malocclusion Prevalence, Type and Severity between Cerebral Palsy and Healthy Subjects: A Prospective Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Determinations of the Type of Cerebral Palsy (CP)
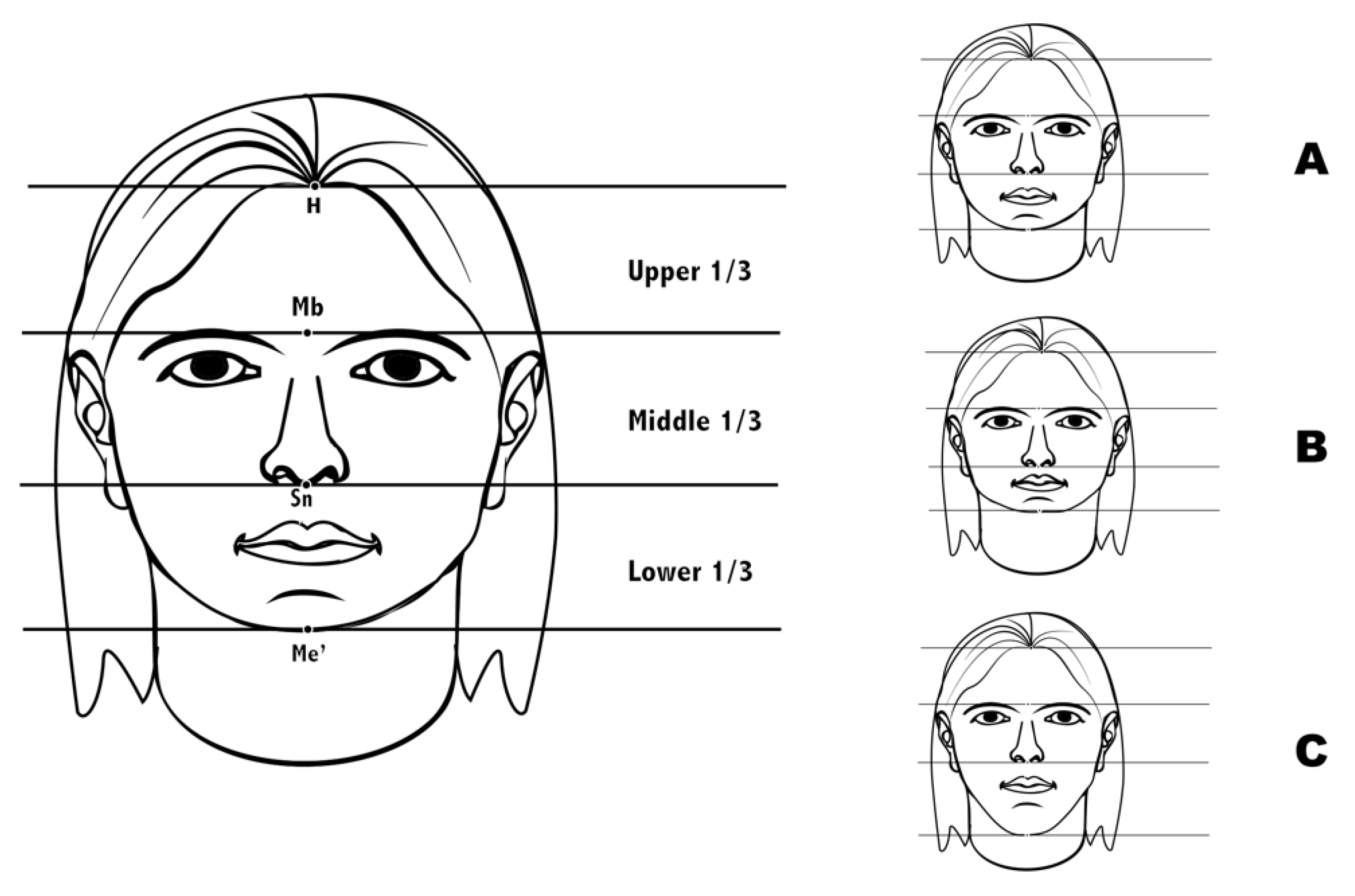
2.3. Extraoral Facial Thirds Measurements
2.4. Intraoral Occlusal Measurements
2.5. Dental Aesthetic Index (DAI) Components
2.6. Diet and Oral Habits Questionary
2.7. Breathing Type
2.8. Statistical Analysis
3. Results
3.1. Reproducibility
3.2. Sample Size and Groups
3.3. Extraoral Facial Thirds Measurements
3.4. Intraoral Occlusal Measurements
3.5. Dental Aesthetic Index (DAI) Components
3.6. Diet and Oral Habits Questionary
3.7. Breathing Type
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rethlefsen, S.A.; Ryan, D.D.; Kay, R.M. Classification systems in cerebral palsy. Orthop. Clin. N. Am. 2010, 41, 457–467. [Google Scholar]
- Blair, E. Epidemiology of the cerebral palsies. Orthop. Clin. N. Am. 2010, 41, 441–455. [Google Scholar] [CrossRef] [PubMed]
- Sankar, C.; Mundkur, N. Cerebral palsy-definition, classification, etiology and early diagnosis. Indian J. Pediatr. 2005, 72, 865–868. [Google Scholar] [CrossRef]
- Dougherty, N.J. A review of cerebral palsy for the oral health professional. Dent. Clin. N. Am. 2009, 53, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Krigger, K.W. Cerebral palsy: An overview. Am. Fam. Physician 2006, 73, 91–100. [Google Scholar]
- Winter, K.; Baccaglini, L.; Tomar, S. A review of malocclusion among individuals with mental and physical disabilities. Spec. Care Dent. 2008, 28, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Miamoto, C.B.; Ramos-Jorge, M.L.; Pereira, L.J.; Paiva, S.M.; Pordeus, I.A.; Marques, L.S. Severity of malocclusion in patients with cerebral palsy: Determinant factors. Am. J. Orthod. Dentofac. Orthop. 2010, 138, e1–e5. [Google Scholar] [CrossRef]
- Proffit, W.R. Equilibrium theory revisited: Factors influencing position of the teeth. Angle. Orthod. 1978, 48, 175–186. [Google Scholar] [PubMed]
- Harvold, E.; Chieri, G.; Vargervik, K. Experiments on the development of dental malocclusions. Am. J. Orthod. 1972, 61, 38–44. [Google Scholar] [CrossRef]
- Mamaghani, S.M.; Bode, H.; Ehmer, U. Orofacial findings in conjunction with infantile cerebral paralysis in adults of two different age groups-a cross-sectional study. J. Orofac. Orthop. 2008, 69, 240–256. [Google Scholar] [CrossRef] [PubMed]
- Franklin, D.L.; Luther, F.; Curzon, M.E. The prevalence of malocclusion in children with cerebral palsy. Eur. J. Orthod. 1996, 18, 637–643. [Google Scholar] [CrossRef] [PubMed]
- Strodel, B.J. The effects of spastic cerebral palsy on occlusion. ASDC J. Dent. Child. 1987, 54, 255–260. [Google Scholar] [PubMed]
- Papazian, O.; Alfonso, I. Cerebral palsy theraphy. Rev. Neurol. 1997, 25, 728–739. [Google Scholar] [PubMed]
- Jenny, J.; Cons, N.C. Establising malocclusion severity levels on the dental aesthetic index (DAI) scale. Aust. Dent. J. 1996, 41, 43–46. [Google Scholar] [CrossRef]
- Bensi, C.; Costacurta, M.; Docimo, R. Oral health in children with cerebral palsy: A systematic review and meta-analysis. Spec. Care Dent. 2020, 40, 401–411. [Google Scholar] [CrossRef]
- Medeiros-Rodrigues-Cardoso, A.; Duarte-Silva, C.R.; Nóbrega-Gomes, L.; Marinho-Davino de Medeiros, M.; Nascimento-Padilha, W.W.; Cabral-Cavalcanti, A.F.; Leite-Cavalcanti, A. Prevalence of Malocclusions and Associated Factors in Brazilian Children and Adolescents with CerebralPalsy: A Multi-Institutional Study. Int. J. Dent. 2020, 29, 1–10. [Google Scholar] [CrossRef]
- Martínez-Mihi, V.; Silvestre, F.J.; Orellana, L.; Silvestre-Rangil, J. Resting position of the head and malocclusion in a group of patients with cerebral palsy. J. Clin. Exp. Dent. 2014, 6, e1–e6. [Google Scholar] [CrossRef]
- Vellappally, S.; Gardens, S.J.; Al Kheraif, A.A.; Krushna, M.; Babu, S.; Hashem, M.; Jacob, V.; Anil, S. The prevalence of malocclusions and its association with dental caries among 12–21 year-old disabled adolescents. BMC Oral. Health 2014, 14, 123. [Google Scholar] [CrossRef]
- Oliveira, A.C.; Paiva, S.M.; Martins, M.T.; Torres, C.S.; Pordeus, I.A. Prevalence and determinant factors of malocclusion in children with special needs. Eur. J. Orthod. 2011, 33, 413–418. [Google Scholar] [CrossRef][Green Version]
- Bakarcić, D.; Lajnert, V.; Maricić, B.M.; Jokić, N.I.; Vrancić, Z.R.; Grzić, R.; Prpić, I. The Comparison of Malocclusion Prevalence Between Children with Cerebral Palsy and Healthy Children. Coll Antropol. 2015, 39, 663–666. [Google Scholar]
- Arnett, G.W.; Bergman, R.T. Facial keys to orthodontic diagnosis and treatment planning—Part II. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 395–411. [Google Scholar] [CrossRef]
- Angle, E. Classification of maloclussion. Dent. Cosmos 1899, 41, 248–269. [Google Scholar]
- Santos, M.T.; Masiero, D.; Ferreira, N.; Lorenzetti, M.R. Oral conditions in children with cerebral palsy. J. Dent. Child 2003, 70, 40–46. [Google Scholar]
- Carmagnani, F.G.; Gonçalves, G.K.; Corrêa, M.S.; dos Santos, M.T. Occlusal characteristics in cerebral palsy patients. J. Dent. Child 2007, 74, 41–45. [Google Scholar]
- Barrionuevo, L.; Solís, F. Anomalías dento maxilares y factores asociados en niños con parálisis cerebral. Rev. Child. Pediatr. 2008, 79, 272–280. [Google Scholar] [CrossRef][Green Version]
- Foster, T.D.; Griffiths, M.I.; Gordon, P.H. The effects of cerebral palsy on the size and form of the skull. Am. J. Orthod. 1974, 66, 40–49. [Google Scholar] [CrossRef]
- Pope, J.E.C.; Curzon, M.E.J. The dental status of cerebral palsied children. Pediatr. Dent. 1991, 13, 156–162. [Google Scholar]
- Oreland, A.; Heijbel, J.; Jagell, S. Malocclusion in physically and/or mentally handicapped children. Swed. Dent. J. 1987, 11, 103–119. [Google Scholar]
- De Carvalho, R.B.; Mendes, R.F.; Prado, R.R.; Moita-Neto, J.M. Oral health and oral motor function in children with cerebral palsy. Spec. Care Dent. 2011, 31, 58–62. [Google Scholar] [CrossRef]
- Rosembaum, C.H.; McDonald, R.E.; Levitt, E.E. Occlusion of cerebral palsied children. J. Dent. Res. 1966, 45, 1696–1700. [Google Scholar] [CrossRef]
- Schwartz, S.; Gisel, E.G.; Clarke, D.; Haberfellner, H. Association of occlusion with eating efficiency in children with cerebral palsy and moderate eating impairment. J. Dent. Child. 2003, 70, 33–39. [Google Scholar]
- Du, R.Y.; McGrath, C.; Yiu, C.K.T.; King, N.M. Oral health in preschool children with cerebral palsy: A case-control community-based study. Int. Paediatr. Dent. 2010, 20, 330–335. [Google Scholar] [CrossRef] [PubMed]
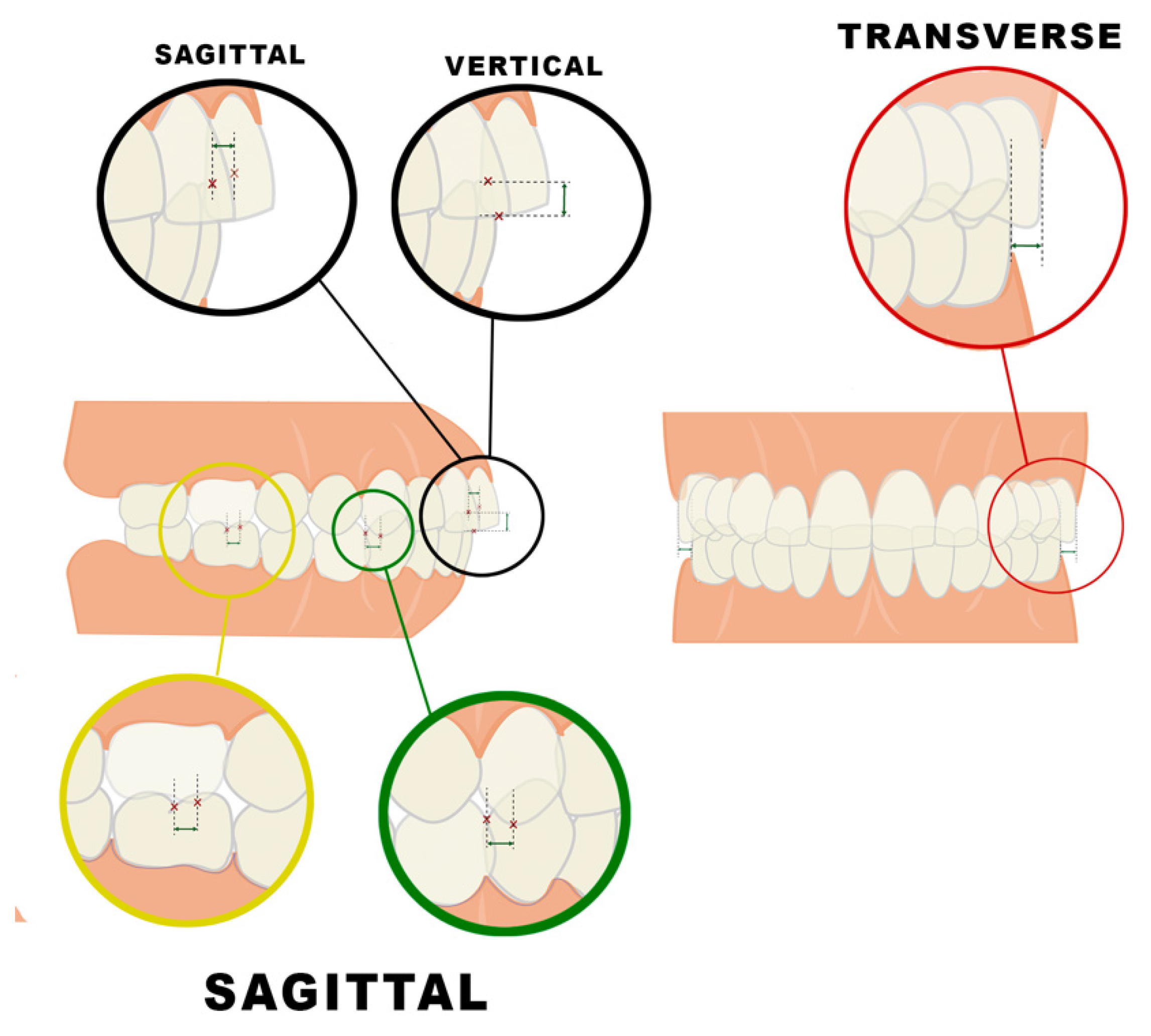
| SAGITTAL PLANE | |||
|---|---|---|---|
| MOLAR CLASS Distance between the mesiobuccal cusp of the upper first molar and the mesiobuccal sulcus of the lower first molar | I | II | III |
| =0 mm | >0 mm | <0 mm | |
| CANINE CLASS Distance between the cusp of the upper canine and the contact point between canine and lower first premolar | I | II | III |
| =0 mm | >0 mm | <0 mm | |
| OVERJET Distance between the labial surface of the lower central incisor and the incisal margin of the upper central incisor considering normal 0–4 mm | |||
| VERTICAL PLANE | |||
| OVERBITE Distance between upper and lower incisal margins. Considering normal 0–4 mm. −1 mm or below was considered open bite | |||
| TRANSVERSE PLANE | |||
| TRASNVERSE RELATION Distance between the buccal surfaces of the upper and lower posterior molars (unilateral or bilateral nature) | NORMAL | NARROW | CROSSBITE |
| =2 mm | Narrow = 0–2 mm | Crossbite < 0 mm | |
| DAI Components | SCORE | |||
|---|---|---|---|---|
| 0 | 1 | 2 | ||
| 1 | Number of visible missing teeth in both arches (incisors, canines and premolars) | |||
| 2 | Assessment crowding in the incisal segments | No crowded segments | One crowded segment | Two crowded segments |
| 3 | Assessment spacing in the incisal segments | No spaced segments | One spaced segment | Two spaced segments |
| 4 | Measurement of any midline diastema (mm) | |||
| 5 | Largest anterior irregularity on the maxilla (mm) | |||
| 6 | Largest anterior irregularity on the mandible (mm) | |||
| 7 | Measurement of anterior maxillary overjet (mm) | |||
| 8 | Measurement of anterior mandibular overjet (mm) | |||
| 9 | Measurement of vertical anterior open bite (mm) | |||
| 10 | Assessment of sagittal molar relation; largest deviation from normal either left or right | Normal | 1/2 cusp either mesial or distal | One full cusp or more either mesial or distal |
| TOTAL | ||||
| RESULTS Group 1 < 25 points = no anomalies with no need of orthodontic treatment Group 2 = 26–30 points, indicative of malocclusion, with optional treatment Group 3 = 31–35, indicative of severe malocclusion, with highly recommendable treatment Group 4 > 36 points, indicative of very severe malocclusion, in which treatment proves crucial | ||||
| VARIABLES | CP Group | Control Group | p-Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| SAGITTAL RELATION. RIGHT MOLAR CLASS | |||||
| Class I | 26 | 43.3 | 41 | 68.3 | 0.039 * χ² |
| Class II | 24 | 40.0 | 6 | 10.0 | |
| Class III | 9 | 15.0 | 13 | 21.6 | |
| SAGITTAL RELATION. LEFT MOLAR CLASS | |||||
| Class I | 16 | 26.6 | 36 | 60.0 | 0.194 χ² |
| Class II | 24 | 40.0 | 9 | 15.0 | |
| Class III | 18 | 30.0 | 15 | 25.0 | |
| SAGITTAL RELATION. RIGHT CANINE CLASS | |||||
| Class I | 22 | 36.6 | 39 | 65.0 | 0.007 * χ² |
| Class II | 28 | 46.6 | 15 | 25.0 | |
| Class III | 8 | 13.3 | 6 | 10.0 | |
| SAGITTAL RELATION. LEFT CANINE CLASS | |||||
| Class I | 19 | 31.6 | 42 | 70.0 | 0.018 * χ² |
| Class II | 28 | 46.6 | 12 | 20.0 | |
| Class III | 11 | 18.3 | 6 | 10.0 | |
| SAGITTAL RELATION. OVERJET | |||||
| Mean ± SD = 5.6 ± 5.0 mm Max (16 mm) Min (−9 mm) | Mean ± SD = 2.4 ± 1.5 mm Max (6 mm) Min (−1 mm) | <0.001 *** t | |||
| VERTICAL RELATION. OVERBITE | |||||
| Mean ± SD = −7.5 ± 6.7 mm Max (−1 mm) Min (−20 mm) | Mean ± SD = −2.0 ± 1.2 mm Max (−3 mm) Min (−1 mm) | <0.001 *** t | |||
| TRANSVERSE RELATION | |||||
| Normal | 16 | 26.7 | 52 | 86.7 | <0.001 *** χ² |
| Narrowing | 33 | 55.0 | 5 | 8.3 | |
| Unilateral Cross Bite | 9 | 15.0 | 1 | 1.7 | |
| Bilateral Cross Bite | 2 | 3.3 | 2 | 3.3 | |
| GROUP | DAI SCORES | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤25 | 26–30 | 31–35 | ≥36 | p-Value | Mean ± SD (Min–Max) − Median | p-Value | |||||
| n | % | n | % | n | % | n | % | ||||
| CP | 3 | 5.0 | 10 | 16.7 | 7 | 11.7 | 40 | 66.7 | <0.001 *** χ² | 50.1 ± 27.4 (22.0–133.0) − 40.5 | <0.001 t *** |
| Control | 44 | 73.3 | 10 | 16.7 | 3 | 5.0 | 3 | 5.0 | 23.3 ± 5.3 (14.0–41.0) − 22.0 | ||
| DAI/OralVariables | CP Group | Control Group | p-Value, Factor | p-Value, Group | p-Value, Interaction | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| CROWDING incisal segments | |||||||
| 0 segment | 21 | 35.0 | 17 | 28.3 | 0.584 | <0.001 *** | 0.179 |
| 1 segment | 24 | 40.0 | 28 | 46.7 | |||
| 2 segments | 15 | 25.0 | 15 | 25 | |||
| SEPARATION incisal segments | |||||||
| 0 segment | 26 | 43.3 | 53 | 88.3 | 0.467 | <0.001 *** | 0.562 |
| 1 segment | 18 | 30.0 | 6 | 10.0 | |||
| 2 segments | 16 | 26.7 | 1 | 1.7 | |||
| TRANSVERSE RELATION | 0.006 ** | <0.001 *** | 0.133 | ||||
| SAGITTAL MOLAR RELATION | |||||||
| Normal | 7 | 11.7 | 31 | 51.7 | 0.242 | <0.001 *** | 0.519 |
| Semi-cusp | 35 | 58.3 | 24 | 40.0 | |||
| Complete cusp | 18 | 30.0 | 5 | 8.3 | |||
| Mean ± SD | Mean ± SD | ||||||
| Right Molar Relation | 0.9 ± 3.5 | −0.2 ± 1.7 | 0.140 | <0.001 *** | 0.530 | ||
| Left Molar Relation | 0.6 ± 3.6 | −0.1 ± 1.6 | 0.422 | <0.001 *** | 0.887 | ||
| Maxillary Maximum irregularity | 1.1 ± 1.2 | 0.9 ± 1.2 | 0.073 | <0.001 *** | 0.734 | ||
| Mandibular Maximum irregularity | 1.9 ± 1.5 | 1.0 ± 0.7 | 0.417 | <0.001 *** | 0.855 | ||
| INTERINCISAL DIASTEMA | 1.0 ± 1.7 | 0.2 ± 0.7 | <0.001 *** | <0.001 *** | 0.220 | ||
| VERTICAL RELATION | −1.0 ± 7.0 | 2.6 ± 2.0 | <0.001 *** | <0.001 *** | <0.001 *** | ||
| VERTICAL ANTERIOR Open bite | −7.5 ± 6.7 | −2.0 ± 1.2 | |||||
| OVERJET | 5.6 ± 5.0 | 2.4 ± 1.5 | <0.008 *** | <0.001 *** | 0.723 | ||
| Increased overjet | 8.80 ± 2.9 | 5.14 ± 0.37 | |||||
| TYPE OF DIET | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BREATHING TYPE | TOTAL | SOLID | SEMISOLID | SHREDDED | FED BY TUBE | |||||
| n | % | n | % | n | % | n | % | n | % | |
| TOTAL | 60 | 100 | 27 | 100 | 11 | 100 | 18 | 100 | 4 | 100 |
| NASAL | 14 | 23.3 | 12 | 44.4 | 1 | 9.1 | 1 | 5.6 | 0 | 0 |
| MIXED | 46 | 76.7 | 15 | 55.6 | 10 | 90.9 | 17 | 94.4 | 4 | 100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Mihi, V.; Paredes-Gallardo, V.; Silvestre, F.-J.; Silvestre-Rangil, J. Comparison of Malocclusion Prevalence, Type and Severity between Cerebral Palsy and Healthy Subjects: A Prospective Case-Control Study. J. Clin. Med. 2022, 11, 3711. https://doi.org/10.3390/jcm11133711
Martínez-Mihi V, Paredes-Gallardo V, Silvestre F-J, Silvestre-Rangil J. Comparison of Malocclusion Prevalence, Type and Severity between Cerebral Palsy and Healthy Subjects: A Prospective Case-Control Study. Journal of Clinical Medicine. 2022; 11(13):3711. https://doi.org/10.3390/jcm11133711
Chicago/Turabian StyleMartínez-Mihi, Victoria, Vanessa Paredes-Gallardo, Francisco-Javier Silvestre, and Javier Silvestre-Rangil. 2022. "Comparison of Malocclusion Prevalence, Type and Severity between Cerebral Palsy and Healthy Subjects: A Prospective Case-Control Study" Journal of Clinical Medicine 11, no. 13: 3711. https://doi.org/10.3390/jcm11133711
APA StyleMartínez-Mihi, V., Paredes-Gallardo, V., Silvestre, F.-J., & Silvestre-Rangil, J. (2022). Comparison of Malocclusion Prevalence, Type and Severity between Cerebral Palsy and Healthy Subjects: A Prospective Case-Control Study. Journal of Clinical Medicine, 11(13), 3711. https://doi.org/10.3390/jcm11133711








